Abstract
Purpose
To evaluate the efficacy of intramedullary Kirschner wires for the treatment of unstable tibial shaft fractures in children.
Methods
This prospective study was conducted at the Department of Orthopaedic Surgery in Maharishi Markandeshwar Medical College from June 2005 to June 2010. Sixty-six children having closed fracture of the tibial shaft with a mean age of 7.7 years (range, 2–14 years) were recruited from emergency and outpatient department. They were treated with percutaneous intramedullary Kirschner wires. The clinical results of our study were rated on the basis of the criteria of union, nonunion, delayed union or malunion. All children were followed for one year.
Results
Children achieved union in a mean time of 8 weeks (range, 6–10 weeks). Postoperatively, three children (4.55%) had delayed union, one (1.52%) valgus deformity of lower leg, three (4.55%) postoperative knee pain and twelve (18.18%) skin irritation at pin site. Wires were removed after 8–22 weeks without any complications. No patient was lost to follow-up. The results were excellent in 95.45% and good in 4.55% children.
Conclusion
This technique is cost-effective, simple, quick to perform, safe and reliable and avoids prolonged hospitalization with good results.
Keywords: Kirschner wires, Tibial shaft fractures, Children
Introduction
Tibial shaft fractures are common injuries in children1; however, very few require surgical stabilization.2, 3 Surgical stabilization may be indicated for children in whom acceptable positioning is not maintained after closed reduction, and those who are ten years of age and older.4 Tibial shaft fractures requiring surgical stabilization are treated differently in children compared with adults. Locking intramedullary rods are not used in children because of the risk of physeal injury. Treatment options include external fixation,5, 6 elastic stable intramedullary nailing,7, 8 and transfixion pins and casts.9, 10 Intramedullary fixation with elastic nails that is placed percutaneously through the distal femoral metaphysis without violating the physis has become a popular technique for the treatment of femoral fractures in children.11, 12 Two flexible intramedullary nails, introduced in an antegrade or retrograde fashion, cross the fracture site and act as internal splints to maintain length and alignment while allowing sufficient fracture motion to generate callus formation. This technique is commonly referred to as elastic stable intramedullary nailing or flexible intramedullary nailing.8 It has been used successfully for the treatment of paediatric fractures of the tibia, femur, humerus and forearm.13, 14, 15 Compared with titanium nails, Kirschner wires (K-wires) with the low cost, universal availability and the short hospital stay are cost effective and particularly suitable for developing and underdeveloped countries. The present study was to evaluate the efficacy of intramedullary K-wires for the treatment of tibial shaft fractures in children.
Materials and methods
This prospective study was carried out at Department of Orthopaedic Surgery, Maharishi Markandeshwar Medical College from June 2005 to June 2010. Institutional medical ethics committee approved it. Sixty-six children with a mean age of 7.7 years (range, 2–14 years) having closed unstable fracture of tibial shaft were included in present study. All children were given above knee plaster slab prior to operation and preanaesthetic check-up was done.
Inclusion and exclusion criteria
The inclusion criteria were: displaced fractures; multiple fractures which were found to be unstable in closed reduction; fractures displaced in traction; fractures in patients with polytrauma and under intensive care to facilitate nursing; Irritable patients with brain injury.
The exclusion criteria were: undisplaced fractures and fractures in a good position treated by traction and plaster; age less than two years and more than fourteen years; open fractures; fractures requiring open reduction; nonunited fractures.
The goal of this study was to provide rapid healing of the fracture in a correct position, ease of nursing care and early mobilisation. A written informed consent was obtained from the parents of the children. They were followed up after surgery, and were clinically and radiologically assessed for fracture healing, joint movements and implant failure. According to the criteria the results were graded as excellent when the fractures united within 10 weeks (clinically and radiologically) without any complications, good when union occurred within 16 weeks with treatable complications like superficial infection and knee stiffness and poor when union occurred before or after 16 weeks with one or more permanent complications like deep infection, implant failure, nonunion, limb shortening and permanent knee stiffness. Delayed union was recorded when the fracture united in more than two to four months (radiograph showed external callus traversed by a zone of radiolucency, a typical picture of fibrocartilaginous delayed union). Nonunion was noted when union had not occurred following six months of treatment. Follow-up was done for one year. In majority of the patients, percutaneous K-wire fixation of the tibia was performed within one week of the injury.
