Abstract
Influenza A virus is a pathogen of global medical importance causing significant health and socio-economic costs every year. Influenza virus is an unusual pathogen in that it is pleomorphic, capable of forming virions ranging in shape from spherical to filamentous. Despite decades of research on the influenza virus, much remains unknown about the formation of filamentous influenza viruses and their role in the viral replication cycle. Here, we discuss what is known about influenza virus assembly and budding, focusing on the viral and host factors that are involved in the determination of viral morphology. Whilst the biological function of the filamentous morphology remains unknown, recent results suggest a role in facilitating viral spread in vivo. We discuss these results and speculate on the consequences of viral morphology during influenza virus infection of the human respiratory tract.
Keywords: Influenza virus, Morphology, Filaments, Assembly, Budding
Introduction
Between 1918 and 1920, an estimated 50–100 million people died from the first recorded pandemic of a viral infection commonly known as the flu [1]. This outbreak, nowadays known as the Spanish flu, was caused by the Influenza A virus (IAV). Since 1920, IAV has continued to cause pandemics with the most recent being the 2009 H1N1 swine flu pandemic [2] which was estimated to have infected over 60 million people and caused 12,000 deaths in the USA alone [3].
IAV is a pleomorphic virus of the Orthomyxoviridae family consisting of a segmented, single stranded, negative sense RNA genome [4]. Responsible for seasonal outbreaks and occasional pandemics IAV is a major burden on health systems globally and is estimated to cost the US economy $87.1bn annually [5]. Five to 15 % of the Northern hemisphere’s population is estimated to be affected per annum [6] with 250,000–500,000 deaths globally per year [7]. The most severe illness occurs in immuno-compromised, elderly and very young individuals and is often followed by secondary bacterial pneumonia, resulting in significant morbidity and mortality.
IAV infects the cells of the upper respiratory tract, causing illness in a wide range of hosts, including humans, pigs, horses and birds. Birds are thought to be the reservoir for IAV in the wild [8] and are a key source for the emergence of novel IAV strains [9], such as the 1918 Spanish flu. Recent strains emerging from the wild bird population include the high pathogenicity avian influenza virus strains H5N1 and H7N9, currently circulating in Eastern Asia where they have up to a 60 % case-fatality rate in humans, though do not yet spread efficiently from person to person [10].
The Influenza A Virus
The IAV genome comprises of 11 genes on eight RNA segments. These can broadly be categorised as encoding the viral structural or non-structural proteins. Haemagglutinin (HA), neuraminidase (NA), nucleoprotein (NP) and matrix proteins one and two (M1 and M2) are primarily structural proteins with additional functional roles, whilst the polymerase subunits (PB1, PB2 and PA) and the non-structural proteins (NS1 and NS2) serve mainly function roles during virus replication. NP binds to and is involved in the packaging of the viral genome along with the polymerase subunits for transport and assembly [11] and also interacts with various cellular proteins, such as CRM1 involved in nuclear export of the replicated viral genome [12]. HA is responsible for virus attachment to a target cell by recognition of sialic acid residues on the cell surface [13]. Following attachment, the virus undergoes receptor-mediated endocytosis and subsequent endosomal acidification triggers HA fusion activity wherein HA mediates the fusion of the viral envelope with the endosomal membrane, freeing the viral genome to traffic to the nucleus [14]. NA has enzymatic activity, cleaving sialic acid bonds and releasing newly formed viruses from the host cell [15–17]. NA is the target of small molecule pharmaceuticals used to treat influenza: Relenza® (zanamivir) and Tamiflu® (oseltamivir) [18]. These are structural analogues of sialic acid, and work to inhibit the enzymatic action of NA, thus retaining newly formed virus on the host cells. HA and NA are viral surface proteins and the main antigenic determinants of the virus. Antigenic variations in HA and NA give rise to the nomenclature ‘H’ and ‘N’ (e.g. H1N1). The matrix proteins, M1 and M2, are formed from alternative reading frames of RNA segment seven [19]. M1 is the most abundant viral protein forming a scaffold beneath the host membrane derived viral envelope. M1 anchors NA, HA and M2 in place within the envelope and interacts with the viral genome in the ribonucleoprotein (RNP) complex. M2 is a transmembrane ion channel protein, which plays a fundamental role in the initial stages of viral infection. Once in the acidic endosome, M2 allows protons to enter the virus, triggering uncoating [20] and the release of the viral RNP from M1 [21]. M2 also plays a pivotal role in IAV budding by altering membrane curvature, facilitating the assembly of filamentous virions and then mediating membrane scission and the release of budding viruses [22].
