Abstract
Background
Borderline personality disorder (BPD) is characterized by greater engagement in non-suicidal self-injury (NSSI) and suicidality. The aim of the study is to test whether the occurrence of child abuse contributes to these high-risk behaviors in BPD youth.
Materials and methods
BPD female youth aged 13–21 years with (n = 29) and without (n = 29) a history of child abuse were administered clinical interviews assessing diagnostic history, child abuse, NSSI and suicidality (i.e., ideation, plans, and attempts). NSSI and suicidality were subsequently reevaluated at the 1- and 2-month follow-up assessments.
Results
Several findings emerged. First, relative to BPD youth without abuse, the abuse group reported greater past NSSI; however, no significant differences emerged in the follow-up period. Second, the occurrence of child abuse was associated with a 5-fold increase in the rate of lifetime suicide attempts relative to the no abuse group and additionally, prospectively predicted suicide ideation (but not attempts). Last, exploratory analyses indicated that the co-occurrence of physical and sexual abuse was associated with greater past NSSI and suicidality as compared to the no abuse and sexual abuse only participants.
Conclusion
As a whole, child abuse – particularly co-occurring physical and sexual abuse – increases risk for NSSI and suicidality among BPD youth, which may have important treatment implications in this high-risk population.
1. Introduction
Borderline personality disorder (BPD) is a common and debilitating psychiatric disorder. Prevalence rates range between 0.5% and 6% in adult community samples [1] and are as high as 20% among adult inpatients [2]. In youth, prevalence rates are less clear, however, recent epidemiological data show that 1–3% of community samples present with BPD [3–5], while approximately 11–27% of outpatients [6,7] and 43–49% of psychiatric inpatients [8] report BPD during adolescence and young adulthood. BPD in youth is characterized by greater non-suicidal self-injury (NSSI) and suicidal behaviors [9,10], and thus, research is warranted to identify factors that potentiate these high-risk behaviors in BPD youth.
The relationship between early childhood trauma and BPD during adulthood has been extensively studied. Early childhood maltreatment (i.e., abuse and/or neglect) is a significant risk factor for the development of BPD [11–14] cf. [15], and further, prospective longitudinal studies in adults consistently suggest a dose–response relationship between adverse childhood events and BPD. Specifically, more extensive early maltreatment (both type and severity) is associated with greater severity of BPD symptoms and increased impairment in adult psychosocial functioning [16–18]. Collectively, these data suggest that for some, childhood trauma is a core etiological risk factor in the development of BPD.
Recurrent suicidal and self-injurious behaviors also are distinguishing characteristics of BPD, contributing to the highest mortality rates and most costly demand on mental health services [19,20]. In cross-sectional and longitudinal studies with adult BPD populations, childhood abuse increases the risk of suicidal behaviors and the lifetime number of suicide attempts [21,22]. Similarly, in a 16-year prospective follow-up study, both childhood neglect and sexual abuse predict future suicidal behavior [16]. NSSI, the intentional destruction of one’s bodily tissue without the intent to die [9], is highly prevalent (up to 80%) in adult BPD populations [23], and childhood traumatic experiences independently and prospectively predict NSSI [24,25]. Unsurprisingly, comorbid BPD and PTSD also have a robust effect on the presence and frequency of NSSI in BPD adults [26].
Compared to research with adult populations, relatively few investigations have examined the prospective impact of child abuse in youth with BPD, particularly as this relates to self-injurious and suicidal behaviors. Similar to adults, early life adversity appears to play a central role in BPD development and severity in youth. For example, Westen and colleagues [27] found that female adolescents diagnosed with BPD (14–17 years old) report higher rates of abuse by multiple perpetrators and are more likely to experience multiple types of abuse (i.e., both sexual and physical) during childhood as compared to same-age peers with psychiatric difficulties other than BPD. Further, both relational and overt peer victimizations prospectively predict BPD symptoms during adolescence [28]. While it is evident that BPD youth report higher rates of NSSI and suicidal behaviors [9,10,29], it remains unclear whether the experience of early abuse differentially impacts these high-risk behaviors.
To address critical empirical gap in our understanding of BPD youth, the present study tested the prospective impact of childhood abuse (i.e., physical and sexual). In line with past research in adults [24,30,31], we hypothesized that BPD youth with a history of childhood abuse will report more frequent and severe NSSI and suicidality (ideation, planning, attempts) both at baseline and across the follow-up assessments relative to BPD youth without any abuse history. Exploratory analyses also will test the impact of co-occurring abuse – the presence of physical and sexual abuse – on NSSI and suicidality.
2. Materials and methods
2.1. Procedure
The Partners Institutional Review Board approved study procedures. Participants aged 13–17 years provided written assent. Legal guardians and participants aged 18 and older gave written consent. On the first study visit, participants were administered clinical interviews assessing Axis I and II disorders, self-injurious thoughts and behaviors, and trauma. Additionally, participants completed questionnaires assessing psychiatric symptom severity. Participants’ symptoms, NSSI, and suicidality were re-evaluated at the 1- and 2-month follow-up assessments.
2.2. Participants
The sample included 58 female participants aged 13 to 21 years (M = 17.02, SD = 1.91) recruited from an intensive dialectical behavior therapy (DBT) treatment program. All participants met diagnostic criteria for BPD, confirmed with the Structured Clinical Interview for DSM-IV Axis II personality disorders, BPD module (SCID-II) [32]. The participants were predominantly Caucasian (n = 46, 79.3%), and the majority reported family income over $100,000 per year (n = 49, 84.5%). Within the sample, medication use was common: nearly all participants were being treated with at least one psychotropic medication (n = 57, 98.3%). Participants reported using the following categories of medication: 75.4% (n = 43) antidepressants (e.g., selective serotonin reuptake inhibitors), 50.9% (n = 29) atypical antipsychotics (e.g., risperidone), 31.6% (n = 18) mood stabilizers (e.g., lamictal), 14.0% (n = 8) benzodiazepines (e.g., klonopin), 10.5% (n = 6) stimulants (e.g., concerta), and 7.0% (n = 4) naltrexone.
