Abstract
Few studies have examined potential differences between social anxiety disorder (SAD) and generalized anxiety disorder (GAD) in the sensitivity to detect emotional expressions. The present study aims to compare the detection of emotional expressions in SAD and GAD. Participants with a primary diagnosis of GAD (n=46), SAD (n=70), and controls (n=118) completed a morph movies task. The task presented faces expressing increasing degrees of emotional intensity, slowly changing from a neutral to a full-intensity happy, sad, or angry expressions. Participants used a slide bar to view the movie frames from left to right, and to stop at the first frame where they perceived an emotion. The frame selected thus indicated the intensity of emotion required to identify the facial expression. Participants with GAD detected the onset of facial emotions at lower intensity of emotion than participants with SAD (p=0.002) and controls (p=0.039). In a multiple regression analysis controlling for age, race, and depressive symptom severity, lower frame at which the emotion was detected was independently associated and GAD diagnosis (B = −5.73, SE = 1.74, p<0.01). Our findings suggest that individuals with GAD exhibit enhanced detection of facial emotions compared to those with SAD or controls.
Keywords: Anxiety/Anxiety disorders, GAD/generalized anxiety disorder, SAD/social anxiety disorder/social phobia, Cognition, Assessment/Diagnosis
Introduction
Social anxiety disorder (SAD) and generalized anxiety disorder (GAD) are common anxiety conditions that together affect nearly 22 million individuals in the U.S. in a given year (Kessler, Chiu et al. 2005). While much is understood about each anxiety condition, much less in known about how core aspects of their pathophysiology may differ or overlap. Relatively few studies have directly compared these two conditions across experimental tasks. Given the high comorbidity of these conditions (Kessler, Chiu et al. 2005), overlap in effective treatments (e.g. antidepressants), and often incomplete response with available treatments (Ravindran and Stein 2010), it is important to better understand which characteristics are shared and which are unique.
SAD is a distressing and impairing condition characterized by a persistent fear of embarrassment or humiliation in social or performance situations, (Ruscio, Brown et al. 2008). Individuals with SAD have been consistently shown to exhibit a negative bias in the interpretation of social events (e.g. interpreting ambiguous social events in a negative fashion) (Stopa and Clark 2000). While the pathogenesis of SAD is likely multifactorial (e.g., Hayward, Wilson et al. 2008), it has been proposed that fear of social interactions might be linked in part to the way individuals with SAD perceive facial expressions. For example, individuals with clinical or subclinical SAD appear to exhibit heightened initial vigilance for threatening faces (e.g., Stevens, Rist et al. 2009). Neuroimaging and event-related potential electroencephalographic data suggest greater activation of the amygdala (e.g., Straube, Mentzel et al. 2005) and abnormalities in the early stages of perceptual processing in response to the presentation of threatening faces (e.g., Staugaard 2010). A recent review found that SAD was characterized by a biased information-processing of facial expressions of emotion, including attentional bias away from negative faces, inaccurate labeling of negative emotions, enhanced recognition of negative facial displays, and increased memory for negative emotions (Machado-de-Sousa, Arrais et al. 2010).
Cognitive models may explain the negative interpretation bias in individuals with SAD. Clark and Wells (1995) designed a model suggesting social anxiety persists because of the following elements: individuals are not accurately processing the social situation, are engaging in safety behaviors which prevent disconfirmation of feared outcomes, are negatively influencing other’s behavior toward themselves, and are using their own impression of themselves as the main factor which contributes to the idea that others are negatively evaluating them. Additionally, Rapee and Heimberg (1997) suggest that the negative interpretation bias leads to stronger anxiety in social situation, which leads to increased social phobia.
