Abstract
Background
This study aims to (i) estimate the prevalence of blood-injection-injury phobia (BIIP) diagnosed as present at any time during the life prior to the interview, with or without another Specific Phobia diagnosed as present during the 12 months prior to the interview, (ii) characterize types and frequencies of co-occurring fears, (iii) evaluate the association with chronic medical conditions and lifetime psychiatric comorbidity, and (iv) explore medical service use associations in a nationally representative sample of older adults.
Methods
A sample of 8,205 older adults, aged 65 years or older, was derived from Wave 1 of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC).
Results
The weighted lifetime prevalence of BIIP with and without 12-month Specific Phobia was 0.6% (95% CI: 0.4–0.8) and 4.2% (95% CI: 3.7–4.8), respectively, and these two groups ranked similarly in terms of sociodemographic, health, and psychiatric characteristics. BIIP most frequently co-occurred with other lifetime fears, and was positively associated with hypertension and lifetime history of anxiety and personality disorders after controlling for sociodemographic and psychiatric confounders.
Conclusions
Our findings suggest that lifetime BIIP may bear mental and physical health significance in older adults.
Keywords: anxiety, phobia, epidemiology, geriatric, late life
Blood-injection-injury phobia in older adults
BIIP is a Specific Phobia sub-type characterized by fear and avoidance of seeing blood and receiving injections. The Baltimore Epidemiologic Catchment Area (ECA) study estimated a lifetime prevalence of 3.5%, most notably among younger women, and reported high comorbidity with other psychiatric conditions (Bienvenu and Eaton, 1998; Bracha et al., 2007). Despite age-related reductions in prevalence, anxiety disorders remain highly prevalent in older adults, and become increasingly associated with physical symptoms (Trollor et al., 2007; Miloyan and Pachana, 2015; Reynolds et al., 2015). BIIP may bear particular health significance in older age groups, due in part to high disability and low rates of health and mental health service use among older adults in general (Trollor et al., 2007; Lin et al., 2011; Brault, 2012). For example, the results of a previous study suggest that BIIP is associated with peripheral vascular and cardiovascular disease among diabetics, presumably due to differences in general health behaviors, or specifically insulin use by injection (Bienvenu and Eaton, 1998). However, these issues have not been addressed in older adults, for whom BIIP may bear important health implications due to the high prevalence of medical conditions that require routine compliance. The purpose of this study is to evaluate the prevalence, medical and lifetime psychiatric comorbidity, and medical service use associated with BIIP in a national sample of older adults.
Method
Sample
The NESARC was undertaken in 2001–2002 in a nationally representative sample of 43,093 civilian, non-institutionalized adults who were sampled from all 50 U.S. states and the District of Columbia (Grant et al., 2003a). African-Americans, Hispanics, and young adults were purposively oversampled, and sampling weights were used to adjust data for oversampling and non-response, and to allow population estimates to be standardized against census data. The overall response rate was 81% and face-to-face interviews were conducted by trained lay interviewers using the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV version (AUDADIS-IV). In the present study, all analyses were limited to participants aged 65 years or older (N = 8,205).
Measures
Lifetime fears and 12-month non-hierarchical Social Phobia (SP) diagnoses were obtained by trained interviewers using the AUDADIS-IV, which has good overall psychometric properties (Grant et al., 2003b). Specifically, the AUDADIS-IV has been found to have good reliability for assessing lifetime SP fears (ICC: 0.71), and fair-to-moderate reliability for SP diagnoses (κ 0.40 for 12-month and 0.48 for lifetime). Sociodemographic and health variables consisted of age, sex, education, personal income, marital status, self-perceived current health, and chronic medical conditions. The presence of chronic medical conditions was determined by asking respondents to report whether they had ever had a diagnosis of any of the following conditions: arteriosclerosis, hypertension, liver cirrhosis, liver disease, angina pectoris, tachycardia, myocardial infarction, heart disease, stomach ulcer, gastritis, and arthritis. Anxiety (panic disorder with or without agoraphobia, social phobia, and generalized anxiety disorder), mood (major depression, dysthymia, mania, and hypomania), substance use (alcohol abuse or dependence, drug abuse or dependence, and nicotine dependence), and personality (conduct, antisocial, avoidant, dependent, obsessive-compulsive, paranoid, schizoid, or histrionic) disorders were diagnosed with the AUDADIS, which asks detailed questions about symptoms related to each of the psychiatric disorders. Past-year medical service use was examined using reports of the following: (a) number of days stayed in hospital, (b) number of times treated in emergency room, and (c) number of injuries that caused one to seek medical help or cut down usual activities for more than half a day.