Twenty-nine participants (50.0%) endorsed past physical or sexual abuse, measured by the Childhood Trauma Questionnaire (CTQ) [33], and the remainder (n = 29, 50.0%) reported no history of physical or sexual abuse. The abuse and no abuse groups did not significantly differ in age (t(56) = .21, p = .84, d = .05), race (χ2(3, n = 58) = 2.37, p = .50, φ = .20), family income (χ2(3, n = 54) = 2.28, p = .52, φ = .21), or in their use of any medication type (χ2s < 3.25, ps > .07, φs < .24).
At the 1-month follow-up assessment, 5 (8.6%) participants did not provide data, resulting in 26 participants within the abuse group and 27 youth within the no abuse group. Eighteen participants (31.0%) did not complete the 2-month assessment, leaving 20 participants within each group. Participants lost to the first follow-up differed from the retained sample on race (χ2(3, n = 58) = 11.64, p = .009, φ = .45), but no other significant differences on demographic characteristics emerged (all ps > .13, all φs < .47). For the 2-month follow-up assessment, there were no differences in demographic characteristics between the original sample and attrited sample (all ps > .25, all φs < .31).
2.3. Measures
2.3.1. Clinical interviews
Trained bachelor-level research assistants, graduate students, and postdoctoral fellows administered the clinical interviews. All interviewers received approximately 50 h of training (e.g., didactics and mock interviews) and regular clinical recalibration meetings ensured the reliability of diagnoses across interviewers. The Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) [34] is a brief, structured interview that assesses Axis I disorders. The MINI-KID has shown good reliability and validity in community [34] and psychiatric [35] adolescent samples. The Structured Clinical Interview for DSM-IV Axis II personality disorders, BPD module (SCID-II) [32] assessed BPD symptomatology, and each participant’s primary psychiatrist or psychotherapist confirmed the BPD diagnosis. Only BPD participants who received a confirmatory diagnosis from the primary psychiatrist were included in the analyses.
The Self-Injurious Thoughts and Behaviors Interview (SITBI) [36] is a structured clinical interview that quantifies the presence, frequency, and severity of NSSI as well as suicidal thoughts and behaviors. It has adequate concurrent validity (i.e., medium-to-large correlations with other measures of suicidality) among adolescent inpatients [37]. Analyses at baseline focused on NSSI (i.e., frequency), suicidal ideation (i.e., number of days), suicide plans (i.e., number of days), and suicide attempts (i.e., frequency) over the past month and the past year. Additionally, lifetime suicide attempts, but not lifetime NSSI, suicidal ideation, or suicide plans, were assessed due to reliability issues reporting these events over a relatively large time span. Follow-up assessments were completed 1 and 2 months after baseline and probed past-month NSSI, ideation and plans.1
2.3.2. Childhood maltreatment
The Childhood Trauma Questionnaire Short Form (CTQ) [33] is a 25-item questionnaire that assesses the respondent’s experiences of childhood trauma. The current study focused on the 5-item subscales of physical and sexual abuse. Item scores ranged from 1 (never true) to 5 (very often true). Participants’ scores were then dichotomized using established criteria [38] to indicate the presence versus absence of physical (≥8) and sexual (≥6) abuse. Internal consistency was excellent for the physical abuse (α = .90) and sexual abuse (α = .95) subscales within the abuse group. As there was minimal variance in the no abuse group, internal consistency for these trauma measures was not calculated.
The Childhood Trauma Interview (CTI) [39], a semi-structured interview that measures abuse and neglect from birth through age 18, was administered. Each area of adversity (separation, physical neglect, emotional abuse, physical abuse, witnessing violence, and sexual abuse) is rated in terms of its severity and frequency. Severity was rated on a scale of 1 (minimal or mild) to 6 (torture or sadism), and frequency was rated on a scale of 1 (less than once per year) to 6 (every day or sometimes more than once a day). Sexual abuse was defined as an event with a severity of 1 or higher, which at a minimum includes “non-contact experiences,” such as “being looked at or spoken to in a clearly sexualized manner.” Physical abuse was defined as an event with a severity of 3 or higher, which includes at least two of the following: being hit with an object, being hit on bare skin, or marks left on the skin. We computed the presence of either physical or sexual abuse based on the CTI and compared CTQ classifications (i.e., “any abuse” = presence of either physical or sexual abuse; “no abuse” = no lifetime physical or sexual abuse). The percentage of agreement between the two measures was 81.0%; disagreements may have been due to the CTI’s inclusion of more mild instances of sexual and physical abuse compared to the CTQ. Nonetheless, the CTQ and CTI showed substantial agreement [40], κ = .62, SE = 0.10, CI95 [0.42–0.82]. The CTI only was used to confirm the reliability and validity of participants’ self-reported abuse experiences whereas the CTQ was used to classify participants in “abuse” and “no abuse” groups.
2.3.3. Symptom severity
The Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD) [41] is a 9-item self-report instrument assessing BPD symptoms. Items are rated from 0 to 4, and greater total scores indicate greater BPD severity. In the current study, the ZAN-BPD reported good internal consistency in the abuse group (α = .81) and acceptable internal consistency in the no abuse group (α = .79). The Scale for Suicidal Ideation (SSI) [42] is a 21-item questionnaire that assesses current suicidal ideation. Items on the SSI range from 0 to 2, with higher scores indicating higher levels of suicidality. In the current study, there was excellent internal consistency in both groups (abuse: α = .95; no abuse: α = .94).
2.4. Data analysis
All analyses were completed using IBM SPSS Statistics version 22.0. Baseline differences between the abuse and no abuse group were compared using: (a) t-tests for symptoms and age and (b) chi-square analyses for other demographic variables and Axis I diagnoses. Poisson regressions tested whether membership in the abuse group versus the no abuse group was associated with NSSI, suicide ideation, plans, and attempts. For the Poisson regressions, robust standard errors were used for the parameter estimates to control for over-dispersion (i.e., variance > mean), consistent with current recommendations [43]. Poisson regressions tested whether being in the abuse group, versus the no abuse group, could uniquely predict NSSI, suicidal ideation, and suicide plans at the 1- and 2-month follow-up assessments, controlling for baseline NSSI and suicidality, respectively. Given the number of statistical tests conducted in our primary analyses, we adjusted the critical alpha to p < .01. For each set of results, we performed two sensitivity analyses: first, we re-ran all models controlling for the number of BPD symptoms that participants endorsed on the SCID-II, and second, we re-ran the models controlling for participants’ self-reported severity of BPD symptoms, indexed by their scores on the ZAN-BPD.