To date, several studies have examined detection and interpretation of emotional facial expressions in individual with social anxiety, with paradigms using either static facial expressions (e.g., Mullins and Duke 2004), ambiguous facial stimuli (e.g., Jusyte and Schonenberg 2014), or changing facial expression (Joormann and Gotlib 2006, Montagne, Schutters et al. 2006, Heuer, Lange et al. 2010), with mixed results. Among the latter type of studies, one (Joormann and Gotlib 2006) used a time pressured morph movies task to assess potential differences in the intensity of facial expression needed to identify an emotion in individuals with SAD compared to those with depression and healthy controls. In this computer based task, participants were presented with faces expressing increasing degrees of emotional intensity, slowly changing from a neutral to a full-intensity happy, sad or angry expression. They were instructed to stop the movie when they accurately identified the emotion being expressed. While the intensity of emotion required to identify happy and sad expressions did not differ, angry facial expressions were identified “earlier” (i.e. with lower intensity expressions) for those with SAD compared to depressed and control participants. In contrast, other research using a morph movies task with no time restriction reported opposite results with individuals with SAD being less “sensitive” than controls when identifying negative facial expressions (Montagne, Schutters et al. 2006). Finally, other (Heuer, Lange et al. 2010) using a similar experiments, failed to detect a significant difference between high socially anxious individuals and non-anxious controls across three types of facial expressions (angry, happy, and disgust) both with and without time pressure. Methodological differences (e.g., differences in the emotions and faces displayed) may in part explain this discrepancy. However, additional research in SAD is needed to clarify this issue.
Generalized anxiety disorder (GAD), in contrast with the social nature of SAD, involves a pattern of persistent worry and anxiety over a variety of day to day matters and is associated with somatic symptoms including restlessness, fatigue, concentration impairment, irritability, muscle tension, and sleep disturbance (APA 2013). Accumulating evidence has more recently implicated emotion-regulation difficulties in the pathogenesis of GAD. For instance, individuals with GAD have been found to experience reduced tolerance of uncertainty (Dugas, Buhr et al. 2004), impaired ability to accept aversive psychological experiences (Roemer, Salters et al. 2005), and heightened experience of emotions coupled with greater difficulty modulating their emotional experience (Mennin, McLaughlin et al. 2009).
In addition, individuals with GAD have been suggested to present both a greater perceived intensity of emotional experiences, and a difficulty identifying primary emotions including anger, sadness, or joy (e.g., Newman, Llera et al. 2013). It is thus possible that difficulty in perceiving the emotions in GAD extends to the emotion recognition of other’s expressions.
Despite distinct clinical presentations, some cross-sectional and longitudinal comorbidity data suggest that GAD and SAD might reflect alternative presentations of a single underlying psychopathology (Bruce, Machan et al. 2001). Prior research has also suggested that anxiety may be associated with specific emotion recognition alterations (Easter, McClure et al. 2005). On the other hand, individuals with trait anxiety have been suggested to recognize the facial expression of fear better than controls (Surcinelli, Codispoti et al. 2006). Similar to SAD, individuals with GAD have finally been shown to exhibit greater vigilance for threatening faces relative to neutral faces, compared to normal controls (Bradley, Mogg et al. 1999).
To date, however, no study has examined performance of detection of emotional expressions in GAD, or compared GAD to SAD. If both GAD and SAD shared an underlying anxiety diathesis leading to heightened emotion sensitivity, they should both be associated with detection of emotional expressions at lower intensity of expressions, compared to controls. On the other hand, if heightened sensitivity to facial emotional expression is driven by the social fears inherent in SAD, individuals with SAD should detect emotions earlier than individuals with GAD. Alternately, if heightened sensitivity to facial emotional expression is driven by increased perceived intensity of emotional experiences reported in GAD, then GAD would be associated with enhanced emotion detection, while among those with SAD, a greater internal focus or emotional avoidance would result in reduced attention and later detection of emotions.
The present study aims to compare the detection of emotional expression between individuals with a primary diagnosis of SAD, GAD, and controls. We hypothesized that compared to controls, individuals with SAD and GAD would exhibit earlier detection of angry (threatening) faces (relative to sad and happy).