Statistical analyses
Prevalence estimates for BIIP were calculated with survey weights to allow for comparison to census data and estimates for the entire nation. Those endorsing lifetime BIIP with and without a 12-month SP diagnosis were compared using a binary logistic regression analysis. Odds ratios predicting lifetime psychiatric conditions, chronic medical conditions, and service use from BIIP were calculated with logistic regression, with and without adjustment based on sociodemographic characteristics and psychiatric diagnoses. Due to the large number of comparisons, we opted to use a p-value threshold of 0.01 in lieu of the standard 0.05. All statistical analyses were performed using Stata 12 (StataCorp, 2011).
Results
Sociodemographic characteristics of the sample
The total sample consisted of 8,205 older adults aged 65 years or older (Mage = 75±7; 62% female). Approximately 33% of participants completed high school, with 35 % completing at least some college. Eighty-five percent reported a personal income of less than $35,000 per year, with 34% reporting an annual income of less than $10,000. Forty-three percent of participants reported being married or cohabiting, 52% reported being widowed, divorced or separated, and 5% reported being widowed. Eighty-two percent of participants were White, 8% were Black, 2% were Native American, 3% were Asian, and 5% were Hispanic. Sixty-five percent of participants reported their self-perceived current health to be good, very good, or excellent, and 56% reported having a maximum of one chronic medical condition. Approximately half of all the older adults in the sample reported having at least one lifetime fear.
Prevalence of lifetime BIIP with and without 12-month SP
A total of 386 participants reported having a lifetime BIIP, corresponding to a weighted population prevalence of 4.2% (95% CI: 3.7–4.8). Among those with lifetime BIIP, a total of 51 participants met 12-month DSM-IV diagnostic criteria for SP, corresponding to a weighted population prevalence of 0.6% (95% CI: 0.4–0.8). Respondents’ age was not significantly related to the prevalence of BIIP (Table 1).
Table 1.
Weighted lifetime BIIP prevalence estimates among older age groups
| 65–74 N = 4,186 | 75–84 N = 2,878 | 85+ N = 879 | TOTAL N = 7,943 | |
|---|---|---|---|---|
| Lifetime BIIP with or without 12-month SP | 4.2 (3.4–5.0) | 4.6 (3.7–5.5) | 3.3 (2.0–4.5) | 4.2 (3.7–4.8) |
| Lifetime BIIP with 12-month SP | 0.6 (0.3–0.9) | 0.5 (0.3–0.7) | 0.5 (0.04–1.04) | 0.6 (0.4–0.8) |
Note: The results of binary logistic regression analyses indicated that there were no significant age-related differences in BIIP prevalence among older adults.
A binary logistic regression analysis was conducted in order to compare those who did or did not meet 12-month SP criteria (coded 1 and 0 respectively) along with their lifetime BIIP in terms of sociodemographic, health, and psychiatric characteristics. None of the variables in this model significantly differentiated the two groups at the 0.01 threshold, so subsequent analyses no longer distinguish the two groups.
