Abstract
Background:
Current literature describing the periacetabular osteotomy (PAO) is mostly limited to retrospective case series. Larger, prospective cohort studies are needed to provide better clinical evidence regarding this procedure. The goals of the current study were to (1) report minimum 2-year patient-reported outcomes (pain, hip function, activity, overall health, and quality of life), (2) investigate preoperative clinical and disease characteristics as predictors of clinical outcomes, and (3) report the rate of early failures and reoperations in patients undergoing contemporary PAO surgery.
Methods:
A large, prospective, multicenter cohort of PAO procedures was established, and outcomes at a minimum of 2 years were analyzed. A total of 391 hips were included for analysis (79% of the patients were female, and the average patient age was 25.4 years). Patient-reported outcomes, conversion to total hip replacement, reoperations, and major complications were documented. Variables with a p value of ≤0.10 in the univariate linear regressions were included in the multivariate linear regression. The backward stepwise selection method was used to determine the final risk factors of clinical outcomes.
Results:
Clinical outcome analysis demonstrated major clinically important improvements in pain, function, quality of life, overall health, and activity level. Increasing age and a body mass index status of overweight or obese were predictive of improved results for certain outcome metrics. Male sex and mild acetabular dysplasia were predictive of lesser improvements in certain outcome measures. Three (0.8%) of the hips underwent early conversion to total hip arthroplasty, 12 (3%) required reoperation, and 26 (7%) experienced a major complication.
Conclusions:
This large, prospective cohort study demonstrated the clinical success of contemporary PAO surgery for the treatment of symptomatic acetabular dysplasia. Patient and disease characteristics demonstrated predictive value that should be considered in surgical decision-making.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
A variety of hip-preservation procedures have been developed and proposed for the treatment of symptomatic acetabular dysplasia1-6. In 1988, Ganz and colleagues introduced the Bernese periacetabular osteotomy (PAO) for acetabular reorientation2. This procedure is performed through 1 incision, maintains posterior column integrity, preserves the acetabular blood supply, enables powerful multiplanar acetabular reorientation, and provides reliable healing1,2,7-16. Nevertheless, the published clinical evidence regarding this procedure is mostly limited to single-surgeon or single-institution retrospective case series17. Controversy remains relative to surgical indications, consistency of clinical outcomes, predictors of treatment results, survivorship, and generalizability of the procedure. Therefore, there exists a major need for large, prospective patient cohorts in investigations of PAO surgery.
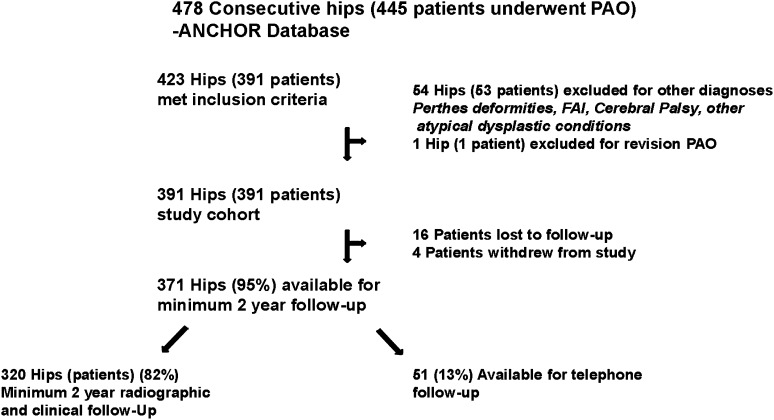
Given the major need for better clinical evidence to guide surgeon and patient decision-making, we developed a multicenter hip preservation study group, named ANCHOR (Academic Network of Conservational Hip Outcomes Research). Patient enrollment and comprehensive data collection began in 200818, and to date, we have enrolled 1,393 PAO patients. We recently completed minimum 2-year follow-up on our first 478 hips (the PAO-1 cohort). This data set is the source for the current report (Fig. 1).
Fig. 1.
Summary of the ANCHOR PAO cohort study.
The purposes of the current study were to (1) report minimum 2-year patient-reported outcomes (pain, hip function, activity, overall health, and quality of life), (2) investigate preoperative clinical and disease characteristics as predictors of clinical outcomes, and (3) report the rate of early failures and reoperations among patients undergoing contemporary PAO surgery.