Methods
Participants
Participants were 116 individuals with a primary anxiety disorder (n=70 with SAD, n=46 with GAD) and 118 healthy controls, aged 18 or older, recruited through advertisement and clinical referral to the Massachusetts General Hospital. Mean (SD) age for the overall sample was 38.45(13.32) years, and 75% (n=128) were men (see Table 1). Psychiatric diagnoses were determined by clinical interviewers certified in administering the Structured Clinical Interview for DSM-IV (First 1994). Exclusions for SAD and GAD participants included lifetime psychosis, bipolar disorder, mental disorder due to a medical condition or substance, current eating disorders, and alcohol or substance use disorders within the past 6 months. Controls could have no DSM-IV Axis I disorders, with the exception of a past history of alcohol or substance use disorders in remission for at least 12 months (n=18; 15%). Fourteen percents (n=10) of those with primary SAD (n=70) had a secondary GAD, while 29% (n=13) of those with primary GAD (n=46), had secondary SAD comorbidity. Current major depressive episode was present among 14% of participants with SAD, and among 9% of those with GAD.
Table 1.
Socio-Demographic and Clinical Characteristics of Individuals with Generalized Anxiety Disorder (n=46), Social Anxiety Disorder (n=70), and Psychiatric Disorder Free Controls (n=118)
| Omnibus p-valuea | p-value for Two-by-Two Post-Hoc Comparisonsb | ||||||
|---|---|---|---|---|---|---|---|
| Controls N=118 |
GAD N=46 |
SAD N=70 |
Controls vs. GAD | Controls vs. SAD | GAD vs. SAD | ||
| Age, years, mean (SD) | 40.4 (13.0) | 40.5 (14.2) | 33.8 (12.3) | 0.002 | 1.000 | 0.021 | 0.003 |
| Sex, % female (n) | 49.2 (58) | 45.7 (21) | 38.6 (27) | 0.37 | 0.687 | 0.159 | 0.449 |
| Race, % white (n) | 68.6 (81) | 89.1 (41) | 82.9 (58) | 0.007 | 0.007 | 0.032 | 0.35 |
| Depressive Symptoms | |||||||
| MADRS, mean (SD) | 1.9 (2.3) [n=103] | 16.1 (5.6) [n=38] | 12.9 (7.0) [n=63] | <0.001 | <0.001 | <0.001 | 0.005 |
| Frame Facial Expression Was Detected | |||||||
| Angry | 42.8 (12.2) | 36.6 (13.2) | 45.4 (13.1) | 0.0029 | 0.026 | 0.648 | 0.002 |
| Happy | 31.4 (14.1) | 24.4 (11.6) | 32.2 (14.8) | 0.0068 | 0.013 | 1.0 | 0.011 |
| Sad | 54.7 (16.6) | 50.4 (14.9) | 60.1 (15.9) | 0.0053 | 0.005 | 0.083 | 0.357 |
Notes:
Between group comparison, Chi2 for categorical variables, and one-way analysis of variance for continuous variables
bonferroni post hoc test for continuous variables
Procedures
All participants completed written informed consent prior to participation, and all study procedures were approved by the Partners IRB. Participants were then assessed for psychiatric diagnoses and eligibility before completing the morph movies experiment. They also completed self report scales assessing their current affective state and psychiatric symptoms before completing the tasks. The morph movies task followed a binocular rivalry task, the results of which have been previously reported (Anderson, Dryman et al. 2013). Participants received $30 financial compensation for participation.
Materials
Morph Movies Task
Detection of emotional expressions was assessed using a morph movies task previously described in detail (Niedenthal, Halberstadt et al. 2000). Briefly, for this task, photographs of actor/models displaying emotions were digitally morphed, with a photograph of the same actor expressing neutral emotion to create 100-frame movies in which a face initially expressing an emotion became gradually neutral. Pictures of 10 happy, sad, angry, and neutral faces of male and female actor–models were selected for this task. These images are part of a larger set of photographs pre-tested on a group of 83 participants who established the validity of the actors’ facial expressions (e.g., Niedenthal, Halberstadt et al. 2000). Morph software (Maxwell, 1994) was used to map a set of anchor points onto an image of an actor with a neutral expression onto the same actor expressing an emotion. Digital movies composed of 100 facial composites, in which the facial expression gradually became more emotional were then produced.
