Abstract
NLRP6 is a member of the Nod like receptor family, whose members are involved in the recognition of microbes and/or tissue injury. NLRP6 was previously demonstrated to regulate the production of IL-18 and is important for protecting mice against chemically-induced intestinal injury and colitis-associated colon cancer. However, the cellular mechanisms by which NLRP6 reduces susceptibility to colonic inflammation remain unclear. Here, we determined that NLRP6 expression is specifically upregulated in Ly6Chi inflammatory monocytes that infiltrate into the colon during dextran sulfate sodium (DSS)-induced inflammation. Adoptive transfer of WT Ly6Chi inflammatory monocytes into Nlrp6−/− mice was sufficient to protect them from mortality, significantly reducing intestinal permeability and damage. NLRP6-deficient inflammatory monocytes were defective in TNFα production, which was important for reducing DSS-induced mortality and was dependent on autocrine IL-18 signaling by inflammatory monocytes. Our data reveal a previously unappreciated role for NLRP6 in inflammatory monocytes, which are recruited after DSS-induced intestinal injury to promote barrier function and limit bacteria-driven inflammation. This study highlights the importance of early cytokine responses, particularly NLRP6-dependent and IL-18-dependent TNFα production, in preventing chronic dysregulated inflammation.
Keywords: colitis, inflammatory monocytes, TNFα, NLRP6
Introduction
Inflammatory bowel disease (IBD) is a major health problem that results in significant morbidity and mortality due to recurrent episodes of bloody diarrhea, weight loss, and complications from chronic intestinal inflammation, such as cancer. Current approved therapies for IBD rely primarily on symptom management and inhibiting inflammation, but do not address the underlying mechanism behind IBD pathogenesis. The current prevailing model for the pathogenesis of IBD is the development of an imbalance in the microbial community structure within the intestine, or dysbiosis, and/or aberrant immune responses to commensal bacteria in a genetically susceptible host.1 A better understanding of events that lead to dysregulated inflammation is needed to identify targets for treatment and cure.
Recently, the Nod like receptor (NLR), NLRP6, has been shown to be important for promoting intestinal homeostasis and for protection against the development of colitis and colitis associated tumorigenesis in mice.1-4 The mechanism by which NLRP6 protects against colitis remains to be fully elucidated. Gene ontogeny analyses have established a link between NLRP6 and intestinal epithelial cell (IEC) repair.4 NLRP6 also regulates IL-18 production, which is important for epithelial repair and protection against inflammation-associated colon tumorigenesis.1, 2, 4-6 NLRP6 is highly expressed in IECs, and bone marrow (BM) chimera experiments demonstrated that IL-18 production by epithelial cells is important for reduced susceptibility to DSS-induced intestinal injury and inflammation, suggesting that NLRP6 functions primarily in epithelial cells to promote IL-18 production and epithelial repair. NLRP6 also regulates autophagy within intestinal goblet cells to affect mucus secretion, which contributes to intestinal homeostasis.7 However, NLRP6 is also expressed in hematopoietic cell populations, and we have previously demonstrated that NLRP6 functions in BM-derived cells to limit colitis-associated tumorigenesis.1 Thus, the specific cell type that is important for NLRP6-mediated protection against the development of colitis and tumorigenesis has not been definitively identified.
In this study, we examined the expression of NLRP6 in various hematopoietic cell populations within the lamina propria (LP) during DSS-induced intestinal injury and determined that inflammatory monocytes, defined as CD11b+Ly6GintLy6Chi cells, induce NRLP6 expression in response to DSS. More importantly, the adoptive transfer of wildtype (WT) Ly6Chi monocytes into Nlrp6−/− mice improves survival after DSS treatment. NLRP6-deficient Ly6Chi monocytes had impaired production of TNFα and reactive oxygen species (ROS), and the injection of recombinant TNFα (rTNFα) into Nlrp6−/− mice early during DSS treatment was sufficient for protection against mortality. We further demonstrate that Il18−/− and Il18r1−/− Ly6Chi inflammatory monocytes have similar defects in TNFα production, and their adoptive transfer into Nlrp6−/− mice failed to rescue DSS-induced mortality, suggesting that autocrine IL-18 signaling by inflammatory monocytes is important for TNFα production and protection against acute intestinal injury. Altogether, these studies reveal a protective role for early TNFα production by inflammatory monocytes, which is at least, in part, IL-18- and NRLP6-dependent and is critical for limiting dysregulated commensal-driven intestinal inflammation.
Results
NLRP6 function in Ly6Chi inflammatory monocytes reduces susceptibility to DSS-induced intestinal injury
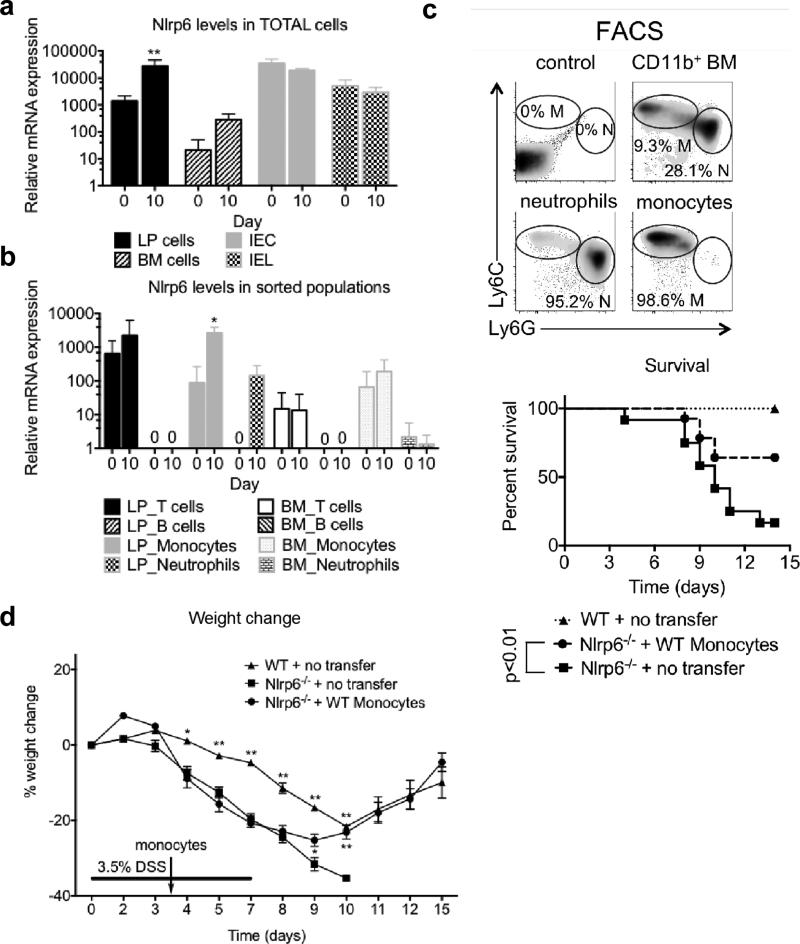
We previously demonstrated that Nlrp6−/− mice are more susceptible to DSS-induced colitis as well as colitis-associated tumorigenesis after treatment with the carcinogen azoxymethane (AOM) and DSS.1, 2, 4 Furthermore, NLRP6 activity in BM-derived cells was important for limiting inflammation-associated tumors.1 To identify the cell type responsible for the protective effects of NLRP6, expression of NLRP6 was measured in different cell populations in the BM and colon LP before and after DSS treatment. We analyzed NLRP6 mRNA expression in IECs, intraepithelial lymphocytes (IELs), BM, and LP cells from WT mice on day 0 and day 10 (at the end of 5 days of 2% DSS) in the AOM/DSS model of colitis-associated tumorigenesis.1 We determined that NLRP6 expression was upregulated in the LP, but not IEC, IEL or BM cells in response to DSS (Figure 1a). Within the LP, NLRP6 was specifically increased in myeloid cells, and in particular, Ly6Chi monocytes and neutrophils, after DSS treatment with the highest induction in Ly6Chi inflammatory monocytes (Figure 1b). In contrast, NLRP6 expression did not change in T cells and was undetectable in B cells (Figure 1b). We confirmed the upregulation of NLRP6 expression in LP cells and myeloid cells within the LP in WT mice treated with DSS only, indicating that the observed change in NLRP6 expression is not dependent on AOM (Supplementary Figure 1).
Figure 1. NLRP6 is induced in lamina propria Ly6Chi monocytes during DSS induced inflammation, and is important for reducing susceptibility to colitis.