Methods
Patient Selection
This multicenter, prospective, observational cohort study was approved by each participating institution’s institutional review board. From January 1, 2008, to December 31, 2010, 11 surgeons at 8 North American medical centers prospectively enrolled 478 consecutive hips (445 patients) treated with PAO (the PAO-1 cohort). All participating surgeons have experience in PAO surgery19. All patients were offered study participation. Patients were included if they underwent a PAO for the treatment of symptomatic acetabular dysplasia. Fifty-four hips (53 patients) that underwent a PAO for other diagnoses were excluded, as was 1 hip (1 patient) that underwent revision PAO (Fig. 1). After exclusions, there were 423 hips (391 patients) available for inclusion. For multivariate analysis, 32 additional hips were excluded to avoid bias because they underwent staged bilateral procedures. For these patients, data regarding the first hip treated were used in statistical analyses. This created our study cohort of 391 hips (391 patients). Sixteen of the patients (16 hips) were lost to follow-up and 4 patients (4 hips) withdrew. Therefore, 371 (95%) of the 391 eligible patients (hips) were available for the minimum 2-year follow-up (mean follow-up, 2.6 years; range, 2.0 to 5.4 years) (Fig. 1).
Study Population
Of the included 391 patients (391 hips), 308 (79%) were female and 83 (21%) were male. The average age at surgery was 25.4 years (range, 10.2 to 53.6 years). The average body mass index (BMI) was 24.9 kg/m2 (range, 17.05 to 46.61 kg/m2); 113 (29%) of the patients were overweight (BMI of 25 to <30 kg/m2), and 54 (14%) of the patients were obese (BMI of ≥30 kg/m2). Fifty-nine (15%) of the hips had previously undergone ipsilateral hip surgery (Tables I and II). At the time of PAO, 70 hips underwent concomitant hip arthroscopy and 233 had additional procedures other than arthroscopy (not including isolated open arthrotomy) (Table III).
TABLE I.
PAO Cohort Patient Characteristics*
| Variable | Summary Statistics |
| Age at surgery† (yr) | 25.4 ± 9.5 (10.2-53.6) |
| Male‡ | 83 (21%) |
| Right hip‡ | 230 (59%) |
| Caucasian‡ | 343 (88%) |
| BMI† (kg/m2) | 24.9 |
| Normal (<25 kg/m2)‡ | 224 (57%) |
| Overweight (25 to <30 kg/m2)‡ | 113 (29%) |
| Obese (≥30 kg/m2)‡ | 54 (14%) |
| Comorbidities‡ | |
| Depression | 50 (13%) |
| Back pain | 89 (23%) |
| Diabetes | 2 (0.5%) |
| Previous ipsilateral hip surgery‡ | 59 (15%) |
Study cohort of 391 patients (391 hips).
The values are presented as the mean and, for age, the standard deviation with the range in parentheses.
The values are presented as the number, with the percentage in parentheses.
TABLE II.
Prior Ipsilateral Procedures in the PAO Cohort*
| Total no. of patients with prior ipsilateral hip surgery† | 59 |
| Procedure‡ | |
| Pelvic osteotomy | 22 (37%) |
| Hip arthroscopy | 18 (31%) |
| Other | 17 (29%) |
| Proximal femoral osteotomy | 13 (22%) |
| Open reduction | 13 (22%) |
| Closed reduction | 6 (10%) |
| Acetabuloplasty | 3 (5%) |
| Shelf procedure | 2 (3%) |
| Limited open osteochondroplasty | 2 (3%) |
| Capsulorrhaphy | 2 (3%) |
| Surgical dislocation | 1 (1.7%) |
| Acetabular osteochondroplasty | 1 (1.7%) |
| PAO | 1 (1.7%) |
| Open reduction/capsulorrhaphy | 1 (1.7%) |
| Labral repair/refixation | 1 (1.7%) |
Study cohort of 391 patients (391 hips).
Includes patients with prior bilateral surgery.
The values are given as the number of patients, with the percentage of patients who underwent the prior ipsilateral hip surgery in parentheses.
TABLE III.
Concomitant Procedures at the Time of PAO*
| Procedure | No. |
| Open arthrotomy | 300 |
| Arthroscopy | 70 |
| Surgical hip dislocation | 10 |
| Acetabular chondroplasty | 14 |
| Acetabular rim osteoplasty | 4 |
| Acetabular microfracture | 3 |
| Femoral head/neck osteochondroplasty | 230 |
| Femoral head chondroplasty | 7 |
| Femoral head microfracture | 2 |
| Femoral intertrochanteric osteotomy | 13 |
| Femoral relative neck lengthening | 4 |
| Partial labral resection | 27 |
| Labral refixation/repair | 22 |
| Ligamentum teres debridement | 8 |
| Trochanteric advancement | 3 |
| Proximal femoral osteotomy | 2 |
| Psoas lengthening/release | 2 |
| Synovectomy | 1 |
| Capsuloplasty | 1 |
| Capsulorrhaphy | 1 |
| Other | 8 |
Study cohort of 391 patients (391 hips). Patients may have had >1 additional concomitant procedure to optimize hip reconstruction.