Participants were told they would view movies in which a face initially expressed neutral emotion. They were instructed to slide a bar at the bottom of the screen from left to right, playing each movie at their own speed, and to stop the movie at the first frame where they perceived the face to express an emotion. Participants were also able to slide the bar right to left to decrease emotional intensity. No verbal labels were provided about which emotion they should expect to see. Thus, the principal judgments in this task were non-verbal. Participants clicked the mouse on a button at the bottom of the computer screen to register the frame of expression onset, and a new trial began with a neutral expression. The dependent variable was the frame at which the participant marked the initial facial expression as first visible (frame 1=fully ‘neutral’ expression; frame 99=fully ‘emotional’ expression). Each movie was presented twice, and in a random order to each participant (i.e., 20 neutral-to-angry movie trials, 20 neutral-to-happy movie trials, and 20 neutral-to-sad movie trials).
Psychiatric Assessment
The SCID (First 1994), the most widely used diagnostic instrument for assessing psychiatric disorders was administered by doctoral-level clinicians to confirm that excluded disorders are not present and to document psychiatric and diagnostic history.
Depressive Symptoms
The 10-item clinician-administered Montgomery Asberg Depression Rating Scale (MADRS) is a psychometrically-sound clinician-administered measure of depression (Montgomery and Asberg 1979). Total scores range from 0 to 60 with higher scores reflecting greater depressive symptom severity. The MADRS has been found to be a valid and reliable interview for assessing current depressive symptom severity with high internal consistency (Cronbach’s coefficient alpha in our sample was 0.89), and excellent convergent validity with other measures of depressive symptoms. Here, the MADRS is used as a covariate.
Data Analyses
A series of analyses of variance (ANOVA) with post-hoc Bonferroni tests and chi-square tests were conducted to examine group differences in socio-demographic and clinical variables. In order to examine differences in detection of emotions in SAD vs. GAD vs. control participants, we conducted a mixed-model repeated measures ANOVA, with expression (angry, happy, sad) as the repeated measure, diagnosis as the between subjects factor, and the frame at which the movie was stopped as the dependent variable. Simple effects were also examined for each emotional facial expression (angry, happy, sad) with ANOVA with post-hoc Bonferroni tests. As a follow-up analysis, in order to confirm the effect of GAD on the frame selection to detect emotion, we conducted a multiple regression analysis with the frame at which the emotion was detected as the outcome, and the GAD and SAD diagnoses as predictors, controlling for age, race, and depressive symptom severity. All analyses were performed using Stata 12.1 and the alpha level of significance was set to 0.05 (two-tailed).
Results
Participants’ Characteristics
Participants’ characteristics are reported in Table 1. There was an approximately equal balance of sex across the three groups; however, the three groups differed significantly on age (p=0.002) and race (p=0.007).
Group Differences in Detection of Emotional Expression
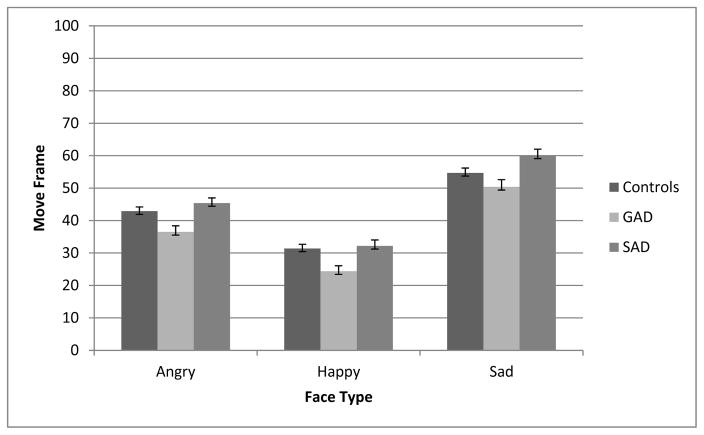
Overall, the frame at which participants stopped the movie was normally distributed, although there were a number of trials in which participants stopped the movie on the first frame (indicating that they saw an emotional expression in the ‘neutral’ face; less than 0.05% of trials) or final frame (maximum expression; 2.86% of trials). Although there was a statistically significant group difference in the number of trials stopped at the first or final frame (2.9% in controls, 3.76% in participants with SAD, and 1.56% in participants with GAD, χ2(2)=28.78, p<0.001), the same overall pattern of findings held when analyses excluded trials that were stopped on the first or last frame. Thus, the data reported here include all trials. Participants detected affective expressions differently depending on their diagnosis (Table 1 and Figure 1). We conducted a mixed-model repeated measures ANOVA, with expression (angry, happy, sad) as the repeated measure, diagnosis as the between subjects factor, and the frame at which the movie was stopped as the dependent variable. Because sphericity assumptions were not met (Mauchly’s W=0.658; p<0.001), Greenhouse-Geisser correction was applied. After inclusion of age, race, and depressive symptom severity as covariates, both the main effect of diagnosis, F(2, 402)=3.0, p<0.05, and the main effect of expression in the movie, F(2, 402)=623.5, p<0.001 were significant, while the interaction between the two factors was not, F(4, 402)=1.65, p=0.18. Bonferroni post hoc tests revealed that all groups required the smaller number of frames to detect happy expressions, followed by angry expressions, and the greatest number of frames to detect for sad expressions (Table 1). The GAD group also detected faces at a lower frame than SAD (p=0.002) and controls (p=0.039) (see Table 1 and, Figure 1).