As 10 participants reported both physical and sexual abuse, exploratory analyses using Poisson regression tested whether the presence of both types of abuse – compared to only sexual abuse and no abuse – was differentially associated with NSSI and suicidal behaviors at baseline and at the 1- and 2-month follow-ups. Given the exploratory nature of these analyses as well as the smaller sample size, a critical alpha of p < .05 was utilized.
3. Results
3.1. Attrition
Participants lost to the first follow-up did not significantly differ from the original sample on diagnostic characteristics or symptom severity (all ps > .27, all φs < .15, all ds < .20). Those lost to the second follow-up also did not significantly differ from the original sample in terms of these characteristics (all ps > .10, all φs < .22, all ds < .38). Relative to the retained sample, participants lost to attrition at the 1-month assessment made more suicide plans in the past month, χ2(10, n = 58) = 19.33, p = .036, φ = .58, and past year, χ2(20, n = 51) = 34.79, p = .021, φ = .83. No other differences in NSSI or suicidal behaviors emerged when comparing participants lost to follow-up with the retained sample (1-month: all ps > .10, all φs < .80; 2-month: all ps > .06, all φs < .74).
3.2. Preliminary analyses
Demographic information, psychiatric comorbidity, NSSI, and suicidality (i.e., ideation, plans, and attempts), stratified by group, are summarized in Table 1. Participants who reported sexual or physical abuse had significantly higher rates of PTSD than the no abuse group; however, the groups did not significantly differ on other Axis I diagnoses. Compared to the no abuse group, the abuse group reported greater BPD symptom severity.
Table 1.
Baseline demographic and clinical data among BPD youth reporting abuse and no abuse.
| Abuse | No abuse | Statistic | p | Effect size | CI95 | |
|---|---|---|---|---|---|---|
|
|
|
|||||
| (n = 29) | (n = 29) | |||||
| Age | 17.07 (1.87) | 16.97 (1.97) | t(56) = −0.21 | .84 | d = 0.05 | |
| BPD symptoms | 18.22 (7.85) | 12.93 (7.06) | t(56) = 2.70 | .009 | d = 0.71 | 0.17–1.24 |
| Suicidal ideation severity | 16.05 (11.13) | 11.08 (10.28) | t(56) = 1.77 | .08 | d = 0.46 | −0.06 to 0.98 |
| Sexual abuse severity | 14.10 (6.75) | 5.00 (0.00) | t(28.38) = 7.26 | <.001 | d = 1.91 | |
| Sexual abuse frequency | 2.59 (2.64) | 0.17 (0.60) | t (30.90) = 4.80 | <.001 | d = 1.26 | |
| Physical abuse severity | 8.65 (5.38) | 5.14 (0.44) | t(28.00) = 3.50 | .001 | d = 0.92 | |
| Physical abuse frequency | 4.83 (6.02) | 2.48 (3.44) | t(44.53) = 1.82 | .08 | d = 0.48 | |
| Psychotropic medications, n (%) | 28 (96.6) | 29 (100) | χ2(1) = 1.02 | .31 | φ = −0.13 | |
| Current comorbidities, n (%) | ||||||
| MDD/dysthymia | 20 (69.0) | 23 (79.3) | χ2(1) = 0.81 | .37 | φ = −0.12 | |
| Substance disorder | 13 (44.8) | 12 (41.4) | χ2(1) = 0.07 | .79 | φ = 0.04 | |
| Posttraumatic stress disorder | 13 (44.8) | 1 (3.4) | χ2(1) = 13.56 | <.001 | φ = 0.48 | |
| Other anxiety disorders | 18 (62.1) | 20 (69.0) | χ2(1) = 0.31 | .58 | φ = −0.07 | |
| Behavioral disorder | 10 (34.5) | 10 (34.5) | χ2(1) = 0.00 | 1.00 | φ = 0.00 | |
| Bipolar disorder (I, II, NOS) | 8 (27.6) | 5 (17.2) | χ2(1) = 0.89 | .35 | φ = 0.12 | |
| Bulimia nervosa | 3 (10.3) | 0 (0.0) | χ2(1) = 3.16 | .08 | φ = 0.23 | |
| Psychotic disorder | 1 (3.4) | 0 (0.0) | χ2(1) = 1.02 | .31 | φ = 0.13 | |
| NSSI and suicidality | ||||||
| NSSI, past month | 9.10 (11.99) | 2.41 (4.99) | χ2(1) = 8.81 | .003 | OR = 3.77 | 1.57–9.06 |
| Suicidal ideation, past month | 11.72 (11.22) | 10.45 (11.34) | χ2(1) = 0.19 | .66 | OR = 1.12 | 0.67–1.88 |
| Suicide plans, past month | 3.97 (5.19) | 1.86 (5.83) | χ2(1) = 1.49 | .22 | OR = 2.13 | 0.63–7.17 |
| Suicide attempts, past month | 1.10 (1.95) | 0.03 (0.19) | χ2(1) = 11.23 | .001 | OR = 32.0 | 4.22–242.95 |
| NSSI, past year | 159.15 (224.16) | 68.59 (132.71) | χ2(1) = 3.63 | .06 | OR = 2.32 | 0.98–5.52 |
| Suicidal ideation, past year | 148.46 (127.60) | 90.07 (100.34) | χ2(1) = 3.74 | .05 | OR = 1.65 | 0.99–2.74 |
| Suicide plans, past year | 35.64 (62.45) | 19.62 (67.80) | χ2(1) = 0.67 | .41 | OR = 1.82 | 0.44–7.57 |
| Suicide attempts, past year | 4.50 (10.01) | 1.36 (3.85) | χ2(1) = 3.21 | .07 | OR = 3.32 | 0.89–12.31 |
| Suicide attempts, lifetime | 7.93 (15.91) | 1.54 (2.73) | χ2(1) = 10.89 | <.001 | OR = 5.16 | 1.95–13.68 |
BPD = borderline personality disorder; BPD symptoms = Zanarini Rating Scale for Borderline Personality Disorder; Depression symptoms = Beck Depression Inventory-II; Suicidal ideation severity = Scale for Suicidal Ideation; Sexual abuse severity = Childhood Trauma Questionnaire (CTQ) mean sexual abuse score; Sexual abuse frequency = Childhood Trauma Interview (CTI), total frequency of sexual abuse experiences; Physical abuse severity = CTQ mean physical abuse score; Physical abuse frequency = CTI, total frequency of sexual abuse experiences; MDD = major depressive disorder; NOS = not otherwise specified; NSSI = non-suicidal self-injury. Critical alpha for all statistical tests reported was p < .01.
