Highlights
-
•
Complicated Meckel’s diverticulum can have different clinical presentations and can cause bowel obstruction especially if a phytobezoar gets impacted in it.
-
•
Surgical management is needed and laparoscopic approach could be an option with a better outcome for treatment of this condition.
Keywords: Meckel’s, Phytobezoar, Obstruction, Laparoscopy
Abstract
Introduction
Meckel’s diverticulum is the most common anomaly of the gastrointestinal tract, occurring in 1–3% of the general population. The most common complication of Meckel’s diverticulum is intestinal obstruction. In this report, we describe a rare cause of intestinal obstruction due to Meckel’s; the phytobezoar. After thorough literature review, the authors found about ten individual reports of the same topic. In all these cases, diagnosis was established intra-operatively.
Case presentation
A forty-seven-year old male presented to the emergency department with a one-day history of abdominal pain associated with vomiting and constipation. Physical examination diagnostic tests revealed features of intestinal obstruction.
Discussion
The lifetime risk of complications in patients with a Meckel’sdiverticulum is usually small and occurs only in up to 4%. In adults’ intestinal obstruction is the most common complication (40%).
Conclusion
Complicated Meckel’s diverticulum can have different clinical presentations and can cause bowel obstruction. An association with bezoars impaction is possible and it should be suspected in adult patients presenting with bowel obstruction of unknown causes especially those with high vegetarian diet.
1. Introduction
Meckel’s diverticulum is an embryological residue resulting from an incomplete obliteration of vitelline duct during fifth week of gestation [1]. The most common complication of Meckel’s diverticulum in adults is intestinal obstruction [2]. It can result from several mechanisms commonly described in medical books such as; volvulus of the intestine around the fibrous band attaching the diverticulum to the umbilicus, intussusception with a diverticulum acting as lead point, entrapment of the intestine by a mesodiverticular band and strictures secondary to chronic diverticulitis [3]. Phytobezoar is a vegetable ball defined as a concentration of poorly digested vegetables and fruit fibers that is found in alimentary tract in particular in the stomach commonly causing symptoms varying from dyspepsia to epigastric mass. A phytobezoar accounts for 4% of the causes of small bowel obstruction occurrence of small bowel obstruction due to phytobezoar within Meckel’s diverticulum is exceedingly rare, seldom reported in literature and deserves to be described.
2. Case presentation
A forty-seven-year old male presented to the emergency department with a one-day history of colicky abdominal pain associated with vomiting and constipation. Pain started gradually in the upper abdomen then became generalized. He had two episodes of vomiting of large amount of food particles mixed with greenish fluid but no hematemesis. No history of fever, loss of weight or previous similar complaint. The patient had no significant past surgical or medical history. Details of the diet history revealed that the patient is not vegetarian but he tends to have excessive amounts of fruits and vegetables.
On examination: the patient was conscious and oriented. Vital signs showed a pulse rate of 69 beat per minute, blood pressure 134/93 mmHg and temperature of 36.4 °C. Bowl sounds were exaggerated and the abdomen was mildly distended, lax with mild epigastric tenderness. No organomegaly or masses were palpated; no surgical scars or hernias were present. Upon rectal examination, the rectum was empty and no masses felt.
