ABSTRACT
Background: Transitional care programs are a growing topic in health care systems across the country, with a focus on achieving a reduction in hospital readmissions and improving patient and medication safety. Numerous strategies have been employed and studied to determine successful approaches to patient transition from the hospital setting to the home setting. Pharmacist-mediated postdischarge telephonic outreach has demonstrated decreased hospital readmission rates in multiple hospital systems.
Objective: To evaluate the effectiveness of pharmacist-facilitated telephonic medication therapy management (MTM) services on reducing hospital readmissions.
Methods: A retrospective chart analysis (n = 314) was performed for patients who received MTM services following hospital discharge between February 23, 2014 and July 4, 2014. The primary outcome was 30-day all-cause readmission. The secondary outcomes were identification of pharmacist interventions for and recommendations about medication-related problems and discrepancies found between the patients' reported medication list and the hospital discharge medication list.
Results: The data revealed no statistically significant difference in hospital readmission rates between the intervention and control groups (odds ratio,1.04; 95% CI, 0.68–1.60). Pharmacists intervened on 189 medication-related problems via facsimile to the prescriber (35.7% of charts), contacted prescribers by phone for 23 medication-related or health-related issues, and identified 823 medication list discrepancies (78.34% of charts).
Conclusion: Although the provision of telephonic MTM services by pharmacists did not result in an improvement in the readmission rate during this study period, pharmacists were able to intervene on numerous medication-related problems and medication list discrepancies.
Keywords: hospital discharge, medication therapy management, readmissions, transition of care
BACKGROUND/OBJECTIVE
As part of the Affordable Care Act, the Hospital Readmission Reduction program was implemented regarding readmission measures effective for all hospital discharges beginning on or after October 1, 2012.1 This program requires the Centers for Medicare & Medicaid Services (CMS) to reduce payments to hospitals by up to 3% for a defined readmission, which is when a patient is readmitted to a hospital within 30 days of discharge.1 As a result, there has been a body of guidance and literature describing the efforts made toward the goal of reducing the number of 30-day readmissions in hospital systems, including those that incorporate pharmacists and pharmacy services.
The American College of Clinical Pharmacy (ACCP) published guidance on process indicators and a means for utilization of pharmacy services in transitions of care including the relocation of a patient from the hospital setting to the home setting, which was the focus of this study.2 The National Transitions of Care Coalition (NTOCC) also endorsed the use of pharmacists in the care plan, including medication reconciliation, medication management sessions, comprehensive medication counseling, assessment of patient and caregiver understanding, and telephonic follow-up.3 Finally, the American Society of Health-System Pharmacists (ASHP) and American Pharmacists Association (APhA) published a best practices paper that provided profiles for 8 successful programs as part of the Medication Management in Care Transitions (MMTC) project.4 These guiding documents support the use of pharmacists and pharmacy services, including medication reconciliation and patient counseling, as part of an interdisciplinary team approach to improving patient outcomes.
Recent studies evaluating pharmacy services in transitions-of-care programs have displayed mixed results. A study in which a comprehensive medication management service using a face-to-face approach was provided for a cohort of patients over the age of 65 years showed no difference in hospital readmissions or emergency department visits.5 Another study in which a population of patients received an intervention from a ward-based pharmacist demonstrated a 16% reduction in hospital visits and an 80% reduction in hospital readmissions for medication-related problems.6 Yet another study demonstrated that pharmacist-facilitated medication review, patient counseling, and telephonic follow-up decreased the rate of preventable adverse drug interactions; however, there was no difference in overall health care utilization.7 Finally, the University of Pittsburgh found that pharmacists were able to identify a mean of 7.8 medication list discrepancies and 2.5 medication-related interventions per patient. This same study also revealed a reduction in readmission rates for patients who received pharmacist intervention services during hospitalization and were subsequently contacted by a pharmacist at home within 72 hours of being discharged.4
The practice model used in this study was different than those previously described in that the pharmacist intervention was performed via the telephone and the pharmacist was not directly involved in the patient's care during hospitalization. The service design incorporated elements recommended by the NTOCC, ACCP, and APhA/ASHP documents as well as successful interventions described in the literature, including medication reconciliation, patient counseling, and additional follow-up calls after discharge. Pharmacy services in this study were conducted from an academic medication therapy management (MTM) call center affiliated with the facility in which the patients were hospitalized.