(a) NLRP6 levels were measured in BM, LP, IECs and IELs of WT mice at day 0 and day 10 of AOM/DSS by qPCR. (b) NLRP6 expression was measured in CD3+B220− CD11b− T cells, CD3− B220+CD11b− B cells, CD3− CD11b+Ly6ChiLy6G− monocytes and CD3− CD11b+Ly6CintLy6G+ neutrophils within the BM and LP. Data are representative of three independent experiments; n=11 for day 0, n=10 for day 10. *, ** - p<0.05, p<0.001, respectively, as compared to day 0 time point of the same genotype. (c) Representative plots of Ly6C versus Ly6G staining of CD11b+ BM cells (top). Kaplan–Meyer survival curves of mice treated with 7 days of 3.5% DSS (bottom). (d) Percent weight change with 3.5% DSS administration. Data are representative of two independent experiments; n=15, n=24, n=14 for WT, Nlrp6−/− and Nlrp6−/− + WT Ly6Chi monocytes groups respectively. *, ** - p<0.05, p<0.001, respectively, as compared to Nlrp6−/−.
Upregulation of NLRP6 in response to DSS in Ly6Chi inflammatory monocytes prompted us to investigate if NLRP6 function in this population of cells was important for maintaining intestinal homeostasis. WT Ly6Chi monocytes (CD3− CD11b+Ly6ChiLy6G−) were FACS-sorted to approximately 99% purity (Figure 1c), and were adoptively transferred into Nlrp6−/− mice on day 3.5 of a 7-day course of high dose DSS (3.5%). In contrast to mock treated Nlrp6−/− mice, which had a 15% survival rate after DSS treatment, Nlrp6−/− mice that received Ly6Chi monocytes were protected from lethality with a survival rate of approximately 70% (Figure 1c). Consistent with improved survival, Nlrp6−/− mice harboring WT Ly6Chi monocytes also showed significantly less weight loss (Figure 1d). These results strongly suggest that NLRP6 is upregulated in inflammatory monocytes that are important for reducing DSS-induced mortality. To demonstrate that donor Ly6Chi monocytes can be recruited to the intestine during DSS treatment, we adoptively transferred Ly6Chi monocytes isolated from transgenic mice that express green fluorescent protein (GFP) into Nlrp6−/− mice during DSS treatment, and detected GFP+ Ly6Chi monocytes in the LP of recipient mice (Supplementary Figure 2a). As confirmation that the recruitment of inflammatory monocytes into the intestinal LP is important for NLRP6-mediated protection against DSS-induced injury and inflammation, we adoptively transferred Nlrp6−/− mice with Ly6Chi monocytes isolated from mice deficient in CCR2, which is expressed by inflammatory monocytes and is required for their recruitment to sites of inflammation,8 and observed no improvement in weights or survival with DSS treatment (Supplementary Figure 2b-d).
Ly6Chi monocytes can be further characterized by their CX3CR1 expression. During intestinal inflammation, Ly6ChiCX3CR1int inflammatory monocytes are recruited to the LP.9 Consistently after 5 days of DSS, all Ly6Chi monocytes in the LP of WT and Nlrp6−/− mice express CX3CR1 (Supplementary Figure 3a). To determine CX3CR1 expression in Ly6Chi donor monocytes in adoptive transfer experiments and track their recruitment in the intestine during DSS treatment, we used CX3CR1-GFP mice, in which CX3CR1-expressing cells are labeled with GFP, as donors and Ccr2−/− mice as recipients. Ly6Chi donor monocytes were mostly CX3CR1int (~80%), (Supplementary Figure 3b), but after transfer into Ccr2−/− mice treated with DSS, all donor CCR2+ cells in the LP were CX3CR1int (Supplementary Figure 3c). These results strongly suggest that Ly6Chi monocytes that migrate into the colon in this model and have protective effects in Nlrp6−/− mice represent a relatively homogenous population of CX3CR1int inflammatory monocytes.
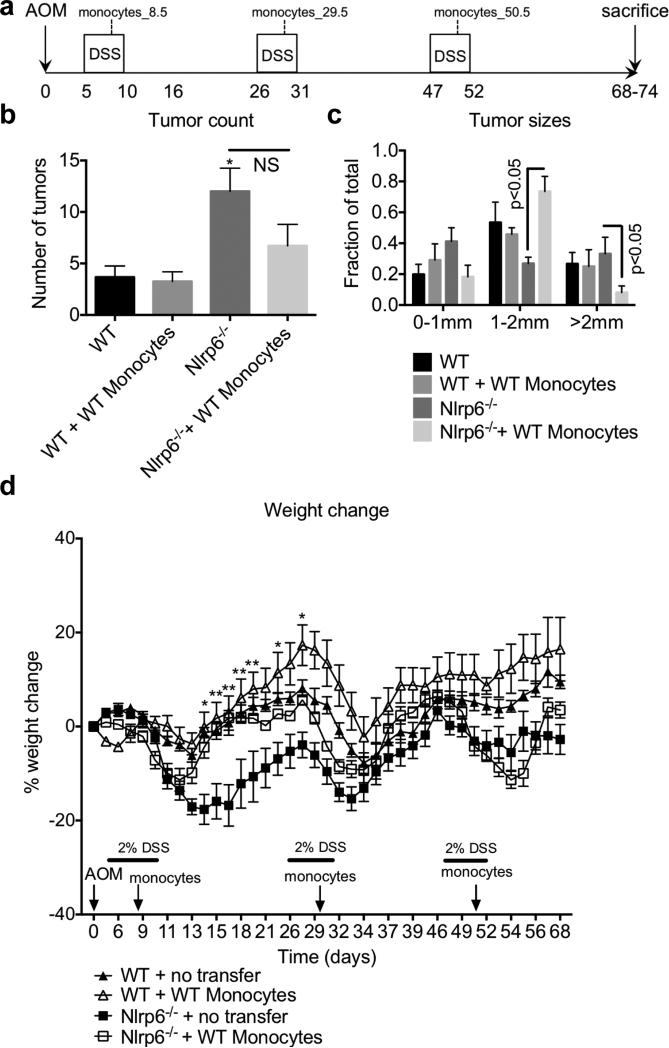
WT Ly6Chi monocytes limit tumor growth in Nlrp6−/− mice
We had previously reported that Nlrp6−/− mice developed more colon tumors compared to WT mice in the AOM/DSS model of inflammation-associated tumorigenesis.1 To determine whether NLRP6 function in inflammatory monocytes is important for reducing inflammation-associated tumorigenesis, we adoptively transferred WT Ly6Chi monocytes into Nlrp6−/− mice 3.5 days after the start of each cycle of 2% DSS (Figure 2a). As previously published, Nlrp6−/− mice developed more tumors compared to WT mice (Figure 2b).1 Adoptive transfer of WT Ly6Chi monocytes resulted in fewer tumors; however, this did not reach statistical significance (Figure 2b). The transfer of WT Ly6Chi monocytes into Nlrp6−/− mice did result in a significant reduction in tumor sizes with fewer tumors greater than 2 mm in size compared to that in Nlrp6−/− mice (Figure 2c), and reduced weight loss early during AOM/DSS treatment (days 14-26, Figure 2d).
Figure 2. Adoptive transfer of WT Ly6Chi monocytes into Nlrp6−/− mice significantly reduces tumor growth in AOM/DSS model of colitis-associated tumorigenesis.
(a) Age and sex-matched Nlrp6−/− and WT mice were treated with AOM followed by three 5-day cycles of 2% DSS. Sorted Ly6Chi monocytes were injected i.v. 3.5 days after the start of each DSS cycle. Three weeks after the last cycle of DSS mice were sacrificed and tumors grossly counted with a stereomicroscope. Number (b) and size (c) of tumors are shown. (d) Percent weight change during AOM/DSS treatment. Data are representative of three independent experiments, n=15, n=10, n=19, n=22 for WT, WT + WT Ly6Chi monocytes, Nlrp6−/− and Nlrp6−/− + WT Ly6Chi monocytes groups respectively. *, ** - p<0.05, p<0.001, respectively, as compared to WT (b) or Nlrp6−/− mice (d).
