Abstract
Purpose
To report complications in the management of complex closed proximal tibial fractures.
Method
A retrospective study was conducted to analyze the infectious and noninfectious complications encountered in the management of high-energy Schatzker type V and VI tibial plateau fractures. All patients were treated at the level 1 trauma centre between January 2011 and March 2014. Sixty two patients were included in the study. The mean patient age was (43.16 ± 11.59) years with 60 males and 2 females. Infectious complications like superficial and deep infection, wound dehiscence, malalignment in the immediate postoperative period and in follow-up period were noted.
Results
The overall complication rate was 30.65% (19 out of 62). Infectious complications were noted in 20.97% cases (13/62). In majority of the cases (8/13), superficial infection was seen which managed with regular dressing and antibiotic administration. The patients (5/13) who had developed deep-seated infection were subjected to repeated debridements, flap coverage, implant removal or amputation depending upon the host response. Thirteen patients had experienced noninfectious complications. Hardware related complications were noticed in six patients and four among them received a secondary procedure. Malalignment was observed in seven patients but only single patient underwent subsequent operative intervention.
Conclusion
Proximal tibial plateau fractures especially Shatzker type V and VI are associated with extensive soft tissue damage even in closed injuries. The complications encountered in the management of these fractures can be minimized with appropriate patient selection and minimal soft tissue dissection.
Keywords: Tibial plateau fractures, Complication, Soft tissue damage
Introduction
The high-energy tibial plateau fractures are associated with extensive soft tissue and degloving injuries. The surgical insult adds further to the preexisting injury and gives nightmare to the operating surgeon. The classical midline incision used for the accurate reduction of these complex fracture patterns is associated with high incidence of wound complications ranging upto 80%.1 To reduce the complication rate, Barei et al2 advocated the use of knee spanning external fixator till the subsidence of soft tissue swelling and blisters. Subsequently the open reduction is performed for definitive fixation of the fracture. The incidence of complications has reduced to a great extent with the use of staged management in these high-energy fractures but still the complication rate has been pegged around 10%.3
The goal of treatment is to avoid further soft tissue injury, and obtain limb axis restoration and accurate intraarticular reduction,4, 5 but it requires excellent soft tissue handling and fracture reduction skills to avoid iatrogenic complications.6, 7 Various treatment options include external fixation with ring or hybrid fixator, locking and non-locking plates through minimally invasive and formal open reduction procedures.8, 9, 10 This study analyzes the complications associated with the management of high-energy proximal tibial fractures treated with locking plates (including minimally invasive techniques and formal open procedures) and also reviews the complications reported earlier in the literature.11, 12 The literature mainly emphases radiological and functional outcome primarily and very few studies focus on the complications encountered in the management of these complex fractures managed with locking plates.
Patients and methods
We performed a retrospective review at level one trauma centre of patients affected by high-energy tibial plateau fractures (Schatzker type V and VI) treated by open reduction and internal fixation with locking plates through minimally invasive techniques from January 2011 to March 2014. The inclusion criteria were as follows: patients aged between 18 and 60 years; no previous involvement of ipsilateral lower limb by surgery, fracture or arthritis; a minimum follow-up of two years; closed fracture of the proximal tibia; patients treated with locking plates; high-energy tibial plateau fractures (type V and VI) or AO type 41-C1, C2 and C3; no surgical intervention carried out prior to presentation at the institution.
All the preoperative and postoperative clinical data were obtained by reviewing the data sheets obtained from the medical record section of the institute. The hospital data sheet included brief history of the incident, mechanism of injury, delay in surgery, operative notes and revision surgery if any required. The data sheets of the patients were also specifically searched for intraoperative and postoperative complications. The patients were contacted on phone and/or conventional mail. All the patients were informed of the study and consent to participate was taken. A total of 62 patients were willing to participate in the study.
The mean patient age was (43.16 ± 11.59) years; 60 patients were males and 2 were females. The mechanism of injury was motor vehicle accident in 50 cases, fall from height in 3, assault in 1 and in 8 cases pedestrian was hit by a vehicle.