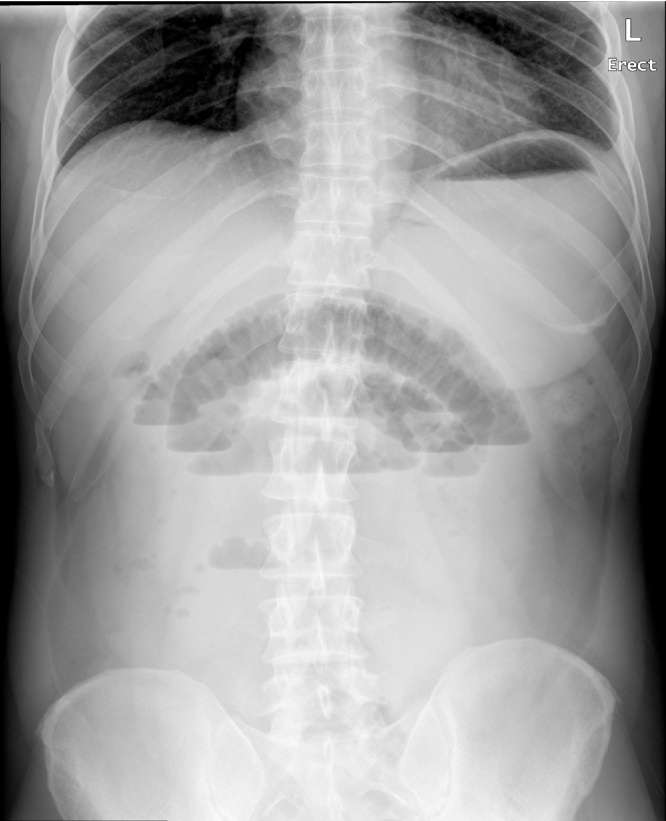
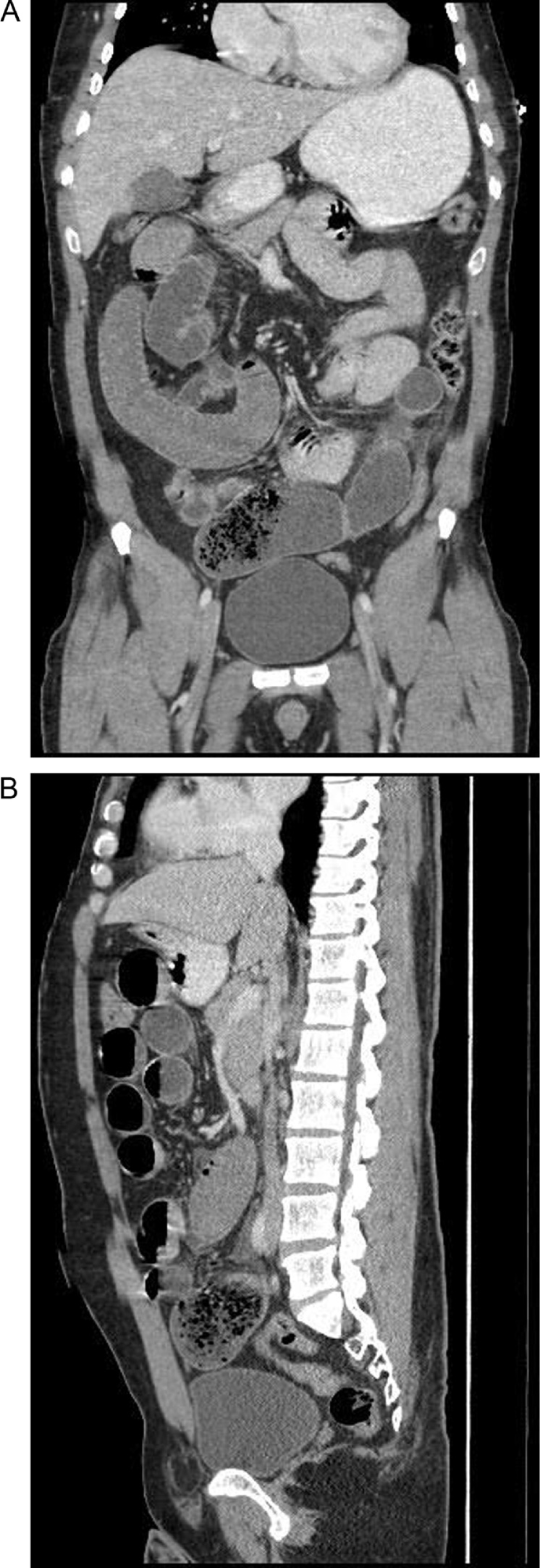
Laboratory tests showed a White Cell Count (WBC) of 15300cells per microliter (mcL). Other lab tests were unremarkable. An abdominal X-ray showed dilatation of small bowl loops with multiple air fluids levels (Fig. 1).Computed Tomography (CT) scan with intravenous (IV) and oral contrast was done and showed features of small bowel obstruction at the level of the terminal ileum with outpouching of an ileal segment in the form of diverticulum (Fig. 2A,B).
