Abstract
Background: Environmental tobacco smoke (ETS) exposure is associated with an increased risk of many diseases. Many countries have ratified a national smoking ban in public places, but studies on factors related to smoking issues in public places post-ban are lacking. Aim: To identify facilitators and barriers that influenced smokers’ compliance with smoking bans in public places. Methods: Using PubMed, MEDLINE, and the Web of Science database, we conducted a systematic search of English articles published before June 2015 on factors of smokers’ compliance with the smoking bans in public places. Results: A total of 390 references were identified, among which seventeen articles (twelve quantitative studies, two qualitative studies, three mixed-method studies) were included in this review. These studies focused on four types of public places including recreational venues (n = 7), hospital (n = 5), school (n = 4), and workplace (n = 1). Factors at the individual-, interpersonal-, and organizational-level were identified: at the individual level, nicotine dependence, insufficiency of tobacco-related knowledge, and the negative attitudes towards smoking bans were the most commonly identified barriers; at the interpersonal level, the smoking behaviors of people around, close relatives, and friends’ approval were the main barriers; and at the organizational level, the main barriers were inefficient implementation of the bans and the inconvenience of the designative smoking areas. Conclusions: This synthesis of the literature provided evidence of the identified barriers and facilitators of smokers’ compliance with the smoking bans. It will be beneficial for the policy-maker to consider interventions on multiple levels of factors to overcome the barriers and enhance smokers’ compliance with the smoking bans in public places.
Keywords: facilitators, barriers, smoking bans, public places, environmental tobacco smoke
1. Introduction
Exposure to environmental tobacco smoke (ETS) has been associated with premature death and morbidity [1]; it has been documented to be as harmful as active smoking and is the cause of a wide spectrum of morbidity and more than 600,000 premature deaths worldwide [2]. There is no safe level for ETS exposure [3] and, globally, there are more than one billion smokers who can potentially expose others to ETS [4]. In response to this important public health issue, as of September 2010, national smoke-free legislation, which is a key policy under the WHO Framework Convention on Tobacco Control (FCTC), has been ratified by over 170 countries [5]. The main goals of a smoking ban in public places are to protect non-smokers from the dangers of environmental tobacco smoke and provide a supportive environment for those who want to quit smoking [6,7]. It has been well documented that smoking bans are beneficial for improving cardiovascular health outcomes and reducing smoking-related mortality [8]. Different countries have different attitudes towards the smoking bans and strategies for effective implementation. The bans differ across countries [9]. Studies have shown that developed countries were more successful in implementing the smoking bans than developing countries [10] where the support for the bans might be limited by the lack of knowledge and awareness about the adverse effects of passive smoking [11]. A recent review also found the impact of legislative bans on smoking prevalence and tobacco consumption [12]. Smokers’ individual characteristics may affect whether smokers choose to smoke in public places post-ban [5]. For example, some smokers were indifferent to both their own health and others’ [13] and viewed smoking as their freedom and right, so the health promotion on the banning smoking in the public places might be less effective for them [14]. It is also difficult for some smokers to voluntarily comply with the ban without the external restrictions, such as the responsible, sufficient monitoring and effective legal enforcement system [15]. Even though some smokers realize the harm of environmental tobacco smoke [16], the appearance of nicotine withdrawal symptoms and cigarette cravings can make smokers violate the ban unintentionally [17,18].
In order to promote the implementation of smoking bans in the public places and deal with the issue of continued smoking post-ban, it is imperative to explore the factors related to the smokers’ compliance with the bans [19]. To date, no such overview has been provided. Therefore, this review aims to fill the gap and identify the facilitators and barriers of smokers’ compliance with smoking bans in the public places.
2. Methods
2.1. Search Strategy
A comprehensive search was conducted using PubMed, MEDLINE, and the Web of Science database for all studies published before June 2015 on the facilitators and barriers of smokers’ compliance with smoking bans in public places. We used a set of combinations of keywords in the literature search, including words reflecting smokers (extended to patients, employees, students, staff, and patrons), compliance (e.g., comply, compliant), smoke-free (e.g., nonsmoking, no-smoking), ban (e.g., legislation, rule), predictor (e.g., barrier, factor), and public places (e.g., school, hospital). The full search strategy with adapted terms is included in supplementary material.
2.2. Inclusion and Exclusion Criteria
Studies included should provide either qualitative, quantitative or mixed-method (i.e., cross-sectional, case-control, and cohort design) data on barriers and/or facilitators of smokers’ compliance with the smoking bans in the public places and been written in English. Studies that focused on places, such as home, personal car, outdoor, and prison, were excluded. Reviews, comments, letters, posters, book chapters, and books were also excluded. Two reviewers (Zhou L. and Jiang C.) independently conducted the screening by title and abstract firstly and then further reviewed the full texts for eligibility. Wherever differences occurred between the two reviewers, consensus was reached by mutual discussion.