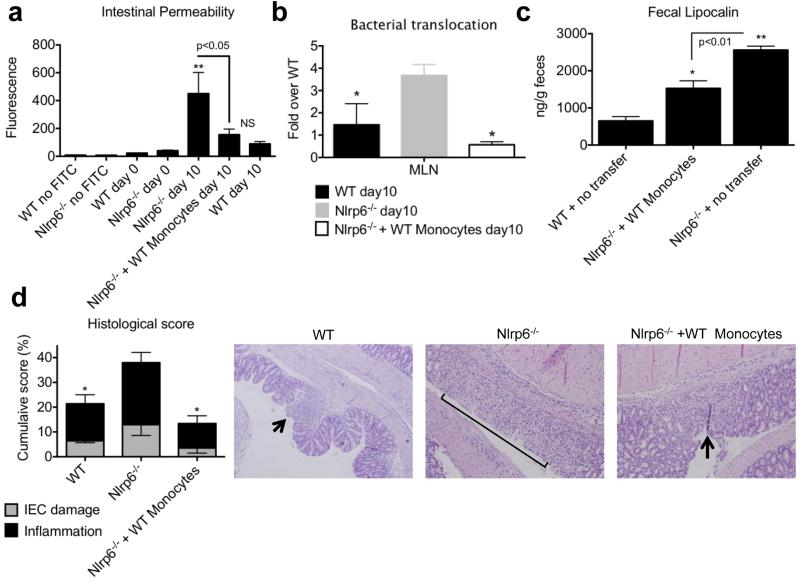
NLRP6 function in Ly6Chi monocytes promotes resistance against DSS-induced damage
To determine the effects of WT Ly6Chi monocytes within the colon of Nlrp6−/− mice during the acute inflammatory response to DSS, we looked specifically on day 10 of the AOM/DSS model of tumorigenesis when mice have completed 5 days of 2% DSS prior to the onset of chronic, dysregulated inflammation in Nlrp6−/− mice.1 Increased intestinal permeability is a classical hallmark of DSS induced IEC damage.1, 2, 4 To determine if the adoptive transfer of WT Ly6Chi monocytes affected intestinal permeability, mice were gavaged with FITC-dextran and its passage into the peripheral circulation was measured. As demonstrated previously,1 naïve WT and Nlrp6−/− mice had very low levels of serum fluorescence indicative of an intact epithelial barrier, whereas DSS-treated mice, especially Nlrp6−/− mice, had higher levels of serum fluorescence suggesting increased intestinal permeability (Figure 3a).1 Importantly, the intestinal permeability of Nlrp6−/− mice adoptively transferred with WT Ly6Chi monocytes was similar to that of WT mice after exposure to DSS, and was significantly reduced compared to that of mock-treated Nlrp6−/− mice (Figure 3a). Consistently, there was a reduction in bacterial translocation into the mesenteric lymph nodes (MLNs) as measured by qPCR in Nlrp6−/− mice adoptively transferred with WT Ly6Chi monocytes (Figure 3b). Levels of fecal lipocalin-2, a surrogate marker of intestinal epithelial damage,10 were also reduced in Nlrp6−/− mice adoptively transferred with WT Ly6Chi monocytes (Figure 3c). Histological scoring of colitis demonstrated reduced intestinal epithelial damage and inflammation in the presence WT Ly6Chi monocytes (Figure 3d). Thus, NLRP6 activity in Ly6Chi inflammatory monocytes is important in limiting DSS-induced damage.
Figure 3. Adoptive transfer of WT Ly6Chi monocytes into Nlrp6−/− mice limits bacterial translocation and intestinal damage.
Age- and sex-matched Nlrp6−/− and WT mice were treated with AOM followed by 5 days of 2% DSS. WT Ly6Chi monocytes were adoptively transferred into Nlrp6−/− mice 3.5 days after start of DSS. (a) Mice were gavaged FITC-dextran at end of 5 days of DSS followed by serum collection and measurement of fluorescence 4 hours later. (b) Normalized levels of total bacteria/MLN as measured by qPCR after 5 days of 2% DSS. (c) Fecal lipocalin-2 levels as measured by ELISA after 5 days of DSS. (d) Histological inflammatory scores based on extent of inflammatory cell infiltration and IEC damage;Micrographs of H&E sections are at 200x magnification. Arrow points to focal erosion with inflammatory infiltrate. Bracket indicates ulcerated epithelium with inflammatory infiltrate in LP and submucosa. Data are representative of three independent experiments, n=15, n=16, n=20 for WT, Nlrp6−/− and Nlrp6−/− + WT Ly6Chi monocytes groups respectively. *, ** - p<0.05, p<0.001, respectively, as compared to day 0 of both genotypes (a), or as compared to Nlrp6−/− (b,c) or as compared to WT (d).
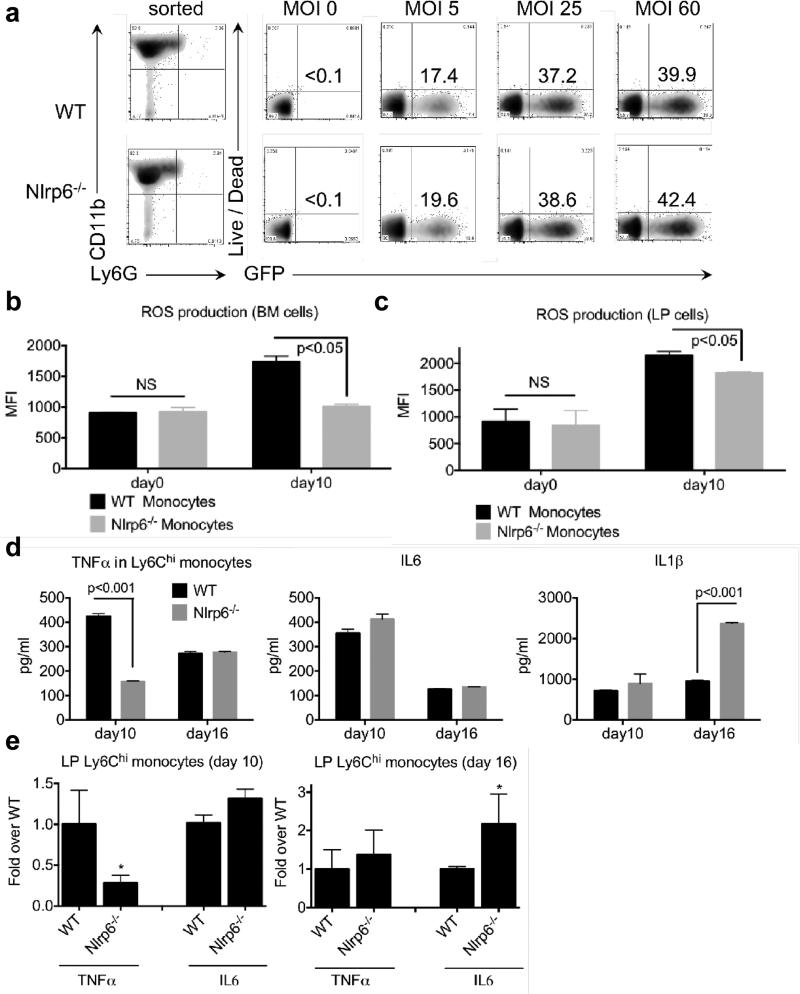
Nlrp6−/− Ly6C hi inflammatory monocytes have impaired TNFα and ROS production
Inflammatory Ly6Chi monocytes perform critical functions during inflammation, including phagocytosis, production of ROS, and secretion of cytokines.11 These functions limit bacterial translocation, promote tissue repair, and ultimately, help to resolve inflammation. To determine whether Nlrp6−/− Ly6Chi inflammatory monocytes have a defect in phagocytosis, Ly6Chi monocytes were isolated from naïve and AOM/DSS-treated WT and Nlrp6−/− mice (day 10).1 In agreement with previous studies, we observed no defect in phagocytosis as BM-sorted Ly6Chi monocytes from WT and Nlrp6−/− mice exhibited equivalent levels of internalized GFP+ E.coli (Figure 4A).12 However, ROS production was significantly reduced in BM-derived and LP-isolated Nlrp6−/− Ly6Chi monocytes as compared to WT Ly6Chi monocytes after DSS treatment (Figure 4b, c). We next measured levels of various cytokines produced by LP inflammatory Ly6Chi monocytes isolated from AOM/DSS-treated Nlrp6−/− mice and cultured overnight. Nlrp6−/− LP-derived inflammatory monocytes exhibited decreased early production of TNFα at the completion of DSS, whereas other cytokines such as IL-6 and IL-1β were produced at levels similar to that by WT Ly6Chi monocytes (Figure 4d). Consistently, TNFα mRNA expression was also significantly reduced in Nlrp6−/− LP Ly6Chi monocytes (Figure 4e). By day 16, however, approximately one week after completion of DSS, TNFα levels were no longer significantly different between WT and Nlrp6−/− inflammatory monocytes, suggesting that NLRP6-independent pathways may be compensating (Figure 4d). The defect in TNFα production was specific to Nlrp6−/− inflammatory monocytes as Nlrp6−/− resident LP macrophages, defined as CD11b+Ly6Clow/− F4/80highLy6G− cells,9 exhibited no differences in cytokine production compared to WT (Supplementary Figure 4). In mice treated with 5 days of DSS alone, we observed similar defects in TNFα production, but not IL-1β, by Nlrp6−/− Ly6Chi monocytes associated with increased fecal lipocalin levels in Nlrp6−/− mice (Supplementary Figure 5).