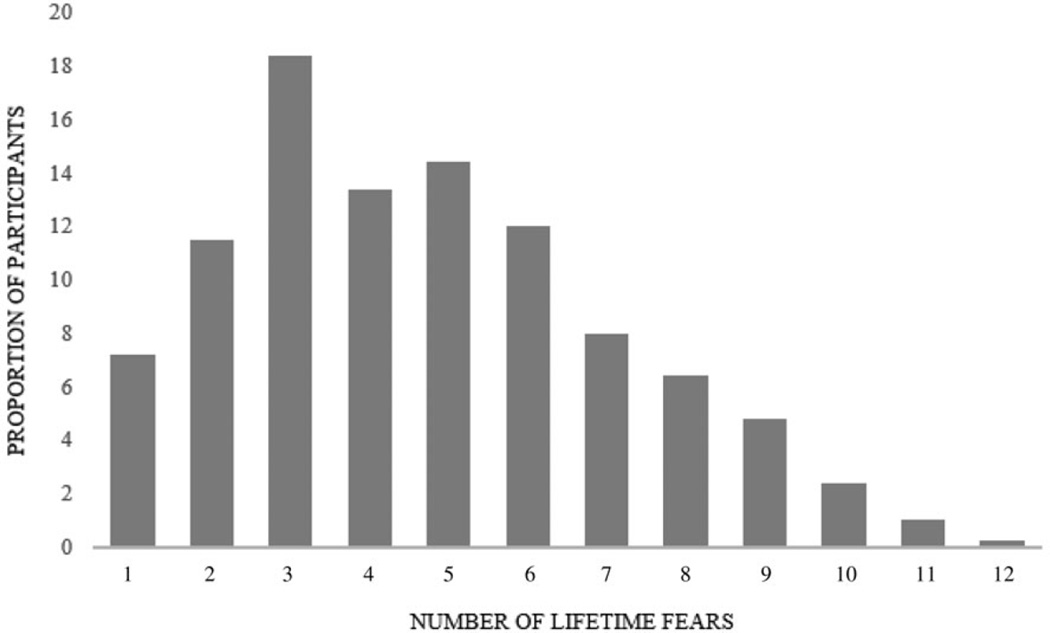
Type and frequency of co-occurring lifetime fears
BIIP occurred together with other lifetime fears in over 90% of all cases (Figure 1). The two most common co-occurring lifetime fears were of animals and heights, each endorsed by approximately half of the individuals with BIIP. It is surprising that only approximately one-third of those with BIIP reported a lifetime fear of dentists and one-fifth reported a lifetime fear of hospitals.
Figure 1.
Frequency of lifetime fears among older adults with blood-injection-injury-phobia.
Psychiatric comorbidity
Lifetime BIIP was significantly associated with lifetime anxiety, mood, and personality disorders in the unadjusted model. These associations persisted after adjusting for sociodemographic characteristics. After adjusting for other psychiatric disorders, however, only the associations with lifetime SP, any lifetime anxiety disorder, and personality disorders remained significant (Table 2).
Table 2.
Prediction of lifetime psychiatric disorders from lifetime BIIP
| UNADJUSTED | SOCIODEMOGRAPHICa | SOCIODEMOGRAPHIC AND PSYCHIATRICb |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Anxiety disorders | ||||||
| Panic disorder | 1.96 | 1.15–3.31 | 1.83 | 1.08–3.10 | 1.15 | 0.63–2.11 |
| Social phobia | 3.99 | 2.49–6.43** | 3.90 | 2.45–6.19** | 2.88 | 1.71–4.85** |
| Generalized anxiety disorder | 2.42 | 1.43–4.08* | 2.14 | 1.26–3.63* | 1.39 | 0.81–2.39 |
| Any anxiety disorder | 2.55 | 1.83–3.56** | 2.42 | 1.73–3.38** | 1.84 | 1.25–2.73* |
| Mood disorders | ||||||
| Major depression | 1.85 | 1.33–2.57** | 1.69 | 1.21–2.35* | 1.16 | 0.78–1.72 |
| Dysthymia | 2.18 | 1.25–3.80* | 1.96 | 1.11–3.44 | 1.31 | 0.70–2.47 |
| Mania or hypomania | 2.76 | 1.54–4.92* | 2.56 | 1.39–4.71* | 1.53 | 0.77–3.05 |
| Any mood disorder | 1.89 | 1.58–2.61** | 1.73 | 1.28–2.34* | 1.25 | 0.85–1.82 |
| Substance use disorders | ||||||
| Alcohol abuse/dependence | 0.93 | 0.65–1.34 | 1.25 | 0.85–1.85 | 1.05 | 0.71–1.57 |
| Any drug abuse/dependence | 2.43 | 0.84–7.09 | 2.19 | 0.76–6.33 | 1.40 | 0.42–4.61 |
| Any substance use disorder | 0.94 | 0.66–1.35 | 1.26 | 0.86–1.86 | 1.04 | 0.71–1.56 |
| Nicotine dependence | 1.67 | 1.15–2.43* | 1.74 | 1.19–2.54* | 1.42 | 0.94–2.15 |
| Personality disorders | ||||||
| Any personality disorder | 2.64 | 1.86–3.73** | 2.76 | 1.96–3.86** | 2.25 | 1.57–3.21** |
p < 0.01,
p < 0.001.