2.3. Data Extraction
Data about the included studies were extracted, which included the name of the first author, year of publication, study setting (the type of public places and country), study design, sampling methods, sample characteristics, barriers and/or facilitators of smokers’ compliance with the smoking bans in the public places, and measurements/definitions of compliance.
2.4. Data Synthesis
All themes relevant to facilitators and barriers of smokers’ compliance with smoking bans in public places were identified and extracted from all eligible studies. Through discussion and consensus among three reviewers (Zhou L., Niu L., and Jiang H.), these themes were summarized and then categorized using the following main domains of the Social Ecological Model [20,21]: individual level, interpersonal level, and organizational level.
2.5. Quality Assessment
The quality of the included studies was assessed using the quality assessment tool “QUALSYST” from the study “Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields” [22]. It contains 14 items for quantitative study and 10 items for qualitative study. Each item was scored based on the degree to which the specific criteria were met (“yes” = 2, “partial” = 1, and “no” = 0). Items which were not applicable (marked as “NA”) were excluded from the summary score. The summary score for each study was calculated as the division of the total score obtained across relevant items by the possible maximum scores. Mixed-method studies were assessed by quantitative and qualitative studies items separately, and then the average score was calculated as a summary score. The summary score ranged from 0 to 1 with a higher score indicating better quality. Two reviewers (Zhou L. and Jiang C.) independently evaluated the quality of the included articles. Wherever the ratings differed between the two reviewers, they discussed until a consensus was reached.
3. Results
3.1. Search Results
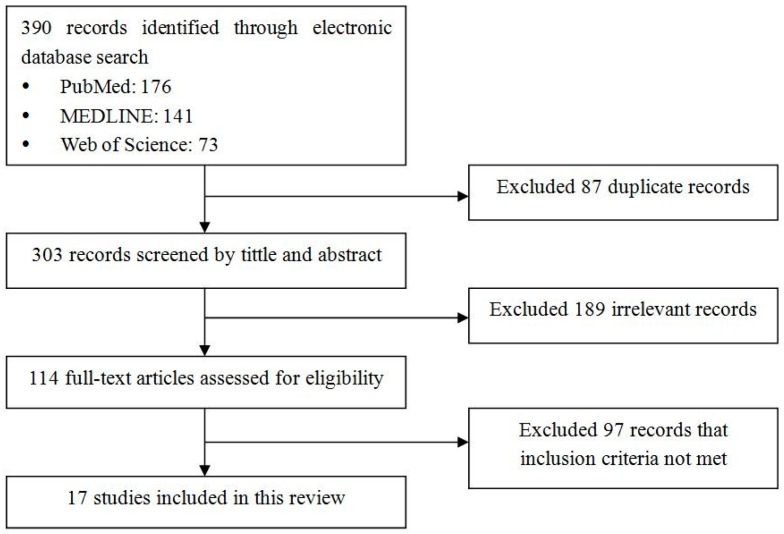
The flowchart of literature search is presented in Figure 1. A total of 390 articles were identified in the search, and 87 duplicated articles were retrieved from three databases. After the evaluation of titles and abstracts, 189 irrelevant articles were excluded. We assessed 114 full-text articles for eligibility and, finally, 17 articles published between 1998 and 2015 were included in this review. In these included studies, one article [23] was published before 2000, eight articles [16,17,18,24,25,26,27,28] were published between 2000 and 2009, and eight articles [5,9,29,30,31,32,33,34] were published after 2010.
Figure 1.
Flowchart for review of studies on facilitators and barriers of smokers’ compliance with smoking bans in public places.
3.2. Characteristics of the Study
As shown in Table 1, the included studies focused on four types of public places including recreational venues (e.g., bars, restaurants; n = 7) [5,9,24,26,27,28,29], hospital (n = 5) [17,18,23,25,30], school (n = 4) [16,31,32,33], and workplace(n = 1) [34]. Eight studies were conducted in North America (two in Canada [26,30] and six in the USA [18,23,24,28,29,33], four in European countries [16,17,25,31], one in Asian countries [9], one in Australia [32], and three in multiple countries [5,27,34]. Twelve quantitative studies [5,9,16,17,18,23,25,26,27,29,31,34] were identified in this review. Nine studies were cross-sectional [9,16,17,23,25,26,27,31,34] and three were cohort [5,18,29]. Sample sizes ranged from 101 to 9046 participants. In the survey instrument, six studies [18,23,27,29,31,34] used self-designed questionnaires, six studies [5,9,16,17,25,26] used the scale from the published literature, five studies [9,17,23,25,26] of which provided information on the reliability or validity. Two qualitative studies [30,32] used semi-structured interviews and purposive sampling methods, with a sample size of 37 [32] and 82 [30] respectively. Additionally, three studies used mixed-method design [24,28,33].
