Abstract
Host-directed therapies (HDTs) constitute promising alternatives to traditional therapy that directly targets the pathogen but is often hampered by pathogen resistance. HDT could represent a new treatment strategy for leishmaniasis, a neglected tropical disease caused by the obligate intracellular parasite Leishmania. This protozoan develops exclusively within phagocytic cells, where infection relies on a complex molecular interplay potentially exploitable for drug targets. We previously identified naloxonazine, a compound specifically active against intracellular but not axenic Leishmania donovani. We evaluated here whether this compound could present a host cell-dependent mechanism of action. Microarray profiling of THP-1 macrophages treated with naloxonazine showed upregulation of vATPases, which was further linked to an increased volume of intracellular acidic vacuoles. Treatment of Leishmania-infected macrophages with the vATPase inhibitor concanamycin A abolished naloxonazine effects, functionally demonstrating that naloxonazine affects Leishmania amastigotes indirectly, through host cell vacuolar remodeling. These results validate amastigote-specific screening approaches as a powerful way to identify alternative host-encoded targets. Although the therapeutic value of naloxonazine itself is unproven, our results further demonstrate the importance of intracellular acidic compartments for host defense against Leishmania, highlighting the possibility of targeting this host cell compartment for anti-leishmanial therapy.
Author Summary
Leishmaniasis is a poverty-related disease threatening 350 million people throughout the world. It is caused by the protozoan parasite Leishmania, a digenetic organism that switches from an extracellular stage in the sand fly vector to an intracellular stage in phagocytes of the vertebrate host. Drugs currently available to treat leishmaniasis are toxic to the patient and drug-resistant parasites are emerging, urging for new therapeutics. A novel strategy to tackle intracellular pathogens entails targeting the host cell, in order to indirectly interfere with pathogens growth. Here we analysed the mechanism of action of naloxonazine, a compound previously shown to specifically affect the intracellular amastigote stage of Leishmania. We show that this compound affects acidic compartments of macrophages and that these naloxonazine-induced modifications are responsible for Leishmania intracellular growth inhibition. Even though the therapeutic potential of naloxonazine itself is not proven, our results reveal the possibility of targeting host cell intracellular acidic compartments for anti-leishmanial therapy.
Introduction
Protozoan parasites of the genus Leishmania are the causative agents of a wide variety of diseases ranging from self-healing or severe mucocutaneous lesions to a visceral disease which is lethal in the absence of treatment. Leishmaniasis is one of the most significant neglected tropical diseases, with an estimated 12 million people infected. Leishmania parasites have a digenetic life cycle; switching from an insect vector in which parasites dwell as extracellular promastigotes, to a mammalian host, where parasites reside exclusively intracellulary (intramacrophage amastigote stage).
Pentavalent antimonials (SbV) like sodium stibogluconate (SSG) have been the first-line treatment against leishmaniasis for several decades but their clinical value has become compromised by increasing treatment failure and the emergence of resistant parasites. This concern is particularly important in the Indian subcontinent where visceral leishmaniasis (VL) caused by Leishmania donovani is endemic and where most VL cases occur [1]. Current treatment alternatives consist of amphotericin B, miltefosine or paromomycin (in mono- or combination therapy) but these compounds also have drawbacks including cost, toxicity or decreased efficacy after a few years of use [2].
Although the mechanism of action of these compounds is not fully understood, they are all known to target Leishmania components, therefore directly interfering with parasite growth: amphotericin B forms a complex with ergosterol, the main sterol of Leishmania cellular membrane, leading to formation of aqueous pores and increased membrane permeability [3]; miltefosine has been shown to inhibit the parasite cytochrome c oxidase and to cause apoptosis-like processes in L. donovani [4]; and paromomycin is an aminoglycoside antibiotic that inhibits protein synthesis in Leishmania with low host cell toxicity [5]. SbV on the other hand, has been shown to target both the parasite and the host cell: SbV is reduced to trivalent antimony (SbIII), which directly alters the parasite redox metabolism and antioxidant defense system, but SbV itself also indirectly affects parasite survival by increasing host cell production of toxic oxygen and nitrogen intermediates, thereby creating additional oxidative and nitrosative stress upon SbIII-sensitized parasites [6]. Antimonial anti-leishmanial activity is thus partly indirect, targeting host cell pathway(s) that consequently affect Leishmania intracellular development.