Figure 4. NLRP6 deficient Ly6Chi monocytes have reduced ROS and TNFα production during the acute inflammatory response to DSS.
(a) Ly6Chi monocytes were sorted from WT or Nlrp6−/− mice and incubated with GFP-labeled E.coli at MOI 0, 5, 25 and 60. Phagocytosis was measured by percent GFP+ Ly6Chi monocytes. Data are representative of two independent experiments, n=6. ROS production (MFI) as measured by CellROX deep red in BM- (b) or LP-derived (c) Ly6Chi monocytes at the indicated time points. Ly6Chi monocytes from WT or Nlrp6−/− mice were sorted from the LP after 5 days of 2% DSS (day 10, AOM/DSS model) or 6 days after completion of DSS (day 16, AOM/DSS model) and cytokine levels were measured by ELISA (d) and by qPCR (e). Data are representative of at least three independent experiments, mean ± SEM; n=14/genotype, (day 10); n=12/genotype (day 0); n=8/genotype (day 16). * - p<0.05, as compared to WT.
To determine if NLRP6 upregulation is associated with TNFα production, we sorted Ly6Chi monocytes from the BM of WT mice, and stimulated them with rosiglitazone, which was previously demonstrated to increase NLRP6 expression in colon epithelial cells.13 We indeed observed upregulation of NLRP6 expression when WT monocytes were treated with rosiglitazone (Supplementary Figure 6a) along with increased TNFα production in WT macrophages, which did not occur to the same extent in Nlrp6−/− Ly6Chi monocytes (Supplementary Figure 6b), suggesting that the TNFα response is indeed partially NLRP6 dependent. We next determined whether a defect in the recruitment of Nlrp6−/− inflammatory monocytes into the LP was associated with decreased TNFα production. However, examination of monocyte populations in the LP of WT and Nlrp6−/− mice on day 0 and day 10 after completion of 5 days of DSS showed, in fact, increased numbers of Ly6Chi monocytes recruited to the LP of Nlrp6−/− mice (Supplementary Figure 7). In order to determine if the impairment in TNFα production by Nlrp6−/− Ly6Chi monocytes was not a result of global deficiency in cytokine responses, we isolated inflammatory Ly6Chi monocytes from the LP of WT and Nlrp6−/− mice on day 10 of AOM/DSS treatment and performed gene expression analysis by microarray. Functional pathway analysis revealed increased mRNA expression of several cytokines and chemokines in Nlrp6−/− Ly6Chi cells, while TNFα was one of the few cytokines that was the most reduced (Supplemental Figure 8).
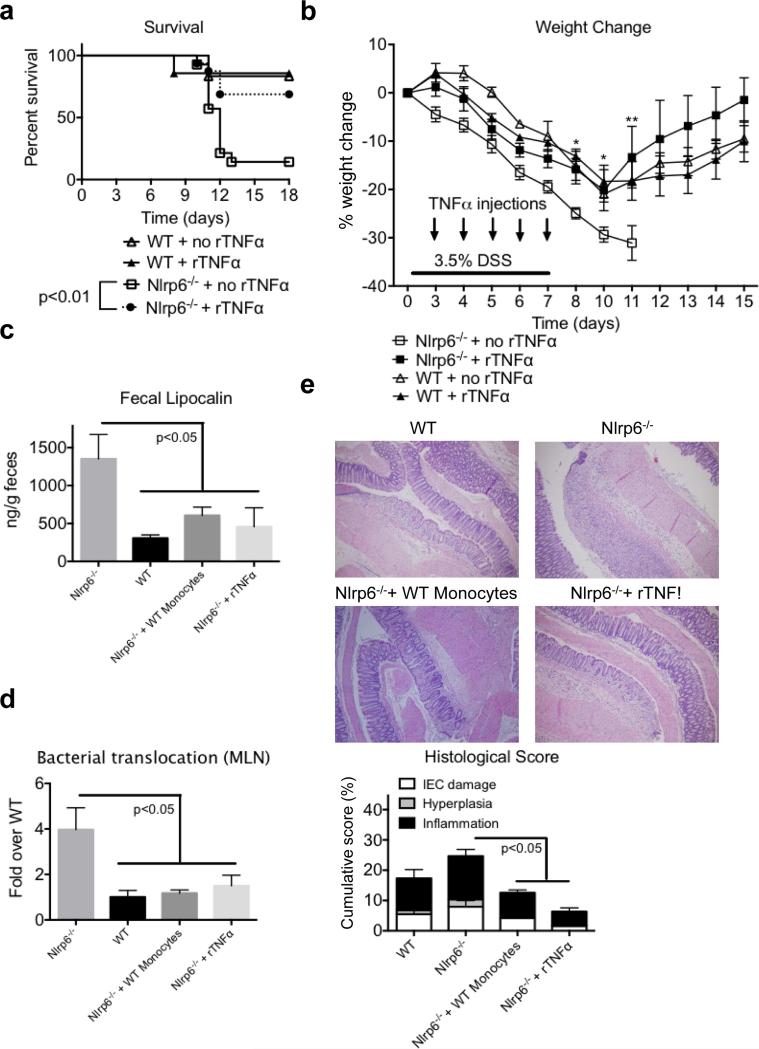
Early production of TNFα is important for resistance against DSS-induced intestinal injury
Elevated levels of TNFα have frequently been associated with disease severity in chronic IBD patients;14 however, TNFα also promotes epithelial restitution after DSS-induced injury.15 To determine whether the early production of TNFα by inflammatory monocytes is important for protection against intestinal damage and DSS-induced mortality, Nlrp6−/− mice were injected with rTNFα on days 3-7 during a 7 day course of high dose 3.5% DSS. As expected, the administration of rTNFα into WT mice had no effect on their survival (Figure 5a-b). In contrast, Nlrp6−/− mice that received rTNFα showed significant improvement in survival with decreased weight loss compared to Nlrp6−/− mice that did not receive supplemental rTNFα. There was reduced colonic inflammation and damage as suggested by decreased lipocalin-2 levels as well as less bacterial translocation into the MLNs in Nlrp6−/− mice that received rTNFα (Figure 5c-d). Finally, histologic examination of colons revealed a significant improvement in inflammatory scores for Nlrp6−/− mice that received rTNFα after 5 days of 2% DSS (day 10 AOM/DSS model), reflecting reduced levels of epithelial damage, hyperplasia, and inflammation (Figure 5e). Altogether, these results suggest that NLRP6 dependent production of TNFα by WT inflammatory monocytes is important for limiting intestinal damage and bacterial translocation, thereby reducing DSS-induced inflammation and mortality.
Figure 5. Recombinant TNFα administration into Nlrp6−/− mice early during DSS treatment reduces susceptibility to DSS-induced colitis.
(a) Kaplan–Meyer survival curves and (b) percent weight change of age- and sex-matched WT and Nlrp6−/− mice treated with 3.5% DSS for 7 days with or without rTNFα injections given on days 3-7. Data are representative of two independent experiments, mean ± SEM; n=15, n=16 for Nlrp6−/− and Nlrp6−/− + 1 μg/mouse rTNFα respectively; n=5 for WT and WT + 1 μg/mouse rTNFα (c) Fecal lipocalin-2 levels measured in WT and Nlrp6−/− mice (day 10, AOM/DSS model) after adoptive transfer of Ly6Chi monocytes or 1 μg TNF given on days 3-5 of DSS (d) Normalized levels of total bacteria/MLN as measured by qPCR after 5 days of 2% DSS (day 10 AOM/DSS model). (e) H&E micrographs at 100x after 5 days of 2% DSS (top) with histological scoring are shown. Bracket indicates diffuse ulceration with inflammatory infiltrate extending throughout the LP and submucosa; n=5, n=6, n=6, n=7 for WT, Nlrp6−/−, Nlrp6−/− + 1 μg/mouse rTNFα, and Nlrp6−/− + WT Ly6Chi monocytes groups respectively.