Table 1.
Overview of included studies.
| First Author and Year | Risk of Bias | Setting/Country | Study Design | Sampling Methods | Sample Characteristics (Sample Size, Gender, Age) | Measurement/Definition of Compliance or Non-Compliance |
|---|---|---|---|---|---|---|
| Quantitative study | ||||||
| Rigotti, 2000 [18] | 0.86 | Hospital/U.S. | Cohort | Random | 650 inpatient smokers; 55% male; age: 49.2 ± 16.2 years | Patients who did not smoke while hospitalized or smoked outdoors only were classified as compliant; those who reported smoking indoors were noncompliant. |
| Sabidó, 2006 [17] | 0.91 | Hospital/Spain | Cross-sectional | Convenient | 229 inpatient smokers; 77% male; age: 50 ± 16.9 years | Compliant: those who did not smoke indoors or who only smoked outdoors; noncompliant: those who smoked indoors. |
| Parks, 2009 [25] | 0.77 | Hospital/UK | Cross-sectional | Convenient | 101 smoking staff; 22.8% male | Those who are compliant with smoke-free policy and only ever smoke off the site; those who are non-compliant and continue to smoke on site. |
| Lazuras, 2009 [16] | 0.73 | University/Greek | Cross-sectional | Convenient | 182 undergraduate smokers | Whether they had ever smoked in a smoke-free sector in public settings. |
| Lazuras, 2012 [34] | 0.73 | Companies/Greece and Bulgaria | Cross-sectional | Random | 170 daily or weekly smokers | Compliance with smoking restrictions in smoker-free sectors at work |
| Galán, 2012 [31] | 0.91 | Schools/Spain | Cross-sectional | Cluster | 1116 student smokers; 42.0% male | Having smoked sometime in the last thirty days on school premises in open or closed spaces. |
| Emmons, 1998 [23] | 0.77 | Hospitals/U.S. | Cross-sectional | Convenient | 358 hospitalized smokers; 45% male; mean age: 46 years | Adherence was defined as self-reporting of abstaining from cigarettes during the hospital stay. |
| Lacchetti, 2001 [26] | 0.86 | restaurants,workplaces, bingo halls, and hockey arenas/Canada | Cross-sectional | Random | 423 adult smokers | Compliance with more restrictions. |
| Li, 2010 [9] | 0.86 | Recreational venues/China | Cross-sectional | Stratified multistage cluster sampling | 2403 smokers who reported patronizing recreational venues; 84.0% males; age: 47.36 ± 8.53 | Smoking vs not smoking in recreational settings. |
| Nagelhout, 2011 [5] | 0.91 | Bars/Ireland, France, Netherlands, Germany | Cohort | Probability sampling | 4634 smokers; | Smoking in smoke-free bars. |
| Irvin, 2015 [29] | 0.91 | Korean bars and restaurants/U.S. | Cohort | Probability sampling | 224 current smokers of Korean descent who visited a Korean bar or restaurant bars and restaurants; 84.4% male; | Smoked inside Korean bars or restaurants. |
| Borland, 2006 [27] | 0.95 | recreational venues/U.S., Canada, UK, and Australia | Cross-sectional | Stratified random sampling | 9046 adult smokers; female (52.7%–56.6%) | Smoking inside recreational venues. |
| Qualitative study | ||||||
| Shopik, 2012 [30] | 0.85 | Hospital/Canada | Semi-structured interview | Convenient | 82 current smokers | Smoking in the hospital during hospitalization. |
| Jancey, 2014 [32] | 0.80 | University/Australian | An environmental audit; direct observation; intercept interview. | Convenient | 37 smokers (27% staff and 73% students); 83.8% male; 59.4% aged between 18 and 29 years |
Smoking behavior on campus. |
| Mixed-method study | ||||||
| Moore, 2006 [28] | 0.72 | Bars/U.S. | Structure observations, semi-structure interviewers | Study 1: random Study 2: opportunistic sampling |
Study 1: 479 observations study 2: 35 bar staff and patrons |
Non-compliance: patron smoking. |
| Moore, 2009 [24] | 0.78 | Bars/U.S. | High-structure naturalistic observations, semi-structured interviews | Random | 121 stand-alone bars | Indoor smoking by bar patrons and staff. |
| Russette, 2014 [33] | 0.72 | School/U.S. | Semi-structure interview with 22-item survey and two open-ended questions | Convenient | 60 student and non-student smokers; 52% male; mean age: 28 years | Smoking on campus property or off campus property. |
3.3. Risk of Bias
Overall, the quality of the included studies was good. Breakdown of quality appraisal markings was shown in the supplementary materials (Tables S1 and S2). The QualSyst scores ranged from 0.72 [28,33] to 0.95 [29], with a median score of 0.85 and an interquartile range of 0.77–0.91. For 15 quantitative studies (including three mixed method studies), the most frequently missing one was control of potential confounders. For five qualitative studies (including three mixed-method studies), where study quality was diminished was lack of verification procedure.