Targeting host cell pathways to interfere with the intracellular development of pathogens is a strategy increasingly investigated for antimicrobial therapy that might bring novel therapeutic approaches in a context of increased treatment failure and poor alternatives [7,8]. Following this line, a recent high-throughput screening campaign against kinetoplastids at GlaxoSmithKline identified several compounds associated with human proteins with no known homologs in kinetoplastids, highlighting the possibility of targeting host-pathogen interactions[9].
Here we report the host-dependent anti-leishmanial activity of naloxonazine, a mu-opioid receptor (MOR) antagonist. This compound was first identified in a high-throughput screen against Leishmania donovani intracellular amastigotes [10]. We now show that it affects host cell intracellular compartments thereby inhibiting Leishmania establishment in the phagolysosomal vacuole.
Methods
Parasite strains, culture conditions and compounds
Parasite strains used in this study included L. donovani 1S2D (MHOM/SD/62/1S-cl2D), L. donovani 1S2D expressing the enhanced green fluorescent protein (eGFP) and two L. donovani clones of clinical isolates from the Terai endemic region in Nepal (MHOM/NP/02/BPK282/0cl4 and MHOM/NP/03/BPK275/0cl18 respectively susceptible and resistant to SSG and further designated SSG-S BPK282 and SSG-R BPK275). Promastigotes were maintained at 26°C in hemoflagellate modified Eagles’s medium (HOMEM) supplemented with 20% Foetal Bovine Serum (FBS). Differentiation of promastigotes into axenic amastigotes was achieved as described previously [11]. THP-1 cells (human acute monocytic leukemia cell line–ATCC TIB202) were grown in RPMI supplemented with 10% FBS and 50 μM 2-mercaptoethanol at 37°C in 5% CO2. For Leishmania infections, THP-1 cells were treated with 0.1 μM phorbol myristate acetate (PMA, Sigma) at 37°C for 48 h to achieve differentiation into adherent, non-dividing macrophages. Cells were washed and incubated with complete RPMI medium containing stationary phase L. donovani promastigotes at a macrophage/promastigote ratio of 1/10. After 4 h incubation at 37°C, non-internalized promastigotes were removed by 3 successive washes with PBS and incubated with naloxonazine, naloxone, β-funaltrexamine, CTOP, endomorphine, DAMGO, sinomenine, concanamycin A (all purchased from Sigma) or imatinib (Cell Signaling Technology) for 24 to 72 h. Half maximal inhibitory concentrations (GI50) were determined using a high-content imaging assay as described previously [10]. Briefly, compounds were serially diluted 3-fold in DMSO, with final assay concentrations ranging from 50 μM to 0.02 μM (1% final concentration of DMSO), 2 μM amphotericin B and 1% DMSO were used as positive and negative controls respectively. For confocal microscopy, infected cells were washed with PBS, fixed for 30 minutes with 4% formaldehyde, rinsed again with PBS and stained with 4’,6’-diamidino-2-phenylindole (DAPI 300 nM). Images were acquired with an LSM 700 Zeiss confocal microscope.
Evaluation of naloxonazine stability by LC-MS/MS
20 μM naloxonazine was incubated for 50 h in RPMI 10% FBS- 50 μM 2-mercaptoethanol with or without THP-1 cells at a concentration of 106 cells/ml. 100 μl of culture media were collected at different time points (T0; 0,5; 1; 5; 10; 20; 30; 45 and 50 h) and kept frozen. 20 μl of these samples were then mixed with 40 μl cold acetonitrile containing either 2 μM naloxone or 2 μg/mL K777 (N-methylpiperazine-PhehomoPhe-vinylsulfone-phenyl), centrifuged, and 3 μL per sample injected into an API4000 (AB Sciex) LC-MS/MS system and analysed with positive-ion-mode electrospray ionization. A binary mobile phase (A,15% methanol:water; B, 100% methanol:water; both containing 0.1% formic acid, 0.1% ACN and 160 mg/L NH4OAc) was pumped at 0.5 mL/min through a 4.6 x 50 mm, 5 μm, 100 Å pore Kinetex C18 column (Phenomenex). The gradient used was: 0–0.5 min, 0% B; 0.5–3.0 min, linear ramp to 100% B; 3.0–4.0 min, 100% B; 4.0–4.5 min, linear ramp to 0% B; 4.5–7.0 min, 0% B. MS settings were as follows: common settings were temperature = 600°C, GS1 (ion source nebulizer gas) = GS2 (ion source heater gas) = 50 lbf in-2; CUR (curtain gas) = 35 lbf in-2; CAD (collision gas) = 12 lbf in-2; IS (ion spray voltage) = 5500 V; analyte-specific settings for naloxonazine, naloxone and K777, repectively, were DP (declustering potential) = 101 V, 76 V and 56 V; EP (entrance potential) = 13.2 V, 10 V and 10 V; CE (collision energy) = 47 eV, 37 eV and 57 eV; CXP (collision cell exit potential) = 18 V, 14 V and 18 V. The MS/MS transitions used were naloxonazine, m/z 651.5 → 325.3; naloxone, 328.3 → 253.1; K77, 575.5 → 101.3, and retentions were 3.16, 3.03 and 4.43 min, respectively.
