Enlarged deep medullary veins are considered to be developmental venous anomalies associated with various etiologies including Sturge-Weber syndrome (SWS).1–4 Such deep veins may provide collateral blood flow through the deep venous system following the blockade of the superficial cortical veins by the SWS leptomeningeal venous malformation.2 MRI with susceptibility-weighted imaging (SWI) is sensitive to detect such deep veins.3,4 However, postnatal appearance of enlarged deep medullary veins has not been documented in SWS.
We present 2 children with SWS who developed enlarged medullary veins during the early clinical disease course. These children were identified from a group of 15 children with SWS (median age 3.5 years) who underwent longitudinal multimodal neuroimaging including SWI and postgadolinium T1 (T1-Gad) images on a 3T scanner as well as glucose PET along with neurocognitive evaluations (Bayley Scales of Infant and Toddler Development, 2nd edition, for children younger than 30 months, and Wechsler Preschool and Primary Scale of Intelligence, 3rd edition, for children 30–87 months) to estimate global intellectual functioning (IQ). They all participated in a research study approved by the Wayne State University Human Investigation Committee.
Case reports.
Patient 1.
A 7-month-old girl had a right facial port wine birthmark and extensive right hemispheric involvement with leptomeningeal contrast enhancement and a few enlarged medullary veins in the parietal and temporal lobes on baseline MRI (figure 1A). Follow-up MRI 2 years later detected a large medullary vein connecting the frontal cortex with the periventricular veins (figure 1A and figure e-1 at Neurology.org). This vein was visualized on both SWI and T1-Gad images and showed a typical corkscrew configuration. Baseline PET showed mild increased glucose uptake in the right fronto-temporo-parietal cortex, consistent with transient interictal hypermetabolism previously described in children with SWS.5 This progressed to severe hypometabolism at follow-up in the parietal cortex, while the frontal cortex metabolism showed only minimal hypometabolism (figure 1A). The child had occasional seizures, minimal left hemiparesis, and stable IQ (70 at baseline and 72 at follow-up).
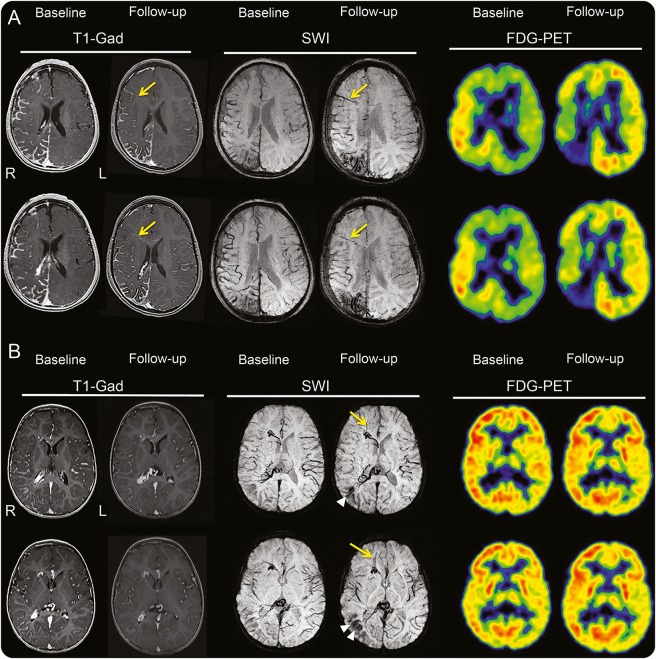
Figure 1. Baseline and follow-up MRI and PET of the 2 patients.
(A) A 7-month-old girl with extensive right hemispheric involvement at baseline. Both postgadolinium (T1-Gad) and susceptibility-weighted images (SWI) show a new deep medullary vein (yellow arrows) connecting the lateral frontal cortex with the periventricular area at follow-up (age 31 months); this vein is not visualized on the baseline images, which show isolated medullary veins only in the posterior regions, where interval progression of calcification is detected along with development of severe hypometabolism on PET. The temporo-parietal cortex shows transient interictal hypermetabolism progressing to hypometabolism, while the frontal region shows only minimal hypometabolism at follow-up. (B) A 21-month-old boy with right posterior leptomeningeal enhancement, enlarged medullary veins in the frontal and posterior regions, and enlarged choroid plexus at baseline. SWI detects a cluster of additional, new deep medullary veins (yellow arrows) connecting the frontal pole with the periventricular veins on the follow-up images (age 3 years). SWI also shows progressive calcification in the right posterior quadrant (white arrowheads). PET shows no interval decrease of glucose metabolism.
Patient 2.
A 21-month-old boy had a right facial port wine birthmark and right hemispheric involvement including temporo-parieto-occipital leptomeningeal enhancement, enlarged choroid plexus, and deep medullary veins (figure 1B). Follow-up SWI 15 months later showed new deep medullary veins in the right prefrontal region, connecting the anterior frontal cortex with enlarged periventricular veins (figures 1B and e-1). Baseline PET showed largely symmetric glucose metabolism with no progression at follow-up. He remained seizure-free, had only minimal monoparesis in his left hand, and his IQ was 92 (up from 58 at baseline).