The average delay in definitive fixation was (9.27 ± 4.49) days after the initial injury. The patients were treated in staged manner with application of external fixator till the subsidence of soft tissue swelling and appearance of wrinkle sign. The definitive procedure with locking plates was carried out subsequently. Those associated with compartment syndrome were treated with four compartment fasciotomy and spanning external fixation with delayed fixation and spilled thickness grafting or delayed primary closure.
All patients were given preoperative antibiotics (1.5 gm cefuroxime intravenous) as per the institution protocol after sensitivity testing. The operative procedure was performed in a standard operating room under regional or general anesthesia and tourniquet control. The fracture was approached through anterolateral or posteromedial side depending upon the fracture configuration. The posteromedial exposure was performed through skin incision given just posterior to the posteromedial edge of tibia and following the course of pes tendons. The pes tendons were retracted anteriorly while the medial gastrocnemius was retracted posteriorly to expose the posterior surface of the tibia. Anterolaterally, the skin incision was given centering over the Gerdy's tubercle. The submensical arthrotomy was performed to visualize the articular surface wherever required. The provisional fracture reduction was confirmed under fluoroscopy. The patients were subjected to single or dual plating depending upon the fracture configuration. The use of autologous bone graft or bone graft substitutes was left to the discretion of the operating surgeon. Physical therapy was started on second postoperative day which included active and passive range of motion exercises of knee. The patients were allowed progressive partial weight bearing postoperatively and full weight bearing was authorized at 12 weeks. The bony union was defined as healing by direct means as seen in two radiographic planes. Another consideration for healing was full painless weight bearing. Follow-up radiographic assessment consisted of serial radiographs. The specific radiographs consisted of anteroposterior and lateral radiographs at the knee joint. They were taken immediately postoperatively, at six weeks, three month, one year and two years after surgical intervention. The radiographs were evaluated for signs of bony consolidation, residual intraarticular step-off, loss of alignment and failure of implant. The joint reduction was considered to be satisfactory if articular depression or tibial condylar widening was equal to or less than 5 mm. Malunion was defined as axial alignment of varus/valgus greater than five degrees, rotation greater than ten degrees and shortening of more than 2 cm calculated after bony union.13 Deep and superficial infections were categorized upon the basis of extent of infection extending below or above the fascia. Patients were also inquired about the subsequent soft tissue procedures, hardware removal, and any other procedure for alignment, nonunion or malunion.
Data were presented as means ± standard deviation, and analyzed by Fisher's exact two tailed test. All statistically significant variables were subjected to a multivariate logistic regression model to assess which variable was independently associated with higher incidence of infection. In the final multivariate logistic regression model, p < 0.05 was considered statistically different. The statistical package used for analyses was SAS 9.2.
Results
Using our inclusion criteria, 62 patients were available for the present retrospective cohort study; 25 patients sustained Schatzker type V and 37 patients experienced type VI fractures. The mean follow-up was (36.96 ± 11.59) months (ranging 24 months–63 months). Among them, 39 patients were followed up between 24 and 36 months, and 23 patients for more than 36 months. The average delay in surgery was (9.27 ± 4.49) days. In 11 cases the delay was more than two weeks due to associated injuries. Six patients had to undergo fasciotomy for compartment syndrome, among whom four required split skin thickness grafting and two had primary closure of wound. Three patients had peroneal nerve palsy and all of them had spontaneous recovery. Five patients had associated contralateral lower limb and upper limb injuries. Seven patients had ligamentous and meniscal injuries detected after the fixation of fracture. Three among them had isolated medial collateral injury and one had associated lateral meniscus injury with medial collateral injury which was managed conservatively. Two patients had anterior cruciate ligament with lateral meniscus injury and one among them had medial collateral ligament injury in addition to it. One patient had posterior cruciate ligament injury associated with medial meniscus injury. Ligament reconstruction was not done in these patients as they were not willing for the second operative intervention. Six patients underwent manipulation under anesthesia for severe postoperative stiffness.
The overall complication rate noted in the study was 30.65% (19 out of 62). Twelve patients were advised second operative procedure; however only ten opted for the subsequent procedure. The complications encountered in the management of high-energy tibial plateau fractures have been summarized in Table 1.
Table 1.