Viral Assembly and Budding
It is thought that IAVassembly and budding occurs at lipid raft domains on the apical surface of the host cell plasma membrane, where IAV proteins are brought together in high concentrations within specific membrane regions [23]. NA and HA are both fundamentally associated with these domains, with the transmembrane domain of HA promoting the raft association [24]. HA has the ability to induce budding of virus-like particles (VLPs) in and of itself, forming vesicles similar in appearance to viruses [25]. This suggests that HA may possess an intrinsic capacity to alter membrane curvature. Alternatively, the induction of membrane curvature may be driven by the crowding of HA molecules within a defined space (i.e. within a lipid raft domain). However, HA VLP budding only produces spherical particles, whereas VLPs are filamentous when M1 is also expressed [26••]. After the formation of a viral bud, the virus remains attached to the host cell through a small membrane neck. At this point, the M2 protein alters membrane curvature, constricting the neck and causing membrane scission [27]. The enzymatic action of NA can then release the fully formed virus from the host cell. Throughout this process, it is not clear when the genome is recruited to the budding virion nor the effects RNP binding has on the budding process or the formation of filamentous virions.
Viral Morphology
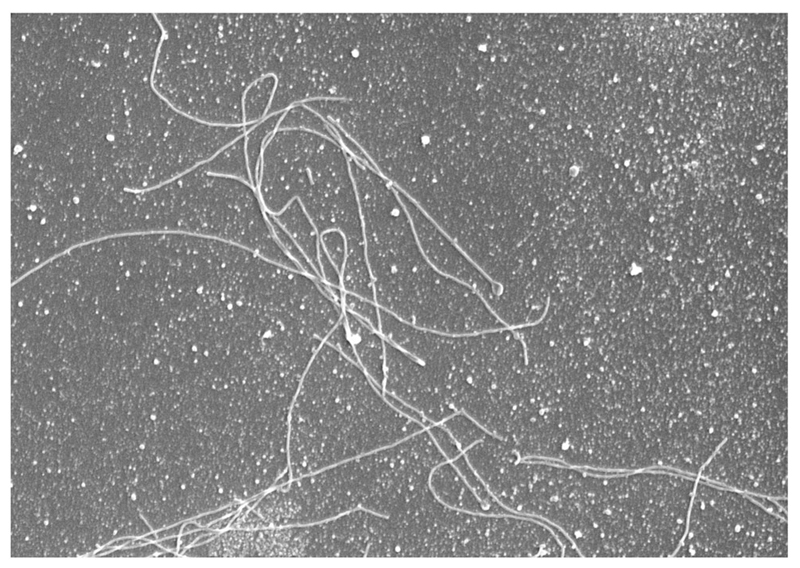
IAV is a pleomorphic virus, known to display a range of morphological states, from filamentous to spherical, with ovoid or bacilliform intermediates often observed (Fig. 1). In certain cases, IAV strains may produce solely spherical virions; however, filament-producing strains always produce a mixture of both filamentous and spherical virions. It is known that filamentous viruses contain only one copy of the IAV genome, thus each sphere, bacilliform or filament is thought to be a single infectious unit regardless of length. Structurally, viral filaments are roughly equal, or slightly smaller in diameter (80–100 nm) to spherical virus (120 nm), but extend to a significant length, sometimes upwards of 20 μm, with lengths over 50 μm not unheard of. Filamentous viruses are particularly of note as they are recurrently observed in human clinical infections [28–34, 35••, 36] (for example, filamentous virions are seen in lung sections from fatal cases of the 2009 H1N1 pandemic [37]). In contrast, many laboratory strains produce solely spherical virions. The biological function of this morphology is not known nor is it understood how host adaptation can select for a specific viral morphology; however, repeated passaging of filamentous human clinical isolates in chicken eggs causes a morphological adaptation resulting in the production of only spherical virus [28, 38] whereas adaptation to growth in guinea pigs restores filament formation [35••]. Mutations of several different viral proteins can influence filament formation during the process of adaptation. For example, the filamentous A/Udorn/72 strain becomes spherical with a single point mutation in the M1 protein [39–41]. Thus, a range of both host and viral factors governs the formation of filamentous virions during influenza virus assembly and budding.
Fig. 1.
Filamentous and spherical influenza virions. MDCK cells were infected with 3 MOI of A/Udorn/72 influenza virus for 18 h. The supernatant was harvested, fixed and processed for scanning electron microscopy. Image is 14 × 20 μm
Viral Determinants of Morphology
Many different studies have investigated the viral factors that determine morphology, with most focusing on the structural proteins M1 and M2 and their role in viral assembly. M1 plays a crucial role in the assembly and budding of both filamentous and spherical IAV [23, 24]. In 2004, Elleman and Barclay reported that M1 was also the main viral determinant of filamentous morphology [42]. Swapping the ‘M’ RNA segment from the spherical strain, A/Puerto Rico/8/1934 (PR8), with the M segment of the filamentous strain, A/Udorn/1972 (Udorn), enabled the conversion of a spherical strain into a filamentous strain (when M-Udorn was inserted into PR8) and a filamentous strain into a spherical strain (M-PR8 into Udorn) [23, 40]. In 2007, Chen et al. showed that M1 is required for the formation of filamentous VLPs, though it was not required to form bacilliform (<1 μm) or spherical VLPs [25, 43, 44].
