Abstract
Posttraumatic external carotid artery pseudoaneurysm with arteriovenous fistula is a rare condition. An 8-year-old child presented with painful pulsatile swelling in the preauricular region following a penetrating glass shrapnel injury. Detailed evaluation showed distal external carotid artery pseudoaneurysm with fistula, which was draining into the retromandibular vein. Endovascular treatment was performed. This case highlights the role of endovascular intervention for such rare complicated vascular pathologies.
Keywords: Arteriovenous fistula, endovascular treatment, pseudoaneurysm
Introduction
Extracranial carotid artery pseudoaneurysms are very rare and make less than 4% of total peripheral arterial pseudoaneurysms.[1] Among these, external carotid artery pseudoaneurysm is rare and the pseudoaneurysm with fistula is even rarer.
Etiology can be radiotherapy,[2] surgical iatrogenic injury,[3,4] and posttraumatic.[5] These cases pose different diagnostic and therapeutic challenges to the clinician. Color Doppler ultrasound and computed tomography (CT) angiography are the primary modalities used for diagnosis, and in most of the cases are sufficient for diagnosis. However, digital subtraction (DSA) angiography remain the gold standard to establish the diagnosis, evaluate the angioarchitecture, and planning of endovascular management.[6]
In our case, it was penetrating trauma to the artery as well as vein, which led to pseudoaneurysm formation from the external carotid artery, which was subsequently fistulizing with the retromandibular vein.
Case Report
An 8-year-old child presented to our hospital with painful swelling in the right preauricular region following a penetrating glass shrapnel injury. The glass shrapnel was removed and wound was stapled by local treating surgeon. There were two episodes of bleeding from the site, which was treated conservatively outside in a peripheral hospital. Then, he started developing ipsilateral facial nerve palsy and enlargement of the swelling, for which he was referred to our center. On local examination, he had tender pulsatile swelling in the right preauricular region. Patient also had grade 4 facial palsy [Figure 1A].
Figure 1 (A-D).
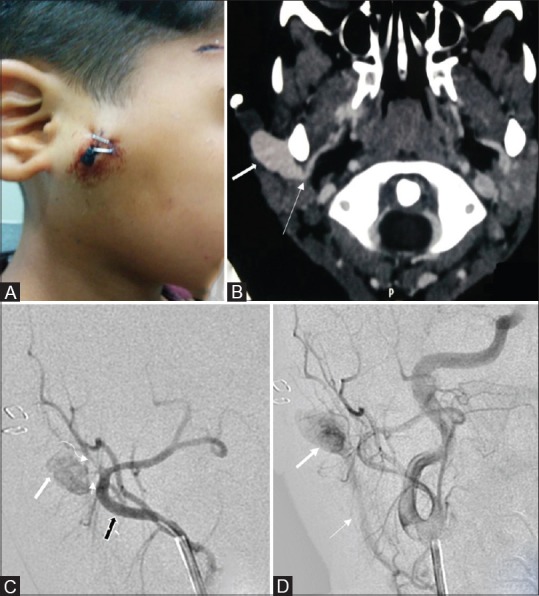
(A) Clinical picture shows right preauricular swelling with staples. (B) CT angiography of the neck vessels shows a narrow neck (thin arrow) pseudoaneurysm arising from the right distal ECA. Fundus of the pseudoaneurysm (thick arrow) is lying just deep to the skin. (C) Right ECA angiogram shows pseudoaneurysm (thick white arrow) from the distal ECA (thick black arrow) with rent (thin arrow) just at the origin of STA (curved arrow). (D) Delayed right common carotid angiogram shows the A-V fistula that is pseudoaneurysm (thick arrow) draining into the retromandibular vein (thin arrow)
Color Doppler ultrasound showed a narrow neck pseudoaneurysm from the distal external carotid artery. Typical ying-yang phenomenon was seen. CT angiography showed a pseudoaneurysm originating from distal external carotid artery. Rest of the carotid circulation was normal [Figure 1B].
Endovascular treatment was done under general anesthesia. Catheter angiography showed pseudoaneurysm from distal right external carotid artery close to the origin of superficial temporal artery (STA).
There was a very small rent at the origin of STA with slow opacification of pseudoaneurysm, which was slowly draining out into the retromandibular vein [Figure 1C and D]. CT angiography did not show early draining vein as delayed venous phase was not performed.
6F Guiding catheter was placed in the distal external carotid artery. Attempts were made to enter the rent with marathon microcatheter and mirage microwire, however, it was unsuccessful due to the extremely small size of the rent, which was located just at the origin of the superficial temporal artery.
The distal external carotid artery at the site of the rent was occluded with free platinum Hilal coils and subsequently dilute Glue (NBCA) was injected into the coil mesh. The rationale for using coils with glue was that coils act as a meshwork for Glue (a liquid embolic agent) in the region of interest, thus preventing non-target embolization. Final external carotid artery angiogram showed occlusion of distal external carotid artery with non-opacification of the pseudoaneurysm and good reformation of internal maxillary artery and STA through collaterals [Figure 2A and B].
Figure 2 (A-C).
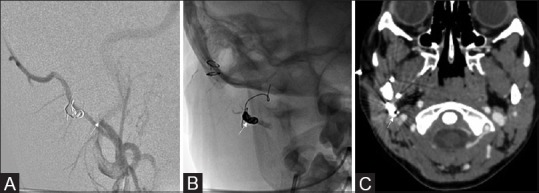
(A) Post right common carotid angiogram shows occlusion of distal external carotid artery (thin white arrow). (B) Plain skull radiograph in anteroposterior view shows the coil mass and glue (NBCA) cast (thin white arrow). (C) CT angiography of the neck vessels after 4 weeks shows complete thrombosis of the pseudoaneurysm and reduction of its size with coil mass in the distal external carotid artery (thin white arrow)
Post procedure the swelling was non-pulsatile. Follow up at two weeks showed reduction of the swelling. CT scan after 4 weeks showed thrombosis of pseudoaneurysm with reduction in its size [Figure 2C]. Staples were subsequently removed. At 3 months follow-up, there was complete resolution of the swelling with partial recovery from lower motor neuron facial palsy.
