Abstract
Empirical evidence suggested that mind-body interventions can be effectively delivered online. This study aimed to examine whether preventive online mindfulness interventions (POMI) for non-clinical populations improve short- and long-term outcomes for perceived-stress (primary) and mindfulness (secondary). Systematic search of four electronic databases, manuscript reference lists, and journal content lists was conducted in 2016, using 21 search-terms. Eight randomized controlled trials (RCTs) evaluating effects of POMI in non-clinical populations with adequately reported perceived-stress and mindfulness measures pre- and post-intervention were included. Random-effects models utilized for all effect-size estimations with meta-regression performed for mean age and %females. Participants were volunteers (adults; predominantly female) from academic, workplace, or community settings. Most interventions utilized simplified Mindfulness-Based Stress Reduction protocols over 2–12 week periods. Post-intervention, significant medium effect found for perceived-stress (g = 0.432), with moderate heterogeneity and significant, but small, effect size for mindfulness (g = 0.275) with low heterogeneity; highest effects were for middle-aged individuals. At follow-up, significant large effect found for perceived-stress (g = 0.699) with low heterogeneity and significant medium effect (g = 0.466) for mindfulness with high heterogeneity. No publication bias was found for perceived-stress; publication bias found for mindfulness outcomes led to underestimation of effects, not overestimation. Number of eligible RCTs was low with inadequate data reporting in some studies. POMI had substantial stress reduction effects and some mindfulness improvement effects. POMI can be a more convenient and cost-effective strategy, compared to traditional face-to-face interventions, especially in the context of busy, hard-to-reach, but digitally-accessible populations.
Keywords: Mind-body relations, Randomized controlled trial, Computer, Psychological stress
Highlights
-
•
Most interventions utilized simplified Mindfulness-Based Stress Reduction protocols.
-
•
Post-intervention, medium effect and heterogeneity for perceived stress (g = 0.432)
-
•
Post-intervention, small effect and low heterogeneity for mindfulness (g = 0.275)
-
•
At follow-up, large effect and low heterogeneity for perceived-stress (g = 0.699)
-
•
At follow-up, medium effect and high heterogeneity for mindfulness (g = 0.466)
1. Context
Mindfulness can be described as deliberately paying attention, non-judgmentally, in the present moment with simultaneous awareness of thoughts, emotions, and physical sensations (Gunaratana, 1993). Traditionally, this concept originated in the Vipassana components of Theravada Buddhism from South-East Asia and Mahayana Buddhism (e.g., Zen) from East Asia (Kitagawa, 1979). These traditions, recognizing the busy mind, prized attaining a sense of choice and improving internalized control. In Western cultures, mindfulness is practiced as a spiritual exercise of Buddhism, but more commonly, as either a complementary psychotherapy for certain clinical conditions (i.e., treatment) or as secular attitudinal training for enhancing psychological functioning and relieving stress (i.e., prevention) (Chiesa, 2010). To date, no clear operational definition of “mindfulness” exists and terms like “meditation” and “mindful attention” are used interchangeably.
1.1. Rationale
Persistent stress leads to health problems such as cardiovascular disease, stroke, depression, upper respiratory tract infections, and autoimmune disorders (McEwen, 1998). For adults, it affects work performance and, for students, academic achievement through reduced productivity, high absenteeism and presenteeism that generate substantial financial burdens. For example, the estimated cost of U.S. workplace stress alone was $125–190 billion per year (5%–8% of national health spending) (Goh et al., 2016). Numerous preventive mindfulness interventions have focused on managing occupational stress and enhancing work efficiency (Cohen-Katz et al., 2005). However, many face-to-face stress reduction interventions are fraught with excessive human resource allocations and time conflict issues. Meanwhile, mindfulness interventions conducted for treatment purposes (Reibel et al., 2001) outnumber those conducted for prevention of unhealthy conditions; for example, mindfulness studies designed to treat eating disorders (Kristeller and Hallett, 1999, Kristeller and Wolever, 2011, Kristeller et al., 2006) outnumber those for improving eating behaviors of non-clinical populations (Barnes et al., 2016). Nevertheless, recent surveys indicate that some wellness-related mind-body practices are increasingly popular among both U.S. adults and children (Black et al., 2015, Clarke et al., 2015, Stussman et al., 2015).
Online interventions are appealing because they are more cost-effective and user-friendly (Cutshall et al., 2011). In modern society, digital access and internet use have increased considerably (Zickuhr and Smith, 2012), especially among young people (Pew Research Center's Internet and American Life Project, 2012), with sizable portions of computer and smart phone use devoted to non-occupational pursuits, such as social networking and health tracking (Pew Research Center's Internet and American Life Project, 2012). While use of face-to-face interventions in institutional and community settings increased during the past decade as a strategy of complementary treatment, worksite performance enhancement, or stress management (Bohlmeijer et al., 2010, Grossman et al., 2004, Tsai and Crockett, 1993), preventive online mindfulness interventions (POMI) remain relatively uncommon. Mindfulness interventions conducted exclusively for prevention have varied widely by targeted health outcome and participant type, with only a few conducted online (Aikens et al., 2014, Allexandre et al., 2016, Cavanagh et al., 2013, Glueck and Maercker, 2011, Mak et al., 2015, Morledge et al., 2013, Wahbeh et al., 2016, Wolever et al., 2012). Therefore, a critical need exists to systematically assess the effectiveness of mindfulness interventions delivered online for the purpose of reducing perceived stress and increasing mindfulness since such an assessment has not yet been undertaken.
1.2. Objectives
To examine whether POMI, designed for non-clinical population improves short- and long-term outcomes related to perceived-stress (primary outcome) and mindfulness (secondary outcome), this meta-analysis reviewed randomized controlled trials (RCTs) comparing perceived stress and mindfulness outcomes of participants against non-participating control groups.
2. Evidence acquisition
2.1. Protocol
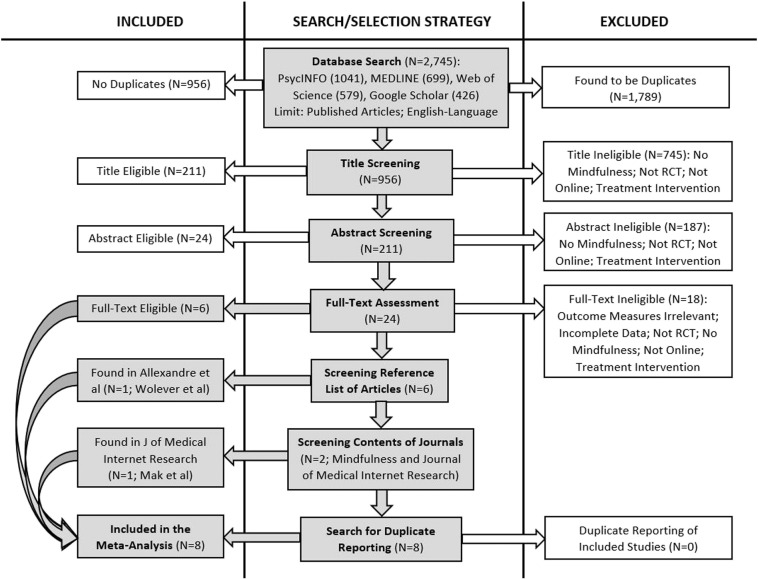
Inclusion criteria, outcome measures, and analysis methods were specified prior to literature search (Fig. 1) and documented in a protocol (Liberati et al., 2009).