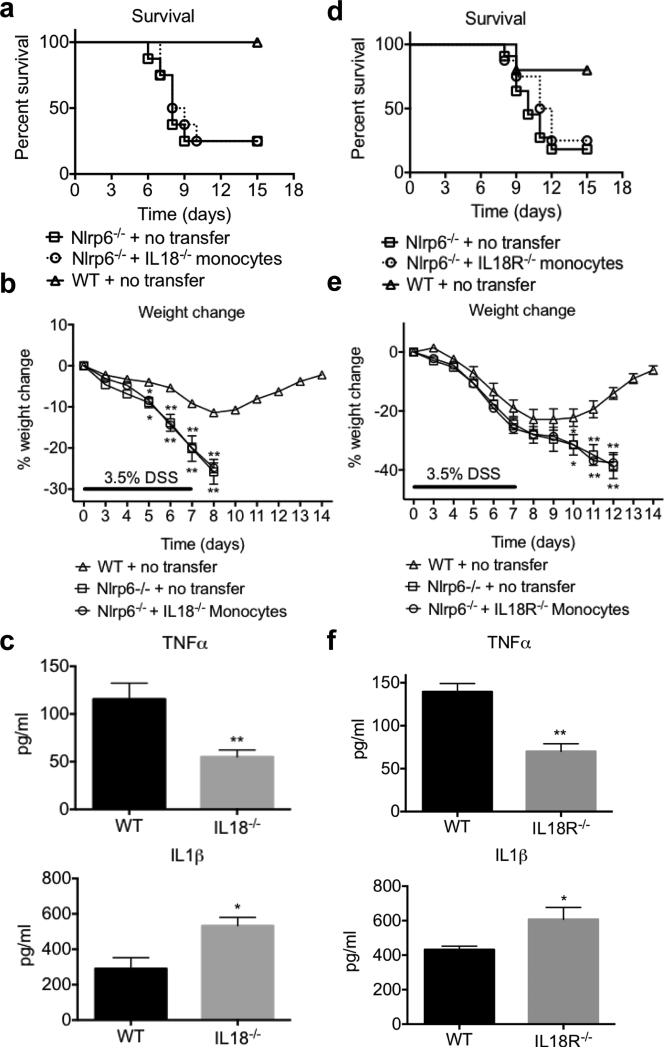
Production of TNFα by Ly6Chi inflammatory monocytes is dependent on IL-18 signaling
We have previously demonstrated that Nlrp6−/− mice have impaired production of mature IL-18, which is important for epithelial repair to limit commensal-driven inflammation.1 Although it was previously shown that IL-18 is predominantly produced by the intestinal epithelium,3 LP cells are also capable of secreting IL-18.16 Importantly, we also observed reduced levels of IL-18 production by Ly6hi inflammatory monocytes isolated from DSS-treated Nlrp6−/− mice compared to that from WT (Supplementary Figure 9). To determine if IL-18 production by Ly6Chi monocytes is important for resistance to DSS induced mortality, Nlrp6−/− mice were adoptively transferred with Il18−/− Ly6Chi monocytes, and survival of these mice was compared to that of mock-transferred Nlrp6−/− and WT mice after 7 days of 3.5% DSS (Figure 6a). Nlrp6−/− mice that received Il18−/− monocytes had similar levels of mortality and weight loss compared to Nlrp6−/− mice (Figure 6a,b). Interestingly, Ly6Chi monocytes isolated from DSS treated Il18−/− mice also had impaired production of TNFα, but not IL-1β, indicating that TNFα production by Ly6Chi monocytes is, in part, IL-18 dependent (Figure 6c).
Figure 6. Autocrine IL-18 production by Ly6Chi monocytes protects against DSS-induced colitis by increasing TNFα production.
Ly6Chi monocytes were purified from WT, Il18−/− or Il18r1−/− mice and i.v. injected (2×106 cells/mouse) into Nlrp6−/− recipients at day 3.5 of a 7 day course of 3.5% DSS. Mice survival (a) and weight loss (b) for WT, Nlrp6−/− and Nlrp6−/− + Il18−/− Ly6Chi monocytes was assessed. n=8/group (c) Ly6Chi monocytes were sorted from the LP after 5 days of 2% DSS (day 10 AOM/DSS model) from Il18−/− mice, and cytokine levels in overnight cultures were measured by ELISA. n=4 per group. Mice survival (d) and weight loss (e) after adoptive transfer of Il18R−/− Ly6Chi monocytes into Nlpr6−/− mice. n=5 for WT, n=11 for Nlrp6−/− and n=8 for Nlrp6−/− + Il18r1−/− Ly6Chi monocytes (f) Cytokine levels measured from culture supernatants of WT and Il18R−/− Ly6Chi monocytes after 5 days of 2% DSS (day 10 AOM/DSS model), n=4/group. *, ** - p<0.05, p<0.001.
To determine whether inflammatory monocytes respond to IL-18 to promote TNFα production and resistance to DSS, Nlrp6−/− mice were also adoptively transferred with Il-18R−/− monocytes and survival measured after treatment with high-dose DSS. Nlrp6−/− mice that received Il-18R−/− monocytes were equally susceptible to DSS induced mortality and weight loss as mock-treated Nlrp6−/− mice (Figure 6d, e). Furthermore, cultures of Ly6Chi cells isolated from DSS-treated Il18r1−/− mice also exhibited a defect in TNFα production, while secretion of IL-1β was actually increased rather than decreased (Figure 6f). These data strongly suggest that autocrine IL-18 signaling by inflammatory monocytes is important for regulating TNFα production early during the acute inflammatory response to DSS to promote resistance to intestinal injury and lethality.
Discussion
NLRP6 is a member of the NLR family that is important for maintaining intestinal homeostasis.3 Our studies provide important insights into the mechanism by which NLRP6 protects against the development of colitis. We show that NLRP6 functions particularly in Ly6Chi inflammatory monocytes that are recruited to the intestinal LP during inflammation to protect the host against DSS-induced epithelial injury and subsequent life-threatening immunopathology. NLRP6 deficiency in inflammatory monocytes was also associated with defective TNFα production early in response to DSS, which, in turn, is important for reducing mortality. Our data further suggest that TNFα production is mediated by autocrine IL-18 signaling by Ly6Chi inflammatory monocytes. Therefore, we propose a model in which NLRP6 activation in inflammatory monocytes recruited in response to DSS-induced inflammation results in IL-18 secretion that upregulates their production of TNFα, which promotes epithelial repair and timely resolution of damage.15
Although IL-18 levels can be elevated in patients with active inflammatory disease,16, 17 studies in mice have also demonstrated the protective effects of IL-18 as I118−/− and Il18r1−/− mice are more susceptible to colitis and colitis-associated colon tumorigenesis.18 This discrepancy may reflect differential roles of IL-18 that is dependent on timing and context. The production of IL-18 early during DSS-induced inflammation is important for epithelial restitution and resolution of inflammation, but in the setting of chronic, dysregulated inflammation, excessive IL-18 production can exacerbate disease.19 Consistently, impairment in IL-18 production during DSS-induced colitis by NLRP6-deficient mice is observed only early on during and after DSS treatment before the development of significant intestinal damage and inflammation.1 Our data demonstrates that Nlrp6−/− Ly6Chi monocytes in the LP also have impaired early IL-18 production. However, it is not currently known whether the reduced IL-18 secretion is due to decreased inflammasome-mediated caspase-1 activation or reflects a defect in a non-canonical mechanism that remains to be identified. In addition, the mechanism for IL-18-mediated protection is unclear. Previous studies suggested that IL-18 is predominantly expressed by the epithelium and that epithelial-derived IL-18 is important for protection against DSS-induced damage.3, 20 IL-18 production is also associated with upregulation of IL-22, which is implicated in epithelial repair.21 Our study suggests an additional mechanism for IL-18 function, which is to upregulate TNFα production in inflammatory monocytes.
TNFα levels can be significantly elevated in IBD patients, and TNFα antagonism is an approved therapy for IBD. The excessive production of TNFα observed in patients with IBD and in mouse models of colitis likely reflects active disease that is already chronic and dysregulated. However, similar to IL-18, early production of TNFα is important for tissue repair and maintaining intestinal homeostasis.15, 22-24 Germ free mice or mice that lack the adaptor protein MyD88, which functions downstream of TLR-mediated bacterial sensing, have significant DSS-induced epithelial damage associated with the lack of induction of reparative cytokines, including TNFα.15, 25 In addition, TNFα blockade in WT mice results in increased susceptibility to colitis.22, 24 Tnfr1−/− or Tnfr2−/− mice as well as Tnfα−/− mice also develop more severe DSS-induced colitis with elevated levels of pro-inflammatory cytokines, increased epithelial damage, and increased mortality as compared to WT mice.24, 26-28 Although there has been conflicting data that demonstrate a pathogenic role for TNFR2 in DSS-induced colitis,29 inflammatory monocytes are more likely to express TNFR1, while TNFR2 upregulation in colonic epithelial cells is observed in patients with inflammatory bowel disease.30, 31 Altogether, these studies are consistent with our data since Nlrp6−/− mice that receive rTNFα early during DSS treatment exhibit reduced intestinal inflammation and bacterial translocation.