This study was conducted to evaluate the impact of patient-centric MTM services on 30-day readmission rates. This study also examined the number and type of medication-related problems identified, interventions recommended based on the problems identified, and the medication list discrepancies recognized during the provision of services.
METHODS
Design and Setting
The study involved a retrospective chart review on 314 patients who participated in a patient-centric, telephonic transitions-of-care MTM program. The MTM services were part of a continuous quality improvement transitions-of-care pilot project for patients being discharged from the hospital. Licensed pharmacists provided the MTM services with administrative support from certified, registered pharmacy technicians. A daily patient discharge list was generated by the hospital and provided to the Medication Therapy Management Communication and Care Center (MTMCCC) for patient identification. Each patient eligible to participate in the program was contacted via telephone by a technician or a licensed pharmacist within 72 hours of hospital discharge. Three attempts at contact were made for all patients in the program. If the patient was reached with 1 of the 3 call attempts, then he or she was offered the telephonic MTM services. If the patient was not reached after 3 attempts and/or did not return the center's calls, he or she was not considered a part of the program. During the initial call, the technician explained the program and offered MTM services. If the patient agreed, then the technician gathered additional demographic and lifestyle information from the patient and live transferred the call to a pharmacist for completion of the comprehensive medication review (CMR). If the patient was unable to complete the call at that time, the technician scheduled an appointment for the CMR and the pharmacist called the patient back directly.
The MTM services utilized in this study followed the 5 core elements of an MTM service model as outlined by the APhA MTM in Pharmacy Practice framework.8 The 5 core elements of the MTM services provided included a CMR, a personalized medication list, a medication action plan, documentation of the services, provider intervention(s), and follow-up services. All patients who participated in the program and received a CMR were contacted for a follow-up call by a technician who transferred the call to the pharmacists, or by a pharmacist, within 14 to 30 days after the initial CMR was completed. Three attempts were made to contact all patients for the follow-up review. During the follow-up review call, it was confirmed that the patients received the documents that were sent by mail following the CMR; these included a personalized medication list and a medication action plan. Also during the follow-up review call, the patients and their medication regimen were assessed for any resolutions to previously identified clinical issues and were evaluated for any new or additional medication-related or health-related problems that may have arisen since the CMR. Technicians provided administrative support, including creating an electronic chart for each patient utilizing a pre-established spreadsheet template; entering basic demographic information obtained from the hospital discharge report into the patient's spreadsheet; making call attempts to patients to explain the program and gather additional demographic and lifestyle information before live transferring the call to a pharmacist for completion of the CMR or scheduling an appointment for a CMR; making call attempts to patients for follow-up reviews and transferring them to the pharmacists; and mailing documents to patients and faxing documents to the patients' physicians after the completion of the medication review. This study was approved by the associated institutional review board.
Inclusion/Exclusion Criteria
Patients were included in the study if they had been discharged from the hospital to home from the hospital's internal medicine or hospitalist services and were discharged on at least 4 maintenance medications as listed in their electronic medical record. Patients who were on the hospital's family medicine or specialty service and those who were enrolled in a Community-Based Care Transitions Program (CCTP) were excluded, as they were receiving transitions-of-care services from a different organization. Also excluded were patients who were uninsured, listed as dually eligible for Medicare and Medicaid services, or had an admission secondary to cancer treatment or radiation therapy.