Complications encountered in operatively treated cases.
| Complication | Number of cases | Cases required subsequent operative procedure (n) |
|---|---|---|
| Superficial infection | 8 | 0 |
| Deep infection | 5 | 5 |
| Malalignment in postoperative period | 5 | 0 |
| Malalignment in the follow-up period | 2 | 1 |
| Peroneal nerve palsy | 3 | 0 |
| Hardware-related problems | 6 | 4 |
Infection is one of the most dreaded complications faced while managing these types of fractures.14 The incidence of infection was 20.97% (13/62). Among them majority (8/62) had developed superficial infection at the surgical site. The patients with superficial infection were treated with regular dressings and oral antibiotics. There was complete resolution of infection within one month in all these cases.
The deep infection was noted in 8.06% cases (5/62). Three patients with closed injury had developed deep seated infection. The average delay in plate application was 14.5 days and dual plating was done in all 3 cases. The patients experienced wound dehiscence with discharge (Fig. 1, Fig. 2). The patients were managed with multiple debridements and subsequent flap coverage with gastrocnemius in two cases. In one case the primary closure of the wound was obtained after debridements. They were given intravenous antibiotics at six to eight weeks and subsequently oral antibiotics at three to five months. One among them had been consuming tobacco for more than ten years.
Fig. 1.

Wound dehiscence with exposure of lateral tibial locking plate.
Fig. 2.

Flap coverage over the proximal tibia.
Three patients had to undergo implant removal as deep seated infection was not resolved even after repeated debridements and antibiotic administration (Fig. 3, Fig. 4, Fig. 5). The patients experienced restriction of movements at the knee joint. However the movements were unaffected in one patient (Fig. 6). In one patient the infection was not resolved even after implant removal and had opted for above knee amputation. The intraoperative culture was positive for pseudomonas aeruginosa on one occasion. He was an occasional smoker and was a known diabetic for the last five years managed with oral hypoglycemic.
Fig. 3.

Multiple discharging sinuses even after repeated debridements.
Fig. 4.

Image showing active discharging sinus from lateral aspect of proximal tibia.
Fig. 5.

Chronic discharging sinus after implant removal.
Fig. 6.
Good range of movement in a patient with chronic discharging sinus.
One patient among the three who underwent fasciotomy developed deep seated infection in the follow-up period. The application of plate was delayed by three weeks after fasciotomy in all the cases. The index case had developed deep infection after two months of the plate application. There was serous discharge and the intraoperative cultures were negative (Table 2). The patient was taken up for debridement twice and there was no compliant at last follow up (38 months).
Table 2.
Profile of patients with deep seated infection.
| Case no. | Fracture type (AO classification) | Microorganism | Clinical features | Treatment |
|---|---|---|---|---|
| 6 | 41C2 | Staphylococcus aureus | Purulent discharge, wound dehiscence | Debridement, flap coverage |
| 13 | 41C3 | Methicillin resistant staphylococcus aureus | Purulent discharge, wound dehiscence | Debridement, implant removal, flap coverage |
| 15 | 41C3 | No growth | Serous discharge | Debridement, implant removal |
| 19 | 41C2 | No growth | Serous discharge | Debridement |
| 53 | 41C2 | Pseudomonas aeruginosa | Serous discharge, wound dehiscence | Debridement, implant removal, external fixator, above knee amputation |
Six patients experienced hardware related complications. Three patients underwent removal of single proximal row screw due to pain associated with the medial soft tissue sleeve irritation by lateral locking plate. Three patients complained of mechanical symptoms or pain due to hardware irritation due to lateral locking plates. Among them one patient had opted for implant removal and other two were managed conservatively. All the three patients had bone to locking plate distance less than 1 cm.
