Abstract
Background:
Antihypertensive drugs have been linked to new-onset osteoporotic fracture (NOF), and different classes of antihypertensive drugs may alter the risk for the development of NOF; however, the classic effect of different antihypertensive drugs on the development of NOF in the elderly has not been well studied during long-term follow-up.
Methods:
In this study, we investigated the association between different classic antihypertensives and the development of NOF in the elderly. This was a longitudinal cohort study performed using data from claim forms submitted to the Taiwan Bureau of National Health Insurance in Central Taiwan, China including case patients with NOF aged 65–80 years from January 2002 to December 2012 and non-NOF controls. Prescriptions for antihypertensives before the index date were retrieved from a prescription database. We estimated the hazard ratios (HRs) of NOF associated with antihypertensive use. Non-NOF controls served as the reference group.
Results:
A total of 128 patients with NOF were identified from among 1144 patients with hypertension during the study period. The risk of NOF after adjusting age, sex, comorbidities, and concurrent medications was higher among the users of angiotensin-converting enzyme (ACE) inhibitors (HR, 1.64; 95% confidence interval [CI], 1.01–2.66) than among nonusers. Patients who took calcium channel blockers (CCBs) (HR, 0.70; 95% CI, 0.49–0.99) were at a lower risk of developing NOF than nonusers. Loop diuretics, thiazide diuretics, angiotensin receptor blocker, beta-blocker, and alpha-blocker were not associated with the risk of NOF.
Conclusions:
Elderly with hypertension who take CCBs are at a lower risk of NOF and that the use of ACE inhibitors was associated with a significantly increased risk of developing NOF during the 11-year follow-up.
Keywords: Antihypertensive Drugs, Elderly, New-onset Osteoporosis Fracture
Introduction
Aging of the world's population is inevitable. Concerns about the health care of the elderly, particularly in terms of age-related diseases, have gradually increased worldwide.[1,2] Osteoporotic fracture, which is more common in older than in younger individuals, is considered an age-related disease. Osteoporotic fractures result in significant health-care costs because they have been shown to adversely affect the health-related quality of life and have become a major public health problem.[3,4]
Hypertension is a risk factor for osteoporotic fracture and significantly contributes to morbidity and mortality both in men and women.[4,5,6] Recently, several prospective trials led to a debate on whether the use of antihypertensive drugs is associated with new-onset osteoporotic fracture (NOF) in hypertensive patients undergoing treatment.[7,8,9,10] However, the results of these studies are inconsistent, partly because of a head-to-head comparison of antihypertensive agents and short follow-up periods.[10,11,12] It is also unclear whether certain antihypertensive drug classes are associated with a higher risk of NOF when compared with other antihypertensive drug classes in the elderly population during long-term follow-up. Therefore, this study aimed to investigate the effect of classic antihypertensive drugs (diuretics, beta-blockers, calcium channel blockers [CCBs], alpha-blockers, angiotensin-converting enzyme [ACE] inhibitors, and angiotensin receptor blockers [ARBs]) on NOF among elderly hypertensive patients by conducting a retrospective cohort study in Taiwan, China.
Methods
Study population
Data were collected from claim forms of the Taiwan National Health Insurance (NHI) that had been submitted to the Taiwan Bureau of National Health Insurance in Central Taiwan, China, from January 2002 to December 2012. The Taiwan NHI program has been operating since 1995 and represents approximately 99% of population in Taiwan, China. The claim forms contain inpatient and outpatient records. The information from the claim forms is stored in two tables: a visit table and a prescription table. Visit tables contain patient identification numbers, sex, age, three diagnostic codes, medical expenditures, and hospital and physician information. Prescription tables contain the quantity and expenditure of all drugs, surgeries, and treatments. Patients were included in the study if they had been diagnosed with hypertension without osteoporotic fracture at baseline (January 1, 2002). We summarized the claim records of each patient into one record.