Operative technique
All children were operated upon under general anaesthesia. The affected limb was cleaned and draped. The appropriate diameter of the wires depended on the size of the medullary canal of the child. The size of the implant is selected to be approximately 40% of the diameter of the medullary canal at the level of isthmus, and two equally sized implants are used to prevent asymmetric force on opposite cortices.
Two stainless steel K-wires of 30–45 cm in length and 2.5–3.5 mm in diameter were prepared by bending them at an approximate angle of 45°, 2 cm from the tip and cutting off the sharp points to prevent inadvertent penetration of the cortex. The wires were not pre-bent in a “C” or “S” curve. The wires were loaded onto a “T” handled introducer with a Jacob's chuck. Two small skin incisions were made distal to the proximal growth plate of tibia, one anterolaterally and the other anteromedially. Entry portals were made into the proximal tibial metaphysis distal to the growth plate of the proximal tibia with a sharp bone awl anterolaterally and anteromedially. The wires were introduced via antegrade approach by hand or gentle hammering. The lateral wire was introduced first. The tips of the wire were placed just proximal to the growth plates of the distal tibia, with the bends pointing towards the side of the entry portal. Angular and rotational malalignment spontaneously correct on passage of the wires across the fracture. Image intensifier screening in two planes perpendicular to each other confirmed proper placements of the wires. The tail portions of the wires were bent towards the fracture and cut 1 cm away from the entry portal in the cortex. The skin wounds were sutured and dressed. Fracture stability, correct linear and rotational alignment were assessed on table. All children had received a preoperative bolus of intravenous antibiotic. Retrograde medullary Kirschner wiring was carried out in one small child with a single intramedullary K-wires. The entry portal was on the lateral cortex proximal to the growth plate of the distal tibia. Above knee slab supplementations were done in the immediate postoperative period for a period of four to six weeks. Sutures were removed on the 10th day after surgery, and then all the patients were mobilised, non-weight-bearing for 4–6 weeks. Weight bearing in a walking plaster was permitted when adequate callus was seen at the fracture site.
Evaluations on follow-up were done according to a fixed protocol. The children were followed up at 2 weeks, 6 weeks, 12 weeks, 6 months and 12 months. The time to weight bearing and to union were recorded, as well as the range of knee motion and limb length discrepancy. Union was defined radiographically when bridging callus was visible on two standard views with partial obliteration of the fracture line, and clinically when bony tenderness and pain on weight bearing were absent. Any differences in the limb length were measured, keeping both lower limbs in identical position (with pelvis squared) and measuring the distance from the anterior superior iliac spine to the inferior tip of the medial malleolus. Rotational deformity and any significant varus or valgus angulations at the fracture site were measured radiologically. Fractures were considered to be united when tricortical callus was visible on the radiographs and there was no tenderness at the fracture site on clinical examination. Generally, sufficient callus formation is shown at 4 weeks in paediatric fractures, and radiological fracture consolidation has been reported to be achieved at 7–8 weeks.