siRNA-mediated MOR knock-down
MOR-specific siRNA was purchased from Qiagen (Hs_OPRM1_7 FlexiTube siRNA). THP-1 cells were transfected with 1 μM of siRNA using the Amaxa nucleofector kit V following the manufacturer’s instructions. Control cells were mock transfected in parallel (“mock” control). After nucleofection, THP-1 cells were resuspended in complete RPMI medium (5. 105 cells/ml), treated with PMA for 24 h and infected with stationary phase L. donovani 1S2D promastigotes as described above. Parasite infectivity was assessed 48 h after infection. Down-regulation of MOR mRNA level was analysed 24 h after nucleofection and 48 h after infection by qRT PCR as described below using the following primer sets: MOR fwd: 5’ GGTACTGGGAAAACCTGCTGAAGATCT, rev: 5’ GGTCTCTAGTGTTCTGACGAATTCGAGTGG and 18S rRNA: Fwd 5' ACCGATTGGATGGTTTAGTGAG, Rev 5' CCTACGGAAACCTTGTTACGAC. The relative expression level of MOR was determined based on the Ct value normalized to the Ct value of the reference 18S rRNA. siRNA treated cells were compared to the mock transfected cells.
RNA extraction and microarray
Non-infected, PMA-activated THP-1 cells (5.105 cells/ml, 10 ml) were treated with 10 μM of naloxonazine or 10 μM of naloxone. After 4 h of treatment, compounds were removed by 2 washes with PBS and cells were further incubated 20 h in compound-free RPMI medium. This time-point was chosen to maximize the chances of detecting naloxonazine-induced transcriptional changes while limiting the observation of downstream effects. Total RNA was extracted using TRIzol (Invitrogen) and amplified with the Amino Allyl MessageAmp™ II aRNA Amplification Kit (Ambion) following the manufacturer’s protocol. The monofunctional NHS-ester Cy3 and Cy5 dyes (GE Healthcare Life Sciences) were coupled with 10 μg amplified RNA. The two aRNA pools to be compared were mixed and applied to the Human Exonic Evidence Based Oligonucleotide (HEEBO) array (Stanford Functional Genomics Facility). HEEBO oligonucleotide set consists of 44,544 70mer probes that were designed using a transcriptome-based annotation of exonic structure for genomic loci. Four samples (two from naloxonazine-treated and two from naloxone-treated cells) were competitively hybridized on two individual chips (further called “array1” and “array2”). The hybridization was performed at 63°C for 16 h in a humidified slide chamber containing the labeled probe, 3X SSC, and 0.2% SDS. After hybridization, the hybridization chamber was removed from the 63°C water bath, washed with 0.6X SSC, 0.03% SDS, and then 0.06X SSC. Microarrays were scanned using a GenePix Pro Axon 4000B scanner, data were analysed with the Acuity software (Molecular Devices). Fluorescent data were background adjusted and the ratios of naloxonazine-treated to naloxone-treated data were calculated for each probe set. Sets of genes showing a ratio > 2 were functionally clustered using DAVID [12,13].