Study design
Participants were included in the study if they had been diagnosed with hypertension (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 401–405) from January 1, 2002 to June 30, 2002. At least one of the following enrollment criteria had to be met for inclusion in the study: (1) two or more outpatient visits within a 6-month period; (2) all prescriptions of antihypertensive drugs continuously administered to the patients for more than 6 months within an 11-year follow-up period; or (3) one or more inpatient admissions with a diagnosis of hypertension. The primary end point was the development of NOF, which was defined by the time an osteoporotic fracture (ICD-9-CM codes 733.11 and 805–829) or fracture-related surgery (ICD-9-CM codes 78.1, 78.4, 78.5, 78.9, 79, and 81)first appeared in the inpatient or outpatient claim records. Comorbidities related to osteoporotic fracture were defined according to the ICD-9-CM code and included coronary artery disease (ICD-9-CM code 410–415), hyperlipidemia (ICD-9-CM code 272), diabetes mellitus (ICD-9-CM code 250), and chronic kidney disease (ICD-9-CM code 585). Antihypertensive drugs are available only by prescription in Taiwan, China. Patients using only one type of antihypertensive drug before the development of NOF were categorized as single users based on the antihypertensive drug class prescribed, including loop or thiazide diuretics, alpha-blockers, beta-blockers, CCBs, ACE inhibitors, and ARBs. Patients using more than one type of antihypertensive drug before the development of NOF were categorized as combined users. Patients who fulfilled any of the following criteria were excluded from the study: (1) had a prior history of osteoporotic fracture or fracture-related surgery; (2) patients taking calcium supplements, biphosphates, selective serotonin-specific reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants, estrogen, or calcitonin; and (3) patients suffering from other major medical problems, leaving the patient with a life expectancy of <6 months. Initially, 1567 outpatients fulfilled the inclusion criteria; however, 291 patients were excluded from the study based on the diagnosis of osteoporotic fracture before January 1, 2002. Therefore, a total of 1276 patients were enrolled in the study at baseline [Figure 1]. Furthermore, 118 patients who were lost at follow-up and 17 patients who died without the diagnosis of NOF or NOF-related death were excluded from the study. Finally, a total of 1144 outpatients were included in this study. This study was approved by the Ethics Committee of China Medical University Hospital (DMR101-IRB2-194). The Ethics Committee waived the need for patient consent for this study.
Figure 1.
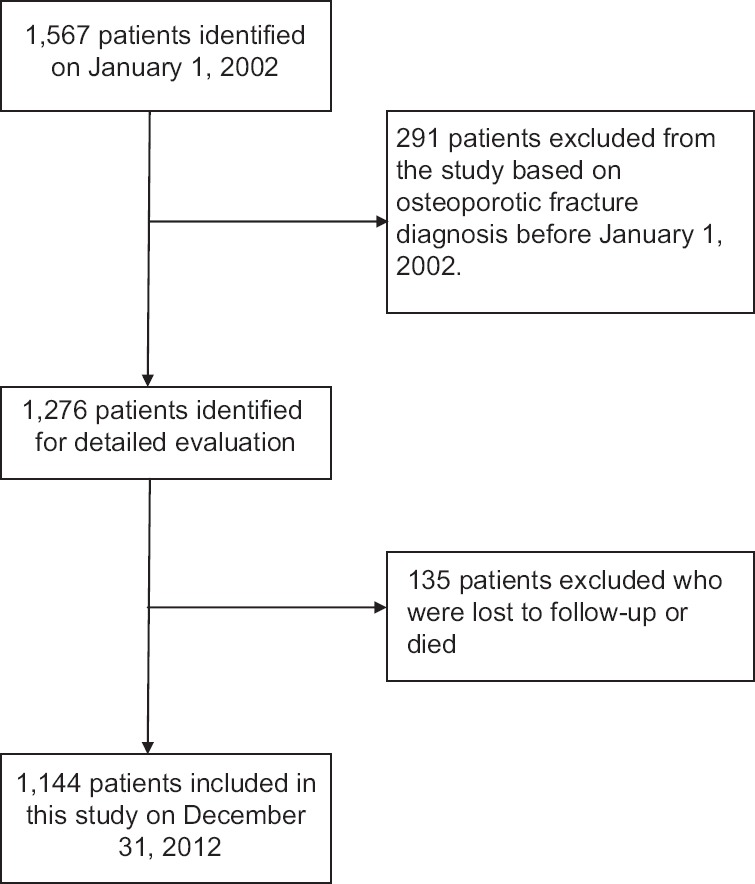
Flowchart of selection of patients for the inclusion in this study.