Follow-up
The children were started on non-weight-bearing crutch walking and knee physiotherapy 2–3 days after the surgery and were ready for discharge 3–4 days after surgery. The children with polytrauma stayed on for a longer period in the hospital because of associated injuries. Full weight-bearing was allowed after clinicoradiological fracture union. Union was defined clinically by the absence of bony tenderness and abnormal mobility at the fracture site, and no pain at the fracture site on weight bearing. Radiological fracture union was defined by the presence of callus bridging the fracture and partial obliteration of the fracture line in two views perpendicular to each other. The clinical results of our study were rated on the basis of the criteria of union, nonunion, delayed union or malunion.16 The children were assessed for malunion both linear and rotational, and limb length discrepancy. The wires were removed between 8 and 22 weeks. These children were assessed clinically and radiologically for union timing at one year following surgery. Children were assessed for delayed union (more than two to four months postoperative) and nonunion (six months following surgery).17 Functional outcomes were evaluated according to the Johner and Wruhs criteria.16 As a part of the subjective assessment, patients were asked in questionnaire if they were very satisfied, satisfied or not satisfied with the outcome of treatment.
Results
Totally, 66 children with the age of 2–14 years were included in this study, and among them 40 were girls and 26 were boys. There were 30 left-sided and 36 right-sided fractures. Forty-two children suffered a road traffic accident and twenty-four had a fall from a height. All were closed fractures. There were transverse fractures in 45 children, oblique in 8, spiral in 5, comminuted in 7 and segmental in 1; fractures were at middle one third in 42 children (30 boys and 12 girls), proximal one third in 11 (7 boys and 4 girls) and distal one third in 13 (3 boys and 10 girls) of tibia. Out of 66 children, 55 had isolated tibial shaft fractures and 11 had associated injuries. Two children had ipsilateral forearm fractures, one ipsilateral femoral fracture, two contralateral femoral fractures, two contralateral forearm fractures, two ipsilateral and one contralateral humeral fractures and one child had head injury. All children were followed up for one year. None was lost to follow-up. The clinical results of our study were based on the criteria of union, nonunion, delayed union or malunion.17 Functional outcomes were evaluated according to the Johner and Wruhs criteria.16 The children were followed up according to their clinical status. Sixty-three patients had union within ten weeks. Union was achieved in three children in sixteen weeks. One child had valgus deformity in lower tibia more than 5° however child had no difficulty in walking.
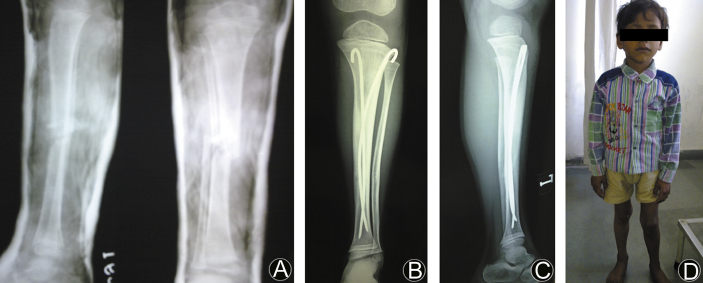
Children were allowed to start walking with crutches on the second day of operation, as they feel comfortable. All children, except two, started partial weight-bearing on the 6th week and full weight-bearing on the 12th week. These children had non-weight-bearing ambulation until the callus became visible on radiographs. They had comminution at fracture site. All children had full range of motion of their knees and ankles. Three children complained postoperative knee pain, which was spontaneously resolved in two weeks. None of the children in our series developed migration or sinking of the intramedullary wires. Skin irritation by the protruding wire ends was encountered in 12 patients. In the majority of cases, we noted that the alignment achieved intraoperatively was maintained at the time of the final review. However, two patients with significant communition had some progression of deformity. No patient had any rotational deformity. Limb lengthening of less than 1.5 cm was found in 3 cases both clinically and radiologically, which was clinically insignificant. In our study, there were three (4.55%) delayed unions which were corrected within three weeks. K-wires were removed between 8 and 22 weeks. The results were excellent in 95.45% and good in 4.55% children. In subjective overall assessment 95.45% patients were fully satisfied and 4.55% were satisfied with the outcome of treatment (Fig. 1).
Fig. 1.