Figure 1.
Mean Frame Angry, Happy, and Sad Expressions Detected by Individuals with Social Anxiety Disorder, Generalized Anxiety Disorder, and Controls. Error bars Represent Standard Errors.
Association of GAD Diagnoses with Detection of Emotional Expression
A multiple regression analysis (F(5, 606) = 4.99, p<0.001) revealed that lower frame at which the emotion was detected was only independently associated with age (B = -0.11, SE = 0.04, p<0.05), and GAD diagnosis (B = -5.73, SE = 1.74, p<0.01).
Discussion
This study is the first to compare performance in the detection of emotional expression across two anxiety disorders. Furthermore, to our knowledge, no prior studies have examined performance in the detection of emotional expression among individuals with GAD. Participants with a primary diagnosis of GAD required lower intensity of emotion to detect the onset of facial expressions compared to participants with SAD or controls. These group differences were not accounted for by depression symptom severity.
While some have proposed that GAD and SAD might reflect a common underlying pathology (Pine, Cohen et al. 1998, Bruce, Machan et al. 2001), our results suggest that distinct underlying pathophysiological processes regarding emotion detection may be present. Our findings of enhanced detection of emotion in GAD compared to SAD are consistent with recent research showing differences in emotion dysregulation between the disorders. For instance, individuals with GAD appear to experience their emotions more intensely than those with SAD (Turk, Heimberg et al. 2005). Similarly, Blair et al. (2008) found in a functional neuroimaging study different patterns of cerebral activation in response to neutral, fearful, and angry facial expressions between individuals with GAD and SAD. However, their results showed that participants with GAD had a lower level of neural activation in response to the presentation of negative faces (relative to neutral faces) compared to those with SAD. Although seemingly inconsistent, these findings may be explained by contemporary models of GAD which suggest that individuals with GAD both experience heightened negative affect and employ affect-suppressing strategies (i.e., worry), which may explain their increased sensitivity to emotionally-salient facial expressions but reduced neural activation (Mennin, Heimberg et al. 2002, Turk, Heimberg et al. 2005). Future research should examine how different contexts and stimuli impact emotion-regulation strategies used by those with GAD.
Another point to be considered regarding our current findings is that the results may have been impacted by the lack of time pressure in the task. Since the task was not time-pressured and participants could go back and forth through the movie, responses could have stemmed not from early perceptual processes but from late cognitive/response processes. These late processes could be influenced by various factors that may drive GAD participants to select a lower intensity of emotion including more intense feeling of emotions. Individuals with GAD have also been suggested to exhibit a greater perceived intensity of emotional experiences (e.g., Newman, Llera et al. 2013). It is possible for example, that participants with GAD selected a frame with less emotion intensity as a strategy to avoid heightened feeling of emotions. The increased amount of time allowed for decision making exposed participants to an increasingly ambiguous situation without feedback. Prior research suggest that individuals with GAD may exhibit low tolerance of uncertainty (Dugas, Buhr et al. 2004). Although germane to all anxiety disorders (McEvoy and Mahoney 2012), intolerance of uncertainty is particularly pronounced among individuals with GAD relative to those with SAD (Boswell, Thompson-Hollands et al. 2013). Thus, while the nature of worry and anxiety inherent in GAD may have led to detection of emotional faces at lower frame than for SAD or controls, an alternate explanation is that the untimed nature of the task, which allowed individuals to scroll back and forth through the movie, enabled individuals with GAD to be more careful in their assessments and/or greater concern about missed detections led them to report detection with earlier frames. Further studies identifying the specific factors and processes that may explain the unique response strategies used by participants with GAD are thus warranted.