3.3. Baseline NSSI and suicidality
Results for baseline analyses are presented in Table 1. Abuse was associated with more NSSI in the past month as well as more frequent past month and lifetime suicide attempts. Suicidal ideation also was more common in the abuse group, but this did not survive the more conservative critical alpha. In sensitivity analyses, the NSSI and suicide attempt findings remained statistically significant when we controlled for the number of BPD symptoms that participants endorsed (ps < .013, ORs > 3.41). When we controlled for ZAN-BPD scores, abuse was still significantly associated with past month and lifetime suicide attempts (ps < .003, ORs > 21.62), but not with past month NSSI (p = .05, OR = 2.73). Participants with a history of abuse also had more severe suicidal ideation (i.e., higher SSI scores) than those who had no abuse history but at a trend level.
3.4. Predicting NSSI and suicidality
Table 2 summarizes our findings at the 1-month and 2-month follow-up assessments. Abuse group was not associated with the frequency of NSSI at either follow-up. At the 1-month follow-up, being in the abuse group, versus the no abuse group, was associated with more past month suicidal ideation. This effect remained when we controlled for BPD symptom count (p = .03, OR = 1.70) and was marginally significant when we controlled for BPD symptom severity (p = .05, OR = 1.69). At the same time, neither of these findings survived the conservative alpha threshold. Abuse group was not associated with the frequency of suicide plans at the 1-month follow-up assessment; however, at the 2-month follow-up, abuse was associated with more frequent suicidal ideation. The effect of abuse on suicidal ideation at the 2-month follow-up remained statistically significant in both sensitivity analyses (ps < .04, ORs > 2.31).
Table 2.
Predicting non-suicidal self-injury and suicidality at the 1- and 2- month follow-up assessments.
| Predictor | b (SE) | χ2 | OR | CI95 |
|---|---|---|---|---|
| NSSI 1-month [χ2(2, n = 53) = 123.29, p < .001, AIC = 399.06] | ||||
| Baseline NSSI | 0.05 (.01) | 36.14*** | 1.06 | 1.04–1.08 |
| Abuse | 0.12 (.53) | 0.05 | 1.13 | 0.40–3.21 |
| SI 1-month [χ2(2, n = 53) = 223.32, p < .001, AIC = 446.58] | ||||
| Baseline SI | 0.06 (.01) | 52.68*** | 1.06 | 1.05–1.08 |
| Abuse | 0.63 (.26) | 5.76* | 1.89 | 1.12–3.16 |
| SP 1-month [χ2(2, n = 53) = 9.75, p = .008, AIC = 122.67] | ||||
| Baseline SP | 0.07 (.04) | 3.09 | 1.08 | 0.99–1.17 |
| Abuse | 0.57 (1.03) | 0.30 | 1.76 | 0.24–13.25 |
| NSSI 2-month [χ2(2, n = 40) = 27.72, p < .001, AIC = 205.37] | ||||
| Baseline NSSI | 0.04 (.02) | 4.79* | 1.04 | 1.00–1.08 |
| Abuse | 0.34 (.69) | 0.24 | 1.40 | 0.36–5.41 |
| SI 2-month [χ2(2, n = 40) = 155.98, p < .001, AIC = 375.07] | ||||
| Baseline SI | 0.05 (.01) | 13.03*** | 1.05 | 1.02–1.08 |
| Abuse | 0.99 (.35) | 7.87** | 2.69 | 1.35–5.36 |
| SP 2-month [χ2(2, n = 40) = 74.22, p < .001, AIC = 227.66] | ||||
| Baseline SP | 0.09 (.04) | 4.68* | 1.09 | 1.01–1.18 |
| Abuse | 2.94 (1.25) | 5.56* | 18.97 | 1.64–219.21 |
NSSI = non-suicidal self-injury; SI = suicidal ideation; SP = suicide planning. Critical alpha for all statistical tests reported was p < .01.
p < .05.
p < .01.
p < .001.
3.5. Exploratory analyses
Exploratory analyses were limited by the sample size and focused on group differences between participants reporting: (a) no abuse (n = 29), (b) sexual abuse only (n = 19), and (c) co-occurring physical and sexual abuse (n = 10).2 The no abuse (M = 16.97, SD = 1.97), sexual abuse only (M = 17.47, SD = 1.93), and co-occurring abuse groups (M = 16.30, SD = 1.57) did not significantly differ in age, F(2, 55) = 1.28, p = .29, η2p = .04. However, the three groups differed in baseline BPD symptom levels, F(2, 55) = 7.58, p = .001, η2p = .22, such that the co-occurring abuse group (M = 23.05, SE = 2.24) reported more severe BPD symptoms than both the no abuse group (M = 12.93, SE = 1.32; p < .001, d = 1.38) and the sexual abuse group (M = 15.68, SE = 1.63; p = .010, d = 1.02). There was no difference between the sexual abuse and no abuse groups (p = .19, d = .39). In addition, the groups differed on SSI scores, F(2, 55) = 6.58, p = .003, η2p = .19, such that the co-occurring abuse group (M = 23.95, SE = 3.16) endorsed higher levels of suicidal ideation than the no abuse group (M = 11.08, SE = 1.85; p = .001, d = 1.18) and the sexual abuse group (M = 11.90, SE = 2.29; p = .003, d = 1.19). There were no significant differences in suicidality between the sexual abuse and no abuse groups (p = .78, d = .09).
