INTRODUCTION
A commonly-encountered clinical scenario in primary care involves an adolescent or young adult, with no past medical history, presenting with wheeze and breathlessness, occurring in association with exercise.1
However, the differential diagnosis for this presentation is broad. Such patients are often diagnosed with exercise-induced asthma and prescribed a short-acting bronchodilator.1 Recently there has been increasing recognition that an alternative diagnosis should be considered,2 specifically a condition termed exercise-induced laryngeal obstruction (EILO), a phenomenon in which closure of the larynx occurs during high-intensity exercise. This narrowing causes a significant reduction in airflow, thereby precipitating breathlessness and wheeze.
Some have termed this condition exercise-induced vocal cord dysfunction (VCD), although the narrowing most frequently occurs at a level above the vocal cords (that is, involves supra-glottic structures) and thus EILO is an appropriate descriptor.
The reason EILO develops in some individuals is currently unclear. A primary function of the glottis is to defend the airway, and thus the larynx resides in a primed status that favours closure. The larynx is richly innervated and may become hypersensitive upon repeated exposure to laryngeal irritants. Moreover, the forces and pressure change that are manifest across the larynx during intense exercise appear to play a role in precipitating laryngeal closure.
Distinguishing between exercise-induced bronchoconstriction and EILO can be diagnostically challenging, particularly in a primary care setting. The aim of this short article is thus not to provide a complete review of EILO, but to highlight pertinent features for focus in a clinic-based assessment, and to indicate those requiring specialist referral.
PREVALENCE
The diagnosis of EILO is most often made in adolescents. A recent cross-sectional study of 12–13-year-olds in Sweden demonstrated a population prevalence of approximately 6%.3 Another study has shown that EILO may be as prevalent as exercise-induced bronchoconstriction, explaining ‘treatment-refractory’ symptoms in around a quarter of young athletic patients referred with exertional respiratory symptoms.4 Nielsen et al found EILO coexisting with exercise-induced bronchoconstriction in just over 10% of individuals, perhaps explaining why ‘partial’ resolution of symptoms is seen in some young patients treated with inhaler therapy.4
PRESENTATION
EILO typically presents as a young athletic female, <20 years, reporting shortness of breath, increased respiratory effort, throat discomfort, and/or chest tightness and a wheeze that develops during intense exercise, often during competitive events.
The differential diagnosis for exertional dyspnoea is broad and requires an initial exclusion of ‘red flag’ respiratory and cardiac symptoms and signs, for example, chest pain, palpitations, haemoptysis, and the presence of cardiac signs such as a cardiac murmur.
Classically the ‘wheeze’ of EILO occurs during the inspiratory phase of the breathing cycle and is high pitched in quality, that is, stridulous. This differentiates it from the expiratory polyphonic basal wheeze heard with lower-airway narrowing.
Symptom onset in EILO usually occurs during strenuous exercise and settles rapidly (within 5 minutes of exercise cessation). This contrasts with exercise-induced bronchoconstriction, in which symptoms occur following exercise cessation (5–10 minutes). Patients with EILO not infrequently report cough or throat discomfort that can persist for some time following exercise.
DIAGNOSTIC CRITERION AND ASSESSMENT
Several clinical features can be useful in differentiating EILO from exercise-induced bronchoconstriction (Table 1). It should be noted, however, that questions thought to be of discriminatory value (for example, difficulty ‘breathing in’ when exercising) have actually been shown to have poor diagnostic value when studied formally. Likewise, there is no evidence to suggest that a diagnosis of EILO can be reliably confirmed or refuted by resting or post-exercise spirometry, or by peak flow measurement.5 Moreover, because EILO occurs during strenuous exercise, investigations performed in a ‘resting’ state are unlikely to be diagnostically helpful.
Table 1.