Fig. 1.
Flow of information through different phases of the study selection process.
2.2. Eligibility criteria
2.2.1. Types of studies
RCTs, examining online administration of mindfulness training, published in or translatable into English, were eligible. Only studies published in peer-reviewed journals were eligible; thus, unpublished materials, dissertations, and abstracts were excluded. Although exclusion of unpublished materials increases publication bias, the peer review process potentially reduces inclusion of studies with lower methodological quality, thus also reducing selective reporting bias. No publication year or country restriction was imposed.
2.2.2. Types of participants
Participants of any age, receiving no mental health disorder treatment, were considered. Participants were either self-referrals or those invited to participate in a workplace or academic setting intervention. Participants with a clinical mental illness diagnosis were excluded from this review, as mindfulness training might not be preventive for them.
2.2.3. Types of intervention
Studies were eligible if they assessed perceived stress reduction and mindfulness effects of mindfulness interventions, exclusively delivered online, by comparing effects on perceived-stress and mindfulness between intervention and control groups. No restriction was imposed on study setting, intervention intensity/strategy, or participants' digital literacy. Interventions not assessing the effects of online mindfulness training alone, for example, those combining online mindfulness training with face-to-face mindfulness training or other mind-body practices (e.g., yoga), were excluded.
2.2.4. Types of outcome measures
Primary outcome measure was perceived-stress, measured on a standard instrument (e.g. but not limited to Perceived Stress Scale (PSS) (Cohen and Williamson, 1988, Cohen et al., 1983) administered to intervention and control groups pre- and post-intervention and at follow-up. Secondary outcome measure was mindfulness, measured on a standard instrument such as Cognitive and Affective Mindfulness Scale Revised (CAMS-R) (Feldman et al., 2007), Five Facets of Mindfulness Questionnaire (FFMQ) (Baer et al., 2006), and Mindfulness Attention Awareness Scale (MAAS) (Brown and Ryan, 2003). While these instruments are conceptually similar to each other, they also are dissimilar due to differences in the number and nature of mindfulness constructs (Sauer et al., 2013). For example, CAMS-R measured four factors (attention, present focus, awareness, acceptance) and FFMQ measured five factors (nonreactivity to inner experience, noticing sensations, acting with awareness, describing with words, nonjudging of experience), whereas MAAS measured one factor (attention) only. Other outcomes such as work-family conflict, emotions, mood, and anxiety were not with in this study's purview. Outcome measures were excluded if not well-defined or unobtainable with sufficient detail.
2.3. Information sources
A systematic search was conducted to locate studies of POMI through March 2016 in four electronic databases: MEDLINE, PsycINFO, Web of Science, and Google Scholar. Additionally, reference lists from six POMI study articles were scanned and contents pages of two journals were hand-searched. An expert in the field was also consulted.
2.4. Search
Combinations of 21 search terms were used in database searches: online, internet, automated, computer, web, digital, app, e-health, m-health, social media, mobile applications, smartphone, mindfulness, meditation, mind-body, focused attention, open monitoring, breath counting, guided imagery, randomized controlled trial, and random allocation. (Appendix-1 provides an example of full search strategy.) Articles not published in or that were untranslatable into English were ignored due to unavailability of experts with pertinent language skills.
2.5. Study selection
Search was subsequently narrowed via hand-search to include only preventive interventions. Two authors ensured that no eligible preventive intervention was excluded in the final hand-search. Then, two authors, using an unblinded standard approach, independently assessed selected articles for eligibility; disagreements were resolved by consensus. Consequently, studies were finalized for meta-analysis inclusion.
2.6. Data collection process
Based on “Minimum Standards” found in the (Cochrane Consumers and Communication Review Group, 2015) data extraction template (Cochrane Consumers and Communication Review Group, 2015), a data extraction sheet was developed and piloted on three randomly-selected studies eligible for meta-analysis. Two authors independently completed the data extraction sheet for all eligible studies. Disagreements were resolved by consensus; a third author was involved if agreement was not reached. One article author was contacted for additional information.
2.7. Data items
Data were extracted from included studies regarding design, participants, interventions, results, and limitations (Appendix-2; Table 1).
Table 1.
Mean comparisons for perceived-stress and mindfulness in included studies: pre- and post-intervention and after follow-up.
| Author (year) | Perceived stress mean scores and standard deviations |
Mindfulness mean scores and standard deviations |
||||||
|---|---|---|---|---|---|---|---|---|
| Instrument (# of items) | Pre-test Mean (SD) | Post-test Mean (SD) | Follow-up Mean (SD) | Instrument (# of items) | Pre-test Mean (SD) | Post-test Mean (SD) | Follow-up Mean (SD) | |
| Aikens et al. (2014) | PSS (14) | M = 24.46 (6.29) | M = 18.00 (7.01) | M = 18.81 (6.72) | FFMQ (39) | M = 24.69 (5.16) | M = 27.94 (5.49) | M = 29.23 (5.14) |
| C = 24.76 (8.16) | C = 23.32 (8.45) | C = No follow up | C = 24.38 (5.47) | C = 24.62 (5.46) | C = No follow-up | |||
| Allexandre et al. (2016) | PSS (10) | M = 25.6 (5.4) | M = 19.8 (7.6) | M = 19.4 (7.7) | MAAS (15) | M = 3.20 (0.87) | M = 3.43 (1.16) | M = 3.32 (1.07) |
| C = 25.4 (5.7) | C = 24.0 (7.2) | C = 22.5 (7.2) | C = 3.48 (0.89) | C = 3.37 (0.92) | C = 3.47 (1.13) | |||
| Cavanagh et al. (2013) | PSS (10) | M = 21.70 (7.87) | M = 18.96 (6.75) | – | FFMQ (39) | M = 117.76 (21.48) | M = 116.24 (16.94) | – |
| C = 21.78 (7.27) | C = 21.46 (6.79) | C = 123.33 (20.16) | C = 116.92 (20.67) | |||||
| Glueck and Maercker (2011) | PSQ (20) German | M = 40.06 (16.38) | M = 34.36 (15.06) | M = 27.89 (11.18) | FMI (14) German | M = 37.04 (5.37) | M = 38.77 (5.38) | M = 41.16 (6.05) |
| C = 35.09 (13.39) | C = 34.72 (15.35) | C = No follow up | C = 39.95 (6.46) | C = 40.67 (6.78) | C = No follow-up | |||
| Mak et al. (2015) | PSS (10) Chinese | M = 1.72 (0.60) | M = 1.65 (0.53) | M = 1.70 (0.53) | FFMQ (39) Chinese | M = 3.13 (0.52) | M = 3.19 (0.53) | M = 3.16 (0.49) |
| C = 1.63 (0.70) | C = 1.62 (0.70) | C = 1.63 (0.70) | C = 3.18 (0.42) | C = 3.15 (0.43) | C = 3.22 (0.41) | |||
| Morledge et al. (2013) | PSS (10) | M = 22.4 (7.1) | M = 17.2 (6.0) | M = 16.0 (6.4) | MAAS (15) | M = 3.45 (0.89) | M = 4.03 (0.80) | M = 4.02 (0.82) |
| C = 22.3 (7.1) | C = 18.8 (7.6) | C = 18.9 (7.3) | C = 3.29 (0.90) | C = 3.65 (0.89) | C = 3.68 (0.96) | |||
| Wahbeh et al. (2016) | PSS (10) | M = 11.0 (7.0) | M = 14.4 (4.6) | – | FFMQ (39) | M = 134.8 (20.9) | M = 145.1 (19.7) | – |
| C = 10.9 (3.4) | C = 14.4 (6.3) | C = 136.4 (20.6) | C = 146.9 (22.1) | |||||
| Wolever et al. (2012) | PSS (10) | M = 24.52 (3.46) | M = 14.91 (5.70) | – | CAMSR (12) | M = 30.24 (6.06) | M = 34.96 (6.56) | – |
| C = 23.52 (3.79) | C = 19.34 (6.26) | C = 30.01 (5.75) | C = 32.37 (6.55) | |||||
Note: M = online mindfulness intervention; C = control; SD = standard deviation; PSS = Perceived Stress Scale; PSQ = Perceived Stress Questionnaire; FFMQ = Five Facet Mindfulness Questionnaire; MAAS = Mindful Attention Awareness Scale; FMI = Freiburg Mindfulness Inventory; CAMS-R = Cognitive and Affective Mindfulness Scale-Revised.