Odds ratios adjusted for age, sex, education, income, marital status, geographic region, and urbanicity.
Odds ratios adjusted for age, sex, education, income, marital status, geographic region, ubranicity, and other psychiatric disorders.
Medical comorbidity
Lifetime BIIP was significantly associated with hypertension, tachycardia, stomach ulcer, and gastritis in the unadjusted model and after adjusting for sociodemographic variables. After additionally adjusting for psychiatric diagnoses, only the association with hypertension remained significant (See Table 3). With regard to service use, lifetime BIIP was significantly associated with number of injuries during the past year that required the respondent to cut down physical activity for at least half a day in the unadjusted model and after adjusting for sociodemographic characteristics, but not after additionally adjusting for lifetime psychiatric diagnoses (Table 4).
Table 3.
Prediction of chronic medical conditions from lifetime BIIP
| UNADJUSTED | SOCIODEMOGRAPHICa | SOCIODEMOGRAPHIC AND PSYCHIATRICb |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Arteriosclerosis | 0.96 | 0.57–1.61 | 1.06 | 0.63–1.78 | 0.93 | 0.55–1.58 |
| Hypertension | 1.61 | 1.26–2.06** | 1.52 | 1.18–1.94* | 1.46 | 1.14–1.87* |
| Liver cirrhosis | 1.03 | 0.13–8.24 | 1.06 | 0.13–8.57 | 1.06 | 0.15–7.69 |
| Liver disease | 1.10 | 0.24–5.08 | 1.06 | 0.23–4.84 | 1.09 | 0.23–5.18 |
| Chest pain | 1.39 | 0.97–2.00 | 1.35 | 0.94–1.95 | 1.18 | 0.81–1.71 |
| Tachycardia | 1.77 | 1.24–2.53* | 1.65 | 1.15–2.37* | 1.45 | 1.01–2.09 |
| Myocardial infarction |
1.33 | 0.77–2.68 | 1.41 | 0.70–2.84 | 1.29 | 0.64–2.60 |
| Heart disease | 1.02 | 0.64–1.61 | 1.06 | 0.67–1.70 | 0.95 | 0.60–1.50 |
| Stomach ulcer | 2.37 | 1.46–3.86* | 2.08 | 1.28–3.37* | 1.83 | 1.10–3.04 |
| Gastritis | 1.92 | 1.30–2.86* | 1.81 | 1.22–2.69* | 1.56 | 1.03–2.35 |
| Arthritis | 1.12 | 0.87–1.44 | 1.01 | 0.78–1.30 | 0.91 | 0.69–1.20 |
p < 0.01,
p < 0.001, PY: past year.
Odds ratios adjusted for age, sex, education, income, marital status, geographic region, urbanicity.
Odds ratios adjusted for age, sex, education, income, marital status, geographic region, urbanicity, and other psychiatric disorders.
Table 4.
Prediction of medical service use from lifetime BIIP
| UNADJUSTED | SOCIODEMOGRAPHICa | SOCIODEMOGRAPHIC AND PSYCHIATRICb |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Number of days in hospital in PY |
1.00 | 0.71–1.40 | 1.02 | 0.72–1.45 | 0.97 | 0.68–1.38 |
| Number of times treated in emergency room in PY |
1.15 | 0.86–1.53 | 1.15 | 0.86–1.53 | 1.07 | 0.81–1.44 |
| Number of injuries requiring medical help or to cut down physical activity in PY |
1.55 | 1.13–2.13* | 1.56 | 1.14–2.15* | 1.49 | 1.08–2.06 |
p < 0.01,
p < 0.001, PY: past year.
Odds ratios adjusted for age, sex, education, income, marital status, geographic region, urbanicity.
Odds ratios adjusted for age, sex, education, income, marital status, geographic region, urbanicity, and psychiatric comorbidity.