Interestingly, in filamentous viruses, M1 appears to adopt a helical conformation [14], which is not apparent in spherical virus, suggesting that structural variations in the M1 protein may govern viral structure [45]. As the most abundant viral protein, M1 forms a layer under the viral envelope and is responsible for interacting with NA, HA and M2 to form a scaffold-like complex [46]. It is postulated that M2 can stabilise this complex during budding to allow for continued M1 polymerisation and the formation of a viral filament [22, 47]. In support of this hypothesis, it has been observed that mutation of the M2 protein can dramatically affect viral morphology, with mutations in the c-terminal amphipathic helix converting a filamentous virus into a spherical one [47], whereas truncation of the c-terminus at residue 70 enables filament formation from an otherwise spherical virus [48]. The effect of M2 on viral filament formation has also been studied using the monoclonal antibody 14C2, which has been shown to inhibit filamentous virus formation whilst permitting spherical virus to bud [47]. 14C2 binds to the ectodomain of M2 and is thought to disrupt the binding between the M2 cytoplasmic tail and M1 [47]. This is consistent with other data showing that mutation of the M2 cytoplasmic tail between residues 70–77 reduces M1-M2 interactions and subsequently the amount of M1 and RNP packaged in virions [49, 50]. Intriguingly, a single amino acid substitution in the M2 cytoplasmic tail of the filamentous Udorn strain, Y76A, significantly reduced the number and length of filamentous viruses produced [50]. However, recovery of the filamentous morphology was seen with the addition of a S71Y mutation, though it is not clear if these mutations also affect M1-M2 interactions [50]. In either case, it is possible that the M2 protein affects viral filament formation by altering membrane curvature, stabilising the site of budding and therefore enabling M1 polymerisation and the elongation of a viral filament [18, 20]. Thus, M2 appears to modify filament formation through binding and recruitment of M1, whereas M1 itself is required for the actual structuring of the filament. This suggests that filamentous virion production is likely a multifaceted process, affected by several different viral proteins, all occurring in the context of an array of cellular partners.
Host Determinants of Morphology
IAV is pleomorphic, adopting both spherical and filamentous forms [45]. As described, viral morphology can be altered through adaptation to different hosts, implying that there are host-specific influences on filament formation [35••]. Filamentous IAV is consistently found in human clinical isolates from laboratory confirmed cases, in the 2009 H1N1 pandemic [37] and as far back as the 1957–1958 pandemic [38], with the first identification having occurred in 1946 [51]. It is known that filament forming strains become spherical after repeated passage in embryonated chicken eggs, whereas the filamentous morphology is retained during passage in Madin-Darby canine kidney (MDCK) cells [28, 35••, 52]. Thus, host cell factors play a considerable role in filament formation, and IAV morphology may represent an adaptation to a specific host cell environment. Previous research has identified several host proteins that affect viral morphology. In particular, when the Udorn virus is grown in polarised MDCK cells, filamentous virus is produced from the apical plasma membrane [23, 24, 45]. Chemical disruption of the actin cytoskeleton causes depolarization of the cells and specifically reduces filamentous virus production whilst having no effect on the budding of spherical virus [53]. Considering that the upper respiratory tract consists of highly polarised epithelial cells and is the primary site of human infection, the detection of filamentous IAV in human clinical samples may be directly related to epithelial cell polarisation. However, other experiments have shown that human embryonic kidney 293T cells are capable of producing filamentous virions, despite an absence of cell polarisation and a lack of a defined apical membrane [54]. Thus, the impact of cell polarisation on viral morphology may be more complicated and may be influenced by other host cell proteins or processes.
In 2010, Bruce et al. reported that Rab11 and Rab11-family interacting protein 3 (FIP3) are necessary for the formation of filamentous virus [55]. Rab11 is a GTPase involved in the recycling endosome pathway and plays a role in protein and vesicle transport [56]. Rab11 is necessary for the budding of all morphologies of IAV [54]; however, Rab11-FIP3 is essential for the formation of filamentous IAVs [55]. The FIPs regulate localisation and trafficking of target proteins [57] by interacting with motor proteins, such as myosin Vb [58] and kinesin [59]. FIP3 is involved in the regulation of Rab11 and, subsequently, in several cellular pathways, such as the essential trafficking of endosomes to the cleavage furrow during cytokinesis [60] and the regulation of actin filaments [57]. The polymerase subunit PB2 of the viral RNP complex interacts with Rab11, which is complexed with cellular transport vesicles and FIP3 [61, 62•]. RNPs then essentially ‘piggyback’ on these vesicles, travelling with Rab11 from the MTOC to the site of virus budding along the microtubule network [63]. Once near the plasma membrane, these RNP-Rab11-vesicle complexes uncouple in an uncharacterized mechanism, alluded to by the fact that budded virus (both spherical and filamentous) are devoid of Rab11 [64]. It is speculated that interactions with M1 are then responsible for organisation of RNPs at the plasma membrane, as M1 is intrinsically associated with RNPs in late stage infection to prevent their re-entry in to the nucleus [65]. It has not yet been demonstrated, however, if the association with M1 uncouples the Rab11-RNP complexes or if Rab11-transported vesicles contribute any additional components to the budding virus. One possible Rab11-associated component is FIP3, though how this protein contributes to viral filament formation remains unclear. However, it is apparent that the morphology of IAV depends on both cellular and viral factors.