Average mindfulness scores of Aikens et al. were estimated, using means and standard deviations reported for each facet of the Five Facet Mindfulness Questionnaire.
Follow-up time varied by intervention (see Appendix-1). No follow-up in Cavanagh et al., Wahbeh et al., and Wolever et al. Aikens et al. and Gluck and Maercker had follow-up of intervention group only. All eight studies were randomized controlled trials; see Appendix-1 for characteristics of sample and intervention in individual studies.
Follow-up time varied by intervention (see Appendix-1). No follow-up in Cavanagh et al., Wahbeh et al., and Wolever et al. Aikens et al. and Gluck and Maercker had follow-up of intervention group only. All eight studies were randomized controlled trials; see Appendix-1 for characteristics of sample and intervention in individual studies.
2.8. Risk of bias in eligible studies
As effect-size depends on methodological quality and outcome measures of eligible studies, two reviewers independently assessed methodology quality, outcome measures, and extent of loss to follow-up plus data collector adequacy.
2.9. Summary measures
Mean perceived-stress differences between intervention and control groups or mean perceived-stress changes from baseline to follow-up assessment were primary outcome measures. Mindfulness was the secondary outcome assessed in each eligible study. Depending on the study, mean, mean difference, and mean change were utilized with standard error, standard deviation, confidence interval, or p-value for effect-size calculation.
2.10. Methods of analysis
Comprehensive Meta-Analysis Software Version-3 (2016) was utilized. Study means, obtained without variance estimates (standard deviation or standard error), were imputed using known statistics. In paired group analysis of baseline vs follow-up data, within-person variance was estimated from mean and variance estimates of pre- and post-intervention stages, assuming independence. For continuous data, Cohen's d was directly obtained, and subsequently, bias-corrected standardized mean difference (Hedges' g) was calculated (Borenstein et al., 2010). Relative weights were assigned to studies based on sample size. Results were tested for heterogeneity (using Q and I2) and outliers (Borenstein et al., 2010). High-resolution forest plots were developed separately with random effects.
2.11. Risk of bias across studies
Effect of each trial was plotted using the inverse of its standard error to visually assess any negative or small effect-size versus sample size correlations (Rothstein et al., 2005). Assuming some small studies with negative or non-significant findings are unpublished, funnel plots of intervention mean difference were visually evaluated for asymmetry to identify publication bias possibility; Duval and Tweedie's trim-and-fill method was also utilized. Nevertheless, these tests can be affected by study heterogeneity and differences in methodological quality (Rothstein et al., 2005).
2.12. Additional analyses
To assess the impact of participant characteristics on meta-analysis findings, protocol pre-specified performing meta-regression by mean age, along with percentage of females (Thompson and Higgins, 2002).
3. Evidence synthesis
3.1. Study selection
Eight RCTs were eligible for inclusion (Fig. 1). The comprehensive literature search utilizing 15 search terms was followed by adjustment for duplicates, producing 956 citations; study titles were screened and 745 were removed because they obviously did not meet inclusion criteria. Similarly, abstracts of 211 remaining articles were screened via inclusion criteria and 187 were removed; major reasons for exclusion were not involving mindfulness, not conducted online, not a RCT, and conducted as treatment intervention. Furthermore, two studies were discarded due to full-text unavailability. Detailed full-text examination of 24 remaining studies revealed that 18 did not meet inclusion criteria (Kemper et al., 2015, Krusche et al., 2013, Ljotsson et al., 2011, Murray et al., 2015, Zernicke et al., 2013), for example, Michel et al. measured strain-based work-family conflict, but had no direct measure of perceived-stress (Michel et al., 2014). Scanning reference lists of the remaining six studies identified one additional eligible study (Wolever et al., 2012), with yet another identified by hand-searching contents pages from two journals (Mak et al., 2015). No duplicate reports of the included eight eligible studies were found (Aikens et al., 2014, Allexandre et al., 2016, Cavanagh et al., 2013, Glueck and Maercker, 2011, Mak et al., 2015, Morledge et al., 2013, Wahbeh et al., 2016, Wolever et al., 2012); therefore, the number of eligible studies is equal to the number included in the review (Appendix-2).
3.2. Study characteristics
Of studies in the meta-analysis, six were conducted in the U.S., one in Switzerland and Austria (Glueck and Maercker, 2011), and one in Hong Kong (Appendix-2) (Mak et al., 2015). Summarized study characteristics are the following.
3.2.1. Methods
All studies were RCTs, retrieved from 2011 to 2016 issues of seven peer-reviewed journals published in English. Six studies contained a waitlist control group that received delayed intervention; waitlist control group in Wolever et al. (2012) or received a list of stress management resources, but waitlist control groups in the other five studies were inactive. Parallel control group of Wahbeh et al. (2016) received online health and wellness education; the control group of Morledge et al. (2013) was inactive. Number of intervention groups varied with three in Allexandre et al. (2016) and Wolever et al. (2012) and two in Mak et al. (2015) all other studies had one intervention group. Five RCTs had a post-intervention follow-up period, varying from four weeks (Morledge et al., 2013) to one year (the Allexandre et al. (2016) second follow-up time-point); only three studies included both intervention and control group follow-up (Allexandre et al., 2016, Mak et al., 2015, Morledge et al., 2013).