Study Variables
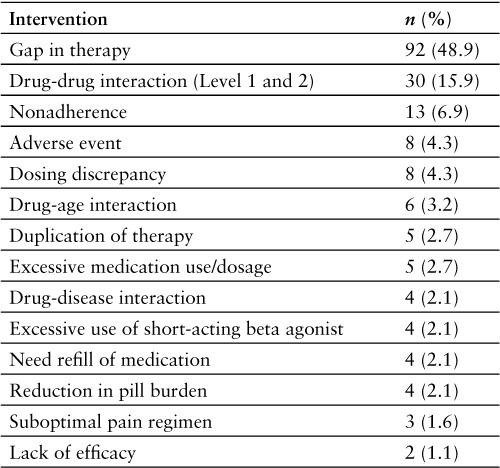
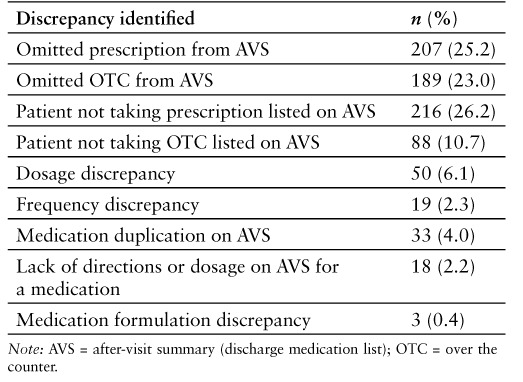
The primary endpoint for this study was 30-day, all-cause hospital readmission. The secondary endpoint was pharmacist interventions for medication-related problems and identified discrepancies between the patient-reported medication list and the hospital discharge medication list (also called the after visit summary or AVS). A medication-related problem was defined as any event or situation involving the patient's medication treatment that interfered with or prevented the patient from experiencing optimal therapy. Medication-related problems that were referred to the prescriber by facsimile were classified into 14 categories (Table 1). Medication-related problems that were addressed via the telephone generally involved an acute care need and did not fit into the specific categories as described in the faxed interventions. A medication-related discrepancy was reported as any difference between the patient-reported medication list and the medication list generated from the electronic medical record upon the patient's discharge from the hospital. These discrepancies were classified into 9 categories (Table 1).
Table 1.
Definitions of medication-related problems and discrepancies
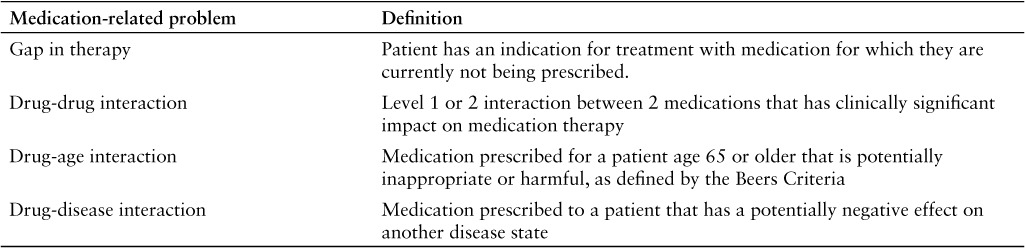
Table 1.
Definitions of medication-related problems and discrepancies (CONT.)
Statistical Analysis
A segmented time-series analysis was performed on the data to evaluate for the primary outcome. Thirty-day readmission data for patients who received a CMR were obtained from the hospital and transmitted to a third-party statistics group for analysis. A per-protocol analysis was utilized. Secondary outcomes were manually categorized and totaled using Microsoft Excel.