Discussion
Direct carotid artery injury with formation of pseudoaneurysm and arteriovenous fistula is not a common entity, and is usually associated with neurological symptoms and high morbidity due to risk of bleeding. Endovascular management is an effective therapy in the management of pseudoaneurysm as compared to surgery.[7]
Mortality rates are significantly are significantly high at more than 20% for surgery as compared with 1% in endovascular treatment for carotid artery injuries.
Exact localization of the lesion is mandatory before planning an endovascular treatment. Color Doppler ultrasound is the first investigation for vascular injuries. It may show the site of injury as well the status of proximal and distal arterial system. Color Doppler also has the added benefit of velocity measurement over CT angiography.[8] Cerebral CT angiography is rapid, non-invasive, and very accurate in the diagnosis of neurovascular injuries.[6] Maximum intensity projection and three-dimensional volume rendering provides very good spatial resolution.
Digital subtraction angiography (DSA) provides most accurate details of parent artery, site of origin of pseudoaneurysm any associated complication such as dissection or thrombosis, and associated findings such as arteriovenous fistula, as in our case.[9] DSA is important for the planning of endovascular treatment.
Available options include occlusion by glue, fibered platinum, or detachable coils or a combination of these materials.[6] Treatment options include parent vessel sacrifice in ECA pseudoaneurysm. The arteriovenous fistula needs to be disconnected by occlusion of the communicating channel with coils or dye. However, in difficult cases like this case where neck of the pseudoaneurysm is difficult to localize as the rent was very small and was located just at the origin of STA, occlusion of the parent artery can yield good success. The occlusion of pseudoaneurysm also cures the extremely slow flow fistula associated with pseudoaneurysm. Follow up imaging of the endovascular treatment can establish the durability of the results.
To our knowledge, concurrent pseudoaneurysm and arteriovenous fistula has not been described yet in maxillofacial region in the Indian literature.[10]
Conclusion
Posttraumatic external carotid artery pseudoaneurysm may cause catastrophic complications such as intractable bleeding and various neurological complications. External carotid artery pseudoaneurysm with fistula is a very rare entity and endovascular management is a safe and durable option of treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cogbill TH, Moore EE, Meissner M, Fischer RP, Hoyt DB, Morris JA, et al. The spectrum of blunt injury to the carotid artery: A multicenter perspective. J Trauma. 1994;37:473–9. doi: 10.1097/00005373-199409000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Chaloupka JC, Roth TC, Putman CM, Mitra S, Ross DA, Lowlicht RA, et al. Recurrent carotid blowout syndrome: Diagnostic and therapeutic challenges in a newly recognized subgroup of patients. Am J Neuroradiology. 1999;20:1069–77. [PMC free article] [PubMed] [Google Scholar]
- 3.Krempl GA, Noorily AD. Pseudoaneurysm of the descending palatine artery presenting as epistaxis. Otolaryngol Head Neck Surg. 1996;114:453–6. doi: 10.1016/S0194-59989670217-6. [DOI] [PubMed] [Google Scholar]
- 4.Karas DE, Sawin RS, Sie KC. Pseudoaneurysm of the external carotid artery after tonsillectomy. A rare complication. Arch Otolaryngol Head Neck Surg. 1997;123:345–7. doi: 10.1001/archotol.1997.01900030133017. [DOI] [PubMed] [Google Scholar]
- 5.Rhee CS, Jinn TH, Jung HW, Sung MW, Kim KH, Min YG. Traumatic pseudoaneurysm of the external carotid artery with parotid mass and delayed facial nerve palsy. Otolaryngol Head Neck Surg. 1999;121:158–60. doi: 10.1016/S0194-5998(99)70147-6. [DOI] [PubMed] [Google Scholar]
- 6.Zhao LB, Shi HB, Park S, Lee DG, Shim JH, Lee DH, et al. Acute bleeding in the head and neck: Angiographic findings and endovascular management. AJNR Am J Neuroradiol. 2014;35:360–6. doi: 10.3174/ajnr.A3761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuen JC, Gray DJ. Endovascular treatment of a pseudoaneurysm of a recipient external carotid artery following radiation and free tissue transfer. Ann Plast Surg. 2000;44:656–9. doi: 10.1097/00000637-200044060-00015. [DOI] [PubMed] [Google Scholar]
- 8.Mahmoud MZ, Al-Saadi M, Abuderman A, Alzimami KS, Alkhorayef M, Almagli B, et al. “To-and-fro” waveform in the diagnosis of arterial pseudoaneurysms. World J Radiol. 2015;7:89–99. doi: 10.4329/wjr.v7.i5.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang K, Li R, Lin J, Zheng X, Wang L, Yin W. The Value of Cerebral CT Angiography with Low Tube Voltage in Detection of Intracranial Aneurysms. Biomed Res Int. 2015:876796. doi: 10.1155/2015/876796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khera PS, Moses V, Ahmed M, Kakde S. Superior thyroid artery pseudoaneurysm and arteriovenous fistula following attempted internal jugular venous access and its management. Indian J Radiol Imaging. 2015;25:15–7. doi: 10.4103/0971-3026.150131. [DOI] [PMC free article] [PubMed] [Google Scholar]