Functions of Viral Morphology
The biological significance of IAV morphology in human clinical infections is a subject of great interest. The production of viral filaments appears to be highly inefficient by its nature, consuming anywhere from three to thirty times the amount of plasma membrane used to bud one infectious virus [51, 53]. There are several opinions on why, despite this apparent inefficiency, IAV readily produces filamentous virus in human clinical infections. As there is always a mixed population of spheres and filaments and never solely filaments, it is possible that the two morphologies are playing different roles within the host. It has been found that filament forming mutants of PR8 have higher per-molecule NA activity in vitro [66••]. In addition, NA has been shown to cleave sialic acid bonds within the mucus secreted by airway epithelial cells [67, 68] and the greater number of NA molecules (owing to a longer viral length) may serve to more efficiently clear this mucus layer. It is therefore plausible to think that the filamentous morphology is actually a marker of pathogenicity in vivo, whereby mucus in the airway is cleared by NA on filaments, thus allowing for a more efficient spread of the smaller spherical viruses [69]. This hypothesis is supported by a recent study that suggests that filaments are not released as efficiently as spheres from cells and may remain as cell-associated virions [44].
In 1998, it was shown that spherical and filamentous viruses are comparably infectious in vitro and both contain a single copy of the viral genome [53, 69–71]. However, it has recently been reported that certain subsets of filamentous virions may lack a genome [69]. Vijayakrishnan et al. (2013) reported that longer filaments were typically devoid of a copy of the viral genome, whereas shorter filaments were not. Thus, there might not be a single type of filamentous virions, but rather a range, potentially with different functions. In the tightly packed epithelial layer of the upper respiratory tract, short, cell-anchored, infectious filaments may be able to directly deliver the viral genome to neighbouring cells without the need to release and transmit a viral particle. This process may be facilitated by the more permissive use of macropinocytosis as an alternate cell entry pathway, used by filamentous IAV [72–74]. At the same time, longer, non-infectious filamentous virions may serve to thin and clear host respiratory mucus, facilitating the spread of spherical virions to neighbouring cells and to new hosts.
Conclusions
In this review, we have explored recent findings in how IAV is assembled and budded and how some of these mechanisms, especially from a cellular aspect, may influence the budding of filamentous IAV. Whilst many studies have found an effect of cellular proteins and viral protein sequences on filament formation, the causation and function of filamentous IAV remains to be fully understood. What recent data shows for certain is that IAV morphology is not solely cell or virus dependent but relies on a precise balance and interaction between the two. A single point mutation in a viral protein can alter morphology whereas silencing of a single cellular gene can also affect the ability of an IAV strain to form filamentous virions. Furthermore, a strain that forms filamentous virions in vivo will not necessarily do so in vitro or in a different host species. Ultimately, the role of filamentous IAV in human infection remains an enigma. Given the resource requirements needed to produce a single filamentous IAV as compared to a single spherical virion, it is likely that the filamentous morphology confers some advantage to the virus. Future investigations of IAV host-pathogen interactions will undoubtedly shed more light on the mechanisms of viral morphogenesis, allowing for a better understanding of the mechanisms of influenza virus budding, the functions of viral morphology and the impact of morphology on influenza disease in human clinical infections.
Footnotes
Compliance with Ethical Standards
Conflict of Interest Jeremy Rossman reports grants from Medical Research Council and grants from European Commission, during the conduct of the study.
Badham declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Recent papers of particular interest have been highlighted as:
• Of importance
•• Of major importance
- 1.Johnson NPAS, Mueller J. Updating the accounts: global mortality of the 1918-1920 ‘Spanish’ Influenza Pandemic. Bull Hist Med. 2002;76(1):105–15. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 2.Wang SQ, Du QS, Huang RB, Zhang DW, Chou KC. Insights from investigating the interaction of oseltamivir (Tamiflu) with neuraminidase of the 2009 H1N1 swine flu virus. Biochem Biophys Res Commun. 2009;386(3):432–6. doi: 10.1016/j.bbrc.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Shrestha SS, Swerdlow DL, Borse RH, Prabhu VS, Finelli L, Atkins CY, et al. Estimating the burden of 2009 pandemic influenza a (H1N1) in the United States (April 2009-April 2010) Clin Infect Dis. 2011;521(Suppl):75–82. doi: 10.1093/cid/ciq012. [DOI] [PubMed] [Google Scholar]
- 4.Lamb RA, Choppin PW. The gene structure and replication of influenza virus. Annu Rev Biochem. 1983;52:467–506. doi: 10.1146/annurev.bi.52.070183.002343. [DOI] [PubMed] [Google Scholar]
- 5.Molinari NAM, Ortega-Sanchez IR, Messonnier ML, Thompson WW, Wortley PM, Weintraub E, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–96. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Influenza data and statistics. [Online]. Available: http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/data-and-statistics.