Data Collection
After providing informed consent for participation in this study, patients were given a comprehensive series of questionnaires (see Appendix)18. Patient demographics, medical comorbidities, social history, and previous hip surgery were documented (Table I). The patient-reported outcome measures included the modified Harris hip score (mHHS)20 to assess pain and function; the Hip Disability and Osteoarthritis Outcome Score (HOOS), with 5 subscores21,22 to evaluate lower-extremity function, activity, and quality of life; the University of California, Los Angeles (UCLA) score23 to assess activity level; and the Short Form (SF)-12 Health Survey to measure overall health (version 2, SF-12v2)24. Patients also self-reported their overall satisfaction with surgery, by answering the question, “What is your satisfaction level with your surgery?” Response options included “extremely satisfied,” “very satisfied,” “satisfied,” somewhat satisfied,” and “unsatisfied.” Telephone interviews were attempted for all patients who had not been seen in the clinic. Three-hundred and twenty (82%) of the patients had complete clinical and radiographic follow-up, while 51 (13%) of the patients had telephone follow-up.
Surgeons also documented preoperative diagnoses, findings of a physical examination, radiographic parameters, surgical procedure details, operative findings, and postoperative treatments for each patient (see Appendix)18. Preoperative and follow-up radiographs included, at minimum, standing or supine anteroposterior pelvic, frog, or Dunn lateral and false profile radiographs18. In this report, we focus on the difference between preoperative and postoperative acetabular inclination25, anterior center-edge angle (A-CEA)26, lateral center-edge angle (L-CEA)27, Tönnis grade25, and joint congruity28 (Table IV). The severity of acetabular dysplasia was categorized as mild (L-CEA of ≥15° or acetabular inclination [AI] of <10°), moderate (L-CEA of ≥5° to <15° or AI of ≥10° to <20°), or severe (L-CEA of <5° or AI of ≥20°) according to the consensus of the authors29,30. Intraoperative disease classification was recorded prospectively31.
TABLE IV.
Preoperative and Postoperative Radiographic Parameters Associated with PAO
| Preop. (N = 391) | Postop. (N = 320) | Change (Mean and Std. Dev.)* | P Value | |
| L-CEA | ||||
| Mean (deg) | 8.1 | 29.6 | 20.9 ± 12.4 | <0.001 |
| <5° | 35% | |||
| ≥5° to <15° | 30% | |||
| ≥15° | 35% | |||
| A-CEA | ||||
| Mean (deg) | 6.0 | 30.2 | 23.4 ± 17.0 | <0.001 |
| <5° | 41% | |||
| ≥5° to <15° | 32% | |||
| ≥15° | 28% | |||
| Acetabular inclination | ||||
| Mean (deg) | 22.5 | 5.6 | −16.9 ± 10.7 | <0.001 |
| <10° | 5% | |||
| ≥10° to <20° | 36% | |||
| ≥20° | 59% | |||
| Tönnis classification | ||||
| Grade 0-1 | 91% | 93% | ||
| Grade 2 | 8% | 6% | ||
| Grade 3-4 | 2% | 1% | ||
| Joint congruity | ||||
| Excellent | 34% | 55% | ||
| Good | 54% | 38% | ||
| Fair | 11% | 7% | ||
| Poor | 1% | 0% |
The change is based on patients with preoperative and postoperative measures.
Surgical Treatment
All patients underwent a PAO using the basic technique described by Ganz et al.2, but details of the surgical technique were left to the discretion of the surgeon. Acetabular reduction was assessed with intraoperative radiography. Additional ipsilateral procedures were performed if the surgeon decided it was necessary to optimize the hip reconstruction (Table III).
All failures, defined as conversion to total hip arthroplasty, reoperations, and major complications, were documented prospectively. We previously reported on complications associated with PAO surgery19. Major complications were defined as grade III (requiring intervention) or IV (life-threatening or with the potential for permanent disability) according to the Dindo-Clavien grading scheme32,33 as modified and validated by our group34,35.
Statistical Analysis
Continuous variables, with the exception of BMI, Tönnis grade, and some of the intra-articular variables, are reported as the mean and the standard deviation with the p value and 95% confidence interval (CI). BMI, Tönnis grade, and the continuous intra-articular variables were divided into categories and treated as categorical variables. Categorical variables are reported as percentages. Changes between preoperative and postoperative values were tested with paired-sample t tests. The relationship between each risk factor and the preoperative to postoperative difference in each outcome variable was evaluated with simple linear regression. When an outcome had >1 risk factor with a p value of ≤0.10, a multiple regression analysis was performed. All risk factors with a p value of ≤0.10 were initially included in the model. A backward stepwise method was then used, removing risk factors with a p value of >0.05 in the multivariate model, starting with the least significant and rerunning the model with the remaining risk factors until all remaining independent variables had a p value of ≤0.05. The effect of hospital site on the model was then examined using an indicator variable for each site. Possible interactions between hospital site and the risk factors in the model were evaluated. The relationship of radiographic parameters and intra-articular variables with outcomes were evaluated in analyses of covariance, with the postoperative outcome variable as the dependent variable, the radiographic parameters and intra-articular measurement as the independent variables, and the preoperative scores as the covariate.