Statistical analysis
Data were presented as valid percentages and mean values with standard deviations. Chi-square test and t-test were used for univariate analyses. This study aimed to examine the association between the use of certain antihypertensive drug classes and NOF. The Cox proportional hazard regression model was used to compare the NOF development between antihypertensive drug users and nonusers. Adjusted hazard ratios (HRs) and 95% confidence intervals (CI) were calculated, adjusting for important factors, including age, sex, comorbidities, and concurrent medication. P < 0.05 was considered statistically significant. All statistical calculations were performed using Statistical Analysis software, version 9.3 (SAS institute, Inc., Cary, NC, USA).
Results
Baseline characteristics of patients
Baseline characteristics, comorbidities, and concurrent medication use among the overall study population are shown in Table 1. Among 1144 eligible patients with defined hypertension, 128 (11.4%) developed NOF from January 2002 to December 2012. The mean age for NOF patients was 78.9 years and that of non-NOF patients was 75.6 years. There were statistically significant differences in age between these two groups of patients (P < 0.001).
Table 1.
Baseline characteristics of all eligible patients with defined hypertension
| Characteristics | NOF (n = 128) | non-NOF (n = 1016) | Total (N = 1144) | P* |
|---|---|---|---|---|
| Age (years) | 78.9 ± 7.0 | 75.6 ± 6.3 | 75.9 ± 6.4 | <0.001 |
| Male | 33 (25.8) | 466 (45.9) | 499 (43.6) | <0.001 |
| Female | 95 (74.2) | 550 (54.1) | 645 (56.4) | <0.001 |
| Number of prescription | ||||
| 1 | 44 (34.4) | 220 (21.7) | 264 (23.1) | 0.002 |
| 2 | 45 (35.2) | 378 (37.2) | 423 (37.0) | |
| 3 | 35 (27.3) | 309 (30.4) | 344 (30.1) | |
| 4 | 4 (3.1) | 108 (10.6) | 112 (9.8) | |
| Comorbidities | ||||
| Coronary artery diseases | 10 (7.8) | 89 (8.8) | 99 (8.7) | 0.674 |
| Hyperlipidemia | 33 (25.8) | 382 (37.6) | 415 (36.3) | <0.001 |
| Diabetes mellitus | 38 (29.7) | 370 (36.4) | 408 (35.7) | 0.134 |
| Chronic kidney disease | 10 (7.8) | 90 (8.9) | 100 (8.7) | 0.693 |
| Drug class | ||||
| Loop diuretics | 15 (11.7) | 107 (10.5) | 122 (10.7) | 0.685 |
| Thiazide diuretics | 37 (28.9) | 365 (35.9) | 402 (35.1) | <0.001 |
| Beta-blockers | 43 (33.6) | 422 (41.5) | 465 (40.6) | <0.001 |
| CCBs | 80 (62.5) | 708 (69.7) | 788 (68.8) | <0.001 |
| Alpha-blockers | 4 (3.1) | 94 (9.3) | 98 (8.6) | <0.001 |
| ACE inhibitors | 20 (15.6) | 124 (12.2) | 144 (12.6) | 0.001 |
| ARBs | 57 (44.5) | 536 (52.8) | 593 (51.8) | <0.001 |
| Concurrent medications | ||||
| Aspirin | 110 (85.9) | 854 (84.1) | 964 (84.3) | |
| Statins | 45 (35.2) | 354 (34.8) | 399 (34.9) | |
| PPIs/H2 blockers | 6 (4.7) | 82 (8.1) | 88 (7.7) | 0.176 |
| Non-BZD hypnotics | 34 (26.6) | 271 (26.7) | 305 (26.7) | 0.979 |
| Inhaled corticosteroids | 4 (3.1) | 25 (2.5) | 29 (2.5) | 0.652 |
Data were presented as mean ± SD or n (%).*P value between NOF and non-NOF. NOF: New-onset osteoporotic fracture; CCBs: Calcium channel blockers; ACE: Angiotensin-converting enzyme; ARBs: Angiotensin receptor blockers; PPIs: Proton pump inhibitors; BZD: Benzodiazepine; SD: Standard deviation.