RESULTS
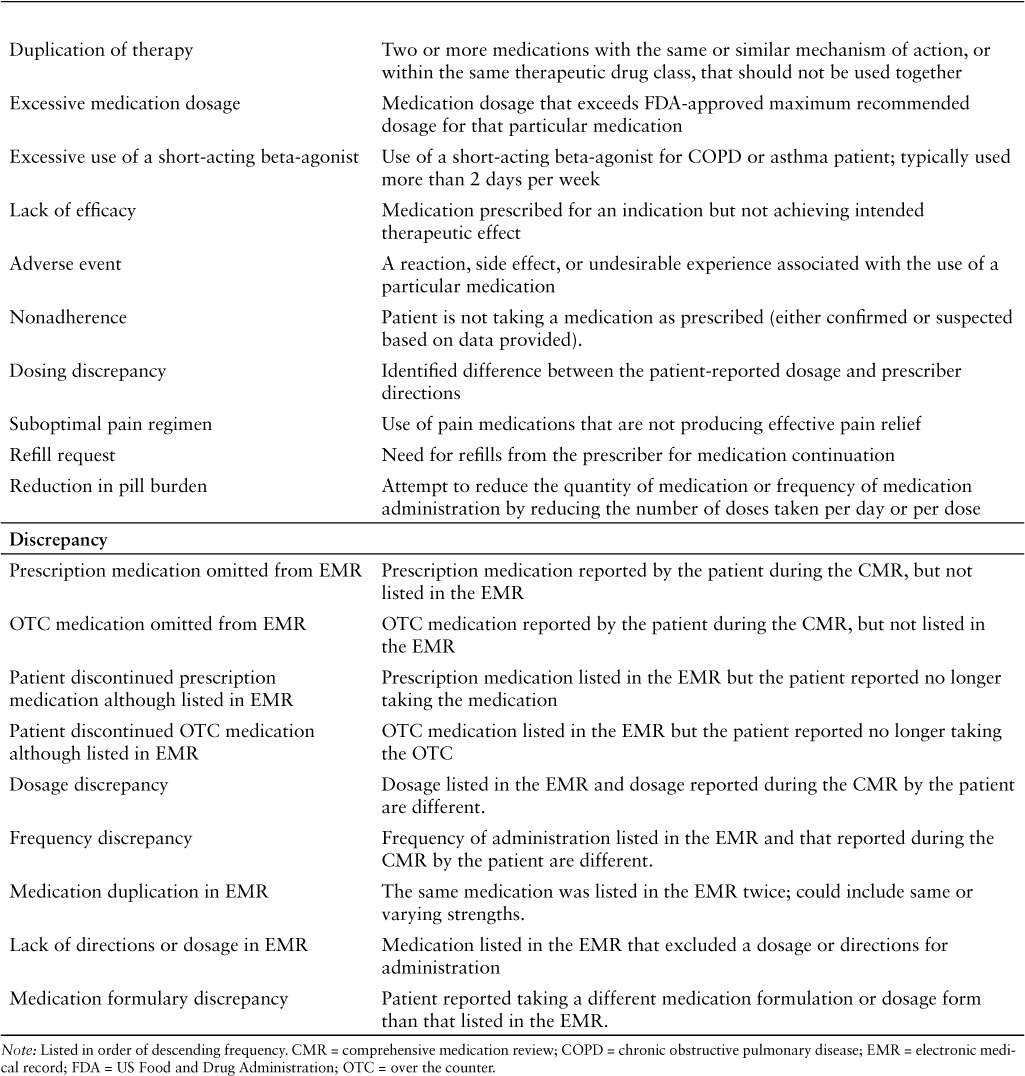
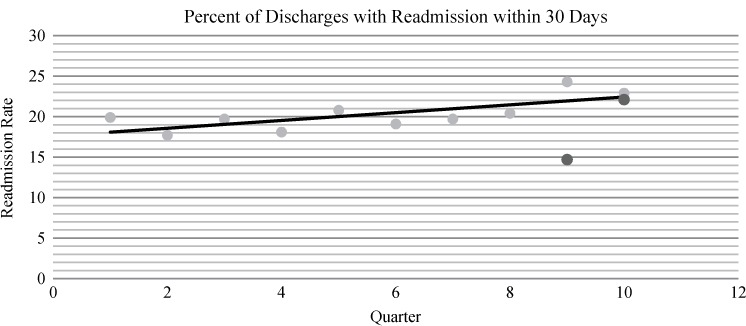
MTM services were offered to patients who were discharged between February 23, 2014 and July 4, 2014. A total of 843 patients were contacted for the provision of a CMR. Of these 843 patients, 314 patients accepted and participated in a CMR with the pharmacist whereas 150 patients declined the services. The remaining 379 patients were unable to be reached by telephone after multiple contact attempts. A majority of the patients who participated were female (59.9%), with an average age of 57.55 years and an average length of the hospital stay of 4.98 days. The average number of medications documented in the electronic medical record and the number actually reported as being taken by the patient were slightly different (Table 2).