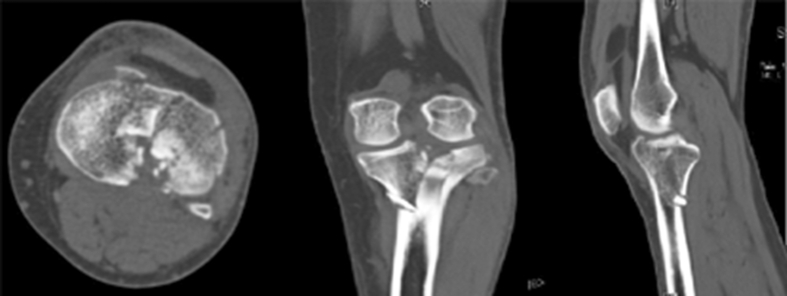
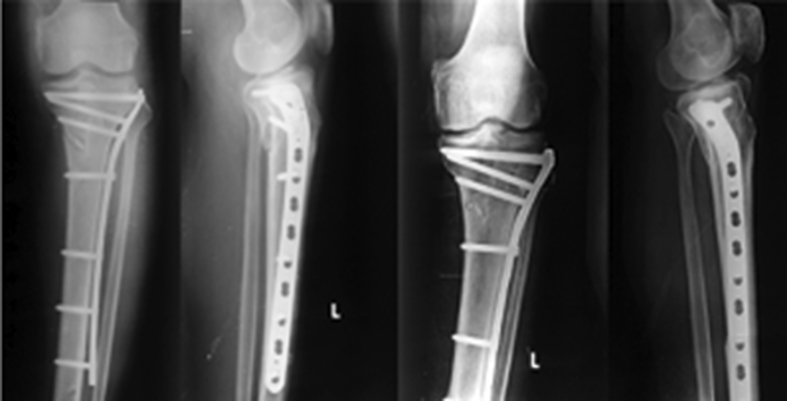
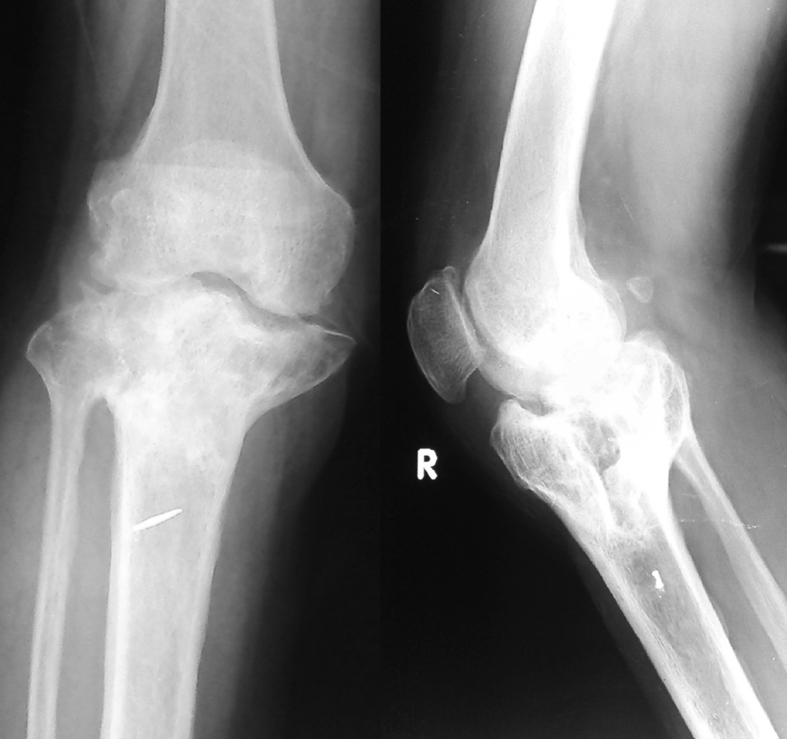
Malalignment was noticed in the postoperative radiographs of five patients while two patients had lost alignment on follow-up. Three patients had varus (Fig. 7, Fig. 8) while one patient had valgus deformity in coronal plane. One among them experienced malunion due to premature implant removal due to associated deep seated infection (Fig. 9). Two patients had hypertension deformity in sagittal plane. One patient with varus deformity had total knee replacement for secondary osteoarthritis at last follow up (36 months). While other patients were not willing for the second procedure.
Fig. 7.
Preoperative CT scan of the patient showing bicondylar fracture of proximal tibia.
Fig. 8.
Progression of varus deformity over one year.
Fig. 9.
Malunited proximal tibia fracture in patient who had undergone plate removal following deep seated infection.
The longer operative time required in infected cases (3 h vs. 2.3 h) was statistically significant in comparison to noninfected group (p = 0.05). The factors like fasciotomy and injury severity score had direct bearing on the infection rate in these closed high-energy fractures. The incidence of infection in patients undergoing fasciotomy (33%) was statistically significant in comparison to the control group (7.2%, p = 0.01). The patients with injury severity score greater than 9 had higher incidence of infection (86% vs. 43%, p = 0.04) in contrast to noninfected tibial fractures.