A: Preoperative anteroposterior and lateral radiographs of tibial shaft fracture (left side) in a five years old child. B and C: Postoperative anteroposterior and lateral radiographs showing fixation with two Kirschner wires. D: Photograph of the child at final follow-up of one year.
Discussion
Diaphyseal tibial fracture is the second most frequent traumatic injury in children requiring hospitalization.18 Clinical results are good; whichever treatment method is chosen but age is a consideration to define the best treatment.19, 20, 21, 22, 23, 24, 25 Closed reduction and plaster application is still the gold standard for tibial fractures in children. However, this procedure requires prolonged immobilization and cautious follow-up. Secondary displacement and nonalignment are not exceptional, particularly in cases of isolated tibial fracture.26 In order to avoid these complications, operative treatment can be performed. Elastic stable intramedullary nailing is the gold standard for osteosynthesis of unstable diaphyseal fractures in children and adolescents.20, 27 In tibial fractures, indications for operative treatment are determined based on a variety of factors including fracture type, location, severity and patient age.22, 28 The encouraging results of elastic stable intramedullary nailing in femoral and forearm fractures led us to use this technique to treat tibial shaft fractures.29, 30 There are various advantages of this technique. Three-point fixation within the medullary canal allows maintenance of both alignment and rotation for most fractures. Flexible intramedullary nails provide fixation that is stable as well as elastic, allowing micromotion at the fracture site when load is applied. This encourages abundant bridging callus formation and facilitates early union.7, 9 Based on the concept of flexible intramedullary nails. Some authors recently advocated the use of intramedullary K-wires fixation for femoral fractures in children with encouraging results.31, 32 Nascimento et al33 advocated flexible titanium nailing for the treatment of all diaphyseal fractures in children. The functional outcomes for the intramedullary nailing group were significantly better than those for the external fixation group in the categories of pain, happiness, sports, and global function.5 In this study, 63 patients underwent union in 6–10 weeks with a mean of 8 weeks. The principle of osteosynthesis with intramedullary K-wires is a biomechanical idea that aims at early bridging callus formation leading to rapid restoration of bony continuity.33 Just like the titanium nails, the flexible K-wires allow controlled oscillating micro movements that permit changing compression on different parts of the fracture line, leading to early external callus formation. Each K-wire provides three points of fixation: one at the entry point, a second at the apex of the curve of the K-wire and a third at the tip, which is embedded in the cancellous bone of the proximal metaphysis. Stability is provided not only by the intramedullary K-wires, but also by the bone itself and surrounding soft tissues.8, 34, 35, 36 The bone provides axial stability and each wire provides three point fixations. The bent tips provide rotational stability. Increasing the number of K-wires enhances the stability of fixation.8, 34, 35, 36 Kiely et al tested the mechanical properties of different combinations of flexible nails in a model of a paediatric femoral fracture. They found no difference in the mechanical properties of paired straight, “S” shaped and “C” shaped nails. Zachert et al37 advocated that for in vitro adolescent femoral spiral fracture model, the stability of elastic stable intramedullary nailing could be significantly improved by two modifications with additional tension screws. Griffet's study38 involved 86 children (average age 11.8 years). As early as day 30, all patients had normal knee mobility and symmetrical foot progress angle. At 2-year follow-up, frontal angulations and leg length discrepancy