In total, 264 (23.1%) patients took a drug of only one class, 423 (37.0%) took drugs from two classes, 344 (30.1%) took drugs from three classes, and 112 (9.8%) took drugs from four classes. Over 50% of the patients took CCBs (788, 68.8%) or ARBs (593, 51.8%). Only 9.8% (86) of the patients took an alpha-blocker. The distributions of prescription loop (10.7%) or thiazide diuretics (35.1%), beta-blockers (40.6%), and ACE inhibitors (12.6%) used are shown in Table 1.
Relative risk of new-onset osteoporotic fracture
The crude HR of NOF was lower for alpha-blockers users [HR, 0.37; 95% CI, 0.11–1.00, Table 2]. After adjusting for age, sex, comorbidities, and concurrent medication, the risk of NOF development was not associated with the use of alpha-blockers [HR, 0.42; 95% CI, 0.15–1.18, Table 2]. Initially, the crude HR of NOF development was not statistically significantly different for CCBs or ACE inhibitor users. However, the risk estimate of NOF after adjusting for age, comorbidities, and concurrent medication for ACE inhibitors users (HR, 1.64; 95% CI, 1.01–2.64) was significantly higher (P < 0.05) than that for nonusers. Patients who took CCBs (HR, 0.70; 95% CI, 0.49–0.99) were at a lower risk of developing NOF than nonusers. Loop diuretics (HR, 1.05; 95% CI, 0.61–1.80; and adjusted HR, 1.11; 95% CI, 0.64–1.93), thiazide diuretics (HR, 0.94; 95% CI, 0.63–1.38; and adjusted HR, 0.97; 95% CI, 0.65–1.44), beta-blockers (HR, 0.70; 95% CI, 0.49–1.01; and adjusted HR, 0.77; 95% CI, 0.52–1.12), and ARBs (HR, 0.89; 95% CI, 0.63–1.26; and adjusted HR, 0.89; 95% CI, 0.63–1.27) were not associated with the risk of NOF development from crude HR to adjusted HR [P > 0.05, Table 2].
Table 2.
Incidence of HRs with 95% CI for new-onset osteoporotic fracture according to prescriptions for antihypertensive drugs compared with nonusers
| Drugs | HR (95% CI) | P | Adjusted HR* (95% CI) | P |
|---|---|---|---|---|
| Loop diuretics | 1.05 (0.61–1.80) | 0.864 | 1.11 (0.64–1.93) | 0.822 |
| Thiazide diuretics | 0.94 (0.63–1.38) | 0.737 | 0.97 (0.65–1.44) | 0.723 |
| Beta-blockers | 0.70 (0.49–1.01) | 0.059 | 0.77 (0.52–1.12) | 0.064 |
| CCBs | 0.77 (0.54–1.10) | 0.147 | 0.70 (0.49–0.99) | 0.048 |
| Alpha-blockers | 0.37 (0.14–1.00) | 0.043 | 0.42 (0.15–1.18) | 0.065 |
| ACE inhibitors | 1.58 (0.98–2.55) | 0.051 | 1.64 (1.01–2.66) | 0.043 |
| ARBs | 0.89 (0.63–1.26) | 0.506 | 0.89 (0.63–1.27) | 0.508 |
*HR was adjusted for age, sex, comorbidities, and concurrent medication. CCBs: Calcium channel blockers; ACE: Angiotensin-converting enzyme; ARBs: Angiotensin receptor blockers; HRs: Hazard ratios; CI: Confidence intervals.
Discussion
In this study, the use of ACE inhibitors was independently associated with an increased risk of NOF development in elderly hypertensive patients. The use of CCBs was also independently associated with a decreased risk of NOF in elderly hypertensive patients. Loop diuretics, thiazide diuretics, beta-blockers, ARBs, and alpha-blockers were not associated with the risk of NOF development in elderly hypertensive patients.