qRT-PCR
RNA was extracted as described above, from non-infected THP-1 cells treated with 10 μM of naloxonazine for 4 h and further incubated 20 h in compound-free RPMI medium. cDNA synthesis was done with Transcriptor Reverse Transcriptase (Roche) and a 15-mer oligo(dT) primer from 1 μg of total RNA. qPCRs were run with the SensiMix SYBR no-ROX kit (Bioline) on a LightCycler 480 (Roche). The following primer sets were used: vATPase subunit c (ATP6V0C): Fwd 5' ATGTCCGAGTCCAAGAGC, Rev 5' CTACTTTGTGGAGAGGATGAG; vATPase subunit a (TCIRG1): Fwd 5’ ATCTGGCAGACTTTCTTCAG, Rev 5’ AAGATGCTGGTGGCGCGACT; B-Actin (ACTB): Fwd 5' TCCCTGGAGAAGAGCTACGA, Rev 5' AGCACTGTGTTGGCGTACAG; 18S rRNA: Fwd 5' ACCGATTGGATGGTTTAGTGAG, Rev 5' CCTACGGAAACCTTGTTACGAC. The relative expression levels of vATPase and actin were determined based on the Ct value of each gene normalized to the Ct value of the reference 18S rRNA. Naloxonazine treated cells were compared to untreated cells.
Western blotting
Total protein extracts of THP-1 cells infected with L.d. 1S2D, treated or not with 10 μM of naloxonazine for 24 or 48 h, were prepared in Laemmli sample buffer (Bio Rad) and analysed by SDS-PAGE and western blotting. The equivalent of 105 cells were loaded per well. Membranes were first incubated with an anti-vATPase subunit a3 (rabbit polyclonal anti-TCIRG1, abcam, 1:1000), and an anti-rabbit HRP (1:5000), then stripped with Restore western blot stripping buffer (Thermofisher) and further incubated with an anti α-tubulin (mouse monoclonal, abcam, 1:1000) and an anti-mouse HRP (1:5000). Proteins were detected by chemoluminescence following the manufacturer’s instructions (PierceECL western blotting substrate, Thermofisher). Quantitative densitometry was performed using Image J.
Lysotracker staining
THP-1 cells infected with eGFP-expressing L. donovani were treated or not with 10 μM of naloxonazine, 10 μM of naloxone or 80 nM of concanamycin A for 24 h, or co-treated with either naloxonazine (10 μM) and concanamycin A (80 nM) or naloxone (10 μM) and concanamycin A (80 nM) for 24 h, then stained with 180 nM of the Lysotracker red DND-99 (Life Technologies) for 1 h at 37°C. For microscopy, cells were further stained with 500 nM of the nucleic acid stain Hoechst 33342 (Life Technologies) and images were acquired with an LSM 700 Zeiss confocal microscope. For flow cytometry, Lysotracker red DND-99 stained cells were first trypsinised with TrypLE Select (Invitrogen), washed with PBS and analysed with a BD FACSVerse flow cytometer and the BD FACSSuite software.
Statistical analysis
GraphPad Prism 5 software was used to determine the statistical significance (Two-way ANOVA or t-test as specified in the figure legends).
Ethics statement
Clinical samples were from an already existing collection (B.P. Koirala Institute of Health Sciences in Dharan). All samples were anonymized and their use was approved by the review boards of the Nepal Health Research Council, Kathmandu, the Institute of Tropical Medicine, Antwerp and the Antwerp University.