3.4. Barriers and Facilitators
3.4.1. Individual Level
As shown in Table 2, people who were heavier smokers [9,16,18,25,29,31], had heavier nicotine dependence [18,24,26,30], had more severe nicotine withdrawal symptoms [17,18], and had illicit drug consumption [31] were more likely to be noncompliant with the smoking bans in public places. In addition, smokers who had no quitting attempts [18] or were in the earlier stage of quitting and with less confidence on successful quitting [17] were more likely to smoke in public places in defiance of the bans. Three studies each reported supportive attitudes towards smoking [9,32,34] and negative attitudes towards the smoking bans [9,32,33]. Having lower education levels [31] and lower levels of knowledge of smoking harms [16] or being unaware of policy boundaries [32,33] were also reported as barriers of compliance with the bans. For hospitalized smokers with physical mobility limitations, it was inconvenient to smoke outside of the hospital [30].
Table 2.
Facilitators and barriers to smokers’ compliance with smoking bans in public places.
| Level | Facilitators | Studies | Barriers | Studies |
|---|---|---|---|---|
| Individual level | Demographic factors | |||
| Male | 1 [17] | Low education level | 1 [31] | |
| Being older | 2 [18,23] | Being older | 1 [34] | |
| Smoking behaviors | ||||
| Lighter smokers | 1 [23] | Heavier smokers | 6 [9,16,18,25,29,31] | |
| Heavier nicotine dependence | 4 [17,18,26,30] | |||
| Nicotine withdrawal symptoms | 2[17,18] | |||
| Quiting smoking | ||||
| Having confidence toquit smoking | 1 [23] | No confidence to quit smoking | 1 [17] | |
| No quit smoking attempts | 1 [18] | |||
| Earlier stage of quit smoking | 1 [17] | |||
| Without substance abuse | 1 [23] | Illicit drug consumption | 1 [31] | |
| Higher level of knowledge about smoking and passive smoking | 3 [5,9,34] | Less awareness of harms of smoking | 1 [16] | |
| Negative attitudes towards smoking | 1 [5] | Supportive attitudes towards smoking | 3 [9,32,34] | |
| Supportive attitudes towards the bans | 3 [5,27,33] | Negative attitude towards smoking | 3 [9,32,33] | |
| Unawareness of policy boundaries | 2 [32,33] | |||
| History of chronic dieases (e.g., dyspnea, heartdisease) | 1 [18] | Limited physical mobility | 1 [30] | |
| Interpersonal level | No parental permission | 1 [31] | Smoking behaviors of people around in the same setting | 3 [24,28,29] |
| Smoking status of the peers | 2 [9,16] | |||
| Peers’dissuasion | 1 [33] | Close relatives and friends’ approval | 1 [16] | |
| Organizational level | Efficient implementation | 3 [27,30,33] | Lack of surveillance | 3 [24,28,30] |
| Convenience of the designative smoking area | 2 [30,33] | Inconvenience of the designative smoking area | 3 [30,32,33] | |
| Private schools (e.g., religious schools) | 1 [31] | Only female bartenders were on duty | 1 [24] | |
| Bars serving predominantly Asian or Irish patrons | 2 [24,28] |
In terms of facilitators, having high levels of knowledge about the harms of smoking and passive smoking [5,9,34] and supportive attitudes towards the smoking bans [5,27,33] were the most commonly reported facilitators of compliance with smoking bans in public places. Smokers who were lighter smokers, without substance abuse, had confidence to quit smoking [23] and those having negative attitudes towards smoking [5] were more likely to be compliant with the smoking bans. People with a history of heart disease and recent dyspnea also tended to be compliant with the bans.
Smokers’ socio-demographic profiles were also associated with their compliance with the bans, but results were mixed. Two studies reported that being older was the facilitator [18,23], while one identified it as a barrier [31]. Additionally, one study indicated that male smokers were more likely to be compliant with the bans than female smokers [17].
3.4.2. Interpersonal Level
Two studies identified that peers’ dissuasion [33] and no parental permission [31] were facilitators. Meanwhile, the smoking status of peers [9,16] and with the approval from close relatives and friends [16] were barriers. People smoking in the same public setting were also identified as a barrier [24,28,29].