Loop diuretics have been shown to accelerate NOF in hypertensive patients who use them continuously for more than three years.[13] Our results contradicted this study but were comparable with the results reported by Solomon et al.,[14] who studied the risk of NOF in 376,061 elderly hypertensive patients using loop diuretics or CCBs. Solomon et al. observed no difference in the relative risk of hip fractures (HR, 1.03; 95% CI, 0.90–1.16), wrist fractures (HR, 0.98; 95% CI, 0.83–1.16), or femur fractures (HR, 0.98; 95% CI, 0.83–1.16) in individuals using a loop diuretic compared with those using CCB.
An observational study showed that patients using thiazide diuretics for more than one year had a decreased risk of developing hip fractures compared with those who did not use these drugs (HR, 0.46; 95% CI, 0.21–0.96);[15] the authors concluded that the long-term use of thiazide diuretic decreased the incidence of NOF. However, our study, which included an 11-year follow-up period, revealed no association between NOF and the use of thiazide diuretics. In addition, many observational studies have demonstrated findings similar to those of our study.[16,17] For example, LaCroix et al.[17] evaluated 9518 hypertensive patients and reported that the relative risk of NOF for patients using thiazide diuretics was 0.88 (95% CI, 0.52–1.74) in East Boston, 0.53 (95% CI, 0.27–1.05) in New Haven, and 0.67 (95% CI, 0.39–1.14) in Iowa.
In vitro data show that the sympathetic nervous system has a catabolic effect on bones.[18,19] Therefore, beta-blockers are generally considered to decrease the risk of NOF.[20,21,22] Many studies have indicated that beta-blockers are associated with a decreased risk of NOF compared with thiazide diuretics.[20,21] For example, Schlienger et al.[21] evaluated 30,601 patients and reported that the relative risk of NOF in patients who used beta-blockers was 0.77 (95% CI, 0.72–0.83) compared with those not using beta-blockers or using a thiazide diuretic. However, our results showed a neutral effect on the risk of developing NOF, similar to the two studies by Rein et al.[23] and Levasseur et al.[24] In the study by Rein et al.,[23] the adjusted relative risk of NOF in individuals using a beta-blocker was 0.92 (95% CI, 0.81–1.05) compared with those not using beta-blocker in a cohort of elderly women. Similarly, Levasseur et al.[24] reported that beta-blockers were not associated with an increased risk of NOF in female hypertensive patients.
In the present study, we found that the use of ACE inhibitors increased the risk of NOF development at a similar level as that found in a previous study, in which 301,591 elderly hypertensive patients were evaluated. The relative risk of developing NOF when using ACE inhibitors was found to be 1.53 (95% CI, 1.12–2.10) in that study.[25] However, many studies have reported that ACE inhibitors decrease the risk of NOF development in hypertensive patients because they block the renin–angiotensin system, thus shifting the balance toward bone formation.[9,26] In the study by Rejnmark et al.,[26] in which 124,655 patients were evaluated, the use of ACE inhibitors was found to decrease the risk of NOF development compared with the use of CCBs (odds ratio, 0.93; 95 % CI, 0.90–0.96).
In this study, ARBs were not associated with a decrease in the risk of NOF development. This result is consistent with the results observed in the report by Butt et al.,[25] which showed a nonstatistically significant increase in NOF of the hip (incidence rate ratio, 1.41; 95% CI, 0.65–3.05). However, some studies found that ARB use was associated with a statistically significant decrease in the risk of NOF development.[14] For example, Solomon et al.[14] evaluated 376,061 hypertensive patients and found that the risk of NOF development decreased in those who used ARBs (HR, 0.76; 95% CI, 0.68–0.86).