Fig. 1.
Abdominal X-ray showing multiple air fluid levels.
Fig. 2.
CT scan showing distal small bowel obstruction.
The patient was resuscitated with IV fluids, antibiotics and pain killers then shiftedto the operating theatrewhere a diagnostic laparoscopy was done and showed aMeckel’s diverticulum forming a mass causing bowel obstruction with proximal dilated small bowl loops. Resection of the involved segment with entero-enteric anastomosiswas done. The resected specimen (Fig. 3) was opened and the diverticulum was forming a mass containing phytobezoar (Fig. 4).
Fig. 3.
Resected bowel segment with Meckel’s.
Fig. 4.
Meckel’s opened showing the Phytobezoar.
Histopathologic examination of the specimen showed mucosal sloughing, submucosal congested blood vessels and acute inflammatory exudate in a Meckel’s diverticulum.
Post- operative, the patient was doing well, but later he developed signs of leak, and exploration revealed a leak from the anastomosis, so resection of the involved segment was done and new anastomosis was reconstructed. Later, the patient did well, tolerated diet and was discharged in a stable condition.
3. Discussion
The lifetime risk of complications in patients with a Meckel’sdiverticulum is usually small and occurs only in up to 4% [4]. Complications differ according to theage of the patient. In adult patients, intestinal obstruction is the most common complication (40%) and, in children, gastrointestinal hemorrhage is the most common[2].
Bowel obstructions from Meckel’s diverticulum most commonly occur due to intussusception, volvulus around an associated band, inflammatory adhesion, or incarceration of the diverticulum within a hernia (Littre’s Hernia) [5].
The term Bezoar came from the Arabic “badzehr”or from the Persian “panzer,” both means counter poison or antidote [6]. Excessive intake of fruits and vegetable fibers, as a feeding habit, can predispose to phytobezoar formation. This is presumably due to collection of fibrous and indigestible food, rich of slags of alimentary material, in an altered or slow flow area or into a stenotic narrowed area. The presence of intestinal dysmotility and poor coordination of the peristaltic waves at the site of the Meckel’s diverticulum could produce decreased ileal motility and slow intraluminal flow with impaction and stickiness of boluses of food[7], [8].
The clinical assessment on its own might not be enough to get a correct diagnosis. About 50–70% of small bowel obstructions are diagnosed by abdominal radiography showing dilated bowel loops, air-fluid levels and thickened bowel wall [9]. CT scan, demonstrating dilated small bowel loop and well-defined round, heterogeneous intraluminal mass in distal segment, is diagnostic. The mass could be outlined by the bowel wall and present characteristic internal gas bubbles. CT scan is useful to localize the bezoar as well as to identify complications like perforation and obstruction [10].
Phytobezoar impaction in a Meckel’s diverticulum is very rare with few reported cases in the English literature [11]. Most of the cases reported in the literature were treated through open laparotomy. One case [11] published in 2011 mentioned the laparoscopic treatment in such cases and another retrospective study [12] has indicated that laparoscopy may be superior to laparotomy for surgical treatment of small bowel obstruction (SBO) caused by bezoar.
In the present case, clinical assessment was consistent with bowel obstruction and the CT findings were not conclusive to identify the cause; this necessitated surgical intervention to delineate the cause and treat the underlying pathology. A laparoscopic approach was successful in management with decreased postoperative complications, less hospital stay and early recovery. In the presence of an experienced laparoscopic surgeon; a minimally invasive approach can be used in selected patients with unclear causes of small bowel obstruction.
4. Conclusion
Meckel’s diverticulum is a potential causeof intestinal obstruction mainly in adults. An association with any type of bezoars impaction is possible and phytobezoarsshould be suspected in adult patients presenting with bowel obstruction of unknown causes especially those with high vegetarian diet. Laparoscopic approach could be a good option with better outcome for treatment of this condition.
Conflict of interest
No conflict of interest is present.