Results
At an average of 2.6 years of follow-up (range, 2.0 to 5.4 years), there were clinically important improvements in all mean patient-reported outcome measures when compared with preoperative baseline scores (Table V). Three hundred and sixty-four (93%) of the patients were satisfied with their outcome (55% extremely satisfied, 26% very satisfied, and 12% satisfied). There was a major decrease in the overall level of pain, which was reflected by a mean increase (less pain) of 28.3 (95% CI, 25.3 to 30.1) for the HOOS pain subscore (p < 0.001). Hip and lower-extremity function improved markedly, as indicated by a mean increase of 23.6 (95% CI, 21.5 to 25.5) for the mHHS and an increase of 21.4 (95% CI, 18.9 to 23.6) for the HOOS activities of daily living subscore (p < 0.001 for both). The improvement in mHHS was also reflective of patient improvement in mean activity level, which was indicated by mean increases of 0.4 (95% CI, 0.23 to 0.77) for the UCLA score and 30.8 (95% CI, 27.5 to 34.1) for the HOOS sports and recreation subscore. Patients’ overall quality of life and overall health improved, as reflected by mean increases of 34.6 (95% CI, 31.4 to 37.0) for the HOOS quality of life score (p < 0.001), 9.2 for the SF-12 physical component summary score (p < 0.001), and 2.2 for the SF-12 mental component summary score (p <0.001). Clinically important changes have been reported to be 6 to 11 points for the HOOS subscales (0 to 100 points)22 and 3 to 5 points for the SF-12 subscales (0 to 100 points)24.
TABLE V.
Preoperative and Postoperative Patient-Reported Outcomes Associated with PAO*
| Mean Score |
Change† |
||||||
| Preop. | Postop. | Mean and Std. Dev. | 95% CI | N | P Value | MCID‡ | |
| mHHS | 61.2 | 85.1 | 23.6 ± 19.2 | 21.5-25.5 | 327 | <0.001 | NA |
| UCLA | 6.8 | 7.2 | 0.4 ± 2.6 | 0.23-0.77 | 330 | 0.003 | NA |
| HOOS | |||||||
| Total symptoms | 58.7 | 79.3 | 20.1 ± 20.1 | 18.3-22.5 | 320 | <0.001 | 9 |
| Pain | 55.8 | 84.3 | 28.3 ± 22.6 | 25.3-30.1 | 308 | <0.001 | 9 |
| Activities of daily living | 67.6 | 89.7 | 21.4 ± 22.1 | 18.9-23.6 | 306 | <0.001 | 6 |
| Sports and recreation | 45.8 | 77.0 | 30.8 ± 30.3 | 27.5-34.1 | 303 | <0.001 | 10 |
| Quality of life | 35.1 | 69.8 | 34.6 ± 27.4 | 31.4-37.0 | 317 | <0.001 | 11 |
| SF-12 | |||||||
| Physical component | 39.4 | 49.0 | 9.2 ± 11.2 | 8.2-10.9 | 322 | <0.001 | 5 |
| Mental component | 51.2 | 52.8 | 2.2 ± 10.5 | 1.03-3.4 | 322 | <0.001 | 3 |
Study cohort of 371 hips in 371 patients available for minimum 2-year clinical follow-up.
The change is based on patients with preoperative and postoperative measures.
MCID = minimal clinically important difference, and NA = not applicable.