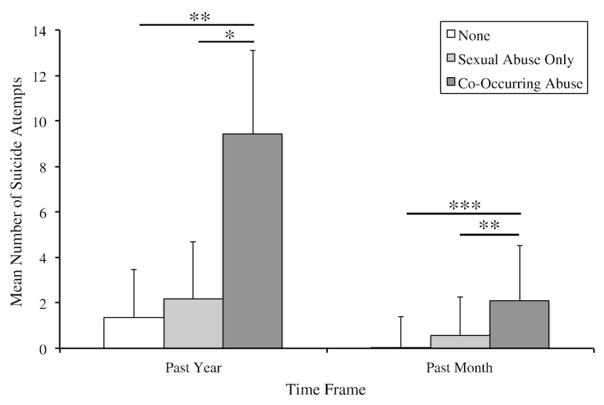
Table 3 summarizes differences in NSSI and suicidal thoughts and behaviors among the three groups. Being in the co-occurring abuse group was associated with: (a) more frequent past month and past year NSSI relative to the no abuse group and (b) greater past month NSSI compared to the sexual abuse group. The remaining associations between group and NSSI were non-significant. Membership in the co-occurring abuse group was associated with: (a) significantly more past month and past year suicidal ideation relative to the sexual abuse group and (b) more past year ideation compared to the no abuse group. All other associations between group and suicidal ideation were non-significant. Being in the co-occurring abuse group also was associated with: (a) more suicide attempts in the past month, past year, and lifetime, relative to the no abuse group and (b) more past month and past year suicide attempts relative to the sexual abuse only group. Additionally, membership in the sexual abuse group, versus the no abuse group, was associated with more past month suicide attempts (see Fig. 1).
Table 3.
Non-suicidal self-injury and suicidality as a function of abuse group status.
| Total effect | NA+ vs. CA | NA+ vs. SA | SA+ vs. CA | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| χ2 | b (SE) | OR | CI95 | b (SE) | OR | CI95 | b (SE) | OR | CI95 | |
| NSSI, past month | 17.03*** | 1.89 (.47)*** | 6.63 | 2.63–16.69 | 0.82 (.51) | 2.27 | 0.84–6.14 | 1.07 (.44)* | 2.92 | 1.23–6.96 |
| Ideation, past month | 6.27* | 0.53 (.27) | 1.69 | 0.99–2.89 | −0.20 (.33) | 0.82 | 0.43–1.57 | 0.72 (.33)* | 2.06 | 1.09–3.90 |
| Plans, past month | 4.49 | 1.17 (.64) | 3.22 | 0.91–11.38 | 0.44 (.67) | 1.56 | 0.42–5.79 | 0.73 (.46) | 2.07 | 0.84–5.11 |
| Attempts, past month | 16.39*** | 4.11 (1.07)*** | 60.9 | 7.48–495.70 | 2.82 (1.03) ** | 16.79 | 2.21–127.49 | 1.29 (.53)* | 3.63 | 1.28–10.30 |
| NSSI, past year | 8.65* | 1.19 (.41)** | 3.28 | 1.46–7.37 | 0.56 (.60) | 1.75 | 0.54–5.73 | 0.63 (.53) | 1.87 | 0.66–5.34 |
| Ideation, past year | 10.76** | 0.85 (.27)** | 2.35 | 1.38–3.99 | 0.23 (.31) | 1.26 | 0.68–2.33 | 0.62 (.30)* | 1.86 | 1.04–3.33 |
| Plans, past year | 0.68 | 0.63 (.88) | 1.88 | 0.33–10.63 | 0.58 (.78) | 1.79 | 0.39–8.17 | 0.05 (.77) | 1.05 | 0.23–4.72 |
| Attempts, past year | 7.48* | 1.94 (.75)** | 6.96 | 1.62–29.99 | 0.46 (.71) | 1.59 | 0.40–6.35 | 1.48 (.71)* | 4.38 | 1.10–17.50 |
| Attempts, lifetime | 15.82*** | 2.26 (.58)*** | 9.62 | 3.11–29.78 | 1.12 (.63) | 3.05 | 0.89–10.43 | 1.15 (.71) | 3.16 | 0.78–12.76 |
NA = no abuse; CA = co-occurring physical and sexual abuse; SA = sexual abuse only; NSSI = non-suicidal self-injury.
Denotes the comparison group.
p < .05.
p < .01.
p < .001.
Fig. 1.
Mean number of past year and past month suicide attempts reported by participants, stratified by abuse group (no abuse, sexual abuse only and co-occurring abuse). Note. ***p < .001; **p < .01; *p < .05. The effect of abuse group (no abuse, sexual abuse only and co-occurring abuse) was significant for both the past year attempts, F(2, 53) = 4.40, = .02, η2p = .14, and past month attempts, F(2, 55) = 9.43, p < .001, η2p = .26.
Table 4 summarizes associations between baseline abuse group status (no abuse, sexual abuse only and co-occurring abuse) and NSSI and suicide ideation at the 1- and 2-month follow-up assessments.3 Controlling for baseline suicidal ideation, sexual abuse (versus no abuse) and co-occurring abuse (versus no abuse) were associated with more frequent suicide ideation at both the 1- and 2-month follow-up assessments. In contrast, abuse group was not associated with the frequency of NSSI at either of the follow-up assessments.
Table 4.