Results
1- Naloxonazine anti-leishmanial activity is dependent on the presence of the host cell and affects both SSG-R and SSG-S parasites
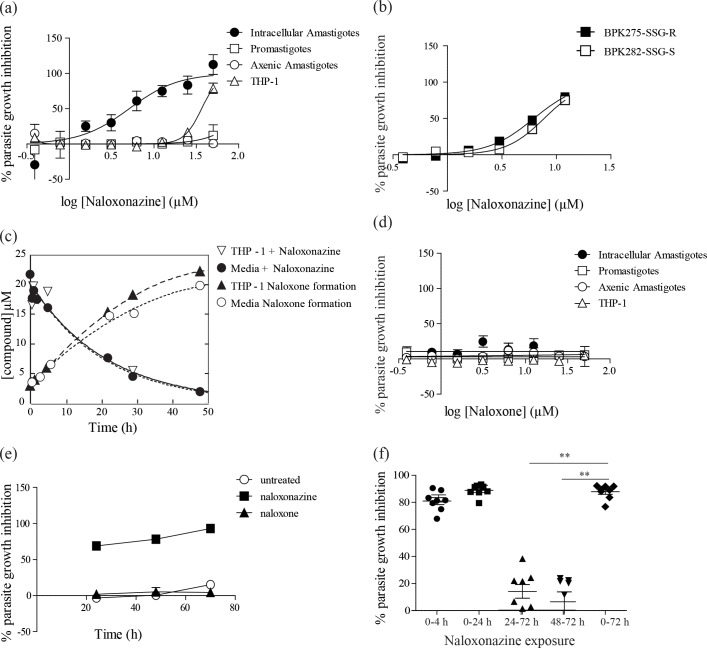
The activity of naloxonazine was tested in vitro against three stages of Leishmania donovani: insect-stage promastigotes, intracellular amastigotes (within the macrophage host cell) and host cell-free axenic amastigotes (an amastigote-like stage obtained from differentiation of promastigotes in vitro in the absence of a host cell). Naloxonazine was shown to be active against the intracellular amastigote stage with a half maximal inhibitory concentration (GI50) of 3,45 μM. It exhibited a reasonable selectivity, with a GI50 of 34 μM against the THP-1 host cell. Remarkably, the compound was inactive against L. donovani promastigotes or axenic amastigotes, indicating the importance of the host cell microenvironment for compound activity (Fig 1A). Naloxonazine was also tested against two L. donovani clinical isolates, one showing susceptibility, the other showing resistance to antimonials (SSG-S and SSG-R strains). The activity of naloxonazine against these isolates was comparable, suggesting that the mechanism of resistance developed against SSG does not affect naloxonazine activity (Fig 1B).
Fig 1. Effect of naloxonazine on Leishmania intracellular growth.
Dose response curve for naloxonazine (a) and naloxone (d) against L. donovani 1S2D intracellular amastigotes, promastigotes, axenic amastigotes and the THP-1 host cell; and dose response curve for naloxonazine against intracellular amastigotes of L. donovani clinical isolates SSG-R or SSG-S (b). Disappearance of naloxonazine and appearance of naloxone during incubation with or without the THP-1 host cell (c). Effect of naloxonazine (10 μM) and naloxone (10 μM) on L. donovani 1S2D intracellular amastigotes growth after 24, 48 and 70 h (e). Data are mean ± SD of three independent experiments. Exposure of L. d. 1S2D-infected THP-1 cells to naloxonazine (10 μM) for different timeframes: 4, 24 or 72 hours (respectively labeled 0–4; 0–24; 0–72) or addition of naloxonazine (10 μM) 24 or 48 hours after infection (labeled 24–72 and 48–72), parasite infectivity was assessed after 72h. Data are pooled from two independent experiments, **p < 0,01 unpaired t-test comparing each condition to the 72 h incubation with naloxonazine (f).
2- Naloxonazine but not naloxone inhibits parasite intracellular growth
The necessity of the host cell presence for naloxonazine’s anti-leishmanial activity might be hypothesized to be linked to the metabolic properties of macrophages, i.e. naloxonazine could be a prodrug dependent on host cell metabolism to gain anti-leishmanial activity. In order to define the exact chemical moiety endowed with anti-leishmanial activity and to evaluate whether the macrophage would metabolize naloxonazine into an active compound, naloxonazine stability during incubation in THP-1 cell medium was evaluated by LC-MS/MS in the presence or absence of THP-1 host cells. Naloxonazine had a half-life of 15 h and was shown to be degraded into naloxone, another MOR antagonist, regardless of the presence of THP-1 macrophages (Fig 1C). Interestingly, naloxone was shown to be inactive against all stages of L. donovani, including the intracellular amastigotes (Fig 1D). Naloxonazine is thus not a prodrug activated by the macrophage host cell but its activity seems inherent, associated with its unperturbed chemical identity.
3- Naloxonazine is active at early stages of infection
The kinetics of naloxonazine activity showed that parasite growth was already inhibited by 70% after 24 h of compound incubation; 95% of growth inhibition was achieved after 72 h incubation (Fig 1E). Remarkably, exposure of infected macrophages to naloxonazine for 4 h, followed by a washing step to remove the compound from the cells and an additional incubation of 70 h, led to the same level of parasite growth inhibition as a 72 h-incubation with the compound (Fig 1F). This observation is in accordance with the degradation time of naloxonazine (Fig 1C). Moreover, delaying addition of naloxonazine to 24 or 48 h after infection reduced its anti-leishmanial effect by 75%, suggesting that naloxonazine is most active at early stages of infection.