Independent predictors of patient-reported outcomes were identified with multivariate regression analysis and included age, sex, BMI, concomitant ipsilateral procedures, and hospital site (Table VI). Increasing age was predictive of improved postoperative HOOS pain scores. Each additional year of age was correlated with 0.29 points (95% CI, 0.20 to 0.56 points) of improvement in postoperative pain score (p = 0.04). Male sex was a negative predictor of the ability to perform activities of daily living; male sex was associated with a clinically important decrease of 9.16 points (95% CI, −15.13 to −3.18 points) in the HOOS activities of daily living score (p = 0.003). Compared with normal BMI (<25 kg/m2), being overweight (BMI of 25 to <30 kg/m2) was correlated with an improvement of 6.05 (95% CI, 0.08 to 12.03) in the postoperative HOOS pain score (p <0.05), a clinically important improvement of 8.36 (95% CI, 2.73 to 13.99) in the HOOS activities of daily living score (p = 0.004), and an improvement of 8.11 (95% CI, 1.14 to 15.08) in the HOOS quality of life score (p = 0.02). Compared with normal BMI, obesity (BMI of ≥30 kg/m2) was correlated with a clinically important improvement of 8.81 (95% CI, 1.43 to 16.19) in the HOOS activities of daily living score (p = 0.02) and 3.58 (95% CI, 0.01 to 7.14) in the postoperative SF-12 physical component summary score (p <0.05). Prior ipsilateral surgery was correlated with an improvement of 0.9 (95% CI, 0.1 to 1.7) in the postoperative UCLA score (p = 0.02). An ipsilateral procedure performed at the time of PAO was predictive of an improvement of 5.35 (95% CI, 0.1 to 10.29) in the HOOS total symptoms score (p <0.05) and a clinically important increase of 4.64 (95% CI, 1.8 to 7.49) in the SF-12 physical component summary score (p = 0.001). There was a significant effect of site on the outcomes of the UCLA score and HOOS total symptoms and total pain. Two sites had significantly lower differences between preoperative and postoperative UCLA scores than did the other sites. Adding an indicator variable for the 2 sites to the model caused the covariate of ipsilateral procedures to become nonsignificant. Although there were significant site effects for the 2 HOOS outcomes, they did not interact with the other variables in the model and did not affect the interpretation of their effect on outcomes.
TABLE VI.
Summary of Independent Predictors for PAO Outcome Measures*
| Independent Predictors of Patient-Reported Outcomes |
||||||||||||
| Age |
Male Sex |
Overweight (BMI of 25 to <30 kg/m2) |
Obese (BMI of ≥30 kg/m2) |
Concomitant Procedures |
Site Effect |
|||||||
| Patient Self-Reported Outcome Measure | Coefficient (95% CI) | P Value | Coefficient (95% CI) | P Value | Coefficient (95% CI) | P Value | Coefficient (95% CI) | P Value | Coefficient (95% CI) | P Value | Coefficient (95% CI) | P Value |
| HOOS | ||||||||||||
| Total symptoms | 5.35 (0.1 to 10.29) | <0.05 | −9.45 (−17.61 to −1.29)† | 0.02 | ||||||||
| Total pain | 0.29 (0.20 to 0.56) | 0.04 | 6.05 (0.08 to 12.03) | <0.05 | −8.81 (−15.8 to −1.81)‡ | 0.01 | ||||||
| Total activities of daily living | −9.16 (−15.13 to −3.18) | 0.003 | 8.36 (2.73 to 13.99) | 0.004 | 8.81 (1.43 to 16.19) | 0.02 | ||||||
| Total quality of life | 8.11 (1.14 to 15.08) | 0.02 | ||||||||||
| SF-12 physical component | 3.58 (0.01 to 7.14) | <0.05 | 4.64 (1.8 to 7.49) | 0.001 | ||||||||
Multivariate analysis based on patient-reported outcome measures for 371 hips in 371 patients available for minimum 2-year clinical follow-up. UCLA, mHHS, and SF-12 mental component summary scores were not independently associated with patient-reported outcomes.
Site 12.
Sites 6 and 12.
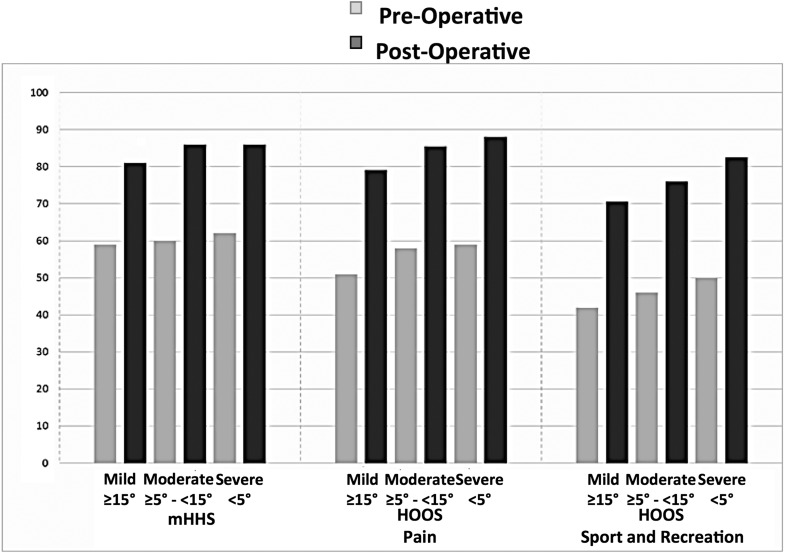
Baseline dysplasia severity was tested by categorizing the severity of deformity as mild (L-CEA of ≥15° or AI of <10°), moderate (L-CEA of ≥5° to <15° or AI of ≥10° to <20°), or severe (L-CEA of <5° or AI of ≥20°) (Fig. 2). A strong correlation was identified with postoperative mHHS and HOOS pain and sports and recreation scores. While all dysplasia severity categories had improvements in patient-reported outcome scores, analyses of covariance demonstrated that patients with severe dysplasia had greater improvements in the mHHS and HOOS pain and sports and recreation scores when compared with those with mild dysplasia (p < 0.02). Those with moderate dysplasia also had a greater improvement in mHHS relative to the mild group (p < 0.02) (Fig. 2). No pairwise differences were demonstrated between the different categories of dysplasia severity as categorized by AI. The severity of the preoperative Tönnis grade of osteoarthritis did not correlate with patient-reported outcome scores. Intraoperative disease classification (labrum and acetabular and femoral head articular cartilage) showed no correlation with patient-reported outcomes (data not shown).