Discussion
In a national sample of older American adults, the weighted lifetime prevalence of BIIP was 4.2%. The Baltimore ECA study estimated a similar lifetime prevalence of 3.5% (Bienvenu and Eaton, 1998); however, a Swedish population register study estimated a much higher lifetime prevalence of 7.9% among older adults (Sigström et al., 2011). Although reasons for this discrepancy are unclear, the actual lifetime prevalence of BIIP may in fact be significantly higher than the estimate reported in the present study, due to recall errors that lead respondents to underestimate the occurrence of psychiatric symptoms earlier in their lives (Moffitt et al., 2010; Takayanagi et al., 2014).
In the present study, those who endorsed a lifetime BIIP with or without a 12-month SP diagnosis were not differentiated by sociodemographic, health, and psychiatric characteristics. This finding is consistent with those of previous studies, which report only marginal differences between older adults with a 12-month diagnosis of SP, a lifetime diagnosis of SP, or sub-threshold SP, relative to asymptomatic controls (Chou, 2009; Grenier et al., 2011).
Lifetime BIIP was significantly associated with hypertension among older adults in our sample after controlling for sociodemographic and psychiatric confounders. We are unable to draw causal inferences about this observed association due to the use of cross-sectional data. However, the higher odds of chronic medical conditions may be due to differences in preventive lifestyle or treatment-seeking behaviors earlier in life (Thyer et al., 1985; Marks, 1988). Although findings from the Baltimore ECA suggest that there may be no major health ramifications of having lifetime BIIP in terms of health-seeking behaviors (Bienvenu and Eaton, 1998), diabetics with BIIP were more likely to report having vascular disease.
Lifetime BIIP was associated with a range of anxiety, mood, and personality disorders in our unadjusted model, and after adjusting for sociodemographic characteristics. After similar adjustments, Bienvenu and Eaton also found high lifetime comorbidity, particularly for mood and anxiety disorders, among those with a lifetime BIIP. After additionally adjusting for comorbid psychiatric conditions, we found that BIIP was significantly and most strongly associated with a lifetime diagnosis of SP and personality disorders. Similarly, Grenier and colleagues reported that older adults with a 12-month diagnosis of SP were more likely to have comorbid anxiety disorders than their sub-threshold counterparts.
Approximately 8% of those with lifetime BIIP did not report any other lifetime fears, suggesting that BIIP usually occurs in tandem with other fears. The two most commonly co-occurring lifetime fears were of animals and heights, consistent with previous findings suggesting that these are the most common fears in general (Magee et al., 1996). Additionally, we found that dental phobia was not among the most frequently co-occurring lifetime fears, consistent with previous findings suggesting that BIIP and dental phobia represent two distinct SP sub-types (De Jongh et al., 1998; van Houtem et al., 2014). Interestingly, fear of hospitals was also among the least frequently co-occurring fears.
A strength of the present study is that it was based on a large, nationally representative sample of the U.S. population. However, there are also some important limitations. First, as previously alluded to, the estimated prevalence of lifetime BIIP may have underestimated the true lifetime prevalence in our sample, due to recall errors that are known to impact the accuracy of lifetime prevalence estimates (Moffitt et al., 2010; Takayanagi et al., 2014). It is possible that those who remember having had a lifetime BIIP (those in our sample) vary in important respects to those who forget or deny earlier fears, for instance in terms of recency or severity, and other characteristics. Additionally, cohort effects may explain observed differences in the prevalence of BIIP between older adult samples (Sigström et al., 2011). Second, in the structured interview, participants were only required to answer ‘yes’ or ‘no’ to whether they had any lifetime fears. Therefore, we were unable to examine whether the intensity of the fear of blood, injection, or injury has an impact on medical and psychiatric comorbidity. Finally, we were unable to investigate in greater detail whether BIIP has a general effect on health behaviors and treatment seeking due to the limited number of questions about medical service use in the AUDADIS. Longitudinal datasets with more detailed measures of health behaviors and service use are needed to further examine this issue.
Acknowledgments
This work was supported by the Johns Hopkins Epidemiology and Biostatistics of Aging Training Program of the National Institute on Aging (NIA) under award number T32AG000247, and NIDA grant 026652 to Dr Eaton.
Footnotes
Conflict of interest
None.