Table 2.
Baseline characteristics (N = 314)
30-Day, All-Cause Readmission
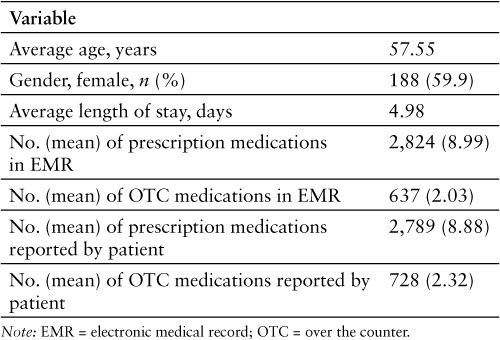
The analysis for the primary outcome included 267 patient charts. Due to post-hospital discharge coding that was not completed until after the provision of the MTM services, 47 of the 314 patients were excluded from analysis because of an admission secondary to cancer treatment or radiation therapy. A segmented time-series analysis was utilized in which 2 years of readmission data, from June 2012 to July 2014, were divided into 10 quarters; this served as a comparative control group for the treatment group. The treatment group fell within quarters 9 and 10 (Figure 1). The data indicated that patients who received the MTM services were less likely to be readmitted; however, there was not a statistically significant difference between the treatment group and control group for the 30-day readmission rate observed during this timeframe (odds ratio [OR], 1.00; 95% CI, 0.67–1.50).
Figure 1.
Percent of discharges with readmission within 30 days. Black dots represent the study group; grey dots indicate the control group.
Pharmacist Interventions
Pharmacists identified and intervened on 212 medication-related problems. Of those interventions, 189 were sent to the physician via facsimile and 23 required contact with the prescriber by telephone. The most common intervention sent to the physician was gaps in therapy (49%), which was followed by drugdrug interactions (16%) and nonadherence concerns (7%). The most commonly identified gaps in therapy were acute coronary syndrome/chest pain without a fast-acting nitrate (19%), diabetic without angiotensin-converting enzyme inhibitor or an angiotensin II receptor blocker (16%) therapy, and heart failure on beta-blocker therapy not indicated for heart failure (12%). The most common reason for contacting a prescriber by phone was for verification of a medication dosage or directions, followed by the need for additional therapy due to the lack of prescribing for an acute or chronic need or medical equipment upon discharge. At least 1 pharmacist intervention was identified in 35.7% of the CMRs completed, with 27 CMRs revealing 2 interventions per patient and 20 CMRs with more than 2 interventions per patient. Categorized pharmacist interventions via facsimile are shown in Table 3. Reasons for contacting physicians via telephone included prescription for medication or medical equipment was not written or given to patient at discharge, incorrect or invalid dosage form was ordered at discharge, need for clarification or verification of medication dose/strength/frequency, and patient medical concern identified during the CMR.
Table 3.
Pharmacist interventions via facsimile (N = 188)
Medication-Related Discrepancies
Pharmacists identified 823 total discrepancies in the patients' medication history during this study. Of the 314 CMRs completed, 246 contained at least one medication list discrepancy (78.34%). The most common discrepancy between the medication list generated by the electronic medical record and the patient-reported medication list was a medication on the electronic medical record that the patient was no longer taking (26.2%), followed by a prescription medication a patient was taking that was not on the electronic medical record (25.2%) and an over-the-counter medication that a patient was taking that was not listed on the electronic medical record (23.0%). Results for these data are shown in Table 4.