- 7.WHO. Influenza seasonal. Geneva: Media Center; 2014. [Online]. Available: http://www.who.int/mediacentre/factsheets/fs211/en/ [Google Scholar]
- 8.Parrish CR, Murcia PR, Holmes EC. Influenza virus reservoirs and intermediate hosts: dogs, horses, and new possibilities for influenza virus exposure of humans. J Virol. 2015;89(6):2990–4. doi: 10.1128/JVI.03146-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharp GB, Kawaoka Y, Jones DJ, Bean WJ, Pryor SP, Hinshaw V, Webster RG. Coinfection of wild ducks by influenza A viruses: distribution patterns and biological significance. J Virol. 1997;71(8):6128–35. doi: 10.1128/jvi.71.8.6128-6135.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowling BJ, Jin L, Lau EHY, Liao Q, Wu P, Jiang H, et al. Comparative epidemiology of human infections with avian influenza A H7N9 and H5N1 viruses in China: a population-based study of laboratory-confirmed cases. Lancet. 2013;382(9887):129–37. doi: 10.1016/S0140-6736(13)61171-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Portela A, Digard P. The influenza virus nucleoprotein: a multifunctional RNA-binding protein pivotal to virus replication. J Gen Virol. 2002;83(4):723–34. doi: 10.1099/0022-1317-83-4-723. [DOI] [PubMed] [Google Scholar]
- 12.Elton D, Simpson-holley M, Archer K, Hallam R, Mccauley J, Digard P, et al. Interaction of the influenza virus nucleoprotein with the cellular CRM1-mediated nuclear export pathway interaction of the influenza virus nucleoprotein with the cellular CRM1-mediated nuclear export pathway. J Virol. 2001;75(1):408–19. doi: 10.1128/JVI.75.1.408-419.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weis W, Brown JH, Cusack S, Paulson JC, Skehel JJ, Wiley DC. Structure of the influenza virus haemagglutinin complexed with its receptor, sialic acid. Nature. 1988;333(6172):426–31. doi: 10.1038/333426a0. [DOI] [PubMed] [Google Scholar]
- 14.Edinger TO, Pohl MO, Stertz S. Entry of influenza A virus: host factors and antiviral targets. J Gen Virol. 2014;95(PART 2):263–77. doi: 10.1099/vir.0.059477-0. [DOI] [PubMed] [Google Scholar]
- 15.Lenten LV, Ashwell G. Studies on the chemical and enzymatic modification of glycoproteins. J Biol Chem. 1971;246(6):1889–94. [PubMed] [Google Scholar]
- 16.Kim CU, Lew W, Williams MA, Liu H, Zhang L, Swaminathan S, et al. Influenza neuraminidase inhibitors possessing a novel hydrophobic interaction in the enzyme active site: design, synthesis, and structural analysis of carbocyclic sialic acid analogues with potent anti-influenza activity. J Am Chem Soc. 1997;119(4):681–90. doi: 10.1021/ja963036t. [DOI] [PubMed] [Google Scholar]
- 17.Palese P, Tobita K, Ueda M, Compans RW. Characterization of temperature sensitive influenza virus mutants defective in neuraminidase. Virology. 1974;61(2):397–410. doi: 10.1016/0042-6822(74)90276-1. [DOI] [PubMed] [Google Scholar]
- 18.Gubareva LV. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 2004;103(1–2):199–203. doi: 10.1016/j.virusres.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 19.Lamb RA, Choppin PW. Identification of a second protein (M2) encoded by RNA segment 7 of influenza virus. Virology. 1981;112(2):729–37. doi: 10.1016/0042-6822(81)90317-2. [DOI] [PubMed] [Google Scholar]
- 20.Wharton SA, Belshe RB, Skehel JJ, Hay AJ. Role of virion M2 protein in influenza virus uncoating: specific reduction in the rate of membrane fusion between virus and liposomes by amantadine. J Gen Virol. 1994;75(4):945–8. doi: 10.1099/0022-1317-75-4-945. [DOI] [PubMed] [Google Scholar]
- 21.Helenius A. Unpacking the incoming influenza virus. Cell. 1992;69(4):577–8. doi: 10.1016/0092-8674(92)90219-3. [DOI] [PubMed] [Google Scholar]
- 22.Rossman JS, Jing X, Leser GP, Lamb RA. Influenza virus M2 protein mediates ESCRT-independent membrane scission. Cell. 2010;142(6):902–13. doi: 10.1016/j.cell.2010.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheiffele P, Rietveld A, Simons K, Wilk T. Influenza viruses select ordered lipid membrane influenza viruses select ordered lipid domains during budding from the plasma membrane. J Biol Chem. 1999;274(4):2038–2044. doi: 10.1074/jbc.274.4.2038. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J, Pekosz A, Lamb RA. Influenza virus assembly and lipid raft microdomains: a role for the cytoplasmic tails of the spike glycoproteins. J Virol. 2000;74(10):4634–44. doi: 10.1128/jvi.74.10.4634-4644.