had decreased and affected 2% of patients. Four patients suffered from superficial infections. There were no cases of osteomyelitis or refracture. Swamy39 stated that 14 children (11 boys and three girls with age of 5–12 years) were treated with stainless steel K-wires as an intramedullary device in the treatment of paediatric femoral shaft fractures. Intramedullary K-wire fixation has a place in the management of paediatric diaphyseal femoral fractures, because it is technically simple, quick to perform, safe and reliable and avoids prolonged hospitalization. However, cautious attention to surgical technique is of paramount importance. It is less rigid than the titanium elastic nails but in the absence of the latter, it affords a cheap and easily available method of osteosynthesis. In our series, three complained postoperative knee pain, which was spontaneously resolved in two weeks. None of the patients in our series developed migration or sinking of the intramedullary wires. In 12 cases, we encountered skin irritation by protruding wire ends at the entry point. Cutting the wires close to the bone and hairpin bend of the wire ends minimised this problem. There were three cases of delayed unions, which were corrected within three weeks. Distal tibia has smaller growth potential and muscle traction distribution is a cause of the valgus deformity of the distal tibia. Valgus deformity of distal tibia more than 5°, which is not acceptable was seen in one case of my study. Percutaneous K-wire fixation for tibial shaft fractures in children has distinct advantages over other conservative and over other operative techniques. The low cost and universal availability of K-wires as compared to titanium nails and the short hospital stay make this treatment cost effective and particularly suitable for developing and underdeveloped countries. This is a simple technique, and sophisticated instrumentation is not required. This is a minimally invasive technique with small stab incisions at the entry point. The amount of blood loss is small as compared to plating.32 Cosmetic damage is minimal as compared to other open techniques like plating. In contrast with the plaster immobilization, it affords advantages of easy nursing care, early mobilization and avoidance of psychological problems due to prolonged immobilization.8, 34, 35, 36 As the children are mobilized early on axillary crutches, they can return to school and play activities earlier. This technique is of considerable value in head injury and comatose patients, when compared to traction or a plaster immobilization. Percutaneous K-wire fixation is a biological method of fixation, which provides a combination of elastic stability and mobility. Closed methods leave the fracture haematoma intact, leading to the formation of early bridging callus. This is an easy to learn technique, with a small learning curve. It may be adapted to treat other diaphyseal fractures in children.8, 34, 35, 36
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Tafazal S., Madan S.S., Ali F. Management of paediatric tibial fractures using two types of circular external fixator: Taylor spatial frame and Ilizarov circular fixator. J Child Orthop. 2014;8:273–279. doi: 10.1007/s11832-014-0583-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.EL Hajj F., Sebaaly A., Kharrat K. Osteochondritis of the distal tibial epiphysis. Case Rep Med. 2012;2012:629150. doi: 10.1155/2012/629150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schulz J., Moor M., Roocroft J. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Jt Surg Am. 2013;95:1159–1165. doi: 10.2106/JBJS.L.01390. [DOI] [PubMed] [Google Scholar]
- 4.Onta P.R., Thapa P., Sapkota K. Outcome of diaphyseal fracture of tibia treated with flexible intramedullary nailing in pediatrics age group; a prospective study. Am J Public Health. 2015;3:65–68. [Google Scholar]