Discussion.
While de novo formation of arteriovenous malformations has been reported,6 the present study provides the first imaging evidence of postnatal appearance of enlarged deep medullary veins in SWS.
In the healthy brain, venous blood from cerebral cortex and subcortical white matter is drained through surface veins, while that from deep white and gray matter is drained to the deep venous system.7 These 2 systems are connected by transmedullary anastomoses, but their functional significance is marginal under physiologic conditions. Early obliteration of the superficial venous drainage can lead to diversion of venous flow from the cortex to the deep venous system with resultant increase in venous pressure, thus redirecting the venous blood towards the deep venous system.1,2 Our data could be consistent with deep venous remodeling not completed during fetal life but continuing during the early clinical course of SWS.
The clinical relevance of frontal lobe deep venous collaterals in SWS remains to be determined. In our 2 children with newly developed medullary veins, the affected frontal lobe showed preserved cortical metabolism during follow-up, suggesting good cortical function. Contrast enhancement in the new deep vein in the younger child indicated blood flow. However, no contrast enhancement was seen in the SWI-detected new veins of patient 2; this could be explained either by the small diameter of these blood vessels or by the paucity (or lack) of actual blood flow through them, possibly due to venous thrombosis. Nevertheless, this child showed no metabolic progression on PET and had only minimal motor deficit and good cognitive development.
These imaging data provide evidence for the postnatal development of enlarged deep medullary veins during the early clinical course of SWS. Such deep veins may represent a venous vascular compensatory mechanism by which superficial brain areas acquire collateral drainage through the deep venous system. This may contribute to maintaining the functional integrity of the affected lobe as suggested by largely intact glucose metabolism demonstrated by longitudinal PET imaging. Whether venous remodeling continues during the later disease course will require longer imaging follow-up.
Supplementary Material
Acknowledgments
Acknowledgment: The authors thank Cathie Germain, MA, and Cynthia Burnett, BA, for assistance with patient scheduling; Jane Cornett, RN, and Anne Deboard, RN, for performing sedation for imaging; Yang Xuan, BS, for MRI acquisition and preprocessing; and Michael Behen, PhD, for cognitive assessment of the patients.
Footnotes
Supplemental data at Neurology.org
Author contributions: Vinod Pilli: performed image processing, analysis, and interpretation; prepared illustrations; and drafted the manuscript. Harry T. Chugani: involved in study conception and design, patient recruitment and follow-up, data interpretation, and revision of the manuscript. Csaba Juhasz: involved in study conception and design, assisted patient recruitment, supervised data collection and analysis, and revised and finalized the manuscript.
Study funding: NIH (NS041922).
Disclosure: V. Pilli has received salary support from grant 041922 from the National Institute of Neurologic Disorders and Stroke (NINDS). H. Chugani has received research support from NINDS grants NS041922, NS064989, NS079429, NS064033, and NS089659, and Department of Defense grant TS130067. C. Juhász has received research support from NINDS grants NS041922, NS064033, NS089659, and NS065705, and National Cancer Institute grant CA123451. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Ruíz DS, Yilmaz H, Gailloud P. Cerebral developmental venous anomalies: current concepts. Ann Neurol 2009;66:271–283. [DOI] [PubMed] [Google Scholar]
- 2.Parsa CF. Sturge-Weber syndrome: a unified pathophysiologic mechanism. Curr Treat Options Neurol 2008;10:47–54. [DOI] [PubMed] [Google Scholar]
- 3.Mentzel HJ, Dieckmann A, Fitzek C, Brandl U, Reichenbach JR, Kaiser WA. Early diagnosis of cerebral involvement in Sturge-Weber syndrome using high-resolution BOLD MR venography. Pediatr Radiol 2005;35:85–90. [DOI] [PubMed] [Google Scholar]
- 4.Juhász C, Haacke M, Hu J, et al. Multimodality imaging of cortical and white matter abnormalities in Sturge-Weber syndrome. AJNR Am J Neuroradiol 2007;28:900–906. [PMC free article] [PubMed] [Google Scholar]
- 5.Alkonyi B, Chugani HT, Juhász C. Transient focal increase of interictal glucose metabolism in Sturge-Weber syndrome: implications for epileptogenesis. Epilepsia 2011;52:1265–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koch MJ, Agarwalla PK, Stapleton CJ, et al. De novo development of a cerebral arteriovenous malformation following radiation therapy: case report and an update to classical arteriovenous malformation nomenclature. J Clin Neurosci 2016;28:162–167. [DOI] [PubMed] [Google Scholar]
- 7.Andeweg J. The anatomy of collateral venous flow from the brain and its value in aetiological interpretation of intracranial pathology. Neuroradiology 1996;38:621–628. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.