Abstract
Pulmonary infarction is an infrequent complication of pulmonary embolism due to the dual blood supply of the lung. Autopsy studies have reported cavitation to occur in only 4–5% of all pulmonary infarctions with an even smaller proportion of these cases becoming secondarily infected. Patients with infected cavitating pulmonary infarction classically present with fever, positive sputum culture, and leukocytosis days to weeks following acute pulmonary embolism. We describe a rare case of acute pulmonary embolism with pulmonary infarction leading to cavitation and subsequent abscess formation requiring left lower lobe resection.
1. Introduction
Acute pulmonary embolism (PE) leads to pulmonary infarction in only 10% of cases because of the dual blood supply of the lungs [1]. Pulmonary infarction causes cavitation in 4–7% of cases [2]. Infarct size larger than 4 cm is a strong risk factor for aseptic necrosis leading to pulmonary cavitation [3]. Infected pulmonary cavitation can lead to pulmonary abscess in a small subset of patients and these patients classically present with fever, leukocytosis, and positive sputum; however it is uncommon to have all 3. We present a rare cause of acute PE leading to cavitation and subsequent pulmonary abscess which required left lower lobe resection.
2. Case Presentation
A previously healthy 62-year-old male presented to the emergency department with complaints of chest pain and dyspnea. CT pulmonary angiogram (CTPA) revealed acute pulmonary emboli within the left lower lobe segmental and subsegmental pulmonary arteries. Imaging also showed a left basilar peripheral groundglass and consolidative opacity likely representing pulmonary infarction (Fig. 1). Intravenous heparin and warfarin therapy were initiated and the patient's hospital course was otherwise unremarkable. Because the patient's venous thromboembolism was unprovoked, he was discharged with a plan for indefinite anticoagulation. The patient returned for a routine outpatient follow-up 3 weeks later with severe cough, generalized malaise, and fatigue. Initial laboratory analysis was unremarkable. A chest radiograph showed interval development of a left lower lobe consolidation with an air-fluid level and pleural effusion (Fig. 2). CTPA demonstrated a large cavitary lesion of the left lower lobe and a loculated pleural fluid collection (Fig. 3). A pulmonary embolus was still evident in the segmental pulmonary artery of the posterior-basilar segment of the left lower lobe. Cardiothoracic surgery was concerned that immediate surgical resection may contaminate the surgical field so intravenous antibiotics and percutaneous drainage of the lung abscess were recommended. The patient was started on intravenous vancomycin and piperacillin/tazobactam and a percutaneous drain was inserted by interventional radiology after 36 hours of antibiotics. The patient clinically decompensated with these treatment modalities, so the patient underwent a left thoracotomy and lysis of adhesions with resection of the left lower lobe. On surgical pathology, the entire left lower lobe was an abscess cavity with copious amounts of purulent material. The procedure was tolerated well and the patient was transitioned to oral antibiotics. Cultures obtained from the percutaneous drain and surgical pathology showed no growth of any organisms.
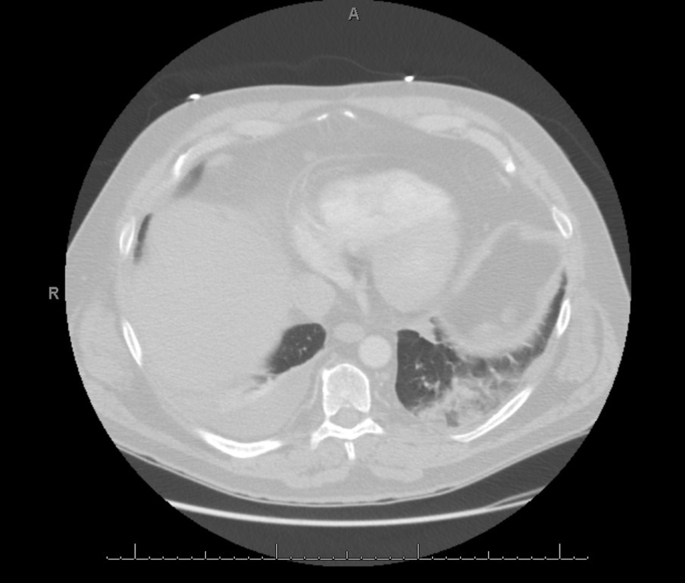
Fig. 1.
Initial CTPA demonstrating a left basilar peripheral opacity, likely representing pulmonary infarction, as well as a contralateral pleural effusion.
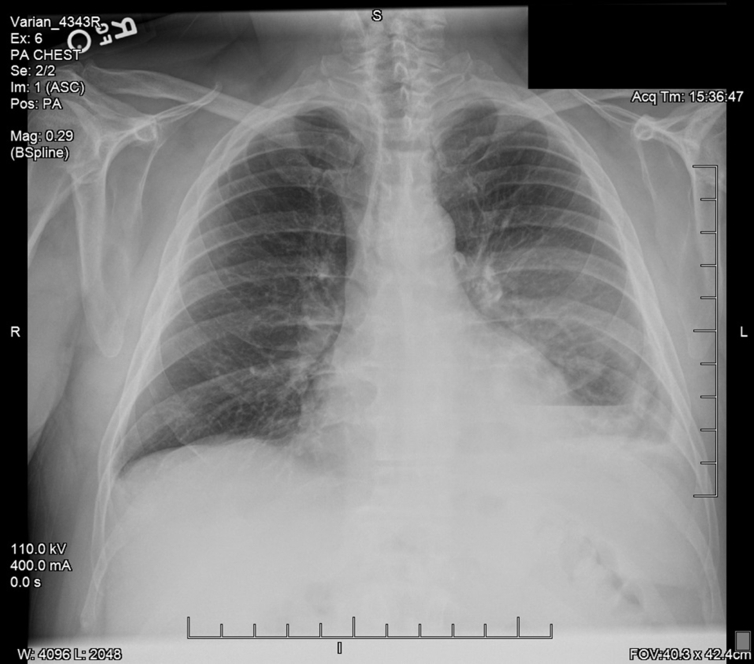
Fig. 2.