The incidence of tobacco consumption was comparable in infected and noninfected group (40% vs. 35%) and there was no significant association (p = 0.18). Other patient dependent variables like age (44.15 years and 42.16 years, p = 0.17), sex (78.4% males and 68% p = 0.12) and diabetes mellitus (20% and 8.8%, p = 0.07) did not have any significant difference with respected to infection rate. The loss of alignment was also not association with the deep seated infection (p = 0.4624).
The factors like operative time, fasciotomy and injury severity score found to be statistically significant on univariate analysis were subjected to multivariate logistic regression analysis. In the analysis it was observed that operative time (odds ratio 1.72, p = 0.05) and injury severity score (odds ratio 1.72, p = 0.05) had independent influence on infection rate; while fasciotomy (odds ratio 2.79, p = 0.12) was not an independent predictor of infection.
Discussion
Open reduction and internal fixation of high-energy tibial plateau fractures remains one of the most accepted methods of fixation.15 The introduction of locking plates and minimally invasive approach has decreased the complication rate by many folds but still the optimal management of these fractures remains controversial.16 Open reduction of the tibial plateau fracture allows direct visualization and reduction of the fracture. Accurate intraarticular reduction achieves good results in terms of final functional outcome.17, 18
In the past the complication rate associated with open reduction was around 23%–100%.19, 20 The higher number of wound complication was due to single incision and extensive soft tissue stripping done especially in dual plating leading to posttraumatic osteomyelitis. Other factors like compromised blood supply to the localized area due to trauma, implant making direct contact with the bone and virulence of the organism significantly contributes to the problem.21 Appropriate initial management with measures like external fixator application, limb elevation and waiting for soft tissue swelling to subside, can avoid infective complications to a large extent.
Benirschke et al22 advocated immediate debridement, thorough washing of wound and fracture fixation followed by delayed wound closure. The creation of large flaps was avoided. Barei et al23 similarly reported marked decrease in the complication rate with the use of dual incisions in the treatment of AO type 41-C3 fractures after the subsidence of soft tissue swelling. In the present retrospective cohort five out of sixty two patients had developed deep infection which was comparable to that described by Barei et al (Table 2). The incidence of superficial infection (8 out of 62) though was higher than deep seated infection, was resolved with regular dressings and oral antibiotics. With better understanding of the fracture configuration and staged managed of these complex fracture patterns, the incidence of infectious complications have been curtailed to a large extent.
Thirteen patients had experienced complications pertaining to noninfectious category. The common among them were hardware related problems and malalingment. The incidence of irritation of medial soft tissue sleeve with the use of lateral locking plates (3 out of 62) were reported higher in our series than reported in literature and it could have been avoided by the operating surgeons with judicious use of fluoroscopy. The irritation due to lateral locking plates is expected due to subcutaneous location of the plate. However the irritation is lower in cases with bone plate distance less than 1 cm.24 Close approximation of plate and bone with the help of reduction forceps can reduce the mechanical symptoms.
Malalignment was reported in immediate postoperative (8% cases) and follow up period (3% cases). In literature, this complication has been reported between 0% and 59%.25, 26, 27 The large variation in reporting could be due to different criteria used for evaluation, reliability of techniques used for measuring and quality of radiographs used for the purpose of evaluation. In cases of malalignment noted in immediate postoperative period, the reason ascertained was inadequate intraoperative reduction. Indirect reduction maneuvers and fluoroscopy should be used judiciously to prevent malalignment especially in cases treated with minimally invasive techniques. The fracture must be reduced accurately before application of the plate. It was also noticed that the patients with AO type 41 C3 had higher incidence of malalignment (4 out of 5) as compared to other variants. This may be due to difficulty encountered with reduction of highly comminuted fractures.
Two cases had loss of alignment in the follow-up period. The loss of alignment is seen especially in comminuted fractures as subchondral purchase of screws is not possible in many such cases due to fixed angle of insertion of screws. However the introduction of variable angle locking plates has reduced this problem but the long-term benefits of the same are yet to be investigated. Varus collapse is a commonly encountered problem in the management of these high-energy fractures treated with single lateral locking plate, but it can be curtailed to large extent with the use of posteromedial buttress wherever required.28, 29, 30 In our study, the posteromedial buttress plate was used in thirty cases out of thirty seven cases of Schatzker type VI tibial plateau fractures. One patient underwent total knee replacement at last follow-up; while other patient refused to undergo any further operative intervention.