We previously demonstrated that NLRP6 functions in a BM-derived cell to limit inflammation-associated tumorigenesis.1 In the current study, we show that NLRP6 was induced specifically in myeloid cells within the LP during DSS-induced colitis. Furthermore, NLRP6 activity in Ly6Chi monocytes is important for reducing susceptibility to DSS-induced colitis. Despite the protection against the detrimental effects of inflammation, we did not see a statistically significant reduction in the number of tumors. Rather, the size of tumors was significantly decreased, suggesting that NLRP6 function in monocytes limits inflammation that primarily drives tumor growth. Consistently, the downregulation of inflammatory responses by removal of NF-kB activity in myeloid cells also resulted in reduced tumor size rather than tumor number.33 However, it is also possible that the administration of Ly6Chi monocytes only once with each DSS cycle is insufficient to affect tumor number, or that another BM-derived cell in addition to monocytes is necessary for protection.
There are two major populations of monocytes in the murine intestinal LP, classical Ly6Chi inflammatory monocytes and Ly6C− monocytes that differentiate into macrophages.11 Ly6Chi monocytes can be further differentiated by their expression level of CX3CR1.34, 35 LP Ly6Chi monocytes can differentiate into CX3CRhi resident macrophages or effector CX3CR1int inflammatory monocytes whose primary function is to rapidly produce pro-inflammatory cytokines after their recruitment to sites of inflammation and injury. Our data strongly indicates that during DSS-induced inflammation, the majority of Ly6Chi monocytes that are recruited to the LP express CX3CR1 and adoptively transferred Ly6Chi inflammatory monocytes recruited to the intestinal LP are predominantly Ly6ChiCX3CR1int (Supplementary Figure 3), consistent with previous studies.36 Although inflammatory monocytes have been implicated in exacerbating colitis since they are capable of producing pro-inflammatory factors, and are found in increased numbers in persistently inflamed tissue,11, 32 they also play important roles in restoring homeostasis and limiting damage. This is largely through their ability to be early responders to tissue injury and produce cytokines, including TNFα and IL18 that have reparative functions thereby allowing epithelial restitution and resolution of inflammation.9 Consistently, depletion of intestinal monocytes in WT mice resulted in increased susceptibility to colitis.37 Our data further highlight a positive impact by Ly6Chi monocytes via NLRP6 as an early source of TNFα to prevent uncontrolled inflammation in response to epithelial damage. NLRP6-deficiency in Ly6Chi monocytes is also associated with defective ROS production, which may further limit translocation of bacteria and exacerbation of intestinal inflammation.38 Indeed, the adoptive transfer of Ly6Chi monocytes resulted in reduced bacterial translocation and improved barrier function. It is possible that the decreased ROS production is related to defective production of TNFα, which is needed to promote the assembly of the NADPH oxidase complex that produces ROS.39 Nonetheless, these results are somewhat surprising in light of the study by Anand et al., which suggests that NLRP6 negatively regulates cytokine responses, including TNFα, in BM-derived macrophages (BMDMs) after exposure to bacterial ligands.12 One possible explanation for this disparate finding is that BMDMs cultured in vitro represent a population distinct from inflammatory monocytes. In fact, we demonstrate that not all monocyte populations regulate TNFα production via NLRP6 as we observed no difference in TNFα production between WT and Nlrp6−/− LP resident macrophages. Thus, it is likely that differential TNFα responses reflect not only differences in the particular cell population and location, but also the context in which inflammation occurs.
How NLRP6 promotes TNFα production in inflammatory monocytes remains to be fully elucidated. The lack of a known NLRP6 receptor agonist has made the identification of cognate signaling pathways challenging. However, our data suggest that the mechanism may be mediated indirectly through the regulation of IL-18 production in monocytes. The adoptive transfer of Il18−/− or Il18r1−/− monocytes into Nlrp6−/− mice failed to rescue DSS-induced mortality, suggesting that autocrine IL-18 signaling by inflammatory monocytes is important for protection against DSS-induced colitis. Furthermore, both Il18−/− and Il18r1−/− monocytes isolated from DSS-treated mice have impaired production of TNFα similar to that observed with Nlrp6−/− monocytes, consistent with a role for NLPR6 in regulating TNFα production in monocytes via IL-18. Although IL-18 is typically associated with the upregulation of Th1 responses, and in particular, IFNγ,40 IL-18 has also been shown to activate monocytes to enhance TNFα production,41, 42 consistent with our data.
In summary, our studies highlight a previously unrecognized role for NLRP6 in modulating IL-18-dependent TNFα production in inflammatory Ly6Chi monocytes that can act as early responders to an inflammatory insult, thereby limiting bacterial translocation, promoting timely epithelial repair, and preventing the onset of dysregulated inflammation. Our data additionally suggest that early production of IL-18 to promote resistance against DSS-induced colitis is mediated not only by the intestinal epithelium, but also by inflammatory monocytes through NLRP6. Together, these results suggest that modulation of NLRP6 activity may be a potential strategy for the prevention and treatment of inflammatory bowel disease.
Materials and Methods
Animal procedures
Adult 7-11 weeks old C57BL/6 WT, Nlrp6−/− , Il18−/− or Il18r1−/− , and GFP+ transgenic C57BL/6 (C57BL/6-Tg(UBC-GFP)30Scha/J) mice were bred in-house under specific pathogen free (SPF) conditions at the University of Michigan. WT, Il18−/− and Il18r1−/− ,GFP+, CCR2−/− and CX3CR1gfp mice mice (all B6 background) were originally purchased from Jackson. Nlrp6−/− in B6 background were previously described.1 Animal studies were conducted under protocols approved by the University of Michigan Committee on the Use and Care of Animals.
DSS-induced colitis and AOM/DSS-induced tumorigenesis
To induce colitis and lethality, mice were treated with 3.5% DSS (MP Biomedicals; m.w. 36,000– 50,000 Da) in regular drinking water for 7 days. To develop colitis-associated tumors, mice were first injected with 10 mg/kg AOM(Sigma) i.p., followed by 5 days of 2% DSS starting on day 5. Mice were allowed to recover for 16 days with regular drinking water, and then treated with two additional cycles of 2% DSS (Figure 2A). Mice were sacrificed after the last cycle of DSS for tumor counting and size measurement by calipers.
Isolation of lamina propria cells
LP cells were isolated as previously described.1 Briefly, colons were cut into small pieces in HBSS buffer (Gibco) supplemented with 2.5% heat-inactivated FBS (Gibco) (HBSS+), and washed with magnetic stirring at 37°C. Colon pieces were then incubated in HBSS+/1 mM DTT at 37°C followed by additional washes and incubation in HBSS+/1mM EDTA. The supernatant containing IECs and IELs was saved for further analysis. The remaining colon pieces were further digested with 400 I.U./mL Type III collagenase (Worthington) and 10 μg/mL DNase I (Worthington) for two hours at 37°C. When all tissue was digested, the cell suspension was filtered through a 70 micron filter, before running on a 75%/40% Percoll gradient to collect enriched LP cells from the interface.
Flow Cytometry
Cell suspensions were treated with anti CD16/CD32 (2.4G2) and then surface stained with combinations of the following fluorochrome-conjugated antibodies: From Biolegend: CD3e–FITC (clone: 145 2C11), Ly6C–FITC or APC/Cy7 (clone: HK1.4), Ly6G–PE/Cy7 (clone: 1A8), CD3e–APC/Cy7 (clone: 145 2C11), CD45R/B220–Pacific Blue (clone: RA3 6B2), CCR2-AlexaFluor647 (clone: SA203G11), CX3CR1-APC (clone: SA011F11), IgG2A,κ-APC isotype control; from BD Biosciences: NK1.1–PerCP/Cy5.5 (clone: PK136); from Ebiosciences: F4/80–APC (clone: BM8), CD4 (L3T4)–FITC (clone: RM4 5), CD11b–FITC (clone: M1/70), CD11b–PE (clone: M1/70), CD4–APC (clone: GK1.5). Cells were acquired on FACSCanto or AriaIII flow cytometers using FACSDiVa software, and data were analyzed using FlowJo software (Tree Star).