Predicting non-suicidal self-injury and suicide ideation at the 1- and 2- month follow-up assessments from baseline abuse group status.
| Predictor | b (SE) | χ2 | OR | CI95 |
|---|---|---|---|---|
| NSSI 1-month [χ2 (3, n = 53) = 125.00, p < .001, AIC = 399.36] | ||||
| Baseline NSSI | 0.06 (.02) | 10.85*** | 1.06 | 1.02–1.10 |
| Abuse | ||||
| None | Ref. | |||
| Sexual only | 0.21 (.55) | 0.14 | 1.23 | 0.42–3.61 |
| Co-occurring | −0.09 (.87) | 0.01 | 0.91 | 0.17–5.01 |
| SI 1-month [χ2(3, n = 53) = 223.86, p < .001, AIC = 448.03] | ||||
| Baseline SI | 0.06 (.01) | 52.81*** | 1.06 | 1.05–1.08 |
| Abuse | ||||
| None | Ref. | |||
| Sexual only | 0.59 (.29) | 4.21* | 1.80 | 1.03–3.14 |
| Co-occurring | 0.68 (.31) | 4.96* | 1.98 | 1.09–3.62 |
| NSSI 2-month [χ2 (3, n = 40) = 40.51, p < .001, AIC = 194.58] | ||||
| Baseline NSSI | 0.02 (.02) | 0.71 | 1.02 | 0.97–1.07 |
| Abuse | ||||
| None | Ref. | |||
| Sexual only | −0.55 (.69) | 0.63 | 0.58 | 0.15–2.23 |
| Co-occurring | 1.07 (.92) | 1.36 | 2.91 | 0.40–17.52 |
| SI 2-month [χ2(3, n = 40) = 157.25, p < .001, AIC = 375.80] | ||||
| Baseline SI | 0.05 (.02) | 10.72** | 1.06 | 1.02–1.09 |
| Abuse | ||||
| None | Ref. | |||
| Sexual only | 1.08 (.34) | 10.02** | 2.96 | 1.51–5.78 |
| Co-occurring | 0.92 (.45) | 4.14* | 2.50 | 1.03–6.05 |
NSSI = non-suicidal self-injury; SI = suicidal ideation.
p < .05.
p < .01.
p < .001.
4. Discussion
The present study examined the impact of child abuse –particularly physical and sexual abuse – on NSSI and suicidality in BPD youth. Three important findings emerged. First, child abuse showed a cross-sectional but not a prospective relationship with NSSI. Second, child abuse (compared to no abuse) is associated with a 5-fold increase in the rate of lifetime suicide attempts, and in line with our hypothesis, prospectively predicted suicide ideation and planning (trend level), but not attempts. Third, exploratory analyses found that the co-occurrence of physical and sexual abuse contributes to more severe NSSI and suicidality.
First, compared to adolescents with no childhood abuse, BPD youth with abuse histories endorsed more frequent NSSI prior to admission to an intensive DBT program. Yet, when controlling for BPD symptom severity, these effects do not persist, suggesting that BPD severity influences NSSI engagement. Contrary to hypotheses, child abuse did not prospectively predict NSSI frequency. As participants were recruited from an intensive treatment program, these null findings may reflect DBT-related effects. Specifically, before initiating DBT, patients must commit to refraining from engaging in self-injuring behaviors and are provided with 24-h skills coaching to help manage urges. In a more naturalistic setting (i.e., BPD youth without treatment), prospective differences might arise, which would be consistent with prior research among BPD adults [44].
Second, the presence of abuse was associated with a 5-fold increase in the rate of past suicide attempts, and this effect predicted above and beyond BPD symptom severity. Similarly, BPD youth with a history of abuse reported higher rates of past suicidal ideation (at a trend level), and prospective findings showed similar differences in suicide ideation during the follow-up period. As a whole, child abuse is a robust predictor of increased suicidality in BPD youth, which is largely consistent with BPD adults [16,21,45]. Given the impact of abuse on suicidal behaviors within this high-risk population, recent treatment protocols have targeted the co-occurrence of BPD and PTSD; particularly as a means of combating persistent symptoms that often are unaffected using more traditional treatments [46]. Such an approach teaches patients to concurrently process trauma-related emotions and cognitions (i.e., via prolonged exposure protocols) while also learning DBT coping strategies to reduce affective lability and self-destructive behaviors. Preliminary findings in adults have demonstrated that patients were 1.5 times less likely to self-injure and 2.4 times less likely to attempt suicide in the dual-focused treatment as compared to standard DBT [47].
Last, exploratory analyses found that the co-occurrence of physical and sexual abuse contributed to greater NSSI and suicidality (i.e., ideation, plans, and attempts). Broadly speaking, this pattern is consistent with the dose–response effect reported in adult populations whereby the cumulative impact of abuse impacts the severity and persistence of self-injurious and suicidal behaviors [48–50] cf. [51]. These findings suggest that traumatic experiences from childhood, and consequent trauma-related or PTSD symptoms, may exert an influence over the lifespan and play a critical role in NSSI [52] and suicidality [16]. Recent studies suggest that self-injury plays a functional role in coping with trauma-related symptoms (which take the form of intrusive memories, trauma-related beliefs, and enduring negative emotions), and in this context, NSSI serves to alleviate the psychological distress associated with trauma-related symptoms [20,31]. One implication of these findings is that more attention needs to be paid to the specific role of trauma-related symptoms and/or co-occurring PTSD diagnoses in the design and delivery of treatments that will be maximally effective for the subgroup of BPD patients who have experienced childhood abuse and present with high levels of NSSI and suicidality. Idiographic, person-centered approaches that account for both the type and severity of abuse may, ultimately, lead to more optimal outcomes for high-risk BPD youth.
4.1. Limitations
Findings should be interpreted in light of several limitations. First, our sample size was relatively small, included only female youth, primarily Caucasian, and was recruited from an intensive DBT program, which may limit generalizability. Further, the relatively short follow-up period precluded our ability to test NSSI and suicidality over longer periods. Second, while the study probed NSSI frequency over time, changes in NSSI frequency may be directly influenced by the intensive treatment. To better understand the trajectory of NSSI, further study within a more naturalistic setting is warranted. Third, the study relied on the retrospective recall of abuse, which may be susceptible to respondent bias. Fourth, bipolar spectrum disorders were diagnosed in 13 participants, which may reflect the acuity of the sample, which was recruited from an intensive DBT program. At the same time, this severity may impact the generalizability of our findings. Last, clinical interviews were not recorded, and thus, inter-rater reliability was not obtained. However, BPD diagnoses were confirmed with the primary clinician, and recalibration meetings were held to ensure diagnostic reliability.