Fig. 2.
Baseline dysplasia severity was tested by categorizing the severity of deformity severity as mild (L-CEA of ≥15° or AI of <10°) (n = 137 hips), moderate (L-CEA of ≥5° to <15° or AI of ≥10° to <20°) (n = 117 hips), or severe (L-CEA of <5° or AI of ≥20°) (n = 137 hips). While all patients had significant improvement in their patient-reported outcome scores, analyses of covariance demonstrated that patients with severe dysplasia had greater improvements in the mHHS, HOOS pain, and HOOS sports and recreation scores when compared with those with mild dysplasia (p<0.02). Those with moderate dysplasia also had a greater improvement in mHHS relative to the mild group (p<0.02).
At the most recent follow-up, 3 (0.8%) of the hips had undergone conversion to total hip arthroplasty and 12 (3%) of the hips required reoperation, excluding hardware removal. The average age, at the time of surgery, of the patients requiring subsequent total hip replacement was 28.3 years (range, 18 to 35 years), and 2 of the 3 each had undergone >2 previous ipsilateral hip procedures. Reoperations included 8 hip arthroscopies for persistent pain after the PAO. Major complications, classified as modified Dindo-Clavien grade III or IV were noted for 26 (7%) of the hips. Transient nerve palsy was noted in 9 (2%) of the cases, 6 with complete resolution. There were 2 cases (0.5%) of pulmonary emboli and 1 (0.3%) deep venous thrombosis (DVT), all treated successfully with anticoagulation. There were 2 cases (0.5%) of deep infection requiring operative debridement. There were 6 fractures (1.5%). There was 1 dislocation requiring closed reduction. Four (1%) of the patients experienced heterotopic ossification requiring excision. One patient fell, causing loss of fixation that required a return to the operating room for refixation of the mobilized acetabulum.
Discussion
While several surgical treatment options have been described for the treatment of acetabular dysplasia1,2,7-16, these reports were mostly limited to retrospective single-surgeon or single-institution series17. In this multicenter, prospective study, we report on our first 391 cases followed for a minimum of 2 years. The procedure has been associated with marked improvements in pain, hip/lower-extremity function, and quality of life. Patient activity increased after the PAO, and patient satisfaction with the surgery was very high (93%). The strongest predictors of successful outcomes were female sex, increased age, and the patient being overweight or obese.
Our data introduce several interesting findings relative to clinical predictors of PAO surgical outcomes. Specifically, increasing age was predictive of improved HOOS pain scores (0.29 points per year), and BMI status as overweight and as obese were positive predictors for multiple outcome measures, including HOOS pain, activities of daily living, and quality of life scores for the former and activities of daily living and the SF-12 physical component summary score for the latter. These observations were unexpected, yet they may reflect patient expectations with surgery. It is possible that older and overweight or obese patients place less demand on the hip and have lower functional expectations. Additionally, male sex was a predictor of a lower HOOS activities of daily living score, suggesting sex-dependent differences in PAO outcomes. Previous studies have highlighted the morphologic differences and potential for poorer outcomes for male patients36. Current information suggests that male patients are at heightened risk for secondary femoroacetabular impingement (FAI) after PAO36,37, and this could negatively impact activities of daily living. Another predictor of suboptimal outcomes was preoperative mild dysplasia compared with severe dysplasia. While the patients with mild dysplasia demonstrated major improvements in all patient-reported outcomes, the improvements were less than those of patients with moderate deformity (mHHS) and those with severe deformity (mHHS, HOOS pain, and HOOS sports and recreation). This finding highlights a very important and unresolved issue in hip-preservation surgery. Patients with mild dysplasia pose substantial challenges relative to diagnosis, treatment, and surgical decision-making. Symptomatic mild dysplasia can be associated with other factors that may impact treatment results, including excessive femoral torsion and soft-tissue laxity. Precise acetabular reorientation is also challenging in the mildly deformed hip, as overcorrection is possible and may lead to post-PAO FAI. It is also known that a high percentage of dysplastic hips (including mildly dysplastic ones) have concurrent femoral deformities associated with FAI38-41 and may be at risk for secondary FAI after PAO.