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen BJ, Leser GP, Morita E, Lamb RA. Influenza virus hemagglutinin and neuraminidase, but not the matrix protein, are required for assembly and budding of plasmid-derived virus-like particles. J Virol. 2007;81(13):7111–23. doi: 10.1128/JVI.00361-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26••.Chlanda P, Schraidt O, Kummer S, Riches J, Oberwinkler H, Prinz S, et al. Structural analysis of the roles of influenza A virus membrane-associated proteins in assembly and morphology. J Virol. 2015;89(17):8957–66. doi: 10.1128/JVI.00592-15. [An investigation of the individual and cumulative roles of HA, NA and M1 in driving VLP budding and viral morphogenesis.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmidt NW, Mishra A, Wang J, Degrado WF, Wong GCL. Influenza virus A M2 protein generates negative gaussian membrane curvature necessary for budding and scission. J Am Chem Soc. 2013;135(37):13710–9. doi: 10.1021/ja400146z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choppin PW, Murphy JS, Tamm I. Studies of two kinds of virus particles which comprise influenza A2 virus strains. III. Morphological characteristics: independence to morphological and functional traits. J Exp Med. 1960;112(18):945–52. doi: 10.1084/jem.112.5.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chu CM, Dawson IM, Elford WJ. Filamentous forms associated with newly isolated influenza virus. Lancet. 1949;1(6554):602. doi: 10.1016/s0140-6736(49)91699-2. [DOI] [PubMed] [Google Scholar]
- 30.Elton D, Bruce EA, Bryant N, Wise HM, Macrae S, Rash A, et al. The genetics of virus particle shape in equine influenza A virus. Influenza Other Respi Viruses. 2013;7(Suppl4):81–9. doi: 10.1111/irv.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Itoh Y, Shinya K, Kiso M, Watanabe T, Sakoda Y, Hatta M, et al. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature. 2009;460(7258):1021–5. doi: 10.1038/nature08260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hayase S, Uno Y, Nii F. Ultrahigh-resolution scanning electron microscopy of MDCK cells infected with influenza viruses. J Electron Microsc (Tokyo) 1995;44:281–8. [PubMed] [Google Scholar]
- 33.Kilbourne ED, Murphy JS. Genetic studies of Influenza Virus. I. Viral morphology and growth capacity as exchangable genetic traits. Rapid in ovo adaptation of early passage Asian strain isolates by combination with PR8. J Exp Med. 1960;111:387–406. doi: 10.1084/jem.111.3.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lang G, Narayan O, Rouse BT, Ferguson AE, Connell MC. A new influenza A virus infection in turkeys II. A highly pathogenic variant, a/turkey/ontario 772/66. Can Vet J. 1968;9(7):151–160. [PMC free article] [PubMed] [Google Scholar]
- 35••.Seladi-Schulman J, Steel J, Lowen AC. Spherical influenza viruses have a fitness advantage in embryonated eggs, while filament-producing strains are selected in vivo. J Virol. 2013;87(24):13343–53. doi: 10.1128/JVI.02004-13. [Demonstration of the morphological changes that occur in influenza viruses during in vivo adaptation to both embryonated chicken eggs and guinea pigs.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shortridge KF, Zhou NN, Guan Y, Gao P, Ito T, Kawaoka Y, et al. Characterization of avian H5N1 influenza viruses from poultry in Hong Kong. Virology. 1998;252(2):331–42. doi: 10.1006/viro.1998.9488. [DOI] [PubMed] [Google Scholar]
- 37.Basu A, Shelke V, Chadha M, Kadam D, Sangle S, Gangodkar S, et al. Direct imaging of pH1N1 2009 influenza virus replication in alveolar pneumocytes in fatal cases by transmission electron microscopy. J Electron Microsc (Tokyo) 2011;60(1):89–93. doi: 10.1093/jmicro/dfq081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kilbourne ED. Studies on influenza in the pandemic of 1957-1958. III. Isolation of influenza A (Asian strain) viruses from influenza patients with pulmonary complications; details of virus isolation and characterization of isolates, with quantitative comparison of isol. J Clin Invest. 1959;38(1 Part 2):266–74. doi: 10.1172/JCI103792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zebedee SL, Lamb RA. Influenza A virus M2 protein: monoclonal antibody restriction of virus growth and detection of M2 in virions. J Virol. 1988;62(8):2762–72. doi: 10.1128/jvi.62.8.2762-2772.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zebedee SL, Lamb RA. Growth restriction of influenza A virus by M2 protein antibody is genetically linked to the M1 protein. Proc Natl Acad Sci. 1989;86(3):1061–5. doi: 10.1073/pnas.86.3.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roberts PC, Lamb RA, Compans RW. The M1 and M2 proteins of influenza A virus are important determinants in filamentous particle formation. Virology. 1998;240(1):127–37. doi: 10.1006/viro.1997.8916. [DOI] [PubMed] [Google Scholar]