This study had certain limitations. The retrospective nature of the study inherited selection bias. The sample size was small (n = 62) and there was no control group. However this study throws adequate light over the complications encountered in the management of complex high-energy proximal tibial fractures. Both infectious and noninfectious complications have a bearing on the final functional outcome. Long-term studies shall be required to know the effect of each complication noticed in the study.
In conclusion, the high-energy Schatzker type V and VI fractures are associated with extensive injury to the soft tissue envelope surrounding the knee. Open reduction and internal fixation with minimally invasive techniques is considered as an acceptable method of fixation of these fractures. However even with the application of staged techniques the number of complications encountered in the management of these fractures is high. With careful selection of patients and minimal soft tissue dissection, the number and extent of complications can be reduced.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Prasad G.T., Kumar T.S., Kumar R.K. Functional outcome of Schatzker type V and VI tibial plateau fractures treated with dual plates. Indian J Orthop. 2013;47:188–194. doi: 10.4103/0019-5413.108915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barei D.P., Nork S.E., Mills W.J. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Jt Surg Am. 2006;88:1713–1721. doi: 10.2106/JBJS.E.00907. [DOI] [PubMed] [Google Scholar]
- 3.Jöckel J.A., Erhardt J., Vincenti M. Minimally invasive and open surgical treatment of proximal tibia fractures using a polyaxial locking plate system: a prospective multi-centre study. Int Orthop. 2013;37:701–708. doi: 10.1007/s00264-013-1820-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sciadini M.F., Sims S.H. Proximal tibial intra-articular osteotomy for treatment of complex Schatzker type IV tibial plateau fractures with lateral joint line impaction: description of surgical technique and report of nine cases. J Orthop Trauma. 2013;27:e18–23. doi: 10.1097/BOT.0b013e31825316ea. [DOI] [PubMed] [Google Scholar]
- 5.Hill A.D., Palmer M.J., Tanner S.L. Use of continuous passive motion in the postoperative treatment of intra-articular knee fractures. J Bone Jt Surg Am. 2014;96:e118. doi: 10.2106/JBJS.M.00534. [DOI] [PubMed] [Google Scholar]
- 6.Ozkaya U., Parmaksizoglu A.S. Dual locked plating of unstable bicondylar tibial plateau fractures. Injury. 2015;46(Suppl 2):S9–S13. doi: 10.1016/j.injury.2015.05.025. [DOI] [PubMed] [Google Scholar]
- 7.Ahearn N., Oppy A., Halliday R. The outcome following fixation of bicondylar tibial plateau fractures. Bone Jt J. 2014;96-B:956–962. doi: 10.1302/0301-620X.96B7.32837. [DOI] [PubMed] [Google Scholar]
- 8.Naik M.A., Arora G., Tripathy S.K. Clinical and radiological outcome of percutaneous plating in extra-articular proximal tibia fractures: a prospective study. Injury. 2013;44:1081–1086. doi: 10.1016/j.injury.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Ramos T., Karlsson J., Eriksson B.I. Treatment of distal tibial fractures with the Ilizarov external fixator–a prospective observational study in 39 consecutive patients. BMC Musculoskelet Disord. 2013;14:30. doi: 10.1186/1471-2474-14-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee T.C., Huang H.T., Lin Y.C. Bicondylar tibial plateau fracture treated by open reduction and fixation with unilateral locked plating. Kaohsiung J Med Sci. 2013;29:568–577. doi: 10.1016/j.kjms.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Devkota P., Manandhar H.K., Khadka P.B. Less invasive stabilization system for the management of proximal tibia fractures. Eur J Orthop Surg Traumatol. 2014;24:993–998. doi: 10.1007/s00590-013-1365-0. [DOI] [PubMed] [Google Scholar]