Our study had limitations. While all patients were diagnosed and treated in a similar fashion, there may have been differences among surgeons’ diagnostic algorithms, treatment indications, and surgical procedure details. From our analysis of the impact of site on PAO outcomes, 2 sites were demonstrated to have lower outcomes in terms of the UCLA and HOOS symptoms and pain scores. Although there were site effects with these HOOS subscores, they did not interact with other variables in the model and did not affect their interpretation. Site did have an impact on the UCLA outcome. The addition of an indicator variable for the sites with lower outcomes caused the previously significant covariate of ipsilateral procedures to become nonsignificant, leaving only the site variable in the model. Additionally, these were short-term follow-up data. As this cohort is followed over time, additional observations will likely assist in the refinement of PAO surgery. The ANCHOR database is also primarily focused on acetabular dysplasia, and measurements of femoral morphology was not reported and how it contributes to hip mechanics is poorly understood.
Mid-term to long-term outcomes of retrospective PAO cohorts have been reported. Steppacher et al. reported on 68 hips followed for an average of 20 years and found a 60% survivorship rate15. Poor clinical outcomes as measured by the Merle d’Aubigné and Postel score were associated with more advanced age at surgery, the preoperative hip score, a positive anterior impingement test, a limp, the osteoarthrosis grade, and the postoperative extrusion index. Matheney et al. reported on 135 hips and documented a 76% survivorship rate at 9 years9. Those authors identified 2 predictors of failure (defined as total hip replacement or a high pain score) including an age of >35 years at the time of surgery or poor/fair preoperative joint congruency. Clohisy et al. performed a systematic review of the literature that encompassed 626 hips followed for an average of 5 years17. Seventy-nine percent had a good or excellent clinical result, 7.3% were converted to total hip replacement, and the major complication rate varied from 6% to 37%. Moderate to advanced preoperative osteoarthritis was a predictor of poor outcome. It is important to note that these studies represent the initial experiences with the PAO. Patient selection criteria and surgical technique have evolved substantially over the past 2 decades.
To our knowledge this prospective, multicenter cohort study represents the largest and most comprehensive data set for contemporary PAO surgery. Our results demonstrate marked improvements in patient-reported outcomes, spanning pain, function, activity, quality of life, and overall health. Among well-selected patients treated with sound surgical technique, favorable clinical outcomes can be expected; the early failure/reoperation rates were low. Continued expansion and follow-up of the ANCHOR PAO cohort will provide high-level clinical evidence to further refine and optimize this powerful hip-preservation procedure.
Appendix
The patient and surgeon questionnaires used in the study are available with the online version of this article as a data supplement at jbjs.org (reproduced from: Clohisy JC, Baca G, Beaulé PE, Kim YJ, Larson CM, Millis MB, Podeszwa DA, Schoenecker PL, Sierra RJ, Sink EL, Sucato DJ, Trousdale RT, Zaltz I; ANCHOR Study Group. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013 Jun;41(6):1348-56. Epub 2013 May 13).
Footnotes
Investigation performed at Washington University, St. Louis, Missouri
Disclosure: This work was supported in part by Award UL1RR024992 from the National Center for Research Resources (J.C.C.). It was also supported in part by the Curing Hip Disease Fund (J.C.C.), the ANCHOR Fund, Smith & Nephew (J.C.C.), and the NFL Charities (J.C.C.). On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work.