- 5.Jung S.T., Park H., Lee J.H., Kim J.R. Residual angulation of distal tibial diaphyseal fractures in children younger than ten years. J Orthop Surg Res. 2014;9:84. doi: 10.1186/s13018-014-0084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kong H., Sabharwal S. External fixation for closed pediatric femoral shaft fractures: where are we now? Clin Orthop Relat Res. 2014;472:3814–3822. doi: 10.1007/s11999-014-3554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karaman I., Halici M., Kafadar I.H. Mid-term results of the elastic intramedullary nailing in paediatric long bone shaft fractures: a prospective study of 102 cases. J Pediatr Orthop B. 2014;23:212–220. doi: 10.1097/01.bpb.0000444460.95927.05. [DOI] [PubMed] [Google Scholar]
- 8.Choudhari P., Chhabra S., Kiyawat V. Evaluation of results of titanium elastic nailing system in paediatric lower extremity fractures of long bones. J Evol Med Dent Sci. 2014;3:15303–15309. [Google Scholar]
- 9.Zarad A.L. Flexible intramedullary nails for unstable fractures of the tibia in children: a retrospective evaluation of effectiveness. Egypt Orthop J. 2014;49:281. [Google Scholar]
- 10.Sisodia G.B., Scott B. Common lower limb injuries in children. Surg Oxf. 2014;32:17–23. [Google Scholar]
- 11.Kaiser M.M., Zachert G., Wendlandt R. Increasing stability by pre-bending the nails in elastic stable intramedullary nailing: a biomechanical analysis of a synthetic femoral spiral fracture model. J Bone Jt Surg Br. 2012;94:713–718. doi: 10.1302/0301-620X.94B5.28247. [DOI] [PubMed] [Google Scholar]
- 12.Nisar A., Bhosale A., Madan S.S. Complications of elastic stable intramedullary nailing for treating paediatric long bone fractures. J Orthop. 2013;10:17–24. doi: 10.1016/j.jor.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim Y.I., Kang H.G., Kim T.S. Palliative percutaneous stabilization of lower extremity for bone metastasis using flexible nails and bone cement. Surg Oncol. 2014;23:192–198. doi: 10.1016/j.suronc.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Lascombes P., Huber H., Fay R. Flexible intramedullary nailing in children: nail to medullary canal diameters optimal ratio. J Pediatr Orthop. 2013;33:403–408. doi: 10.1097/BPO.0b013e318285c54d. [DOI] [PubMed] [Google Scholar]
- 15.Atef A., El Tantawy A. Open unstable metaphyseo-diaphyseal fractures of the tibia in adolescents: treatment by flexible intramedullary nails augmented by external fixator. Int Orthop. 2015;39:921–926. doi: 10.1007/s00264-015-2700-3. [DOI] [PubMed] [Google Scholar]
- 16.Johner R., Wruhs O. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin Orthop Relat Res. 1983;178:7–25. [PubMed] [Google Scholar]
- 17.Sahu R.L. Percutaneous Kirschner wire (K-wire) fixation for humerus shaft fractures in children: a treatment concept. Niger Med J. 2013;54:356–360. doi: 10.4103/0300-1652.122375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pandya N.K., Edmonds E.W. Immediate intramedullary flexible nailing of open pediatric tibial shaft fractures. J Pediatr Orthop. 2012;32:770–776. doi: 10.1097/BPO.0b013e318270468b. [DOI] [PubMed] [Google Scholar]
- 19.Gordon J.E., O'Donnell J.C. Tibia fractures: what should be fixed? J Pediatr Orthop. 2012;32(Suppl. 1):S52–S61. doi: 10.1097/BPO.0b013e318254c7be. [DOI] [PubMed] [Google Scholar]
- 20.Lascombes P., Steiger C., Gonzalez A. Trente-cinq années d’embrochage centro médullaire élastique stable (ECMES) dans les fractures de l’enfant: une méthode toujours jeune. e-Mémoires l'Académie Natl Chir. 2015;14:109–114. [Google Scholar]
- 21.Lascombes P. Flexible intramedullary nailing (FIN) in diaphyseal fractures in children. In: Bentley G., editor. European Surgical Orthopaedics and Traumatology: The EFORT Textbook. Springer-Verlag; Berlin: 2014. pp. 4669–4689. [Google Scholar]
- 22.Economedes D.M., Abzug J.M., Paryavi E. Outcomes using titanium elastic nails for open and closed pediatric tibia fractures. Orthopedics. 2014;37:e619–624. doi: 10.3928/01477447-20140626-52. [DOI] [PubMed] [Google Scholar]