3.4.3. Organizational Level
Efficient implementation of the smoking bans in public places, such as enacting documented smoking bans [27] and formulating rewards and punishment measures [30,33], could effectively decrease smoking in public places. However, in the places that lack surveillance, smokers would be more likely to be noncompliant with the bans [30]. Two studies indicated that the presence of ashtrays in public places was associated with more smokers’ smoking post-ban [24,28]. In a study conducted in bars, there were more customers smoking with only female bartenders on duty, for females had less ability or willingness to enforce the bans [24,28].
In places without convenient designative smoking areas, smokers would be more likely to smoke in no-smoking areas when they needed to [30,33]. Studies suggested that a designated smoking place with an apparent sign [30], convenient traffic, and safe circumstances [30,32,33] were associated with less smoking in public places. Features of the public places were also reported to be related to smokers’ compliance. A study in San Francisco found higher smoking rates in bars with Asian and Irish patrons predominantly than those with Latino patrons predominantly [24,28]. Additionally, a study in American campuses suggested that smokers from public schools were less compliant than those from private schools, especially religious schools [31].
4. Discussion
This review brings together studies on the barriers and facilitators of smokers’ compliance with the smoking bans in public places. Although research on this topic remains underdeveloped by including both quantitative and qualitative studies, this review identified a range of factors at the individual-, interpersonal-, and organizational-levels that tobacco researchers, controllers, and policy-makers should consider.
At the individual level, one of the important factors we identified was knowledge. People who were better informed with the harms of smoking and passive smoking and aware of the policy boundaries were more likely to be compliant with the smoking bans in public places than those with a lower level of knowledge [5,9,16,27,32,33,34]. Additionally, the negative attitudes towards smoking cessation and smoking bans are also identified as one of the key barriers of the smokers’ compliance with the smoking bans [5,9,27,32,33,34]. These results emphasize the need for tobacco-related education for the public and the need to increase publicity of the smoking bans.
Another key barrier was nicotine dependence, i.e., heavy smokers who had heavier nicotine dependence and more severe nicotine withdrawal symptoms were more likely to smoke in the public places regardless of the bans [9,16,17,18,24,25,26,29,30,31]. This implies that smoking cessation programs are needed to help heavy smokers deal with the issue of nicotine dependence, and it needs both higher levels (e.g., interpersonal- and organizational-levels) and individual-level of intervention to deal with their noncompliance with the smoking bans.
At the interpersonal level, according the result, not getting the approval from parents or friends is an important facilitator to the smokers’ compliance with the smoking bans [31,33]. Meanwhile, smoking status of peers [9,16] and with the approval from close relatives and friends [20] were the barriers. This indicates that group interventions could be effective on decreasing smoking issues in the public places post-bans, as the impacts of parents, close relatives, and friends on smokers’ smoking behavior are considerable. Additionally, the people around smoking in the same public setting was the barrier [24,28,29]. One of the reasons for this phenomenon is the lack of explicit enforcement of the bans [35].
In organizational level, implementation of smoking bans is identified as an important factor of compliance [24,27,28,30,33]. The compliance can be strengthened through documented bans, strict measures, and powerful surveillance. Provision of ashtrays could be regarded as tacit approval of smoking in public places [24,28], which weaken the enforcement of smoking bans. These results indicate that each measure of implementing smoking bans should be taken into account to improve smokers’ compliance. To deal with this problem, many interventions are needed, including legislation on smoke-free public places that document the responsibilities of the owners and managers (e.g., the owner of a bar or restaurant, and the director of a hospital), surveillance, corresponding condemnatory regulation, and penalties [14].
Another significant factor identified is the convenience of smoking area [30,32,33]. There is no doubt that smoking and environmental tobacco smoke are harmful for health. Thus, no smoking in public places is needed for the health of smokers and non-smokers [36]. We must protect the nonsmokers’ right to health, but we cannot ignore and deprive of the smokers’ right to make their own choices [37]. In addition, as mentioned before, smoking could be physiologically needed sometimes because of the appearance of nicotine dependence or nicotine withdrawal symptoms [17,18,26,32]. This makes compulsory abstinence a painful challenge for smokers [30], particularly for those who cannot leave a non-smoking area for extended periods of time, such as people with physical mobility limitations and hospitalized patients [30]. Therefore, smokers’ rights and their physiological and psychological smoking needs should be considered when implementing smoking bans. Setting convenient smoking area and prompting them to smoke in designated areas will be helpful to improve smokers’ compliance with the bans.