Chest radiograph showing the interval development of a left lower lobe consolidation with an air-fluid level and pleural effusion.
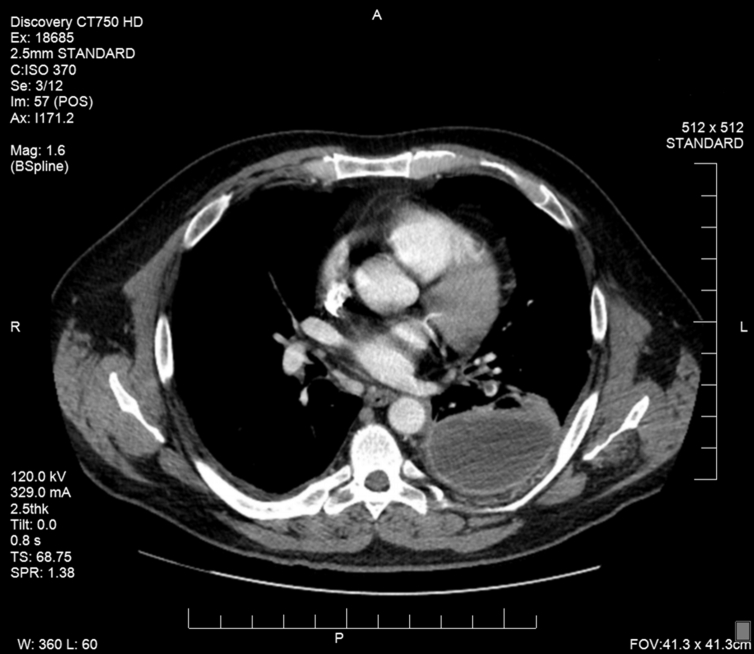
Fig. 3.
Repeat CTPA demonstrating a large cavitary lesion of the left lower lobe with a loculated pleural fluid collection and evidence of a pulmonary embolus in the segmental pulmonary artery of the posterior-basilar segment of the left lower lobe.
3. Discussion
This case radiographically and chronologically highlights the transition of an acute PE with pulmonary infarction to an infected pulmonary cavity with an abscess. This patient's pulmonary infarction size was larger than 4 cm which is a well-known risk factor for pulmonary cavitation. Other risk factors for pulmonary infarction with cavitation include older age, heart failure, and chronic lung disease [2]. Infected pulmonary infarctions lead to cavitation faster than bland infarctions with aseptic necrosis. The mean time to cavitation for an infected pulmonary infarction is 18 days, which is the approximate time interval experienced by our patient [1]. Gram negative organisms are most commonly isolated but positive cultures do not occur in all patients. Our patient was on broad spectrum antibiotics for over 36 hours prior to percutaneous drainage of the left lower lobe abscess which likely affected the culture results. There is a paucity of data on the surgical treatment of infected pulmonary infarction. Some authors have advocated early surgical resection due to of high rates of medical failure which is theorized to be due to the lack of blood supply within the cavity and risk of continued infection [4]. Older case series report high mortality rates for both infected and bland pulmonary cavitation. It is likely that the reported mortality rates are significantly lower in the modern era of medicine due to earlier diagnosis and improved therapies for venous thromboembolism. Clinicians should consider infected cavitating pulmonary infarction in patients with recent PE and symptoms of bacterial pneumonia.
The views expressed are those of the authors and do not reflect the official views or policy of the Department of Defense or its Components.
References
- 1.Rajagopala Srinivas, Devaraj Uma, D’Souza George. Infected Cavitating Pulmonary Infarction. Respir. Care. 2011;56(5):707–709. doi: 10.4187/respcare.00828. [DOI] [PubMed] [Google Scholar]
- 2.Libby L.S., King T.E., LaForce F.M., Schwarz M.I. Pulmonary cavitation following pulmonary infarction. Medicine (Baltimore) 1985;64(5):342–348. doi: 10.1097/00005792-198509000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Wilson A.G., Joseph A.E., Butland R.J. The Radiology of aseptic cavitation in pulmonary infarction. Clin. Radiol. 1986;37:327–333. doi: 10.1016/s0009-9260(86)80263-x. [DOI] [PubMed] [Google Scholar]
- 4.Butler Michael D., Biscardi Frank H., Schain Denise C., Humphries John E., Blow Osbert, Spotnitz William D. Pulmonary resection for treatment of cavitary pulmonary infarction. Ann. Thorac. Surg. 1997;63:849–850. doi: 10.1016/s0003-4975(96)01253-2. [DOI] [PubMed] [Google Scholar]