Funding
No involvement of any funding to be mentioned.
Ethical Approval
Approval was given by consenting the patient.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Bassem Abou Hussein: author.
Ali Khammas: co-author.
Labib Al-Ozaibi: co-author.
Alyaa Abdallah: co-author.
Hajer Busharar: discussion the case.
Ahmad Bdeir: contributor.
Alya Al-Mazroui: contributor.
Faisal Al-badri: contributor.
Guarantor
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non-exclusive for government employees) on a worldwide basis to permit this article (if accepted) to be published in the International Journal of Surgery Case Reports.
Footnotes
The Corresponding author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non-exclusive for government employees) on a worldwide basis to permit this article (if accepted) to be published in the International Journal of Surgery Case Reports.
References
- 1.Sodelund S. Meckel’s diverticulum: a clinical and histopathologic study. ActaChirScand. 1959:13–233. (sup; 248) [Google Scholar]
- 2.Park J.J., Wolff B.G., Tollefson M.K., Walsh E.E., Larson D.R. Meckel diverticulum: the mayo clinic experience with 1476 patients (1950–2002) Ann. Surg. 2005;241:529–533. doi: 10.1097/01.sla.0000154270.14308.5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cifuentes J., Robles R., Parrilla P. Gastric surgery and bezoars. Dig. Dis. Sci. 1992;37:1964–1966. doi: 10.1007/BF01299861. (pubmed) [DOI] [PubMed] [Google Scholar]
- 4.Haber J.J. Meckel’s diverticulum: review of literature and analytical study of 23 cases with particular emphasis on bowel obstruction. Am. J. Surg. 1947;73:468–485. doi: 10.1016/0002-9610(47)90329-2. [DOI] [PubMed] [Google Scholar]
- 5.Yahchouchy E.K., Marano A.F., Etienne J.C., Fingerhut A.L. Meckel’s diverticulum. J. Am. Coll. Surg. 2001 May;192(5):658–662. doi: 10.1016/s1072-7515(01)00817-1. [DOI] [PubMed] [Google Scholar]
- 6.Sharma R.D., Kotwal S., Chintamani Bhatnagar D. Trichobezoar obstructing the terminal ileum. Trop. Doct. 2002;32:99–100. doi: 10.1177/004947550203200217. [DOI] [PubMed] [Google Scholar]
- 7.Frazzini V.I., Jr, English W.J., Bashist B., et al Case report. Small bowel obstruction due to phytobezoar formation within Meckel diverticulum: CT findings. J. Comput. Assist. Tomogr. 1996;20(May–June(2)):390–392. doi: 10.1097/00004728-199605000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Sorensen J.B., Ghani A. Phytobezoar obstruction of a Meckel’s diverticulum. Am. Surg. 1992;58:61–64. [PubMed] [Google Scholar]
- 9.Ripolles T., Gardia J.A., Martinez M.J., Gil P. Gastrointestinal bezoars, sonographic and CT characteristics. AJR. 2001;177:65–69. doi: 10.2214/ajr.177.1.1770065. (PubMed) [DOI] [PubMed] [Google Scholar]
- 10.Bini Roberto, Quiriconi Fabrizio, Tello Aurelio, Fusca Marcella, Loddo Franca, Leli Renzo, Addeo Alfredo. Phytobezoar in Meckel’s diverticulum: a rare cause of small bowel obstruction. Int. J. Surg. Case Rep. 2012;3(5):161–163. doi: 10.1016/j.ijscr.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fagenholz Peter J., Marc M.D., de Moya M.D. Laparoscopic treatment of bowel obstruction due to a bezoar in a meckel’s diverticulum. JSLS. 2011;15:562–564. doi: 10.4293/108680811X13176785204607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yau K.K., Siu W.T., Law B.K., Cheung H.Y., Ha J.P., Li M.K. Laparoscopic approach compared with conventional open approach for bezoar-induced small-bowel obstruction. Arch. Surg. 2005;140(October(10)):972–975. doi: 10.1001/archsurg.140.10.972. [DOI] [PubMed] [Google Scholar]