Disclaimer: The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
References
- 1.Clohisy JC, St John LC, Nunley RM, Schutz AL, Schoenecker PL. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res. 2009. September;467(9):2221-7. Epub 2009 Mar 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988. July;232:26-36. [PubMed] [Google Scholar]
- 3.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984. March;66(3):430-6. [PubMed] [Google Scholar]
- 4.Salter RB. The classic. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip by Robert B. Salter, J. Bone Joint Surg. (Brit) 43B:3:518, 1961. Clin Orthop Relat Res. 1978. Nov-Dec;137:2-14. [PubMed] [Google Scholar]
- 5.Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973. March;55(2):343-50. [PubMed] [Google Scholar]
- 6.Tönnis D. Surgical treatment of congenital dislocation of the hip. Clin Orthop Relat Res. 1990. September;258:33-40. [PubMed] [Google Scholar]
- 7.Biedermann R, Donnan L, Gabriel A, Wachter R, Krismer M, Behensky H. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop. 2008. October;32(5):611-7. Epub 2007 Jun 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartig-Andreasen C, Troelsen A, Thillemann TM, Søballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res. 2012. November;470(11):2978-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am. 2010. September;92(Suppl 1 Pt 2):115-29. [DOI] [PubMed] [Google Scholar]
- 10.Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999. June;363:21-32. [PubMed] [Google Scholar]
- 11.McKinley TO. The Bernese periacetabular osteotomy: review of reported outcomes and the early experience at the University of Iowa. Iowa Orthop J. 2003;23:23-8. [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999. July;364:92-8. [DOI] [PubMed] [Google Scholar]
- 13.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006. September;88(9):1920-6. [DOI] [PubMed] [Google Scholar]
- 14.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239-45. [PubMed] [Google Scholar]
- 15.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008. July;466(7):1633-44. Epub 2008 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009. September;91(9):2169-79. [DOI] [PubMed] [Google Scholar]
- 17.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009. August;467(8):2041-52. Epub 2009 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clohisy JC, Baca G, Beaulé PE, Kim YJ, Larson CM, Millis MB, Podeszwa DA, Schoenecker PL, Sierra RJ, Sink EL, Sucato DJ, Trousdale RT, Zaltz I; ANCHOR Study Group. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013. June;41(6):1348-56. Epub 2013 May 13. [DOI] [PubMed] [Google Scholar]
- 19.Zaltz I, Baca G, Kim YJ, Schoenecker P, Trousdale R, Sierra R, Sucato D, Sink E, Beaulé P, Millis MB, Podeszwa D, Clohisy JC. Complications associated with the periacetabular osteotomy: a prospective multicenter study. J Bone Joint Surg Am. 2014. December 3;96(23):1967-74. [DOI] [PubMed] [Google Scholar]
- 20.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. June;51(4):737-55. [PubMed] [Google Scholar]
- 21.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988. December;15(12):1833-40. [PubMed] [Google Scholar]
- 22.Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip Disability and Osteoarthritis Outcome Score (HOOS)—validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003. May 30;4:10 Epub 2003 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984. February;66(2):228-41. [PubMed] [Google Scholar]
- 24.Ware J Jr., Kosinski M, Turner-Bowker D, Gandek B. How to score Version 2 of the SF-12 Health Survey (with a supplement documenting Version 1). Lincoln, RI: Quality Metric Incorporated; 2002. [Google Scholar]
- 25.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976. September;(119):39-47. [PubMed] [Google Scholar]
- 26.Lequesne M, de Seze. [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies]. Rev Rhum Mal Osteoartic. 1961. December;28:643-52. French. [PubMed] [Google Scholar]
- 27.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939(83):7-38. [Google Scholar]
- 28.Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006. September;88(9):1915-9. [DOI] [PubMed] [Google Scholar]
- 29.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005. February;87(2):254-9. [DOI] [PubMed] [Google Scholar]
- 30.Nepple JJ, Martell JM, Kim YJ, Zaltz I, Millis MB, Podeszwa DA, Sucato DJ, Sink EL, Clohisy JC; ANCHOR Study Group. Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med. 2014. October;42(10):2393-401. Epub 2014 Aug 18. [DOI] [PubMed] [Google Scholar]
- 31.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005. July;87(7):1012-8. [DOI] [PubMed] [Google Scholar]
- 32.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992. May;111(5):518-26. [PubMed] [Google Scholar]
- 33.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. August;240(2):205-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sink EL, Beaulé PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011. June 15;93(12):1132-6. [DOI] [PubMed] [Google Scholar]
- 35.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J; Academic Network for Conservational Hip Outcomes Research Group. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012. August;470(8):2220-6. Epub 2012 Apr 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duncan ST, Bogunovic L, Baca G, Schoenecker PL, Clohisy JC. Are there sex-dependent differences in acetabular dysplasia characteristics? Clin Orthop Relat Res. 2015. April;473(4):1432-9. Epub 2015 Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ziebarth K, Balakumar J, Domayer S, Kim YJ, Millis MB. Bernese periacetabular osteotomy in males: is there an increased risk of femoroacetabular impingement (FAI) after Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2011. February;469(2):447-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009. January;467(1):128-34. Epub 2008 Nov 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robertson DD, Essinger JR, Imura S, Kuroki Y, Sakamaki T, Shimizu T, Tanaka S. Femoral deformity in adults with developmental hip dysplasia. Clin Orthop Relat Res. 1996. June;327:196-206. [DOI] [PubMed] [Google Scholar]
- 40.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008. April;466(4):782-90. Epub 2008 Feb 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br. 1998. July;80(4):711-9. [DOI] [PubMed] [Google Scholar]