Several studies pointed that compliance with smoking bans differed in different places, and similarity of compliance exists in different groups [9,24,27,28,31]. Although no culture-related variables are identified in the existing literature, the impacts of social norms and culture on the smokers’ compliance with the smoking bans should be considered. For example, there is a Chinese saying that “a cigarette builds a bridge, while wine builds a road” [38]. Cigarette sharing is a common social practice in China [14,39,40], and it may influence their openness to smoke inside recreational settings even if there is a smoking ban [8]. In addition to the three levels of factors discussed above, future studies should explore and address the barriers and facilitators related to social norms and culture. In order to improve the implementation of the smoking bans in public place, the policy-makers and implementers need to make interventions and strategies targeting barriers at multiple levels.
5. Strengths and Limitations
In this study, three levels of barriers and facilitators of smokers’ compliance with smoking bans in public places were summarized. Although we used the most relevant databases (i.e., PubMed MEDLINE, and the Web of Science database), gray literature and some literature in other databases might be missed. Additionally, there is a possible selection bias due to included only English papers and, therefore, might have ruled out some relevant literature in other languages reflecting the impact of culture. Despite these limitations, the findings of this study will be beneficial for the policy-makers and public health researchers to take tailored measures to enhance smokers’ compliance according to these identified factors.
6. Conclusions
This synthesis of the literature provided evidence of the identified barriers and facilitators of smokers’ compliance with smoking bans in public places at individual-, interpersonal-, and organizational-levels. At individual level, interventions targeting smoking-related knowledge and attitudes towards smoking cessation and smoking bans should be prioritized. At the interpersonal level, researchers and interveners could plan group interventions, as the impact of close family members, relatives, and friends on smokers’ smoking behaviors are considerable. At the organizational level, the priority should be stricter enforcement of the existing bans and improvement of the convenience of designative smoking areas. More studies are needed to explore and address the barriers and facilitators related to social norms and culture. It will be beneficial for the policy-makers, tobacco researchers, and controllers to consider interventions on the multiple levels of factors to enhance smokers’ compliance with smoking bans in public places.
Acknowledgments
This work was supported by a grant from the China Medical Board (No. CMB-14-188.). The founding sponsors had no role in the study design; in the search, screening and evaluation of articles, and in the writing of the manuscript.
Supplementary Materials
The following are available online at www.mdpi.com/1660-4601/13/12/1228/s1, Search strategy, Quantitative studies, Qualitative studies, Table S1: Breakdown of quality appraisal markings for 14 articles reporting on studies using quantitative methods, Table S2: Breakdown of quality appraisal markings for 10 articles reporting on studies using qualitative methods.
Author Contributions
Li Zhou and Shuiyuan Xiao did the study design. Li Zhou and CaiXiao Jiang conducted the search, screening, and evaluation of articles. Li Zhou, Lu Niu, and Hui Jiang drafted the manuscript, and Shuiyuan Xiao provided critical input in the manuscript editing process. All the authors have read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Wang Y., Yang M., Tian L., Huang Z., Chen F., Hu J., Wang F., Chen G., Xiao S. Relationship between caregivers’ smoking at home and urinary levels of cotinine in children. Int. J. Environ. Res. Public Health. 2014;11:12499–12513. doi: 10.3390/ijerph111212499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Öberg M., Jaakkola M.S., Woodward A., Peruga A., Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet. 2011;377:139–146. doi: 10.1016/S0140-6736(10)61388-8. [DOI] [PubMed] [Google Scholar]
- 3.Atlanta G. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. [(accessed on 20 June 2015)]; Available online: https://stacks.cdc.gov/view/cdc/13252/
- 4.Geneva WHO Report on the Global Tobacco Epidemic, 2008—The Mpower Package. [(accessed on 20 June 2015)]. Available online: http://www.who.int/tobacco/mpower/2008/en/