- 12.Ruffolo M.R., Gettys F.K., Montijo H.E. Complications of high-energy bicondylar tibial plateau fractures treated with dual plating through 2 incisions. J Orthop Trauma. 2015;29:85–90. doi: 10.1097/BOT.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 13.Morris B.J., Unger R.Z., Archer K.R. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma. 2013;27:e196–200. doi: 10.1097/BOT.0b013e318284704e. [DOI] [PubMed] [Google Scholar]
- 14.Rademakers M.V., Kerkhoffs G.M., Sierevelt I.N. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21:5–10. doi: 10.1097/BOT.0b013e31802c5b51. [DOI] [PubMed] [Google Scholar]
- 15.Lachiewicz P.F., Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop Relat Res. 1990;259:210–215. [PubMed] [Google Scholar]
- 16.Stannard J.P., Wilson T.C., Volgas D.A. The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma. 2004;18:552–558. doi: 10.1097/00005131-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Goetz J.E., Fredericks D., Petersen E. A clinically realistic large animal model of intra-articular fracture that progresses to post-traumatic osteoarthritis. Osteoarthr Cartil. 2015;23:1797–1805. doi: 10.1016/j.joca.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y., Fan D.G., Ma B.A. Treatment of complicated tibial plateau fractures with dual plating via a 2-incision technique. Orthopedics. 2012;35:e359–364. doi: 10.3928/01477447-20120222-27. [DOI] [PubMed] [Google Scholar]
- 19.Ramos T., Eriksson B.I., Karlsson J. Ilizarov external fixation or locked intramedullary nailing in diaphyseal tibial fractures: a randomized, prospective study of 58 consecutive patients. Arch Orthop Trauma Surg. 2014;134:793–802. doi: 10.1007/s00402-014-1970-3. [DOI] [PubMed] [Google Scholar]
- 20.Pun T.B., Krishnamoorthy V.P., Poonnoose P.M. Outcome of Schatzker type V and VI tibial plateau fractures. Indian J Orthop. 2014;48:35–41. doi: 10.4103/0019-5413.125490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin S., Mauffrey C., Hammerberg E.M. Surgical site infection after open reduction and internal fixation of tibial plateau fractures. Eur J Orthop Surg Traumatol. 2014;24:797–803. doi: 10.1007/s00590-013-1252-8. [DOI] [PubMed] [Google Scholar]
- 22.Benirschke S.K., Agnew S.G., Mayo K.A. Immediate internal fixation of open, complex tibial plateau fractures: treatment by a standard protocol. J Orthop Trauma. 1992;6:78–86. [PubMed] [Google Scholar]
- 23.Barei D.P., Nork S.E., Mills W.J. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004;18:649–657. doi: 10.1097/00005131-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Phisitkul P., McKinley T.O., Nepola J.V. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007;21:83–91. doi: 10.1097/BOT.0b013e318030df96. [DOI] [PubMed] [Google Scholar]
- 25.Van Dreumel R.L., van Wunnik B.P., Janssen L. Mid-to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46:1608–1612. doi: 10.1016/j.injury.2015.05.035. [DOI] [PubMed] [Google Scholar]
- 26.Parkkinen M., Madanat R., Mustonen A. Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: mid-term clinical and radiographic outcomes of 73 operatively treated patients. Scand J Surg. 2014;103:256–262. doi: 10.1177/1457496914520854. [DOI] [PubMed] [Google Scholar]
- 27.Weaver M.J., Harris M.B., Strom A.C. Fracture pattern and fixation type related to loss of reduction in bicondylar tibial plateau fractures. Injury. 2012;43:864–869. doi: 10.1016/j.injury.2011.10.035. [DOI] [PubMed] [Google Scholar]
- 28.Mueller C.A., Eingartner C., Schreitmueller E. Primary stability of various forms of osteosynthesis in the treatment of fractures of the proximal tibia. J Bone Jt Surg Br. 2005;87:426–432. doi: 10.1302/0301-620x.87b3.14353. [DOI] [PubMed] [Google Scholar]
- 29.Luo C.F., Sun H., Zhang B. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24:683–692. doi: 10.1097/BOT.0b013e3181d436f3. [DOI] [PubMed] [Google Scholar]
- 30.Chen H.W., Chen C.Q., Yi X.H. Posterior tibial plateau fracture: a new treatment-oriented classification and surgical management. Int J ClinExp Med. 2015;8:472–479. [PMC free article] [PubMed] [Google Scholar]