3.2.2. Participants
Sample sizes of eight studies ranged between 16 (pilot study by Wahbeh et al. (2016) and 551 (Morledge et al., 2013) yielding 1316 predominantly female participants; all adults. Of these, 505 were in control conditions, while 530 received online mindfulness interventions (Appendix-2). The remaining 281 participants were excluded from this meta-analysis for three reasons: received another intervention combined with online mindfulness (Allexandre et al., 2016, Mak et al., 2015) received in-person mindfulness training (Wolever et al., 2012) assigned to yoga-based stress reduction (Wolever et al., 2012). Mean age ranged between 22.8 (Mak et al., 2015) and 76.2 (Wahbeh et al., 2016) years. All eight studies targeted non-clinical populations (i.e., university students and staff, company employees, and community members); all subjects volunteered to participate. Exclusively, 2.2% of the sample in Morledge et al. (2013) constituted doctor referrals but physicians excluded patients with psychosis. Exclusion criteria across studies varied: e.g., mental disorders (Glueck and Maercker, 2011, Wahbeh et al., 2016, Wolever et al., 2012) severe/unstable medical conditions and cognitive disability (Wahbeh et al., 2016) and heavy smoking and pregnancy (Wolever et al., 2012) Only subjects with access to computers and internet at university, company/workplace, or home settings were involved.
3.2.3. Intervention
Intervention length varied between 2 weeks (Cavanagh et al., 2013, Glueck and Maercker, 2011) and 12 weeks (Wolever et al., 2012). All interventions except for Cavanagh et al. used simplified protocols of Kabat-Zinn's Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn et al., 1985, Kabat-Zinn et al., 1992), while Aikens et al. (2014) and Mak et al. (2015) additionally involved certified mindfulness-trainers. MBSR typically involves eight weekly two-and-a-half hour classes along with a one-day retreat following week six. Sessions include guided instructions on mindfulness practices, readings and handouts, light stretching and mindful movement, group dialogue, home assignments, and support materials such as guided meditation audio files. Compared to MBSR, interventions included in meta-analysis were less demanding in terms of content, session length, and number of sessions and included no retreat. Wahbeh et al.'s intervention (Wahbeh et al., 2016) integrated MBSR with Mindfulness-Based Cognitive Therapy (MBCT) (Kuyken et al., 2010). Cavanagh et al. involved a version of Mindfulness-Based Self-Help (MBSH) (Ly et al., 2014). Cavanagh et al.'s was delivered in a university's virtual learning classroom (Cavanagh et al., 2013), while Aikens et al. utilized both website and virtual learning classroom (Aikens et al., 2014); all others were delivered exclusively via website. Intervention strategies varied: regular reminder calls and emails (Allexandre et al., 2016, Cavanagh et al., 2013, Glueck and Maercker, 2011, Mak et al., 2015, Morledge et al., 2013); weekly progress tracking surveys and log sheets Aikens et al., 2014, Mak et al., 2015; pre-programmed e-mail coaching and tailored feedback (Aikens et al., 2014, Mak et al., 2015); customized text messaging (Aikens et al., 2014); audio-based meditation exercises (Glueck and Maercker, 2011, Mak et al., 2015), increasing in length and complexity throughout the course; 10-min audio track with guided mindfulness (female or male voice recorded by certified mindfulness therapists) (Cavanagh et al., 2013); 3-minute meditation offered as quick coping strategy (Wahbeh et al., 2016); meditation exercises provided in workbooks or portable mp3 format (Allexandre et al., 2016); use of university's virtual learning facility (Cavanagh et al., 2013); obtaining participants' suggestions for integrating mindfulness into everyday life (Wahbeh et al., 2016); flash animated computer-based exercises (Glueck and Maercker, 2011); and message boards with pre-specified discussion threads (Morledge et al., 2013).
3.2.4. Outcomes
Perceived-stress differences, pre- and post-intervention was one of the primary outcomes in seven RCTs, while all eight measured mindfulness pre- and post-intervention as an outcome. Older adults' adherence to the online mindfulness training was the primary outcome measure in Wahbeh et al.'s pilot study (Wahbeh et al., 2016) which reported perceived-stress as a secondary outcome. Seven RCTs measured perceived-stress on the Perceived-Stress Scale (PSS) (Cohen, 1986); Gluck et al. used the Perceived-stress Questionnaire (PSQ) (Levenstein et al., 1993). The Five Facet Mindfulness Questionnaire (FFMQ) (Baer et al., 2008) measured mindfulness in four studies and the Mindful Attention Awareness Scale (MAAS) (MacKillop and Anderson, 2007) in two; Freiburg Mindfulness Inventory (FMI) (Kohls et al., 2009, Walach et al., 2006) or Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) (Feldman et al., 2007) were utilized in two studies. Regarding the studies that used the same scoring system for chosen questionnaires at all time points, the differences in scale did not influence the effect size, which was calculated based on standardized mean difference. Also, each RCT measured more outcomes than this meta-analysis evaluated (Appendix-2).
3.2.5. Risk of bias within studies
Refer to Table 2.
Table 2.
Risk of bias within individual studies.