This study shows that the use of ACE inhibitors was independently associated with an increased risk of NOF development. On the other hand, the use of ARB was not independently associated with an increased risk of NOF development in elderly hypertensive patients. The mechanism driving this difference is currently not known. However, in a rat ovariectomy model, they found that hypertensive rats treated with ARB experienced less decrease in bone marrow density because of ARB, which can increase the activity of tartrate-resistant acid and bone resorption.[14]
Our results show that the use of CCBs is associated with a statistically significant decrease in the risk of NOF. Previous studies have consistently demonstrated that CCB class of antihypertensive drugs has protective effects on bone metabolism in experimental and human studies.[26,27,28,29] A study, which is similar to our study, reported that the use of CCBs was associated with a 6% (95% CI, 4–9%) decrease in the risk of NOF.[26] In contrast, there has also been a study that reported no protective effect on NOF risk for the users of CCBs.[29]
This study is the long-term longitudinal epidemiological investigation of the association between the use of alpha-blockers and developing osteoporotic fractures, with a follow-up period of 11 years.[10] We found that alpha-blockers were not associated with NOF in elderly hypertensive patients. This study also suggest that alpha-blockers have a neutral effect against NOF. There have been many studies reporting a negative protection relationship of alpha-blockers with NOF.[10,12,30] The statistically significant increase in the risk of NOF among the groups of alpha-blocker users observed in previous studies may be explained by the current use and short-term follow-up.[10]
Some limitations of this study need to be emphasized. First, this was a descriptive retrospective study conducted in Taiwan, China over a period of 11 years. Moreover, we excluded irregularly treated hypertensive patients from the analyses. Therefore, caution must be exercised in interpreting our data. Second, all cases in this study were collected from claimed datasets of the Taiwan NHI that were submitted from the China Medical University Hospital, and the diagnoses were based on physician reports only; therefore, it is unclear how our findings can be generalized to patients in different areas of the world. Third, the process of osteoporosis in patients who developed NOF in this study would have started many years before the diagnoses, and NOF may have coexisted with the process of hypertension for which antihypertensive drugs were used. Thus, the cause and effect relationships between NOF and the antihypertensive drugs cannot be determined in this study. Fourth, the data on genetic evaluation for hypertension, such as CaMK4, PLA2, and GRKs,[5] were not available from the secondary data used for this study. Fifth, the risk factors for osteoporotic fractures, such as obesity, body mass index, smoking status, alcohol consumption, physical activity, family history, and treatment adherence, were also not available from these datasets of Taiwan NHI.
In conclusion, our results show that elderly hypertensive patients who use ACE inhibitors are at a higher risk of developing NOF than patients who are nonusers. The use of CCBs was also independently associated with a decreased risk of NOF in elderly hypertensive patients. Our findings may provide some support for the hypothesis that there are differences in the risk of developing NOF with the use of different classes of antihypertensive drugs in elderly hypertensive patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Min Chen
References
- 1.Liou YS, Ma T, Tien L, Chien C, Chou P, Jong GP. Long-term effects of antihypertensive drugs on the risk of new-onset diabetes in elderly Taiwanese hypertensives. Int Heart J. 2008;49:205–11. doi: 10.1536/ihj.49.205. doi: 10.1536/ihj.49.205. [DOI] [PubMed] [Google Scholar]