- 5.Nagelhout G.E., Mons U., Allwright S., Guignard R., Beck F., Fong G.T., de Vries H., Willemsen M.C. Prevalence and predictors of smoking in “smoke-free” bars. Findings from the international tobacco control (ITC) Europe surveys. Soc. Sci. Med. 2011;72:1643–1651. doi: 10.1016/j.socscimed.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eadie D., Heim D., Macaskill S., Ross A., Hastings G., Davies J. A qualitative analysis of compliance with smoke-free legislation in community bars in Scotland: Implications for public health. Addiction. 2008;103:1019–1026. doi: 10.1111/j.1360-0443.2008.02217.x. [DOI] [PubMed] [Google Scholar]
- 7.Verdonk-Kleinjan W.M., Rijswijk P.C., de Vries H., Knibbe R.A. Compliance with the workplace-smoking ban in the Netherlands. Health Policy. 2013;109:200–206. doi: 10.1016/j.healthpol.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Frazer K., McHugh J., Callinan J.E., Kelleher C. Impact of institutional smoking bans on reducing harms and secondhand smoke exposure. Cochrane Database Syst. Rev. 2016 doi: 10.1002/14651858.CD011856.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li X., Li Q., Dong L., Sun B., Chen J., Jiang Y., Yang Y., Zhou B., Fong G.T. Risk factors associated with smoking behaviour in recreational venues: Findings from the international tobacco control (ITC) China survey. Tob. Control. 2010;19:i30–i39. doi: 10.1136/tc.2009.031336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rivero L.R., Persson J.L., Romine D.C., Taylor J.T., Toole T.C., Trollman C.J., Au W.W. Towards the world-wide ban of indoor cigarette smoking in public places. Int. J. Hyg. Environ. Health. 2006;209:1–14. doi: 10.1016/j.ijheh.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Tanni S.E., Iritsu N.I., Tani M., de Camargo P.A.B., Sampaio M.G.E., Godoy I., Godoy I. Evaluation of hospitalized patients in terms of their knowledge related to smoking. J. Bras. Pneumol. 2010;36:218–223. doi: 10.1590/s1806-37132010000200010. [DOI] [PubMed] [Google Scholar]
- 12.Frazer K., Callinan J.E., McHugh J., van Baarsel S., Clarke A., Doherty K., Kelleher C. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2016;2:CD005992. doi: 10.1002/14651858.CD005992.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chapman S., Freeman B. Markers of the denormalisation of smoking and the tobacco industry. Tob. Control. 2008;17:25–31. doi: 10.1136/tc.2007.021386. [DOI] [PubMed] [Google Scholar]
- 14.Xiao S., Kohrman M. Anthropology in China’s health promotion and tobacco. Lancet. 2008;372:1617–1618. doi: 10.1016/S0140-6736(08)61361-6. [DOI] [PubMed] [Google Scholar]
- 15.Rzeznicki A., Stelmach I., Kowalska A., Krakowiak J., Zebrowski M., Stelmach W. Complying with the smoking ban by students before and after introducing legislative intervention. Int. J. Occup. Med. Environ. Health. 2015;28:369–378. doi: 10.13075/ijomeh.1896.00273. [DOI] [PubMed] [Google Scholar]
- 16.Lazuras L., Eiser J.R., Rodafinos A. Predicting smokers’ non-compliance with smoking restrictions in public places. Tob. Control. 2009;18:127–131. doi: 10.1136/tc.2008.025841. [DOI] [PubMed] [Google Scholar]
- 17.Sabido M., Sunyer J., Masuet C., Masip J. Hospitalized smokers: Compliance with a nonsmoking policy and its predictors. Prev. Med. 2006;43:113–116. doi: 10.1016/j.ypmed.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 18.Rigotti N.A., Arnsten J.H., McKool K.M., Wood-Reid K.M., Pasternak R.C., Singer D.E. Smoking by patients in a smoke-free hospital: Prevalence, predictors, and implications. Prev. Med. 2000;31:159–166. doi: 10.1006/pmed.2000.0695. [DOI] [PubMed] [Google Scholar]
- 19.Goel S., Ravindra K., Singh R.J., Sharma D. Effective smoke-free policies in achieving a high level of compliance with smoke-free law: Experiences from a district of north India. Tob. Control. 2014;23:291–294. doi: 10.1136/tobaccocontrol-2012-050673. [DOI] [PubMed] [Google Scholar]
- 20.Glanz K., Rimer B.K., Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. John Wiley & Sons; Hoboken, NJ, USA: 2008. pp. 465–482. [Google Scholar]
- 21.Sallis J.F., Owen N., Fisher E.B. Twenty: Ecological Models of Health Behavior. Jossey-Bass; San Francisco, CA, USA: 2008. [Google Scholar]
- 22.Kmet L.M., Lee R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. Institute of Health Economics; Edmonton, AB, Canada: 2004. [Google Scholar]
- 23.Emmons K.M., Cargill B.R., Hecht J., Goldstein M., Milman R., Abrams D.B. Characteristics of patients adhering to a a hospital’s no-smoking policy. Prev. Med. 1998;27:846–853. doi: 10.1006/pmed.1998.0368. [DOI] [PubMed] [Google Scholar]