- 23.Lardelli P., Frech-Dörfler M., Holland-Cunz S. Slow recovery of weight bearing after stabilization of long-bone fractures using elastic stable intramedullary nails in children. Med Baltim. 2016;95:e2966. doi: 10.1097/MD.0000000000002966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palmu S.A., Auro S., Lohman M. Tibial fractures in children. A retrospective 27-year follow-up study. Acta Orthop. 2014;85:513–517. doi: 10.3109/17453674.2014.916489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ozkul E., Gem M., ArslAn H. How safe is titanium elastic nail application in the surgical treatment of tibia fractures in children? Acta Orthop Belg. 2014;80:76–81. [PubMed] [Google Scholar]
- 26.Shore B.J., Glotzbecker M.P., Zurakowski D. Acute compartment syndrome in children and teenagers with tibial shaft fractures: incidence and multivariable risk factors. J Orthop Trauma. 2013;27:616–621. doi: 10.1097/BOT.0b013e31828f949c. [DOI] [PubMed] [Google Scholar]
- 27.de Billy B., Gindraux F., Langlais J. Osteotomy and fracture fixation in children and teenagers. Orthop Traumatol Surg Res. 2014;100(1 Suppl):S139–S148. doi: 10.1016/j.otsr.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 28.Nau C., Marzi I., Ziebarth K. Springer; London: 2015. Fractures in Children and Adolescents; pp. 395–417. [Google Scholar]
- 29.Parikh S.N., Jain V.V., Denning J. Complications of elastic stable intramedullary nailing in pediatric fracture management: AAOS exhibit selection. J Bone Jt Surg Am. 2012;94:e184. doi: 10.2106/JBJS.L.00668. [DOI] [PubMed] [Google Scholar]
- 30.Khan A., Athlani L., Rousset M. Functional results of displaced proximal humerus fractures in children treated by elastic stable intramedullary nail. Eur J Orthop Surg Traumatol. 2014;24:165–172. doi: 10.1007/s00590-013-1177-2. [DOI] [PubMed] [Google Scholar]
- 31.Sahu R.L. Percutaneous K-wire fixation for femur shaft fractures in children: a treatment concepts for developing countries. Ann Med Health Sci Res. 2013;3:197–201. doi: 10.4103/2141-9248.113661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jain A., Aggarwal A., Gulati D., Singh M.P. Controversies in orthopaedic trauma-management of fractures of shaft of femur in children between 6 and 12 years of age. Kathmandu Univ Med J. 2014;12:77–84. doi: 10.3126/kumj.v12i1.13647. [DOI] [PubMed] [Google Scholar]
- 33.Nascimento F.P., Santili C., Akkari M. Flexible intramedullary nails with traction versus plaster cast for treating femoral shaft fractures in children: comparative retrospective study. Sao Paulo Med J. 2013;131:5–12. doi: 10.1590/S1516-31802013000100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yaokreh J.B., Odéhouri-Koudou T.H., Koffi K.M. Surgical treatment of femoral diaphyseal fractures in children using elastic stable intramedullary nailing by open reduction at Yopougon Teaching Hospital. Orthop Traumatol Surg Res. 2015;101:589–592. doi: 10.1016/j.otsr.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 35.Stammers J., Barry M. Paediatric femoral fractures. In: Aresti N.A., Barry M., editors. Paediatric Orthopaedic Trauma in Clinical Practice. Springer; London: 2015. pp. 89–103. [Google Scholar]
- 36.Kumar S., Anand T., Singh S. Comparative study using intramedullary K-wire fixation over titanium elastic nail in paediatric shaft femur fractures. J Clin Diagn Res. 2014;8:LC08–10. doi: 10.7860/JCDR/2014/9687.5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zachert G., Rapp M., Eggert R. Additional tension screws improve stability in elastic stable intramedullary nailing: biomechanical analysis of a femur spiral fracture model. Eur J Pediatr Surg. 2015;25:365–372. doi: 10.1055/s-0034-1376394. [DOI] [PubMed] [Google Scholar]
- 38.Griffet J., Leroux J., Boudjouraf N. Elastic stable intramedullary nailing of tibial shaft fractures in children. J Child Orthop. 2011;5:297–304. doi: 10.1007/s11832-011-0343-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Swamy A. Management of pediatric femoral shaft fractures with long intramedullary kirshner wires. Libyan J Med. 2012;7 doi: 10.3402/ljm.v7i0.17275. [DOI] [PMC free article] [PubMed] [Google Scholar]