- 42.Elleman CJ, Barclay WS. The M1 matrix protein controls the filamentous phenotype of influenza A virus. Virology. 2004;321(1):144–53. doi: 10.1016/j.virol.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 43.Bourmakina SV, García-Sastre A. Reverse genetics studies on the filamentous morphology of influenza A virus. J Gen Virol. 2003;84(3):517–27. doi: 10.1099/vir.0.18803-0. [DOI] [PubMed] [Google Scholar]
- 44.Gómez-Puertas P, Albo C, Pérez-Pastrana E, Vivo A, Portela A. Influenza virus matrix protein is the major driving force in virus budding. J Virol. 2000;74(24):11538–47. doi: 10.1128/jvi.74.24.11538-11547.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fujiyoshi Y, Kume NP, Sakata K, Sato SB. Fine structure of influenza A virus observed by electron cryo-microscopy. EMBO J. 1994;13(2):318–26. doi: 10.1002/j.1460-2075.1994.tb06264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nayak DP, Hui EKW, Barman S. Assembly and budding of influenza virus. Virus Res. 2004;106(2):147–65. doi: 10.1016/j.virusres.2004.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rossman JS, Jing X, Leser GP, Balannik V, Pinto LH, Lamb RA. Influenza virus M2 ion channel protein is necessary for filamentous virion formation. J Virol. 2010;84(10):5078–88. doi: 10.1128/JVI.00119-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCown MF, Pekosz A. Distinct domains of the influenza a virus M2 protein cytoplasmic tail mediate binding to the M1 protein and facilitate infectious virus production. J Virol. 2006;80(16):8178–89. doi: 10.1128/JVI.00627-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beale R, Wise H, Stuart A, Ravenhill BJ, Digard P, Randow F. A LC3-interacting motif in the influenza A virus M2 protein is required to subvert autophagy and maintain virion stability. Cell Host Microbe. 2014;15(2):239–47. doi: 10.1016/j.chom.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grantham ML, Stewart SM, Lalime EN, Pekosz A. Tyrosines in the influenza A virus M2 protein cytoplasmic tail are critical for production of infectious virus particles. J Virol. 2010;84(17):8765–76. doi: 10.1128/JVI.00853-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mosley VM, Wyckoff RWG. Electron micrography of the virus of influenza. Nature. 1946;157(3983):263–3. doi: 10.1038/157263a0. [DOI] [PubMed] [Google Scholar]
- 52.Burnet FM, Lind PE. Studies on filamentary forms of influenza virus with special reference to the use of dark-ground-microscopy. Arch Gesamte Virusforsch. 1957;7(5):413–28. doi: 10.1007/BF01241959. [DOI] [PubMed] [Google Scholar]
- 53.Roberts PC, Compans RW. Host cell dependence of viral morphology. Proc Natl Acad Sci U S A. 1998;95(10):5746–51. doi: 10.1073/pnas.95.10.5746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bruce EA, Medcalf L, Crump CM, Noton SL, Stuart AD, Wise HM, et al. Budding of filamentous and non-filamentous influenza A virus occurs via a VPS4 and VPS28-independent pathway. Virology. 2009;390(2):268–78. doi: 10.1016/j.virol.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 55.Bruce EA, Digard P, Stuart AD. The Rab11 pathway is required for influenza A virus budding and filament formation. J Virol. 2010;84(12):5848–59. doi: 10.1128/JVI.00307-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ullrich O, Reinsch S, Urbé S, Zerial M, Parton RG. Rab11 regulates recycling through the pericentriolar recycling endosome. J Cell Biol. 1996;135(4):913–24. doi: 10.1083/jcb.135.4.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hales CM, Griner R, Hobdy-Henderson KC, Dorn MC, Hardy D, Kumar R, et al. Identification and characterization of a family of Rab11-interacting proteins. J Biol Chem. 2001;276(42):39067–75. doi: 10.1074/jbc.M104831200. [DOI] [PubMed] [Google Scholar]
- 58.Hales CM, Vaerman JP, Goldenring JR. Rab11 family interacting protein 2 associates with myosin Vb and regulates plasma membrane recycling. J Biol Chem. 2002;277(52):50415–21. doi: 10.1074/jbc.M209270200. [DOI] [PubMed] [Google Scholar]