Contrary to our hypotheses, the detection of emotional expression also did not differ between individuals with SAD and controls. These results are consistent with the findings of Heuer et. al. (2010) and Justye & Schonenberg (2014), but at odds with another study (Joormann and Gotlib 2006) that found “earlier” detection of angry faces among SAD compared to controls in a time-pressured morph movie task. One possibility is that individuals with SAD are more sensitive to detecting angry facial expressions only under time pressure. As previously suggested (Staugaard 2010), longer exposure durations to the emotionally salient faces may allow for more detailed processing of the stimuli, thereby diminishing differences between individuals with SAD and controls. In other words, because the affective reaction elicited by the presentation of emotional faces may be short-lived, conscious processing overrides automatic processes (Staugaard 2010). On the other hand, consistent with our findings, Heuer et al. (2010) also failed to observe any differences in emotion detection regardless of time pressure. Additional studies are needed to clarify the role of time pressure in processing emotional expressions.
It is worth noting that happy expressions were detected earlier than angry and sad across all groups. Prior literature has also reported that individuals required a lower intensity of emotion to identify happy expressions compared to other expressions including sadness (Joormann and Gotlib 2006, Schönenberg, Christian et al. 2014). As suggested previously (Barrett and Niedenthal 2004), such findings may reflect the differences in the intensity of the end point emotional expressions displayed across emotion type. Because movie frames are morphed composites of a neutral and an end-point expression each happy, angry, and sad morphed movie contains differing amounts of emotional information at a given frame. An alternative explanation may be that the happy expression was easier to detect since it was the only positive emotion. The other two (angry and sad) were negative and similar to each other. It is possible that participants did not respond to the detection of a change but to the detection of a change that enabled them to differentiate between these two emotions.
Some limitations need to be acknowledged. First, anxiety comorbidities were allowed in the current study, and may have limited the study’s internal validity for cross disorder comparisons. Although the presence of some secondary GAD in the SAD group and vice versa would be more likely to diminish rather than enhance group differences. In addition, regression analyses confirmed the association of GAD with emotion detection at a lower frame. In addition, our design did not allow differentiation of sensitivity to emotion or more simple differences in facial information, and we cannot rule out that participants may have rated visual changes in general (i.e., merely detected facial contrasts). Similarly, as indicated above, the design also did not allow for differentiation between perceptual processes and later processes related to criterion (expectancy, interpretation). Finally, we did not assess intelligence quotient.
Despite these limitations, our findings provide preliminary evidence that GAD might be associated with lower threshold for detection of facial emotions. Although these results warrant replication, they provide evidence in favor of distinct pathophysiological processes between individuals with GAD and SAD. Our findings thus point to the importance of incorporating disorder-specific treatment strategies in the treatment of GAD including emotion regulation training and decreased reliance on detrimental strategies (e.g., worry, avoidance). Future research aiming to identify the specific factors and processes explaining the unique response strategies used by participants with GAD are warranted.
Acknowledgments
The present study was funded by a grant from the Highland Street Foundation. In addition, preparation of this manuscript was supported by a National Institute of Health Director’s Pioneer Award (DP1OD003312), by the U.S. Army Research Institute for the Behavioral and Social Sciences (contract W5J9CQ-11-C-0049), and by grant R01 AG030311 awarded to LFB, as well as grant R01 MH093394 awarded to NMS. The views, opinion, and/or findings contained in this article are solely of the authors and should not be construed as an official Department of the Army of DOD position, policy, or decision.