| Author (year) | Blinding of outcome measures | Allocation concealment | Groups were Comparable on outcome measures at the baseline | Description of dropouts and withdrawals | Intent to treat analysis |
|---|---|---|---|---|---|
| Aikens et al. (2014) | Yes | Yes | Yes | Yes | Yes |
| Allexandre et al. (2016) | Yes | Yes | Yes | Yes | Yes |
| Cavanagh et al. (2013) | Yes | Yes | Yes | No | Yes |
| Glueck and Maercker (2011) | Yes | No | No | No | Yes |
| Mak et al. (2015) | Yes | Yes | No | No | Yes |
| Morledge et al. (2013) | Yes | Yes | Yes | Yes | Yes |
| Wahbeh et al. (2016) | Yes | No | Yes | Yes | Yes |
| Wolever et al. (2012) | Yes | Yes | Not reported | Yes | Yes |
3.2.6. Results of individual studies
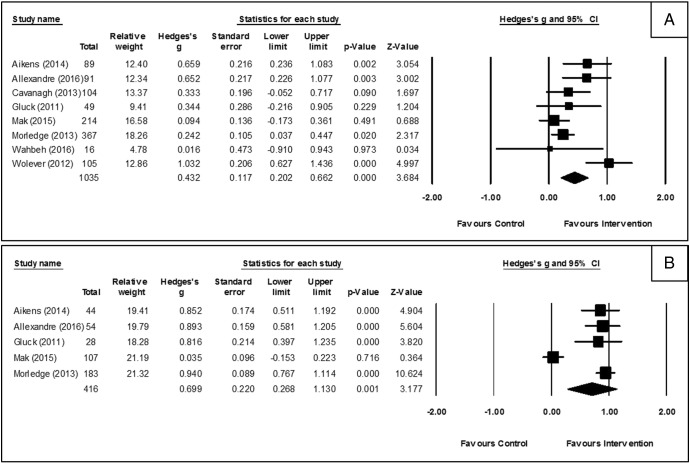
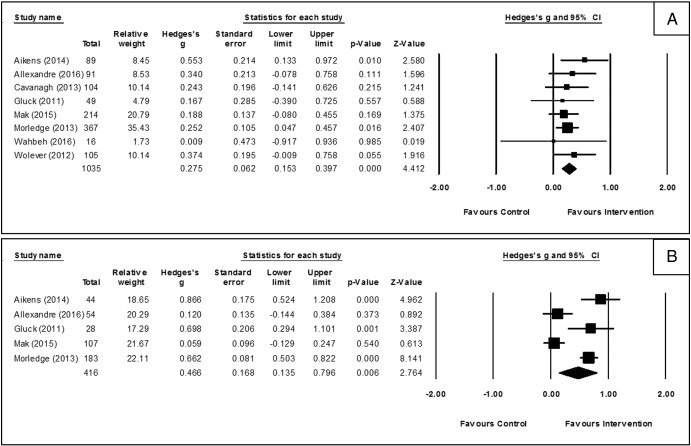
All eight RCTs reported essential data that allowed effect-size calculation for perceived-stress and mindfulness pre- and post-intervention (Table 1). Mean mindfulness scores and standard deviations of Aikens et al. were estimated, using means and standard deviations reported for each facet of the FFMQ. As only three studies evaluated control group at follow-up (Allexandre et al., 2016, Mak et al., 2015, Morledge et al., 2013), the corresponding effect-size estimation utilized comparison of intervention group baseline and follow-up data. Table 1 demonstrates perceived-stress and mindfulness mean scores of intervention and control groups pre- and post-intervention plus at follow-up, if available. Fig. 2 and Fig. 3 present estimated effect-size (Hedges' g) and confidence interval for perceived-stress and mindfulness, respectively, in all included studies, as well as Z-value, statistical significance, and assigned random weight for each.
Fig. 2.
Forest plot for intervention effects on perceived stress: pre-post between-group effects post-intervention and pre-post within-group effects at follow-up.
Fig. 3.
Forest plot for intervention effects on mindfulness: pre-post between-group effects post-intervention and pre-post within-group effects at follow-up.
3.3. Synthesis of results
Meta-analysis consisted of pre-post between-group effects for perceived-stress and mindfulness, estimated post-intervention, and pre-post within-group effects, estimated at follow-up time point. Note that these two types of effect measures cannot be compared because: effect-size estimation method was different, and only five studies were included in the effect-size estimation at follow-up assessment compared to eight studies at post-intervention assessment (Table 1). This analysis considered Hedges' g < 0.10 as no-effect, 0.10–0.29 as small-effect, 0.30–0.49 as medium-effect, and ≥ 0.50 as large-effect; also, I2-values 25% as low-heterogeneity, 50% as moderate-heterogeneity, and 75% as high-heterogeneity (Borenstein et al., 2010, Cohen, 1988, Higgins et al., 2003).
3.3.1. Effects on perceived-stress
Pooled analysis of eight RCTs using random effects, POMI, with comparison control groups, demonstrated a medium effect in reducing perceived-stress (g = 0.432; 95%CI = 0.205–0.669; p = 0.0002); however, 95% confidence interval cutting across 0.30 indicated some probability of having a small effect (Fig. 2). Heterogeneity was moderate (Q = 19.980; p = 0.005; I2 = 64.964); no outlier was detected. Deletion of the small pilot study (N = 16) (Wahbeh et al., 2016) which involved elderly participants (mean age = 76.2 years), increased the effect (g = 0.454; 95%CI = 0.214–0.695; p < 0.0001), but also increased heterogeneity level (Q = 19.391; p = 0.004; I2 = 69.057). In the pooled intervention group analysis of the five RCTs having follow-up periods, interventions were associated with a large effect in reducing perceived-stress from baseline to several weeks or months after conclusion (g = 0.699; 95%CI = 0.268–1.130; p = 0.0001); but, 95% confidence interval cutting across 0.30 indicated some probability of having even a small effect. However, heterogeneity was high (Q = 55.786; p < 0.0001; I2 = 92.830) with an outlier present (Mak et al., 2015) (Fig. 2). Outlier deletion further increased effect-size (g = 0.906; 95%CI = 0.775–1.038; p < 0.0001) and substantially reduced heterogeneity (Q = 0.433; p = 0.933; I2 = 0).
3.3.2. Effects on mindfulness
In the pooled analysis, POMI groups, compared to controls, demonstrated a small effect in improving mindfulness (g = 0.276; 95%CI = 0.154–0.399; p < 0.0001) (Fig. 3). Level of heterogeneity was low (Q = 2.961; p = 0.889; I2 = 0) with no outlier detected. Omission of the Wahbeh et al. (2016) study slightly increased the effect (g = 0.279; 95%CI = 0.156–0.402; p < 0.0001); heterogeneity remained low (Q = 2.655; p = 0.851; I2 = 0). Interventions were associated with a medium effect in improving mindfulness among intervention group participants from baseline to several weeks or months after conclusion (g = 0.473; 95%CI = 0.138–0.807; p = 0.0056); however, 95% confidence interval cutting across 0.30 indicated some probability of having a small effect. High heterogeneity was observed (Q = 36.348; p < 0.0001; I2 = 88.995) with no outlier detected (Fig. 3).
3.4. Risk of bias across studies
Meta-analysis revealed a moderate and low level of heterogeneity for intervention effects on perceived-stress and mindfulness, respectively. Heterogeneity was high for mindfulness effects of interventions at follow-up. Two funnel-plots were created to examine if heterogeneity was related to publication bias. In the funnel-plot demonstrating intervention effect on perceived-stress, the plot bottom contains only one study (Wahbeh et al., 2016) making the plot asymmetrical. However, this small pilot study had much lower than average effect, suggesting the absence of publication bias. Furthermore, use of Duval and Tweedie's trim-and-fill method (Rothstein et al., 2005) did not change point estimate of the random effects model, indicating no missing studies to the right side of the mean effect in the funnel-plot. Distribution of the mindfulness effect of studies appears similar to that for perceived-stress. However, the trim-and-fill method changed the point estimate of random effects model (from 0.275 to 0.280), suggesting one missing study to the right of the mean effect in the funnel-plot (i.e., underestimation of effects, not overestimation).
3.5. Additional analyses
Meta-regression was performed to identify any relationship between mean age of study participants and effect-size for perceived-stress and mindfulness separately. Wahbeh et al. (mean age of 76.2 years) (Wahbeh et al., 2016) was excluded as an outlier. With no reported mean age, Aikens et al. and Morledge et al. (2013) were also excluded. For perceived-stress, mean age of participants in the meta-regression had a positive, significant association with the intervention effect (slope = 0.0375; 95%CI = 0.0177–0.0574; Z = 3.7; p = 0.0002). However, mean age had no significant relationship with the mindfulness effect. For both perceived-stress and mindfulness, meta-regression revealed no association between the percentage of females in the sample and intervention effect.