- 2.Ulu MA, Batmaz I, Dilek B, Çevik R. Prevalence of osteoporosis and vertebral fractures and related factors in patients with ankylosing spondylitis. Chin Med J. 2014;127:2740–7. doi: cma.j.issn.0366-6999.20140367. [PubMed] [Google Scholar]
- 3.Lee YK, Nho JH, Ha YC, Koo KH. Persistence with intravenous zoledronate in elderly patients with osteoporosis. Osteoporos Int. 2012;23:2329–33. doi: 10.1007/s00198-011-1881-x. doi: 10.1007/s00198-011-1881-x. [DOI] [PubMed] [Google Scholar]
- 4.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 5.Nordin C. Essential roles of intracellular calcium release channels in muscle, brain, metabolism, and aging. Curr Mol Pharmacol. 2015;8:206–22. doi: 10.2174/1874467208666150507105105. doi: 10.2174/1874467208666150507105105. [DOI] [PubMed] [Google Scholar]
- 6.Hsiao PC, Chen TJ, Li CY, Chu CM, Su TP, Wang SH, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: A population-based cohort study. Medicine (Baltimore) 2015;94:532. doi: 10.1097/MD.0000000000000532. doi: 10.1097/MD.0000000000000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LaCroix AZ, Ott SM, Ichikawa L, Scholes D, Barlow WE. Low-dose hydrochlorothiazide and preservation of bone mineral density in older adults. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2000;133:516–26. doi: 10.7326/0003-4819-133-7-200010030-00010. doi: 10.7326/0003-4819-133-7-200010030. [DOI] [PubMed] [Google Scholar]
- 8.Lepsen EW, Lundgren JR, Hartmann B, Pedersen O, Hansen T, Jørgensen NR, et al. GLP-1 receptor agonist treatment increases bone formation and prevents bone loss in weight-reduced obese women. J Clin Endocrinol Metab. 2015;91:2909–17. doi: 10.1210/jc.2015-1176. doi: 10.1210/jc.2015-1176. [DOI] [PubMed] [Google Scholar]
- 9.Pérez-Castrillón JL, Silva J, Justo I, Sanz A, Martín-Luquero M, Igea R, et al. Effect of quinapril, quinapril-hydrochlorothiazide, and enalapril on the bone mass of hypertensive subjects: Relationship with angiotensin converting enzyme polymorphisms. Am J Hypertens. 2003;16:453–9. doi: 10.1016/s0895-7061(03)00845-8. doi: 10.1016/S0895-7061(03)00845-8. [DOI] [PubMed] [Google Scholar]
- 10.Wiens M, Etminan M, Gill SS, Takkouche B. Effects of antihypertensive drug treatments on fracture outcomes: A meta-analysis of observational studies. J Intern Med. 2006;260:350–62. doi: 10.1111/j.1365-2796.2006.01695.x. doi: 10.1111/j.1365-2796.2006.01695.x. [DOI] [PubMed] [Google Scholar]
- 11.Kwan E, Straus SE. Assessment and management of falls in older people. CMAJ. 2014;186:E610–21. doi: 10.1503/cmaj.131330. doi: 10.1503/cmaj.131330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schulze-Späte U, Turner R, Wang Y, Chao R, Schulze PC, Phipps K, et al. Relationship of bone metabolism biomarkers and periodontal disease: The Osteoporotic Fractures in Men (MrOS) Study. J Clin Endocrinol Metab. 2015;91:2425–33. doi: 10.1210/jc.2014-4180. doi: 10.1210/jc.2014-4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carbone LD, Johnson KC, Bush AJ, Robbins J, Larson JC, Thomas A, et al. Loop diuretic use and fracture in postmenopausal women: Findings from the Women's Health Initiative. Arch Intern Med. 2009;169:132–40. doi: 10.1001/archinternmed.2008.526. doi: 10.1001/archinternmed.2008.526. [DOI] [PubMed] [Google Scholar]
- 14.Solomon DH, Mogun H, Garneau K, Fischer MA. Risk of fractures in older adults using antihypertensive medications. J Bone Miner Res. 2011;26:1561–7. doi: 10.1002/jbmr.356. doi: 10.1002/jbmr.356. [DOI] [PubMed] [Google Scholar]
- 15.Felson DT, Sloutskis D, Anderson JJ, Anthony JM, Kiel DP. Thiazide diuretics and the risk of hip fracture. Results from the Framingham Study. JAMA. 1991;265:370–3. doi: 10.1001/jama.1991.03460030076032. [PubMed] [Google Scholar]
- 16.Riggs BL, Melton LJ., 3rd The prevention and treatment of osteoporosis. N Engl J Med. 1992;327:620–7. doi: 10.1056/NEJM199208273270908. doi: 10.1056/NEJM199208273270908. [DOI] [PubMed] [Google Scholar]