References
- Anderson E, Dryman MT, Worthington J, Hoge EA, Fischer LE, Pollack MH, Barrett LF, Simon NM. Smiles may go unseen in generalized social anxiety disorder: evidence from binocular rivalry for reduced visual consciousness of positive facial expressions. J Anxiety Disord. 2013;27(7):619–626. doi: 10.1016/j.janxdis.2013.07.004. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5. American Psychiatric Publishing; 2013. [Google Scholar]
- Barrett LF, Niedenthal PM. Valence focus and the perception of facial affect. Emotion. 2004;4(3):266–274. doi: 10.1037/1528-3542.4.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair K, Shaywitz J, Smith BW, Rhodes R, Geraci M, Jones M, McCaffrey D, Vythilingam M, Finger E, Mondillo K, Jacobs M, Charney DS, Blair RJ, Drevets WC, Pine DS. Response to emotional expressions in generalized social phobia and generalized anxiety disorder: evidence for separate disorders. Am J Psychiatry. 2008;165(9):1193–1202. doi: 10.1176/appi.ajp.2008.07071060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boswell JF, Thompson-Hollands J, Farchione TJ, Barlow DH. Intolerance of uncertainty: a common factor in the treatment of emotional disorders. J Clin Psychol. 2013;69(6):630–645. doi: 10.1002/jclp.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley BP, Mogg K, White J, Groom C, de Bono J. Attentional bias for emotional faces in generalized anxiety disorder. Br J Clin Psychol. 1999;38(Pt 3):267–278. doi: 10.1348/014466599162845. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Machan JT, Dyck I, Keller MB. Infrequency of “pure” GAD: impact of psychiatric comorbidity on clinical course. Depress Anxiety. 2001;14(4):219–225. doi: 10.1002/da.1070. [DOI] [PubMed] [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, editors. Social Phobia: Diagnosis, Assessment, and Treatment. New York: Guilford Press; 1995. [Google Scholar]
- Dugas MJ, Buhr K, Ladouceur R. The role of intolerance and uncertainty in etiology and maintenance. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized Anxiety Disorder: Advances in Research and Practice. New York: The Guilford Press; 2004. [Google Scholar]
- Easter J, McClure EB, Monk CS, Dhanani M, Hodgdon H, Leibenluft E, Charney DS, Pine DS, Ernst M. Emotion recognition deficits in pediatric anxiety disorders: implications for amygdala research. Journal of Child & Adolescent Psychopharmacology. 2005;15(4):563–570. doi: 10.1089/cap.2005.15.563. [DOI] [PubMed] [Google Scholar]
- First MS, RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders - Patient version (SCID-1/P version 2.0) New York: New York State Psychiatric Institute Biometrics Research Department; 1994. [Google Scholar]
- Hayward C, Wilson KA, Lagle K, Kraemer HC, Killen JD, Taylor CB. The developmental psychopathology of social anxiety in adolescents. Depress Anxiety. 2008;25(3):200–206. doi: 10.1002/da.20289. [DOI] [PubMed] [Google Scholar]
- Heuer K, Lange WG, Isaac L, Rinck M, Becker ES. Morphed emotional faces: emotion detection and misinterpretation in social anxiety. J Behav Ther Exp Psychiatry. 2010;41(4):418–425. doi: 10.1016/j.jbtep.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Joormann J, I, Gotlib H. Is this happiness I see? Biases in the identification of emotional facial expressions in depression and social phobia. J Abnorm Psychol. 2006;115(4):705–714. doi: 10.1037/0021-843X.115.4.705. [DOI] [PubMed] [Google Scholar]
- Jusyte A, Schonenberg M. Subliminal cues bias perception of facial affect in patients with social phobia: evidence for enhanced unconscious threat processing. Front Hum Neurosci. 2014;8:580. doi: 10.3389/fnhum.2014.00580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado-de-Sousa JP, Arrais KC, Alves NT, Chagas MH, de Meneses-Gaya C, Crippa JA, Hallak JE. Facial affect processing in social anxiety: tasks and stimuli. J Neurosci Methods. 2010;193(1):1–6. doi: 10.1016/j.jneumeth.2010.08.013. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Mahoney AE. To be sure, to be sure: Intolerance of uncertainty mediates symptoms of various anxiety disorders and depression. Behavior therapy. 2012;43(3):533–545. doi: 10.1016/j.beth.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Applying an emotion regulation framework to integrative approaches to generalized anxiety disorder. Clinical Psychology: Science and Practice. 2002;9(1):85–90. [Google Scholar]