4. Conclusions
4.1. Summary of evidence
This meta-analysis summarized the effect of POMI, conducted as RCT, on reduction of perceived-stress (primary outcome) and mindfulness (secondary outcome) in non-clinical populations, both immediately after intervention (compared with control) and at extended follow-up (compared with baseline). Extensive literature search yielded eight RCTs conducted for preventive purposes: to reduce stress, increase mindfulness, improve mental well-being, and enhance work or academic performance. Participants of all included RCTs were, predominantly, female adults. Immediately following the intervention period for comparisons between groups, pooled analysis found significant medium effect-size for perceived-stress, with moderate heterogeneity and significant, but small, mindfulness effect-size with low heterogeneity. Intervention group post-intervention follow-up score comparisons with baseline found a significant large effect for perceived-stress with low heterogeneity (after removal of outlier) and significant medium effect for mindfulness with high heterogeneity. Across studies, intervention effects on perceived stress and mindfulness had a strong positive correlation (r = 0.77).
Seven interventions used simplified protocols of MBSR, originally developed by Kabat-Zinn as an 8-week intervention of face-to-face sessions (2.5 h/week) and home practice exercises (45–60 min/day) plus an all-day weekend class (Kabat-Zinn et al., 1985, Kabat-Zinn et al., 1992), previously found to effectively reduce stress in both clinical and non-clinical populations (Grossman et al., 2004, Shapiro et al., 1998). Medium effects for perceived-stress (g = 0.44), in comparison with previously found effects from reviews of traditional MBSR interventions (g = 0.32 in Bohlmeijer et al. and g = 0.56 in DeVibe et al.) (Bohlmeijer et al., 2010, De Vibe et al., 2012, Gotink et al., 2015), suggested that MBSR concepts and protocols can be modified and simplified for online implementation with comparable effectiveness. Moreover, large effects for perceived-stress at follow-up found through this meta-analysis suggested potential long-term impacts of POMI; whether attributable to subjects' continuing use of intervention websites or integration of learned stress management practices into daily living has not been determined.
Compared to prior syntheses of literature regarding MBSR mindfulness effects (g = 0.70, DeVibe et al.) (De Vibe et al., 2012) and perceived-stress effects found in this analysis, mindfulness effects were much smaller when assessed post-intervention (g = 0.276). Low heterogeneity indicated this as a common POMI issue. Consequently, findings suggested that POMI, while effective for stress reduction, are not equally effective as conventional face-to-face mindfulness interventions for improving participants' mindfulness. However, medium effects for mindfulness at follow-up found through this meta-analysis suggested that mindfulness skills, learned online, were cultivated slowly and sustainably.
This meta-analysis found substantial differences among studies regarding design, setting, participants' age, male/female ratio, intervention characteristics, and outcome measures that possibly can influence effect-size. For instance, an increased effect after deletion of Wahbeh et al. (2016) indicated that the intervention effect on stress may be underestimated when elderly participants are included with young and middle-aged participants. Additionally, meta-regression findings suggested that effect was greater for middle-aged than young participants. Furthermore, previous meta-analysis of psychotherapy interventions demonstrated that participants' health conditions and symptoms influence effect-size (Barak et al., 2008). However, future studies should compare the effect-size differences associated with intervention features (i.e., intervention content and duration, sessions/week, session length, feedback tailored or not) and POMI study settings (i.e., academia, workplace, and community).
Effect-size differences related to participants' compliance should be explored. Unlike POMI, when online mindfulness interventions are conducted as assisted treatment, rehabilitation or palliative care for diagnosed medical conditions such as irritable bowel syndrome, anxiety disorder, chronic pain, and cancer, participant motivation and adherence are presumably high (Ljotsson et al., 2011). But, for POMI, the current study found up to 67% of loss to follow-up in post-intervention and follow-up assessment Morledge et al. (2013). The most important question is how to improve participants' adherence and retention when participants' motivation and need are presumably low in the absence of diagnosed medical conditions. This common barrier to preventive interventions can potentially be reduced in POMI through technological advances that make interventions more attractive and user-friendly (e.g. smartphone app and tailored professional feedback). However, considering the fact that providing tailored feedback requires substantial amounts of human and financial resources, intervention researchers should evaluate effect-size differences between automated feedback and human feedback contexts (Schulz et al., 2014). Most importantly, researchers may explore which intervention features are more effective in a given study setting.
4.2. Limitations
This study had several limitations. Only eight RCTs were eligible for inclusion in this meta-analysis and, as with any review, study population, study quality, intervention, and outcome definitions in this meta-analysis differed across studies (see Table 2 for risk of bias within studies). In addition, only four studies (Aikens, Cavanagh, Gluck and Maercker, and Wolever) fully or partly reported findings from per-protocol analysis. Aikens and Cavanagh did not separately report sample sizes for those who were randomized and who completed their baseline assessment. Because of few eligible studies, subgroup analysis by intervention features and POMI study settings could not be performed. Half of the studies had high loss to follow-up intervention group rates and none adequately reported about intervention adherence of participants. Only five studies had variable length follow-up periods and only three followed-up the control group, hence, estimated effect-sizes, especially for follow-up assessment, should be cautiously interpreted. A considerable level of heterogeneity and an outlier were detected; however, publication bias found for mindfulness outcomes led to underestimation of effects, not overestimation. Finally, outcomes other than perceived-stress and mindfulness, diverse across studies (Appendix-2), were excluded from meta-analysis.
4.3. Implications for practice
Empirical evidence suggested that mental health interventions are effectively delivered online (Barak et al., 2009, Ybarra and Eaton, 2005). Although previous meta-analyses infrequently included some studies of online mindfulness interventions (Goyal et al., 2014), it has been assumed that this is the first meta-analysis which estimated the effects of exclusively POMI on perceived-stress and mindfulness in non-clinical populations. Above findings suggest that POMI, designed for volunteers from academic, workplace, or community settings, substantially reduced stress, with highest effects for middle-aged individuals, and, to some extent, improved mindfulness. Given increased digital access (Zickuhr and Smith, 2012), especially among the young and middle-aged in academic and workplace settings (Pew Research Center's Internet and American Life Project, 2012), POMI can be a more convenient and cost-effective strategy, compared to traditional face-to-face interventions, especially for busy and, consequently, more vulnerable, hard-to-reach, but digitally-accessible, populations (Barak et al., 2009).