Table 4.
Pharmacist-identified medication-related discrepancies
DISCUSSION
This study evaluated the potential impact of a pharmacist-facilitated telephonic MTM service on reducing 30-day, all-cause readmissions. Based upon our analysis, pharmacist-facilitated MTM services did not demonstrate a statistically significant reduction in 30-day readmissions; however, there was an observed decrease in readmissions that favored the treatment group during both quarters in the study.
The model utilized in this study is a unique approach to a transitions-of-care program. Although other programs involving telephonic follow-up from pharmacists have demonstrated reductions in 30-day readmission, these studies utilized pharmacists who were actively involved in the patient's care during an inpatient stay and/or were connected directly with the hospital facility.3,6,9 Many models that utilized pharmacists as described by ASHP-APhA incorporated pharmacy services into a multidisciplinary health care team approach.3 This study was facilitated by pharmacists who were not involved in any element of the patient's care prior to admission, while in the hospital, or with the discharge planning process. More involvement with or connection to the patient's health care team may have increased the effectiveness of the pharmacist intervention in this study, because the pharmacist may have been able to more effectively and quickly resolve health care–related concerns.
Patient selection may have also influenced the results of this study. Unless the admission was related to chemotherapy or radiation as described previously, diagnoses or chronic disease states were not considered for enrollment. Readmission risk stratification was not used as a method of identification. As outlined in the MMTC project, many successful models for pharmacist-facilitated transitional care programs identify patients based on readmission risk and/or specific disease states. For example, Froedtert Hospital and Johns Hopkins focused on patients who were at high risk for readmission or adverse outcomes, whereas the Hennepin County Medical Center focused on patients with congestive heart failure, acute myocardial infarction, and pneumonia diagnoses.4 This study did not risk stratify patients for readmission, nor was it powered to analyze readmission rates based upon specific diagnoses. It is possible that this program may have been more successful if it had targeted a more specific cohort of patients.
Regarding the secondary outcomes, the pharmacists in this study identified numerous medication-related problems for intervention. This study was not able to identify the success or acceptance rate of the faxed interventions, because the pharmacists did not have access to outpatient records in the health system. It is unclear whether these interventions had an impact on preventing any readmissions.
This study demonstrated a novel approach at a transitions-of-care program that was facilitated telephonically and independent of the health care system. Although it did not show statistically significant reduction in 30-day readmissions, it demonstrated an absolute risk reduction as well as insight for future transitions-of-care design. Despite the well-established impact of medication management in transitional care programs, lack of internal staffing resources presents a known challenge in implementing these programs.3,4 Use of an outside organization, similar to that used in this study to help facilitate telephonic follow-up with care transitions, could be an answer to that challenge. From a fiscal perspective, the Hospital Readmission Reduction program determines the penalty based upon specific targeted disease states including congestive heart failure, acute myocardial infarction, pneumonia, chronic obstructive lung disease, elective total hip arthroplasty and total knee arthroplasty, and elective coronary artery bypass graft.1 A proposed change to this study would be to use this model with a focus on a targeted patient population that is risk stratified for readmissions and has specific core disease states that have the largest potential for impact for the hospital system.
Limitations
There were several notable limitations to this study. First, the hospital's crude readmission rates during the quarters analyzed, according to the time series analysis performed, were increased compared to the previous 8 quarters without a clear explanation. This variation in crude readmission rates along with a treatment period of only 2 quarters likely affected the readmission outcome data.
Also, patients who may be predisposed to high readmissions based solely on the complex nature of their disease states may have affected the study results. As previously mentioned, the exclusion criteria were very limited. Due to the relatively small exclusion criteria, patients with disease states such as sickle cell anemia and cystic fibrosis and patients with cognitive impairment or dementia were not excluded from the study. Based on the more complex nature of these various patient populations, the CMR might not have been as effective and readmissions could be somewhat higher in these patients. The inclusion of these more complex patients in this study is a limitation and may have adversely affected the results.