- 24.Moore R.S., Lee J.P., Martin S.E., Todd M., Chu B.C. Correlates of persistent smoking in bars subject to smokefree workplace policy. Int. J. Environ. Res. Public Health. 2009;6:1341–1357. doi: 10.3390/ijerph6041341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parks T., Wilson C.V., Turner K., Chin J.W. Failure of hospital employees to comply with smoke-free policy is associated with nicotine dependence and motives for smoking: A descriptive cross-sectional study at a teaching hospital in the United Kingdom. BMC Public Health. 2009;9:238. doi: 10.1186/1471-2458-9-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lacchetti C., Cohen J., Ashley M.J., Ferrence R., Bull S., de Groh M., Pederson L. Is nicotine dependence related to smokers’ support for restrictions on smoking? Nicotine Tob. Res. 2001;3:257–260. doi: 10.1080/14622200110050475. [DOI] [PubMed] [Google Scholar]
- 27.Borland R., Yong H.H., Siahpush M., Hyland A., Campbell S., Hastings G., Cummings K.M., Fong G.T. Support for and reported compliance with smoke-free restaurants and bars by smokers in four countries: Findings from the international tobacco control (ITC) four country survey. Tob. Control. 2006;15:iii34–iii41. doi: 10.1136/tc.2004.008748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moore R.S., Lee J.P., Antin T.M.J., Martin S.E. Tobacco free workplace policies and low socioeconomic status female bartenders in San Francisco. J. Epidemiol. Community Health. 2006;60:ii51–ii56. doi: 10.1136/jech.2005.045591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Irvin V.L., Hofstetter C.R., Nichols J.F., Chambers C.D., Usita P.M., Norman G.J., Kang S., Hovell M.F. Compliance with smoke-free policies in Korean bars and restaurants: A descriptive analysis in California. Asian Pac. J. Cancer Prev. 2015;16:1083–1089. doi: 10.7314/APJCP.2015.16.3.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shopik N.A., Schultz A.S., Nykiforuk C.I., Finegan B.A., Kvern M.A. Impact of smoke-free hospital grounds policies: Patient experiences and perceptions. Health Policy. 2012;108:93–99. doi: 10.1016/j.healthpol.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Galan I., Diez-Ganan L., Mata N., Gandarillas A., Cantero J.L., Durban M. Individual and contextual factors associated to smoking on school premises. Nicotine Tob. Res. 2012;14:495–500. doi: 10.1093/ntr/ntr174. [DOI] [PubMed] [Google Scholar]
- 32.Jancey J., Bowser N., Burns S., Crawford G., Portsmouth L., Smith J. No smoking here: Examining reasons for noncompliance with a smoke-free policy in a large university. Nicotine Tob. Res. 2014;16:976–983. doi: 10.1093/ntr/ntu012. [DOI] [PubMed] [Google Scholar]
- 33.Russette H.C., Harris K.J., Schuldberg D., Green L. Policy compliance of smokers on a tobacco-free university campus. J. Am. Coll. Health. 2014;62:110–116. doi: 10.1080/07448481.2013.854247. [DOI] [PubMed] [Google Scholar]
- 34.Lazuras L., Zlatev M., Rodafinos A., Eiser J.R. Smokers’ compliance with smoke-free policies, and non-smokers’ assertiveness for smoke-free air in the workplace: A study from the Balkans. Int. J. Public Health. 2012;57:769–775. doi: 10.1007/s00038-012-0338-0. [DOI] [PubMed] [Google Scholar]
- 35.Hovell M.F., Hughes S.C. The behavioral ecology of secondhand smoke exposure: A pathway to complete tobacco control. Nicotine Tob. Res. 2009;11:1254–1264. doi: 10.1093/ntr/ntp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baker F., Ainsworth S.R., Dye J.T., Crammer C., Thun M.J., Hoffmann D., Repace J.L., Henningfield J.E., Slade J., Pinney J., et al. Health risks associated with cigar smoking. JAMA. 2000;284:735–740. doi: 10.1001/jama.284.6.735. [DOI] [PubMed] [Google Scholar]
- 37.Cokkinides V., Bandi P., Ward E., Jemal A., Thun M. Progress and opportunities in tobacco control. CA Cancer J. Clin. 2006;56:135–142. doi: 10.3322/canjclin.56.3.135. [DOI] [PubMed] [Google Scholar]
- 38.Ma S.J., Wang J.F., Mei C.Z., Xu X.F., Yang G.H. Passive smoking in China: Contributing factors and areas for future interventions. Biomed. Environ. Sci. 2007;20:420–425. [PubMed] [Google Scholar]
- 39.Hu M., Rich Z.C., Luo D., Xiao S. Cigarette sharing and gifting in rural China: A focus group study. Nicotine Tob. Res. 2012;14:361–367. doi: 10.1093/ntr/ntr262. [DOI] [PubMed] [Google Scholar]
- 40.Ceraso M., McElroy J.A., Kuang X., Vila P.M., Du X., Lu L., Ren H., Qian N., Jorenby D.E., Fiore M.C. Smoking, barriers to quitting, and smoking-related knowledge, attitudes, and patient practices among male physicians in China. Prev. Chronic Dis. 2009;6:A06. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.