Adoptive transfer experiments
WT, Ccr2−/− or CX3CR1gfp mice were used as donors. Single-cell suspensions were prepared from flushed BM in fully supplemented RPMI followed by lysis of red blood cells and isolation of Ly6Chi monocytes (CD3− CD11b+Ly6ChiLy6G−) by FACs sorting. Two million cells were injected i.v. into Nlrp6−/− , WT or Ccr2−/− recipient mice.
Treatment of mice with recombinant TNFα
WT or Nlrp6−/− mice were administered 1 μg of sterilely filtered recombinant mouse TNFα (PreproTech) i.p. on days 3-7 in the 3.5% DSS colitis model (days 3-7) or days 8-10 in the AOM/ DSS colitis and tumorigenesis model.
Assessment of colon inflammation
Colons were flushed free of feces, opened longitudinally, and jelly-rolled for formalin fixation and paraffin embedding. 5-micron sections were used for H&E staining. Histological assessment was performed in a blinded fashion by a pathologist (KE) using a previously described scoring system1 with modifications. Entire colon sections were assessed for three main parameters: inflammatory cell infiltration, hyperplasia and epithelial damage that were individually scored (0 to 4), (Supplementary Table I). For each mouse, a weighted percent average based on the number of fields with a certain score was calculated for each parameter and then summed to obtain the final score. Assessment of colon weight after DSS treatment was performed by measuring the colon weight (excluding the cecum) after removal of feces normalized by its length (cm).
Intestinal permeability
Mice were fasted for 8 hours with the exception of drinking water prior to the administration of 0.6 mg/kg FITC-dextran (4 kDa; Sigma-Aldrich) by oral gavage. Serum was collected 4 hours later, diluted 1:3 in PBS, and fluorescence measured using a fluorescent spectrophotometer with emission at 488 nm and absorption at 525 nm.
Reverse transcription and quantitative real-time polymerase chair reaction (qPCR)
Total RNA was isolated from LP, BM cells, or from sorted populations of LP cells using the Nucleospin RNA kit (Machery-Nagel). cDNA synthesis was performed using iScript (Bio-Rad), and cDNA was used for qPCR using the SYBR Green Master Mix (Applied Biosystems) on the ABI 7900HT (Applied Biosystems). Ct values were normalized to the β-actin gene. Primer sequences are available upon request.
ELISA
To measure fecal lipocalin-2 levels, fecal samples were homogenized in PBS at 100 mg/ml and supernatant was further diluted in a range of 1:500 to 1:5000 for lipocalin-2/NGAL ELISA (R&D Systems). TNFα, IL-6 and IL-1β ELISAs (all R&D Systems) were performed with 24-hour culture supernatants of Ly6Chi monocytes.
Measurement of ROS
Total cellular ROS were measured by CellROX Deep Red reagent kit (Invitrogen) according to the manufacturer's protocol. Briefly, upon surface staining for flow cytometry, cells were resuspended in 200 μl of pre-warmed HBSS + 2.5 mM Probenecid + CellROX, incubated for 30 minutes at 37° C (in the dark), washed and acquired on FACSCanto or AriaIII flow cytometers (BD Bioscience). CellROX Deep Red has peak excitation and emission at 640 nm and 665 nm.
Phagocytosis assay
eGFP-expressing Eschericha coli (K12) was a kind gift from Gabriel Nunez (University of Michigan). Ly6Chi monocytes were specifically sorted from WT or Nlrp6−/− mice at day 10 of AOM/DSS and incubated for 1.5 hours with E. coli GFP at multiplicity of infection (MOI) 0, 5, 25 or 60. Zombie Violet viability die (Biolegend) was used to identify live Ly6Chi monocytes, which phagocytized GFP+ E.coli using FACSCanto or AriaIII flow cytometers (BD Bioscience).
Bacterial translocation
MLNs were homogenized in PBS by passing through a 70 micron strainer and then plated on Trypticase Soy Agar with 5% Sheep Blood (TSA II) plates (BD) to determine CFUs after 24-hour incubation under aerobic conditions or 48-hours under anaerobic conditions. Total DNA was extracted using the Nucleospin kit (Machery-Nagel), and bacterial load quantified by qPCR the universal 16S rRNA gene primers EUB-For-5’-AGAGTTTGATCCTGGCTC-3’ and EUB-Rev-5’-TGCTGCCTCCCGTAGGAGT-3’.
Statistical analysis
Statistically significant differences were determined using Two-way ANOVA with a Bonferroni post-hoc test (time × genotype, p<0.05), by One Way ANOVA with a Student-Newman-Keuls post-hoc test (p value < 0.05), or by 2 tailed Student's unpaired t test when only 2 groups are compared. Survival curve comparison was performed by Mantel-Cox log-rank test. Kruskal–Wallis one-way analysis of variance non-parametric test was used for non-continuous variables. Data are shown as mean ± SEM. GraphPad Prism6 software was utilized for statistical analysis.
Supplementary Material
Acknowledgements
This work was supported by the National Institutes of Health grant R01CA166879 and American Cancer Society Research Scholar Grant awarded to GYC, National Institutes of Health grant F32CA200144 awarded to SSS and by grant number UL1TR000433 from the National Center for Advancing Translational Sciences awarded to SSS.
Footnotes
Disclosure
The authors have declared that no conflict of interest exists.
References
- 1.Chen GY, Liu M, Wang F, Bertin J, Nunez G. A functional role for Nlrp6 in intestinal inflammation and tumorigenesis. J Immunol. 2011;186(12):7187–7194. doi: 10.4049/jimmunol.1100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen GY. Role of Nlrp6 and Nlrp12 in the maintenance of intestinal homeostasis. Eur J Immunol. 2013;44(2):321–327. doi: 10.1002/eji.201344135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elinav E, Strowig T, Kau AL, Henao-Mejia J, Thaiss CA, Booth CJ, et al. NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell. 2011;145(5):745–757. doi: 10.1016/j.cell.2011.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Normand S, Delanoye-Crespin A, Bressenot A, Huot L, Grandjean T, Peyrin-Biroulet L, et al. Nod-like receptor pyrin domain-containing protein 6 (NLRP6) controls epithelial self-renewal and colorectal carcinogenesis upon injury. Proc Natl Acad Sci U S A. 2011;108(23):9601–9606. doi: 10.1073/pnas.1100981108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allen IC, TeKippe EM, Woodford RM, Uronis JM, Holl EK, Rogers AB, et al. The NLRP3 inflammasome functions as a negative regulator of tumorigenesis during colitis associated cancer. J Exp Med. 2010;207(5):1045–1056. doi: 10.1084/jem.20100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaki MH, Boyd KL, Vogel P, Kastan MB, Lamkanfi M, Kanneganti TD. The NLRP3 inflammasome protects against loss of epithelial integrity and mortality during experimental colitis. Immunity. 2010;32(3):379–391. doi: 10.1016/j.immuni.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wlodarska M, Thaiss CA, Nowarski R, Henao Mejia J, Zhang JP, Brown EM, et al. NLRP6 inflammasome orchestrates the colonic host microbial interface by regulating goblet cell mucus secretion. Cell. 2014;156(5):1045–1059. doi: 10.1016/j.cell.2014.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5(12):953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 9.Zigmond E, Varol C, Farache J, Elmaliah E, Satpathy AT, Friedlander G, et al. Ly6C hi monocytes in the inflamed colon give rise to proinflammatory effector cells and migratory antigen presenting cells. Immunity. 2012;37(6):1076–1090. doi: 10.1016/j.immuni.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 10.Sherwood RA. Faecal markers of gastrointestinal inflammation. J Clin Pathol. 2012;65(11):981–985. doi: 10.1136/jclinpath-2012-200901. [DOI] [PubMed] [Google Scholar]