4.4. Implications for research
Two key areas for future RCTs on POMI were identified: 1) comparisons between intervention effects on sample subgroups, whenever applicable and possible, e.g., by age, sex, income, education, and occupation; 2) comparison of POMI to face-to-face mindfulness interventions with approximately similar content, involving a control group. Since none of the reviewed studies sought to measure the relationship between mindfulness and stress before and after intervention, this can also be a possible future direction for research. Researchers should be encouraged to report essential details of methodology (e.g., blinding) and online intervention (e.g., non-adherence issues). It is also recommended to include a follow-up period post-intervention for all groups with adequate reporting of information, including intervention participants' continuing practice of learned mindfulness exercises. Furthermore, solicitation and reporting of critical feedback from intervention participants is crucial. Finally, despite youths' increased digital access (Pew Research Center's Internet and American Life Project, 2012) and mind-body practices (Black et al., 2015, Zenner et al., 2014), the effectiveness of POMI in adolescents remains unexplored, warranting investigation.
The following are the supplementary data related to this article.
Complete electronic database search strategy for MEDLINE.
Characteristics of randomized controlled trials and preventive online mindfulness interventions included in the meta-analysis.
Conflicts of interest
No conflicts of interest were reported by the authors of this paper.
No financial disclosures were reported by the authors of this paper.
Transparency document
Transparency document.
Acknowledgments
We thank Godfred Antwi for his contribution to data extraction from electronic databases. WJ conceptualized the study, conducted the literature review, and analyzed data. DL prepared the initial drafts of the paper. RE conducted the literature review. MT reviewed and approved the paper. All authors were involved in writing of the paper.
Footnotes
The Transparency document associated with this article can be found, in online version.
References
- Aikens K.A., Astin J., Pelletier K.R. Mindfulness goes to work impact of an online workplace intervention. J. Occup. Environ. Med. 2014;56(7):721–731. doi: 10.1097/JOM.0000000000000209. [DOI] [PubMed] [Google Scholar]
- Allexandre D., Bernstein A.M., Walker E., Hunter J., Roizen M.F., Morledge T.J. A web-based mindfulness stress management program in a corporate call center: a randomized clinical trial to evaluate the added benefit of onsite group support. J. Occup. Environ. Med. 2016;58(3):254–264. doi: 10.1097/JOM.0000000000000680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer R.A., Smith G.T., Hopkins J., Krietemeyer J., Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer R.A., Smith G.T., Lykins E. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Barak A., Hen L., Boniel-Nissim M., Shapira N. A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. J. Technol. Hum. Serv. 2008;26(2–4):109–160. [Google Scholar]
- Barak A., Klein B., Proudfoot J.G. Defining internet-supported therapeutic interventions. Ann. Behav. Med. 2009;38(1):4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- Barnes V.A., Kristeller J.L., Johnson M.H. Impact of mindfulness-based eating awareness on diet and exercise habits in adolescents. Int. J. Complement. Alt. Med. 2016;3(2):1–7. doi: 10.15406/ijcam.2016.03.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black L.I., Clarke T.C., Barnes P.M., Stussman B.J., Nahin R.L. Use of complementary health approaches among children aged 4–17 years in the United States: National Health Interview Survey, 2007–2012. National Health Statistics Reports. 2015;(78):1–19. [PMC free article] [PubMed] [Google Scholar]
- Bohlmeijer E., Prenger R., Taal E., Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J. Psychosom. Res. 2010;68(6):539–544. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- Brown K.W., Ryan R.M. The benefits of being present: mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Cavanagh K., Strauss C., Cicconi F., Griffiths N., Wyper A., Jones F. A randomised controlled trial of a brief online mindfulness-based intervention. Behav. Res. Ther. 2013;51(9):573–578. doi: 10.1016/j.brat.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Chiesa A. Vipassana meditation: systematic review of current evidence. J. Altern. Complement. Med. 2010;16(1):37–46. doi: 10.1089/acm.2009.0362. [DOI] [PubMed] [Google Scholar]
- Clarke T.C., Black L.I., Stussman B.J., Barnes P.M., Nahin R.L. Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Health Statistics Reports. 2015;(79):1–16. [PMC free article] [PubMed] [Google Scholar]
- Cochrane Consumers and Communication Review Group . The Cochrane Collaboration; UK: 2015. Data Extraction Template for Included Studies London. [Google Scholar]
- Cohen S. Contrasting the hassles scale and the perceived stress scale - whos really measuring appraised stress. Am Psychol. 1986;41(6):716–718. [Google Scholar]
- Cohen J. Lawrence Erlbaum Associates; New-York: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Cohen S., Williamson G.M. 1988. Perceived Stress in a Probability Sample of the United-States. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cohen-Katz J., Wiley S., Capuano T., Baker D.M., Deitrick L., Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout: a qualitative and quantitative study, part III. Holist. Nurs. Pract. 2005;19(2):78–86. doi: 10.1097/00004650-200503000-00009. [DOI] [PubMed] [Google Scholar]
- Biostat, Inc.; Englewood, NJ: 2016. Comprehensive Meta-Analysis (CMA) Version-3 [computer program]. Version 3. [Google Scholar]
- Cutshall S.M., Wentworth L.J., Wahner-Roedler D.L. Evaluation of a biofeedback-assisted meditation program as a stress management tool for hospital nurses: a pilot study. Explore (NY) 2011;7(2):110–112. doi: 10.1016/j.explore.2010.12.004. [DOI] [PubMed] [Google Scholar]
- De Vibe M., Bjørndal A., Tipton E., Hammerstrøm K.T., Kowalski K. 2012. Mindfulness Based Stress Reduction (MBSR) for Improving Health, Quality of Life, and Social Functioning in Adults. [Google Scholar]
- Feldman G., Hayes A., Kumar S., Greeson J., Laurenceau J.-P. Mindfulness and emotion regulation: the development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) J. Psychopathol. Behav. Assess. 2007;29(3):177–190. [Google Scholar]
- Glueck T.M., Maercker A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry. 2011;11 doi: 10.1186/1471-244X-11-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh J., Pfeffer J., Zenios S.A. The relationship between workplace stressors and mortality and health costs in the United States. Manag. Sci. 2016;62(2):608–628. [Google Scholar]
- Gotink R.A., Chu P., Busschbach J.J.V., Benson H., Fricchione G.L., Hunink M.G.M. Standardised mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0124344. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Goyal M., Singh S., Sibinga E.M.S. Meditation programs for psychological stress and well-being a systematic review and meta-analysis. JAMA Intern. Med. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P., Niemann L., Schmidt S., Walach H. Mindfulness-based stress reduction and health benefits - a meta-analysis. J. Psychosom. Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Gunaratana H. Wisdom Publications; Boston: 1993. Mindfulness in Plain English. [Google Scholar]
- Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J., Lipworth L., Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J. Behav. Med. 1985;8(2):163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J., Massion A.O., Kristeller J. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am. J. Psychiatr. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Kemper K.J., Lynn J., Mahan J.D. What is the impact of online training in mind-body skills? J. Evid Based Complement. Alternat. Med. 2015;20(4):275–282. doi: 10.1177/2156587215580882. [DOI] [PubMed] [Google Scholar]
- Kitagawa J.M. In: Mahāyāna Buddhist Meditation: Theory and Practice. Kiyota M., editor. Vol. 1979. 1979. p. 3. [Google Scholar]
- Kohls N., Sauer S., Walach H. Facets of mindfulness - results of an online study investigating the Freiburg mindfulness inventory. Personal. Individ. Differ. 2009;46(2):224–230. [Google Scholar]
- Kristeller J.L., Hallett C.B. An exploratory study of a meditation-based intervention for binge eating disorder. J. Health Psychol. 1999;4(3):357–363. doi: 10.1177/135910539900400305. [DOI] [PubMed] [Google Scholar]
- Kristeller J.L., Wolever R.Q. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eat. Disord. 2011;19(1):49–61. doi: 10.1080/10640266.2011.533605. [DOI] [PubMed] [Google Scholar]
- Kristeller J.L., Baer R., Quillian-Wolever R. Mindfulness-based Approaches to Eating Disorders. In: Baer R., editor. Mindfulness-based approaches to eating disorders. Guilford Press; New York: 2006. [Google Scholar]
- Krusche A., Cyhlarova E., Williams J.M.G. Mindfulness online: an evaluation of the feasibility of a web-based mindfulness course for stress, anxiety and depression. BMJ Open. 2013;3(11):10. doi: 10.1136/bmjopen-2013-003498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W., Watkins E., Holden E. How does mindfulness-based cognitive therapy work? Behav. Res. Ther. 2010;48(11):1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Levenstein S., Prantera C., Varvo V. Development of the perceived stress questionnaire - a new tool for psychosomatic research. J. Psychosom. Res. 1993;37(1):19–32. doi: 10.1016/0022-3999(93)90120-5. [DOI] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ljotsson B., Hedman E., Lindfors P. Long-term follow-up of internet-delivered exposure and mindfulness based treatment for irritable bowel syndrome. Behav. Res. Ther. 2011;49(1):58–61. doi: 10.1016/j.brat.2010.10.006. [DOI] [PubMed] [Google Scholar]
- Ly K.H., Truschel A., Jarl L. Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: a randomised controlled trial. BMJ Open. 2014;4(1) doi: 10.1136/bmjopen-2013-003440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J., Anderson E.J. Further psychometric validation of the mindful attention awareness scale (MAAS) J. Psychopathol. Behav. Assess. 2007;29(4):289–293. [Google Scholar]
- Mak W.W.S., Chan A.T.Y., Cheung E.Y.L., Lin C.L.Y., Ngai K.C.S. Enhancing web-based mindfulness training for mental health promotion with the health action process approach: randomized controlled trial. J. Med. Internet Res. 2015;17(1) doi: 10.2196/jmir.3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Michel A., Bosch C., Rexroth M. Mindfulness as a cognitive-emotional segmentation strategy: An intervention promoting work-life balance. J. Occup. Organ. Psychol. 2014;87(4):733–754. [Google Scholar]
- Morledge T.J., Allexandre D., Fox E. Feasibility of an online mindfulness program for stress management-a randomized, controlled trial. Ann. Behav. Med. 2013;46(2):137–148. doi: 10.1007/s12160-013-9490-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray G., Leitan N.D., Berk M. Online mindfulness-based intervention for late-stage bipolar disorder: pilot evidence for feasibility and effectiveness. J. Affect. Disord. 2015;178:46–51. doi: 10.1016/j.jad.2015.02.024. [DOI] [PubMed] [Google Scholar]
- Pew Research Center's Internet & American Life Project . Pew Research Center; 2012. Two-thirds of Young Adults and Those With Higher Income Are Smartphone Owners. [Google Scholar]
- Reibel D.K., Greeson J.M., Brainard G.C., Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen. Hosp. Psychiatry. 2001;23(4):183–192. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- Rothstein H.R., Sutton A.J., Borenstein M. 1-7. 2005. Publication Bias in Meta-analysis. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments. [Google Scholar]
- Sauer S., Walach H., Schmidt S. Assessment of mindfulness: review on state of the art. Mindfulness. 2013;4(1):3–17. [Google Scholar]
- Schulz D.N., Smit E.S., Stanczyk N.E., Kremers S.P.J., de Vries H., Evers S. Economic evaluation of a web-based tailored lifestyle intervention for adults: findings regarding cost-effectiveness and cost-utility from a randomized controlled trial. J. Med. Internet Res. 2014;16(3):383–400. doi: 10.2196/jmir.3159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro S.L., Schwartz G.E., Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J. Behav. Med. 1998;21(6):581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- Stussman B.J., Black L.I., Barnes P.M., Clarke T.C., Nahin R.L. Wellness-related use of common complementary health approaches among adults: United States, 2012. National Health Statistics Reports. 2015;(85):1–12. [PubMed] [Google Scholar]
- Thompson S.G., Higgins J.P.T. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002;21(11):1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- Tsai S.L., Crockett M.S. Effects of relaxation training, combining imagery, and meditation on the stress level of Chinese nurses working in modern hospitals in Taiwan. Issues Ment. Health Nurs. 1993;14(1):51–66. doi: 10.3109/01612849309006890. [DOI] [PubMed] [Google Scholar]
- Wahbeh H., Goodrich E., Oken B.S. Internet-based mindfulness meditation for cognition and mood in older adults: a pilot study. Altern. Ther. Health Med. 2016;22(2):44–53. [PMC free article] [PubMed] [Google Scholar]
- Walach H., Buchheld N., Buttenmuller V., Kleinknecht N., Schmidt S. Measuring mindfulness - the Freiburg Mindfulness Inventory (FMI) Personal. Individ. Differ. 2006;40(8):1543–1555. [Google Scholar]
- Wolever R.Q., Bobinet K.J., McCabe K. Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. J. Occup. Health Psychol. 2012;17(2):246–258. doi: 10.1037/a0027278. [DOI] [PubMed] [Google Scholar]
- Ybarra M.L., Eaton W.W. Internet-based mental health interventions. Ment. Health Serv. Res. 2005;7(2):75–87. doi: 10.1007/s11020-005-3779-8. [DOI] [PubMed] [Google Scholar]
- Zenner C., Herrnleben-Kurz S., Walach H. Mindfulness-based interventions in schools - a systematic review and meta-analysis. Front. Psychol. 2014;5 doi: 10.3389/fpsyg.2014.00603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zernicke K.A., Campbell T.S., Speca M. The eCALM Trial-eTherapy for cancer appLying mindfulness: online mindfulness-based cancer recovery program for underserved individuals living with cancer in Alberta: protocol development for a randomized wait-list controlled clinical trial. BMC Complement. Altern. Med. 2013;13:10. doi: 10.1186/1472-6882-13-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zickuhr K., Smith A. Washington, D.C; Pew Research Center: 2012. Digital Differences: Pew Internet and American Life Project. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Complete electronic database search strategy for MEDLINE.
Characteristics of randomized controlled trials and preventive online mindfulness interventions included in the meta-analysis.
Transparency document.