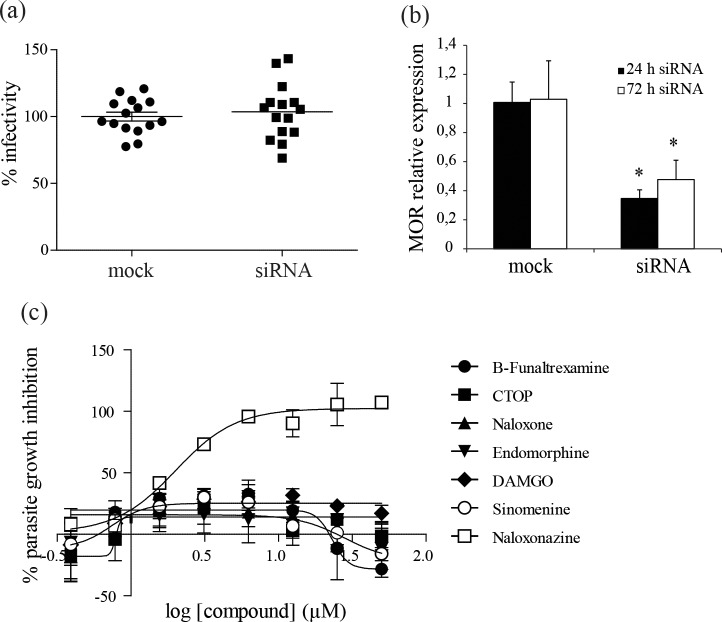
4- Macrophage MOR are not involved in parasite intracellular growth
We hypothesized that naloxonazine anti-leishmanial activity is dependent on its antagonistic effect towards MOR of macrophages. siRNA-mediated knock-down of MOR was therefore carried out in THP-1 cells to evaluate the importance of these receptors for parasite intracellular growth. Fifty percent down-regulation of MOR mRNA was obtained, but this was not accompanied by changes in infection levels (Fig 2A and 2B). The amount or function of the MOR protein was not assessed in the siRNA-treated cells; however, phenocopy of naloxonazine’s effect on L. donovani growth could not be observed with a set of other antagonists or agonists of opioid receptors (Fig 2C), supporting the conclusion that the activity of naloxonazine on Leishmania intracellular growth is independent of opioid receptors.
Fig 2. Importance of opioid receptors for L. donovani intracellular growth.
L.donovani infection of THP-1 cells transfected with MOR-targeting siRNA, infectivity was normalized to mock-transfected controls. Data are pooled from three independent experiments (a). Expression level of MOR was assessed in siRNA-transfected compared to mock-transfected THP-1 cells, 24 h after transfection and 48 h after L. donovani infection (i.e. 72 h after transfection). Data are mean ± SD of three independent experiments, *p < 0,05 two-way ANOVA comparing siRNA-transfected and mock-transfected THP-1 cells (b). Dose response for MOR antagonists naloxonazine, β-funaltrexamine and CTOP, and MOR agonists endomorphine, DAMGO and sinemonine against L. donovani 1S2D intracellular amastigotes. Data are mean ± SD of three independent experiments (c).