- 59.Schonteich E, Wilson GM, Burden J, Hopkins CR, Anderson K, Goldenring JR, et al. The Rip11/Rab11-FIP5 and kinesin II complex regulates endocytic protein recycling. J Cell Sci. 2008;121(Pt 22):3824–33. doi: 10.1242/jcs.032441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wilson GM. The FIP3-Rab11 protein complex regulates recycling endosome targeting to the cleavage furrow during late cytokinesis. Mol Biol Cell. 2004;16(2):849–60. doi: 10.1091/mbc.E04-10-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ying Chou Y, Heaton NS, Gao Q, Palese P, Singer R, Lionnet T. Colocalization of different influenza viral RNA segments in the cytoplasm before viral budding as shown by single-molecule sensitivity FISH analysis. PLoS Pathog. 2013;9(5) doi: 10.1371/journal.ppat.1003358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62•.Amorim MJ, Bruce EA, Read EKC, Foeglein A, Mahen R, Stuart AD, et al. A Rab11- and microtubule-dependent mechanism for cytoplasmic transport of influenza A virus viral RNA. J Virol. 2011;85(9):4143–56. doi: 10.1128/JVI.02606-10. [The report demonstrates that the cellular microtubule network is used by IAV, whereby the viral RNP/PB2 complex interacts with Rab11 for transport to the site of viral assembly.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eisfeld AJ, Neumann G, Kawaoka Y. At the centre: influenza A virus ribonucleoproteins. Nat Rev Microbiol. 2014;13(1):28–41. doi: 10.1038/nrmicro3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shaw ML, Stone KL, Colangelo CM, Gulcicek EE, Palese P. Cellular proteins in influenza virus particles. PLoS Pathog. 2008;4(6):1–13. doi: 10.1371/journal.ppat.1000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martin K, Helenius A. Nuclear transport of influenza virus ribonucleoproteins: the viral matrix protein (M1) promotes export and inhibits import. Cell. 1991;67:117–30. doi: 10.1016/0092-8674(91)90576-k. [DOI] [PubMed] [Google Scholar]
- 66••.Seladi-Schulman J, Campbell PJ, Suppiah S, Steel J, Lowen AC. Filament-producing mutants of influenza A/Puerto Rico/ 8/1934 (H1N1) virus have higher neuraminidase activities than the spherical wild-type. PLoS One. 2014;9(11):1–10. doi: 10.1371/journal.pone.0112462. [In direct relevance to clinical infections, this report shows that filamentous viruses have increased neuraminidase activity. This higher enzymatic activity gained from the morphological change may support a mucus clearing hypothesis for the function of filamentous viruses.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cohen M, Zhang X-Q, Senaati HP, Chen H-W, Varki NM, Schooley RT, et al. Influenza A penetrates host mucus by cleaving sialic acids with neuraminidase. Virol J. 2013;10:321. doi: 10.1186/1743-422X-10-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yang X, Steukers L, Forier K, Xiong R, Braeckmans K, Van Reeth K, et al. A beneficiary role for neuraminidase in influenza virus penetration through the respiratory mucus. PLoS One. 2014;9(10):1–11. doi: 10.1371/journal.pone.0110026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vijayakrishnan S, Loney C, Jackson D, Suphamungmee W, Rixon FJ, Bhella D. Cryotomography of budding influenza Avirus reveals filaments with diverse morphologies that mostly do not bear a genome at their distal end. PLoS Pathog. 2013;9(6) doi: 10.1371/journal.ppat.1003413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Noda T, Sagara H, Yen A, Takada A, Kida H, Cheng RH, et al. Architecture of ribonucleoprotein complexes in influenza A virus particles. Nature. 2006;439(7075):490–2. doi: 10.1038/nature04378. [DOI] [PubMed] [Google Scholar]
- 71.Calder LJ, Wasilewski S, Berriman JA, Rosenthal PB. Structural organization of a filamentous influenza A virus. Proc Natl Acad Sci U S A. 2010;107(23):10685–90. doi: 10.1073/pnas.1002123107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sieczkarski SB, Whittaker GR. Characterization of the host cell entry of filamentous influenza virus. Arch Virol. 2005;150(9):1783–96. doi: 10.1007/s00705-005-0558-1. [DOI] [PubMed] [Google Scholar]
- 73.de Vries E, Tscherne DM, Wienholts MJ, Cobos-Jiménez V, Scholte F, García-Sastre A, et al. Dissection of the influenza Avirus endocytic routes reveals macropinocytosis as an alternative entry pathway. PLoS Pathog. 2011;7(3):e1001329. doi: 10.1371/journal.ppat.1001329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rossman JS, Leser GP, Lamb RA. Filamentous influenza virus enters cells via macropinocytosis. J Virol. 2012;86(20):10950–60. doi: 10.1128/JVI.05992-11. [DOI] [PMC free article] [PubMed] [Google Scholar]