- 17.LaCroix AZ, Wienpahl J, White LR, Wallace RB, Scherr PA, George LK, et al. Thiazide diuretic agents and the incidence of hip fracture. N Engl J Med. 1990;322:286–90. doi: 10.1056/NEJM199002013220502. doi: 10.1056/NEJM199002013220502. [DOI] [PubMed] [Google Scholar]
- 18.Katsumura S, Ezura Y, Izu Y, Shirakawa J, Miyawaki A, Harada K, et al. Beta adrenergic receptor stimulation suppresses cell migration in association with cell cycle transition in osteoblasts-live imaging analyses based on FUCCI system. J Cell Physiol. 2016;231:496–504. doi: 10.1002/jcp.25096. doi: 10.1002/jcp.25096. [DOI] [PubMed] [Google Scholar]
- 19.Takeda S, Elefteriou F, Levasseur R, Liu X, Zhao L, Parker KL, et al. Leptin regulates bone formation via the sympathetic nervous system. Cell. 2002;111:305–17. doi: 10.1016/s0092-8674(02)01049-8. doi: 10.1016/S0092-8674(02)01049-8. [DOI] [PubMed] [Google Scholar]
- 20.Chiu MH, Lee HD, Hwang HF, Wang SC, Lin MR. Medication use and fall-risk assessment for falls in an acute care hospital. Geriatr Gerontol Int. 2015;15:856–63. doi: 10.1111/ggi.12359. doi: 10.1111/ggi.12359. [DOI] [PubMed] [Google Scholar]
- 21.Schlienger RG, Kraenzlin ME, Jick SS, Meier CR. Use of beta-blockers and risk of fractures. JAMA. 2004;292:1326–32. doi: 10.1001/jama.292.11.1326. doi: 10.1007/s00223-006-0213-1. [DOI] [PubMed] [Google Scholar]
- 22.Meisinger C, Heier M, Lang O, Döring A. Beta-blocker use and risk of fractures in men and women from the general population: The MONICA/KORA Augsburg Cohort Study. Osteoporos Int. 2007;18:1189–95. doi: 10.1007/s00198-007-0354-8. doi: 10.1007/s00198-007-0354-8. [DOI] [PubMed] [Google Scholar]
- 23.Reid IR, Gamble GD, Grey AB, Black DM, Ensrud KE, Browner WS, et al. beta-Blocker use, BMD, and fractures in the study of osteoporotic fractures. J Bone Miner Res. 2005;20:613–8. doi: 10.1359/JBMR.041202. doi: 10.1359/JBMR.041202. [DOI] [PubMed] [Google Scholar]
- 24.Levasseur R, Dargent-Molina P, Sabatier JP, Marcelli C, Bréart G. Beta-blocker use, bone mineral density, and fracture risk in older women: Results from the Epidemiologie de l’Osteoporose Prospective Study. J Am Geriatr Soc. 2005;53:550–2. doi: 10.1111/j.1532-5415.2005.53178_7.x. doi: 10.1111/j.1532-5415.2005.53178_7.x. [DOI] [PubMed] [Google Scholar]
- 25.Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172:1739–44. doi: 10.1001/2013.jamainternmed.469. doi: 10.1001/2013.jamainternmed.469. [DOI] [PubMed] [Google Scholar]
- 26.Rejnmark L, Vestergaard P, Mosekilde L. Treatment with beta-blockers, ACE inhibitors, and calcium-channel blockers is associated with a reduced fracture risk: A nationwide case-control study. J Hypertens. 2006;24:581–9. doi: 10.1097/01.hjh.0000203845.26690.cb. doi: 10.1097/01.hjh.0000203845.26690.cb. [DOI] [PubMed] [Google Scholar]
- 27.Ma ZP, Liao JC, Zhao C, Cai DZ. Effects of the 1, 4-dihydropyridine L-type calcium channel blocker benidipine on bone marrow stromal cells. Cell Tissue Res. 2015;361:467–76. doi: 10.1007/s00441-015-2115-x. doi: 10.1007/s00441-015-2115-x. [DOI] [PubMed] [Google Scholar]
- 28.Reid IR. Efficacy, effectiveness and side effects of medications used to prevent fractures. J Intern Med. 2015;277:690–706. doi: 10.1111/joim.12339. doi: 10.1111/joim.12339. [DOI] [PubMed] [Google Scholar]
- 29.Takaoka S, Yamaguchi T, Tanaka K, Morita M, Yamamoto M, Yamauchi M, et al. Fracture risk is increased by the complication of hypertension and treatment with calcium channel blockers in postmenopausal women with type 2 diabetes. J Bone Miner Metab. 2013;31:102–7. doi: 10.1007/s00774-012-0389-6. doi: 10.1007/s00774-012-0389-6. [DOI] [PubMed] [Google Scholar]
- 30.Choi HJ, Park C, Lee YK, Ha YC, Jang S, Shin CS. Risk of fractures in subjects with antihypertensive medications: A nationwide claim study. Int J Cardiol. 2015;184:62–7. doi: 10.1016/j.ijcard.2015.01.072. doi: 10.1016/j.ijcard.2015.01.072. [DOI] [PubMed] [Google Scholar]