Description of authors’ roles
BM and WE conceived and planned the study. BM performed statistical analyses and wrote the manuscript. WE edited the manuscript for important content.
References
- Bienvenu OJ, Eaton WW. The epidemiology of blood-injection-injury phobia. Psychological Medicine. 1998;28:1129–1136. doi: 10.1017/s0033291798007144. [DOI] [PubMed] [Google Scholar]
- Bracha HS, Bienvenu OJ, Eaton WW. Testing the Paleolithic-human-warfare hypothesis of blood-injection phobia in the Baltimore ECA follow-up study: towards a more etiologically-based conceptualization for DSM-V. Journal of Affective Disorders. 2007;97:1–4. doi: 10.1016/j.jad.2006.06.014. [DOI] [PubMed] [Google Scholar]
- Brault MW. Current Population Reports. Washington, DC: US Census Bureau; 2012. Americans with Disabilities: 2010. Household Economic Studies. [Google Scholar]
- Chou K-L. Specific phobia in older adults: evidence from the national epidemiological survey on alcohol and related conditions. American Journal of Geriatric Psychiatry. 2009;17:376–386. doi: 10.1097/JGP.0b013e3181943214. [DOI] [PubMed] [Google Scholar]
- De Jongh A, Bongaarts G, Vermeule I, Visser K, De Vos P, Makkes P. Blood-injury-injection phobia and dental phobia. Behaviour Research and Therapy. 1998;36:971–982. doi: 10.1016/s0005-7967(98)00064-3. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression, and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003b;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003a. [Google Scholar]
- Grenier S, et al. The epidemiology of specific phobia and subthreshold fear subtypes in a community-based sample of older adults. Depression and Anxiety. 2011;28:456–463. doi: 10.1002/da.20812. [DOI] [PubMed] [Google Scholar]
- Lin WC, Zhang J, Leung GY, Clark RE. Chronic physical conditions in older adults with mental illness and/or substance use disorders. Journal of the American Geriatrics Society. 2011;59:1913–1921. doi: 10.1111/j.1532-5415.2011.03588.x. [DOI] [PubMed] [Google Scholar]
- Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the national comorbidity survey. Archives of General Psychiatry. 1996;53:159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- Marks I. Blood-injury phobia: a review. American Journal of Psychiatry. 1988;145:1207–1213. doi: 10.1176/ajp.145.10.1207. [DOI] [PubMed] [Google Scholar]
- Miloyan B, Pachana NA. Clinical significance of worry and physical symptoms in late-life generalized anxiety disorder. International Journal of Geriatric Psychiatry. 2015;30:1186–1194. doi: 10.1002/gps.4273. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds K, Pietrzak RH, El-Gabalawy R, Mackenzie CS, Sareen J. Prevalence of psychiatric disorders in U.S. older adults: findings from a nationally representative survey. World Psychiatry. 2015;14:74–81. doi: 10.1002/wps.20193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigström R, Östling S, Karlsson B, Waern M, Gustafson D, Skoog I. A population-based study on phobic fears and DSM-IV specific phobia in 70-year olds. Journal of Anxiety Disorders. 2011;25:148–153. doi: 10.1016/j.janxdis.2010.08.014. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release. Vol. 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of reports of lifetime mental and physical disorders: results from the baltimore epidemiological catchment area study. JAMA Psychiatry. 2014;71:273–280. doi: 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thyer BA, Himle J, Curtis GC. Blood-injury-illness phobia: a review. Journal of Clinical Psychology. 1985;41:451–459. doi: 10.1002/1097-4679(198507)41:4<451::aid-jclp2270410402>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Trollor JN, Anderson TM, Sachdev PS, Brodaty H, Andrews G. Prevalence of mental disorders in the elderly: the Australian national mental health and well-being survey. American Journal of Geriatric Psychiatry. 2007;15:455–466. doi: 10.1097/JGP.0b013e3180590ba9. [DOI] [PubMed] [Google Scholar]
- van Houtem CM, Aartman IH, Boomsma DI, Ligthart L, Visscher CM, de Jongh A. Is dental phobia a blood-injection-injury phobia? Depression and Anxiety. 2014;31:1026–1034. doi: 10.1002/da.22168. [DOI] [PubMed] [Google Scholar]