Another limitation for this study was the pharmacist's lack of involvement with or knowledge of the patient (and vice versa) prior to the initiation of this program. The pharmacist was not part of the patient's care team preadmission or during admission. The first encounter between the patient and pharmacist was during the telephonic outreach from the pharmacist after the patient was discharged from the hospital. The patient had not met the pharmacist before the offering of the CMR. The patient may have been more likely to accept the services and/or the pharmacist's recommendations if he or she had an established relationship with the pharmacist beforehand.
A final limitation to this study was the competition from other transitional care programs; this influenced the patient pool that was eligible for this program. During the time period of this study, there were several active transitions-of-care programs, including the CCTP, being offered to the discharged patients. The CCTP program recruited and enrolled geriatric patients during their inpatient stay, and it was given priority in patient assignment over this program. Also, the academic health system's pharmacistrun clinics were vying for the same patient pool. The patients being discharged were screened to ascertain whether they were being seen at one of the established clinics. If so, they were removed from the eligible population and therefore were not able to be contacted for this program. This limited the number of available patients and likely affected the results of this study.
Conclusions
Pharmacist-facilitated telephonic MTM services did not demonstrate a statistically significant relationship between exposure to the CMR and reduced readmission rates during the time period of this study. Pharmacists did, however, demonstrate the ability to identify and affect clinical interventions as well as recognize a variety of medication list discrepancies for patients who received the telephonic MTM services. This study provides insights into designing and enhancing pharmacist-led telephone-based transitions of care MTM programs for the future.
ACKNOWLEDGMENTS
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- 1. Centers for Medicare & Medicaid Services. . Readmissions Reduction Program. August 2014. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed May 20, 2015.
- 2. Kirwin J, Canales AE, Bentley ML, . et al. Process indicators of quality clinical pharmacy services during transitions of care. American College of Clinical Pharmacy. Pharmacotherapy. 2012; 32( 11): e338– e347. [DOI] [PubMed] [Google Scholar]
- 3. Improving transitions of care: The vision of the National Transitions of Care Coalition. . National Transitions of Care Coalition. May 2008. http://www.ntocc.org/Portals/0/PDF/Resources/PolicyPaper.pdf. Accessed May 20, 2015.
- 4. Cassano A. ASHP-APhA medication management in care transitions best practices. American Society of Health-System Pharmacists American Pharmacists Association. February 2013. http://media.pharmacist.com/practice/ASHP_APhA_MedicationManagementinCareTransitionsBestPracticesReport2_2013.pdf. Accessed May 21, 2015.
- 5. Westberg S, Swanoksi MT, Renier CM, Gessert CE.. Evaluation of the impact of comprehensive medication management services delivered posthospitalization on readmissions and emergency department visits. J Managed Care Pharm. 2014; 20( 9): 886– 893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gillespie U, Alassaad A, Henrohn D, . et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years and older: A randomized controlled trial. Arch Intern Med. 2009; 169( 9): 894– 900. [DOI] [PubMed] [Google Scholar]
- 7. Schnipper J, Kirwin JL, Cotugno MC, . et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006; 166: 565– 571. [DOI] [PubMed] [Google Scholar]
- 8. American Pharmacist Association, National Association of Chain Drug Stores Foundation. . Medication therapy management in pharmacy practice: Core elements of an MTM service model version 2: March 2008. http://www.pharmacist.com/sites/default/files/files/core_elements_of_an_mtm_practice.pdf. Accessed May 21, 2015. [DOI] [PubMed]
- 9. Gil M, Mikaitis DK, Shier G, Johnson TJ, Sims S.. Impact of a combined pharmacy and social worker program to reduce hospital readmissions. J Managed Care Pharm. 2013; 19( 7): 558– 563. [DOI] [PMC free article] [PubMed] [Google Scholar]