5- Naloxonazine affects acidic compartments of the host cell which in turn limit L. donovani intracellular growth
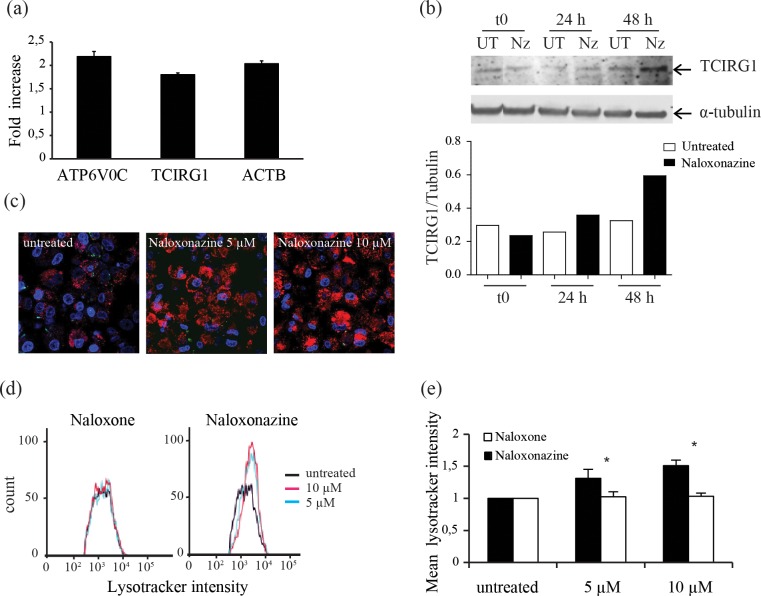
Microarray profiling of THP-1 cells treated with naloxonazine or naloxone was performed to pinpoint host cell pathways differentially affected by the drugs and identify pathways that could be important for Leishmania intracellular growth. A 4 h-compound incubation followed by an additional compound-free incubation of 20 h was chosen, to maximize the chances of detecting naloxonazine-induced transcriptional changes while limiting the observation of downstream effects. Two percent of the probes showed at least two-fold differential gene expression in naloxonazine versus naloxone treated THP-1 cells. These upregulated genes were functionally clustered with the Database for Annotation, Visualization and Integrated Discovery (DAVID [12]). Both the vacuolar H+ ATPase gene family and actin and actin-related genes clusters were perturbed, pointing to a possible effect of naloxonazine on phagolysosome formation or maturation (Table 1). The expression level of two vATPase subunits and actin was also analysed by qRT PCR in naloxonazine-treated compared to untreated cells at the same time point as the one chosen for the microarray experiment. Upregulation of these genes after naloxonazine treatment was confirmed (Fig 3A). Upregulation of vATPase subunit a3 was also established at protein level after 24 and 48 h of treatment (Fig 3B). To test whether naloxonazine could affect the phagolysosome, L. donovani-infected THP-1 cells treated or not with naloxonazine were stained with Lysotracker, a fluorescent acidotropic probe that accumulates in cellular compartments with low internal pH. Stained cells were analysed by confocal microscopy and flow cytometry. The intensity of the Lysotracker signal was increased after naloxonazine treatment, indicating an increased combined volume of acidic vacuoles (Fig 3C, 3D and 3E). These results suggested that naloxonazine influenced the intracellular acidic compartments of the host cell.
Table 1. Vacuolar H+ ATPase gene family members and actin-related genes upregulated in naloxonazine-treated cells.
| genes | name | fold change array1 | fold changearray2 |
|---|---|---|---|
| ATP6V1G2 | ATPase, H+ transporting, lysosomal 13kDa, V1 subunit G2 | 2,03 | 2,14 |
| ATP6AP1 | ATPase, H+ transporting, lysosomal accessory protein 1 | 2,02 | 1,84 |
| ATP6V0D1 | ATPase, H+ transporting, lysosomal 38kDa, V0 subunit d1 | 2,09 | 2,28 |
| ATP6V0C | ATPase, H+ transporting, lysosomal 16kDa, V0 subunit c | 1,72 | 2,25 |
| ATP6V0A4 | ATPase, H+ transporting, lysosomal V0 subunit a4 | 2,11 | 2,55 |
| ATP6V1F | ATPase, H+ transporting, lysosomal 14kDa, V1 subunit F | 1,79 | 2,16 |
| ATP6V1C2 | ATPase, H+ transporting, lysosomal 42kDa, V1 subunit C2 | 1,62 | 2,7 |
| ATP9B | ATPase, Class II, type 9B | 2,46 | 2,87 |
| ATP5E | ATP synthase, H+ transporting, mitochondrial F1 complex | 2,15 | 2,05 |
| ATP5G2 | ATP synthase, H+ transporting, mitochondrial F0 complex | 1,93 | 2 |
| ABCC12 | ATP-binding cassette, sub-family C (CFTR/MRP), member 12 | 2,01 | 1,98 |
| TAPBP | TAP binding protein (tapasin) | 2,07 | 2,45 |
| TCIRG1 | T-cell, immune regulator 1, ATPase, H+ transporting, lysosomal | 2,15 | 2,52 |
| ACTB | actin, beta | 3,1 | 3,23 |
| ARPC1B | actin related protein 2/3 complex, subunit 1B, 41kDa | 2,14 | 2,23 |
| ARPC2 | actin related protein 2/3 complex, subunit 2, 34kDa | 1,65 | 2,27 |
| CAPZB | capping protein (actin filament) muscle Z-line, beta | 2,14 | 2,75 |
| CAPZA1 | capping protein (actin filament) muscle Z-line, alpha 1 | 2,27 | 2,65 |
| TMSB10 | thymosin, beta 10 | 1,76 | 2,24 |
| TMSB4 | thymosin, beta 4 | 1,6 | 2,1 |
Fig 3. Effect of naloxonazine on host cell intracellular acidic compartments.