4.2. Clinical implications and future directions
Recent studies focusing on the treatment of adults with BPD and trauma have highlighted the importance of providing targeted, evidence-based treatment to this population. Childhood abuse experiences can impact and maintain self-injurious and suicidal behaviors, and treatment that includes direct processing of past abuse coupled with standard cognitive-oriented therapies (e.g., DBT PE) may be most beneficial [47]. Presently, little is known about how these treatments would impact BPD youth, and thus, future research using this dual approach may prove to be more effective for reducing NSSI and suicidality within this high-risk population.
Acknowledgments
Randy P. Auerbach was partially supported through funding from: National Institute of Mental Health K23MH097786, the Simches Fund, the Rolfe Fund, and the Warner Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or NIMH.
Footnotes
Analyses were not conducted on suicide attempts at the two follow-up assessments; the small number of occurrences would violate the assumptions of chi-square analyses.
We did not create a physical abuse only group because only 10 participants reported physical abuse, and all 10 also reported co-occurring sexual abuse.
Results for suicide plans at the 1- and 2-month follow-ups are not included here, as these models did not converge; the validity of the models for follow-up suicide plans is therefore uncertain.
Disclosure of interest
Dr. Blaise Aguirre is a consultant for Behavioral Tech, but these activities are not related to the current project. All other authors declare that they have no conflicts of interest.
References
- 1.Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet. 2011;377:74–84. doi: 10.1016/S0140-6736(10)61422-5. [DOI] [PubMed] [Google Scholar]
- 2.Korzekwa MI, Dell PF, Links PS, Thabane L, Webb SP. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr Psychiatry. 2008;49:380–6. doi: 10.1016/j.comppsych.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Leung SW, Leung F. Construct validity and prevalence rate of borderline personality disorder among Chinese adolescents. J Personal Disord. 2009;23:494–513. doi: 10.1521/pedi.2009.23.5.494. [DOI] [PubMed] [Google Scholar]
- 4.Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry. 2001;58:590–6. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- 5.Zanarini MC, Horwood J, Wolke D, Waylen A, Fitzmaurice G, Grant BF. Prevalence of DSM-IV borderline personality disorder in two community samples: 6,330 English 11-year-olds and 34,653 American adults. J Personal Disord. 2011;25:607–19. doi: 10.1521/pedi.2011.25.5.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chanen AM, Jackson HJ, McGorry PD, Allot KA, Clarkson V, Yuen HP. Two-year stability of personality disorder in older adolescent outpatients. J Personal Disord. 2004;18:526–41. doi: 10.1521/pedi.18.6.526.54798. [DOI] [PubMed] [Google Scholar]
- 7.Ha C, Balderas JC, Zanarini MC, Oldham J, Sharp C. Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. J Clin Psychiatry. 2014;75:e457–64. doi: 10.4088/JCP.13m08696. [DOI] [PubMed] [Google Scholar]
- 8.Levy KN, Becker DF, Grilo CM, Mattanah JJ, Garnet KE, Quinlan DM, et al. Concurrent and predictive validity of the personality disorder diagnosis in adolescent inpatients. Psychiatry. 1999;156:1522–8. doi: 10.1176/ajp.156.10.1522. [DOI] [PubMed] [Google Scholar]
- 9.Nock MK, Joiner TE, Jr, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 10.Muehlenkamp JJ, Ertelt TW, Miller AL, Claes L. Borderline personality symptoms differentiate non-suicidal and suicidal self-injury in ethnically diverse adolescent outpatients. J Child Psychol Psychiatry. 2011;52:148–55. doi: 10.1111/j.1469-7610.2010.02305.x. [DOI] [PubMed] [Google Scholar]
- 11.Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. Childhood maltreatment associated with adult personality disorders: findings from the Collaborative Longitudinal Personality Disorders Study. J Personal Disord. 2004;18:193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- 12.Johnson JG, Cohen P, Smailes EM, Skodol AE, Brown J, Oldham JM. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Compr Psychiatry. 2001;42:16–23. doi: 10.1053/comp.2001.19755. [DOI] [PubMed] [Google Scholar]
- 13.Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. J Personal Disord. 2002;16:201–14. doi: 10.1521/pedi.16.3.201.22542. [DOI] [PubMed] [Google Scholar]
- 14.Widom CS, Czaja SJ, Paris J. A prospective investigation of borderline personality disorder in abused and neglected children followed up into adulthood. J Personal Disord. 2009;23:433–46. doi: 10.1521/pedi.2009.23.5.433. [DOI] [PubMed] [Google Scholar]
- 15.Fossati A, Madeddu F, Maffei C. Borderline personality disorder and childhood sexual abuse: a meta-analytic study. J Personal Disord. 1999;13:268–80. doi: 10.1521/pedi.1999.13.3.268. [DOI] [PubMed] [Google Scholar]
- 16.Wedig MM, Silverman MH, Frankenburg FR, Reich DB, Fitzmaurice G, Zanarini MC. Predictors of suicide attempts in patients with borderline personality disorder over 16 years of prospective follow-up. Psychol Med. 2012;42:2395–404. doi: 10.1017/S0033291712000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zanarini MC, Yong L, Frankenburg FR, Hennen J, Reich DB, Marino MF, et al. Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline inpatients. J Nerv Ment Dis. 2002;190:381–7. doi: 10.1097/00005053-200206000-00006. [DOI] [PubMed] [Google Scholar]
- 18.MacIntosh HB, Godbout N, Dubash N. Borderline personality disorder: disorder of trauma or personality, a review of the empirical literature. Can Psychol. 2015;56:227–41. [Google Scholar]
- 19.Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Psychiatry. 2000;157:601–8. doi: 10.1176/appi.ajp.157.4.601. [DOI] [PubMed] [Google Scholar]
- 20.Zanarini MC. Childhood experiences associated with the development of borderline personality disorder. Psychiatr Clin North Am. 2000;23:89–101. doi: 10.1016/s0193-953x(05)70145-3. [DOI] [PubMed] [Google Scholar]