- Mennin DS, McLaughlin KA, Flanagan TJ. Emotion regulation deficits in generalized anxiety disorder, social anxiety disorder, and their co-occurrence. Journal of Anxiety Disorders. 2009;23(7):866–871. doi: 10.1016/j.janxdis.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagne B, Schutters S, Westenberg HG, van Honk J, Kessels RP, de Haan EH. Reduced sensitivity in the recognition of anger and disgust in social anxiety disorder. Cogn Neuropsychiatry. 2006;11(4):389–401. doi: 10.1080/13546800444000254. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Mullins DT, Duke MP. Effects of social anxiety on nonverbal accuracy and response time I: Facial expressions. Journal of Nonverbal Behavior. 2004;28(1):3–33. [Google Scholar]
- Newman MG, Llera SJ, Erickson TM, Przeworski A, Castonguay LG. Worry and generalized anxiety disorder: a review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annual review of clinical psychology. 2013;9:275–297. doi: 10.1146/annurev-clinpsy-050212-185544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedenthal PM, Halberstadt JB, Margolin J, Innes-Ker ÅH. Emotional state and the detection of change in facial expression of emotion. European Journal of Social Psychology. 2000;30(2):211–222. [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55(1):56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behav Res Ther. 1997;35(8):741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Ravindran LN, Stein MB. The pharmacologic treatment of anxiety disorders: a review of progress. J Clin Psychiatry. 2010;71(7):839–854. doi: 10.4088/JCP.10r06218blu. [DOI] [PubMed] [Google Scholar]
- Roemer L, Salters K, Raffa SD, Orsillo SM. Fear and avoidance of internal experiences in GAD: Preliminary tests of a conceptual model. Cognitive Therapy and Research. 2005;29(1):71–88. [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychol Med. 2008;38(1):15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schönenberg M, Christian S, Gaußer AK, Mayer S, Hautzinger M, Jusyte A. Addressing perceptual insensitivity to facial affect in violent offenders: first evidence for the efficacy of a novel implicit training approach. Psychological medicine. 2014;44(05):1043–1052. doi: 10.1017/S0033291713001517. [DOI] [PubMed] [Google Scholar]
- Staugaard SR. Threatening faces and social anxiety: a literature review. Clin Psychol Rev. 2010;30(6):669–690. doi: 10.1016/j.cpr.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Stevens S, Rist F, Gerlach AL. Influence of alcohol on the processing of emotional facial expressions in individuals with social phobia. Br J Clin Psychol. 2009;48(Pt 2):125–140. doi: 10.1348/014466508X368856. [DOI] [PubMed] [Google Scholar]
- Stopa L, Clark DM. Social phobia and interpretation of social events. Behav Res Ther. 2000;38(3):273–283. doi: 10.1016/s0005-7967(99)00043-1. [DOI] [PubMed] [Google Scholar]
- Straube T, Mentzel HJ, Miltner WH. Common and distinct brain activation to threat and safety signals in social phobia. Neuropsychobiology. 2005;52(3):163–168. doi: 10.1159/000087987. [DOI] [PubMed] [Google Scholar]
- Surcinelli P, Codispoti M, Montebarocci O, Rossi N, Baldaro B. Facial emotion recognition in trait anxiety. Journal of anxiety disorders. 2006;20(1):110–117. doi: 10.1016/j.janxdis.2004.11.010. [DOI] [PubMed] [Google Scholar]
- Turk CL, Heimberg RG, Luterek JA, Mennin DS, Fresco DM. Emotion dysregulation in generalized anxiety disorder: A comparison with social anxiety disorder. Cognitive Therapy and Research. 2005;29(1):89–106. [Google Scholar]