Features distinguishing EILO (exercise-induced laryngeal obstruction) and exercise-induced bronchoconstriction
| EILO | Exercise-induced bronchoconstriction | |
|---|---|---|
| Onset | Rapid (within seconds), during peak exercise | Rapid (within minutes), shortly following the termination of exercise |
| Duration | Regresses within few minutes of rest | Resolves typically within 30 minutes |
| Inhaled drug therapy | Largely ineffective, inhaled anticholinergic may reduce symptoms | Beta-2 agonist usually effective |
| Breathing characteristics | Monophonic inspiratory wheeze, prolonged inspiratory phase | Monophonic expiratory wheeze, prolonged expiratory phase |
| Regional limitation | Upper airways, neck | Lower airways, chest |
| Symptoms | Dyspnoea, wheeze, stridor, cough, throat/chest tightness, dysphonia | Dyspnoea, wheeze, cough, chest tightness |
| Precipitating factors/similar symptoms | Exercise, emotional stress, cold air, strong odours | Exercise, infections, cold air, allergies, stress |
It is thus often useful for a clinician to observe a patient as they develop symptoms, for example, when performing the sport that triggers symptoms. If this is not feasible, then the authors have previously found ‘selfie’ mobile-phone-type video recordings of patients when they develop symptoms to be informative. This subsequently allows the clinician to review the characteristics and onset of symptoms, and better discern the nature of the wheeze. The diagnostic accuracy of this approach is yet to be studied formally, although it may prove helpful.
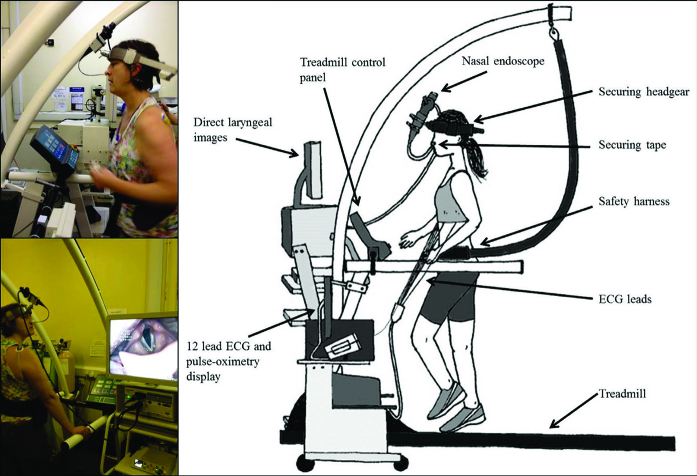
The ‘gold-standard’ means for diagnosis involves real-time evaluation of laryngeal movement during exercise. This test, termed the continuous laryngoscopy exercise (CLE) test, utilises a flexible laryngoscope in a fixed position on specialist headgear (Figure 1), allowing continuous video assessment of laryngeal movement while a patient performs exercise.
Figure 1.
The continuous laryngoscopy exercise (CLE) test.
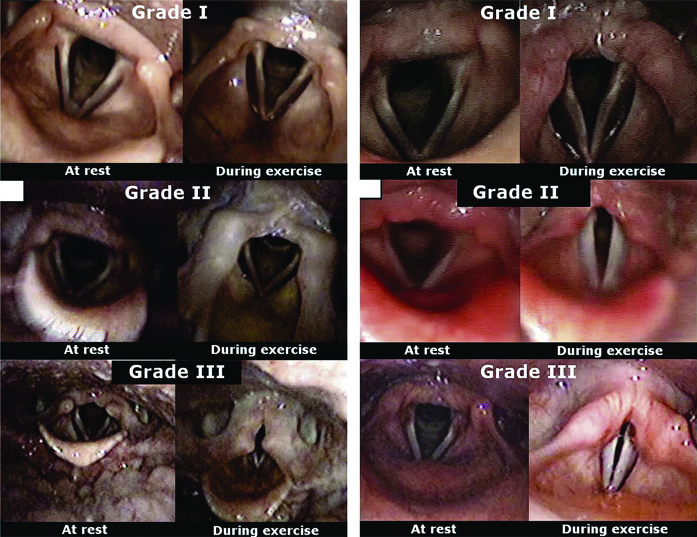
During exercise there is normally complete abduction of the laryngeal structures to maintain laryngeal patency and optimise flow. Thus, EILO is diagnosed on the basis of the development of abnormal degree of adduction of the supra-glottic structures (akin to laryngomalacia) and/or inappropriate closure of the glottis (that is, vocal cords) during the test (Figure 2). This closure generates turbulent flow and increased resistance, which in turn promotes laryngeal closure, resulting in dyspnoea and inspiratory stridor. The CLE test allows patients to visualise where their symptoms are arising from and can also inform treatment. We suggest that individuals be referred for specialist review and a CLE test if there is diagnostic uncertainty +/− a poor response to therapies, and clearly if surgical intervention is being considered.