- 11.Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol. 2011;11(11):723–737. doi: 10.1038/nri3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anand PK, Malireddi RK, Lukens JR, Vogel P, Bertin J, Lamkanfi M, et al. NLRP6 negatively regulates innate immunity and host defence against bacterial pathogens. Nature. 2012;488(7411):389–393. doi: 10.1038/nature11250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kempster SL, Belteki G, Forhead AJ, Fowden AL, Catalano RD, Lam BY, et al. Developmental control of the Nlrp6 inflammasome and a substrate, IL-18, in mammalian intestine. Am J Physiol Gastrointest Liver Physiol. 2010;300(2):G253–263. doi: 10.1152/ajpgi.00397.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reinecker HC, Steffen M, Witthoeft T, Pflueger I, Schreiber S, MacDermott RP, et al. Enhanced secretion of tumour necrosis factor alpha, IL-6, and IL-1 beta by isolated lamina propria mononuclear cells from patients with ulcerative colitis and Crohn's disease. Clin Exp Immunol. 1993;94(1):174–181. doi: 10.1111/j.1365-2249.1993.tb05997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll like receptors is required for intestinal homeostasis. Cell. 2004;118(2):229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Pizarro TT, Michie MH, Bentz M, Woraratanadharm J, Smith MF, Jr., Foley E, et al. IL-18, a novel immunoregulatory cytokine, is up regulated in Crohn's disease: expression and localization in intestinal mucosal cells. J Immunol. 1999;162(11):6829–6835. [PubMed] [Google Scholar]
- 17.Furuya D, Yagihashi A, Komatsu M, Masashi N, Tsuji N, Kobayashi D, et al. Serum interleukin-18 concentrations in patients with inflammatory bowel disease. J Immunother. 2002;25(Suppl 1):S65–67. doi: 10.1097/00002371-200203001-00010. [DOI] [PubMed] [Google Scholar]
- 18.Salcedo R, Worschech A, Cardone M, Jones Y, Gyulai Z, Dai RM, et al. MyD88 mediated signaling prevents development of adenocarcinomas of the colon: role of interleukin 18. J Exp Med. 2010;207(8):1625–1636. doi: 10.1084/jem.20100199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siegmund B. Interleukin-18 in intestinal inflammation: friend and foe? Immunity. 2010;32(3):300–302. doi: 10.1016/j.immuni.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Dupaul-Chicoine J, Yeretssian G, Doiron K, Bergstrom KS, McIntire CR, LeBlanc PM, et al. Control of intestinal homeostasis, colitis, and colitis-associated colorectal cancer by the inflammatory caspases. Immunity. 2010;32(3):367–378. doi: 10.1016/j.immuni.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 21.Huber S, Gagliani N, Zenewicz LA, Huber FJ, Bosurgi L, Hu B, et al. IL-22BP is regulated by the inflammasome and modulates tumorigenesis in the intestine. Nature. 2012;491(7423):259–263. doi: 10.1038/nature11535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naito Y, Takagi T, Handa O, Ishikawa T, Nakagawa S, Yamaguchi T, et al. Enhanced intestinal inflammation induced by dextran sulfate sodium in tumor necrosis factor alpha deficient mice. J Gastroenterol Hepatol. 2003;18(5):560–569. doi: 10.1046/j.1440-1746.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 23.Noti M, Corazza N, Mueller C, Berger B, Brunner T. TNF suppresses acute intestinal inflammation by inducing local glucocorticoid synthesis. J Exp Med. 2010;207(5):1057–1066. doi: 10.1084/jem.20090849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Han G, Chen Y, Wang K, Liu G, Wang R, et al. Protective role of tumor necrosis factor (TNF) receptors in chronic intestinal inflammation: TNFR1 ablation boosts systemic inflammatory response. Lab Invest. 2013;93(9):1024–1035. doi: 10.1038/labinvest.2013.89. [DOI] [PubMed] [Google Scholar]
- 25.Zhan Y, Chen PJ, Sadler WD, Wang F, Poe S, Nunez G, et al. Gut microbiota protects against gastrointestinal tumorigenesis caused by epithelial injury. Cancer Res. 2013;73(24):7199–7210. doi: 10.1158/0008-5472.CAN-13-0827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edelblum KL, Goettel JA, Koyama T, McElroy SJ, Yan F, Polk DB. TNFR1 promotes tumor necrosis factor-mediated mouse colon epithelial cell survival through RAF activation of NF-kappaB. J Biol Chem. 2008;283(43):29485–29494. doi: 10.1074/jbc.M801269200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feng Y, Teitelbaum DH. Tumour necrosis factor--induced loss of intestinal barrier function requires TNFR1 and TNFR2 signalling in a mouse model of total parenteral nutrition. J Physiol. 2013;591(Pt 15):3709–3723. doi: 10.1113/jphysiol.2013.253518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stillie R, Stadnyk AW. Role of TNF receptors, TNFR1 and TNFR2, in dextran sodium sulfate-induced colitis. Inflamm Bowel Dis. 2009;15(10):1515–1525. doi: 10.1002/ibd.20951. [DOI] [PubMed] [Google Scholar]
- 29.Wang K, Han G, Dou Y, Wang Y, Liu G, Wang R, et al. Opposite role of tumor necrosis factor receptors in dextran sulfate sodium-induced colitis in mice. PLoS One. 2012;7(12):e52924. doi: 10.1371/journal.pone.0052924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naude PJ, den Boer JA, Luiten PG, Eisel UL. Tumor necrosis factor receptor cross-talk. FEBS J. 2011;278(6):888–898. doi: 10.1111/j.1742-4658.2011.08017.x. [DOI] [PubMed] [Google Scholar]
- 31.Hijdra D, Vorselaars AD, Grutters JC, Claessen AM, Rijkers GT. Differential expression of TNFR1 (CD120a) and TNFR2 (CD120b) on subpopulations of human monocytes. J Inflamm (Lond) 2012;9(1):38. doi: 10.1186/1476-9255-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varol C, Zigmond E, Jung S. Securing the immune tightrope: mononuclear phagocytes in the intestinal lamina propria. Nat Rev Immunol. 2010;10(6):415–426. doi: 10.1038/nri2778. [DOI] [PubMed] [Google Scholar]
- 33.Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ, et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004;118(3):285–296. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 34.Bain CC, Mowat AM. The monocyte-macrophage axis in the intestine. Cell Immunol. 2014 doi: 10.1016/j.cellimm.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bain CC, Mowat AM. Macrophages in intestinal homeostasis and inflammation. Immunol Rev. 2014;260(1):102–117. doi: 10.1111/imr.12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bain CC, Scott CL, Uronen Hansson H, Gudjonsson S, Jansson O, Grip O, et al. Resident and pro-inflammatory macrophages in the colon represent alternative context-dependent fates of the same Ly6Chi monocyte precursors. Mucosal Immunol. 2013;6(3):498–510. doi: 10.1038/mi.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qualls JE, Kaplan AM, van Rooijen N, Cohen DA. Suppression of experimental colitis by intestinal mononuclear phagocytes. J Leukoc Biol. 2006;80(4):802–815. doi: 10.1189/jlb.1205734. [DOI] [PubMed] [Google Scholar]
- 38.Molloy MJ, Grainger JR, Bouladoux N, Hand TW, Koo LY, Naik S, et al. Intraluminal containment of commensal outgrowth in the gut during infection-induced dysbiosis. Cell Host Microbe. 2013;14(3):318–328. doi: 10.1016/j.chom.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bayir H. Reactive oxygen species. Crit Care Med. 2005;33(12 Suppl):S498–501. doi: 10.1097/01.ccm.0000186787.64500.12. [DOI] [PubMed] [Google Scholar]
- 40.Nakanishi K, Yoshimoto T, Tsutsui H, Okamura H. Interleukin-18 regulates both Th1 and Th2 responses. Annu Rev Immunol. 2001;19:423–474. doi: 10.1146/annurev.immunol.19.1.423. [DOI] [PubMed] [Google Scholar]
- 41.Dai SM, Matsuno H, Nakamura H, Nishioka K, Yudoh K. Interleukin-18 enhances monocyte tumor necrosis factor alpha and interleukin-1beta production induced by direct contact with T lymphocytes: implications in rheumatoid arthritis. Arthritis Rheum. 2004;50(2):432–443. doi: 10.1002/art.20064. [DOI] [PubMed] [Google Scholar]
- 42.Dias-Melicio LA, Fernandes RK, Rodrigues DR, Golim MA, Soares AM. Interleukin 18 increases TLR4 and mannose receptor expression and modulates cytokine production in human monocytes. Mediators Inflamm. 2015;2015:236839. doi: 10.1155/2015/236839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahmadian M, Suh JM, Hah N, Liddle C, Atkins AR, Downes M, et al. PPARgamma signaling and metabolism: the good, the bad and the future. Nat Med. 2013;19(5):557–566. doi: 10.1038/nm.3159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Adachi M, Kurotani R, Morimura K, Shah Y, Sanford M, Madison BB, et al. Peroxisome proliferator activated receptor gamma in colonic epithelial cells protects against experimental inflammatory bowel disease. Gut. 2006;55(8):1104–1113. doi: 10.1136/gut.2005.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shah YM, Morimura K, Gonzalez FJ. Expression of peroxisome proliferator activated receptor-gamma in macrophage suppresses experimentally induced colitis. Am J Physiol Gastrointest Liver Physiol. 2007;292(2):G657–666. doi: 10.1152/ajpgi.00381.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.