- 21.Brodsky BS, Malone KM, Ellis SP, Dulit RA, Mann JJ. Characteristics of borderline personality disorder associated with suicidal behavior. Psychiatry. 1997;154:1715–9. doi: 10.1176/ajp.154.12.1715. [DOI] [PubMed] [Google Scholar]
- 22.Soloff PH, Fabio A. Prospective predictors of suicide attempts in borderline personality disorder at one, two, and two-to-five year follow-up. J Personal Disord. 2008;22:123–34. doi: 10.1521/pedi.2008.22.2.123. [DOI] [PubMed] [Google Scholar]
- 23.Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Psychiatry. 2003;160:274–83. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- 24.Zanarini MC, Laudate CS, Frankenburg FR, Reich DB, Fitzmaurice G. Predictors of self-mutilation in patients with borderline personality disorder: a 10-year follow-up study. J Psychiatr Res. 2011;45:823–8. doi: 10.1016/j.jpsychires.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McFetridge MA, Milner R, Gavin V, Levita L. Borderline personality disorder: patterns of self-harm, reported childhood trauma and clinical outcomes. Psychiatry Open. 2015;1:18–20. doi: 10.1192/bjpo.bp.115.000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rusch N, Corrigan PW, Bohus M, Kuhler T, Jacob GA, Lieb K. The impact of posttraumatic stress disorder on dysfunctional implicit and explicit emotions among women with borderline personality disorder. J Nerv Ment Dis. 2007;195:537–9. doi: 10.1097/NMD.0b013e318064e7fc. [DOI] [PubMed] [Google Scholar]
- 27.Westen D, Ludolph P, Misle B, Ruffins S, Block J. Physical and sexual abuse in adolescent girls with borderline personality disorder. Orthopsychiatry. 1990;60:55–66. doi: 10.1037/h0079175. [DOI] [PubMed] [Google Scholar]
- 28.Wolke D, Schreier A, Zanarini MC, Winsper C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: a prospective study. J Child Psychol Psychiatry. 2012;53:846–55. doi: 10.1111/j.1469-7610.2012.02542.x. [DOI] [PubMed] [Google Scholar]
- 29.Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. 2008;37:363–75. doi: 10.1080/15374410801955771. [DOI] [PubMed] [Google Scholar]
- 30.Harned MS, Jackson SC, Comtois KA, Linehan MM. Dialectical behavior therapy as a precursor to PTSD treatment for suicidal and/or self-injuring women with borderline personality disorder. J Trauma Stress. 2010;23:421–9. doi: 10.1002/jts.20553. [DOI] [PubMed] [Google Scholar]
- 31.Nock MK, Prinstein MJ. Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol. 2005;114:140–6. doi: 10.1037/0021-843X.114.1.140. [DOI] [PubMed] [Google Scholar]
- 32.First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured Clinical Interview for DSM-IV Axis II personality disorders (SCID-II, version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- 33.Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–90. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 34.Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) J Clin Psychiatry. 2010;71:313–26. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- 35.Auerbach RP, Millner AJ, Stewart JG, Esposito EC. Identifying differences between depressed adolescent suicide ideators and attempters. J Affect Disord. 2015;186:127–33. doi: 10.1016/j.jad.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nock MK, Holmberg EB, Photos VI, Michel BD. Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychol Assess. 2007;19:309–17. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- 37.Venta AS, Sharp C. Extending the concurrent validity of the Self-Injurious Thoughts and Behaviors Interview to inpatient adolescents. J Psychopathol Behav Assess. 2014;36:675–82. [Google Scholar]
- 38.Bernstein DP, Fink L. Manual for the Childhood Trauma Questionnaire: a retrospective self-report. New York, NY: Harcourt Brace & Company; 1998. [Google Scholar]
- 39.Fink LA, Bernstein D, Handelsman L, Foote J, Lovejoy M. Initial reliability and validity of the Childhood Trauma Interview: a new multidimensional measure of childhood interpersonal trauma. Psychiatry. 1995;152:1329–35. doi: 10.1176/ajp.152.9.1329. [DOI] [PubMed] [Google Scholar]
- 40.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 41.Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): a continuous measure of DSM-IV borderline psychopathology. J Personal Disord. 2003;17:233–42. doi: 10.1521/pedi.17.3.233.22147. [DOI] [PubMed] [Google Scholar]
- 42.Beck AT, Steer RA, Ranieri WF. Scale for Suicide Ideation: psychometric properties of a self-report version. J Clin Psychol. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 43.Cameron AC, Trivedi PK. Microeconometrics with STATA. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 44.van der Kolk BA, Perry JC, Herman JL. Childhood origins of self-destructive behavior. Psychiatry. 1991;148:1665–71. doi: 10.1176/ajp.148.12.1665. [DOI] [PubMed] [Google Scholar]
- 45.Horesh N, Nachshoni T, Wolmer L, Toren P. A comparison of life events in suicidal and nonsuicidal adolescents and young adults with major depression and borderline personality disorder. Compr Psychiatry. 2009;50:496–502. doi: 10.1016/j.comppsych.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 46.Harned MS. Treatment of posttraumatic stress diosrder with comorbid borderline personality disorder. In: McKay D, Storch E, editors. Handbook of treating variants and complications in anxiety disorders. New York, NY: Springer Press; 2013. pp. 203–21. [Google Scholar]
- 47.Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav Res Ther. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Psychiatry. 2003;160:1453–60. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- 49.Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 50.Yates TM. The developmental psychopathology of self-injurious behavior: compensatory regulation in posttraumatic adaptation. Clin Psychol Rev. 2004;24:35–74. doi: 10.1016/j.cpr.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 51.Heath NL, Toste JR, Nedecheva T, Charlebois A. An examination of nonsuicidal self-injury among college students. J Ment Health Couns. 2008;30:137–56. [Google Scholar]
- 52.Smith NB, Kouros CD, Meuret AE. The role of trauma symptoms in nonsuicidal self-injury. Trauma Violence Abuse. 2014;15:41–56. doi: 10.1177/1524838013496332. [DOI] [PubMed] [Google Scholar]