Figure 2.
Glottic and supra-glottic exercise-induced laryngeal obstruction (EILO). NB Static images taken from CLE with exercise narrowing occurring during inspiratory phase of breathing cycle. Severity of closure is scored by grade of closure (that is, with Grade I as minor closure and grade III as severe); closure above grade II is taken as significant. Adapted from Nielsen et al.4 © Wolters Kluwer. Used with permission.
MANAGEMENT
The first step in managing EILO is to discuss the nature of the problem with the patient affected and for the clinician to consider and highlight the fact that, providing there is not a diagnosis of coexisting exercise-induced bronchoconstriction, medication use can be rationalised. Literature is replete with reports of patients who have been unnecessarily treated with asthma therapies for several years prior to their diagnosis of EILO.4
Time should be spent addressing and minimising the effect of any laryngeal irritants (for example, nasal disease and reflux) and a discussion regarding strategies to improve laryngeal hygiene (for example, avoiding smoking, regular fluid intake, and avoiding dietary caffeine).
Physiotherapy and speech and language therapy currently form the basis of treatment, utilising breathing control techniques to improve laryngeal abduction during exercise. Basic strategies include providing focus on nasal breathing to increase humidification of air, inspiratory muscle training, and overall promotion of a diaphragmatic-predominant breathing pattern.
Emotional stressors may contribute to the development of symptoms in some individuals and certainly in the context of competitive environments. Supportive interventions including counselling and/or relaxation therapy should be considered.
Individuals with severe EILO that remains refractory to the interventions described above can be treated surgically.6 Laser aryepiglottoplasty involves surgical de-bulking of redundant tissue, such as prominent cuneiform tubercles in the aryepiglottic folds that can create obstruction of the laryngeal inlet. The precise place of surgery in the management algorithm of EILO is yet to be fully established.
IMPORTANCE OF TOPIC
It is likely there are many young individuals within the general population who are misdiagnosed as having exercise-induced asthma and who would benefit from the recognition and treatment of EILO.
Patient consent
The patient consented to the publication of these images.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Online version
Read the full-length version of this article online: bjgp.org
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Hull JH, Hull PJ, Parsons JP, et al. Approach to the diagnosis and management of suspected exercise-induced bronchoconstriction by primary care physicians. BMC Pulm Med. 2009;9:29. doi: 10.1186/1471-2466-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hull JH. Not all wheeze is asthma: time for patients to exercise their rights. Thorax. 2015;70(1):7–8. doi: 10.1136/thoraxjnl-2014-206096. [DOI] [PubMed] [Google Scholar]
- 3.Johansson H, Norlander K, Berglund L, et al. Prevalence of exercise-induced bronchoconstriction and exercise-induced laryngeal obstruction in a general adolescent population. Thorax. 2015;70(1):57–63. doi: 10.1136/thoraxjnl-2014-205738. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen EW, Hull JH, Backer V. High prevalence of exercise-induced laryngeal obstruction in athletes. Med Sci Sports Exerc. 2013;45(11):2030–2035. doi: 10.1249/MSS.0b013e318298b19a. [DOI] [PubMed] [Google Scholar]
- 5.Christensen PM, MaltbæK N, Jørgensen IM, Nielsen KG. Can flow-volume loops be used to diagnose exercise induced laryngeal obstructions? A comparison study examining the accuracy and inter-rater agreement of flow volume loops as a diagnostic tool. Prim Care Respir J. 2013;22(3):306–311. doi: 10.4104/pcrj.2013.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maat RC, Hilland M, Røksund OD, et al. Exercise-induced laryngeal obstruction: natural history and effect of surgical treatment. Eur Arch Otorhinolaryngol. 2011;268(10):1485–1492. doi: 10.1007/s00405-011-1656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]