Expression level of vATPase (ATP6V0C and TCIRG1 subunits) and actin (ACTB) after naloxonazine treatment was measured by qRT-PCR on infected THP-1 cells; data are mean ± SD of triplicates from one representative of two experiments (a). Protein levels of vATPase subunit a3 (TCIRG1) in infected macrophages treated with naloxonazine (Nz) for 24 or 48 h (UT = untreated). Protein levels were quantified by densitometry and normalized to the α-tubulin loading control (b). THP-1 cells infected with eGFP-tagged L. donovani (green) treated or not with naloxonazine and stained with Lysotracker (red) and Hoechst 33342 (blue) were analysed by confocal microscopy (c) and flow cytometry (d, e). Data are mean ± SD of two independent experiments each performed with biological triplicates, * p<0,05 two-way ANOVA comparing naloxonazine and naloxone treated cells.
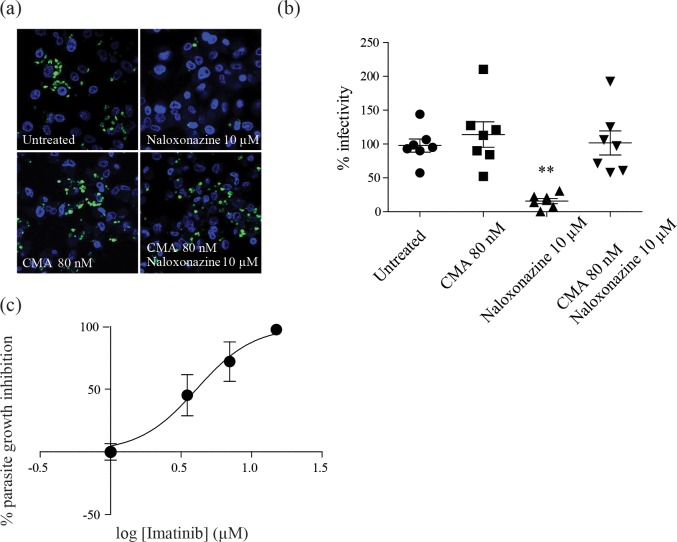
In order to determine if naloxonazine-induced changes in intracellular compartments were responsible for the effect on L. donovani intracellular growth, L. donovani-infected THP-1 cells were treated with both naloxonazine and the vATPase inhibitor concanamycin A. Remarkably, concanamycin A was sufficient to restore normal infection levels in naloxonazine-treated cells, confirming the importance of host cell-acidic compartments for controlling L. donovani intracellular growth (Fig 4A and 4B). To further establish the importance of acidic compartments for Leishmania intracellular growth inhibition, we evaluated the activity of imatinib, an inhibitor of Abelson tyrosine kinase previously shown to trigger intracellular acidification in monocyte-derived macrophages [14, 23]. In agreement with our previous observations, imatinib exhibited anti-leishmanial activity in the low micromolar range (GI50 of 4 μM; Fig 4C).
Fig 4. Host cell acidic compartments affect L. donovani intracellular growth.
THP-1 cells infected with eGFP-tagged L. donovani (green) treated with 10 μM naloxonazine or 80 nM concanamycin A (CMA) or co-treated with both naloxonazine (10 μM) and CMA (80 nM) were stained with DAPI (blue) and analysed by confocal microscopy (a). Infectivity was estimated by manual counting and normalized to untreated cells, **p<0,01 unpaired t-test comparing treated and untreated cells (b). Dose response for imatinib against L. donovani 1S2D intracellular amastigotes (c). Data are representative of three independent experiments.
Discussion
We showed that naloxonazine does not directly target L. donovani but rather interferes with intracellular acidic compartments of the host cell. Upon infection, Leishmania parasites are recognized by phagocytic cells and internalized by phagocytosis in a phagosome/parasitophorus vacuole. During the process of phagocytosis, the phagosome matures through fusion with endosomes and lysosomes, ultimately leading to a highly microbicidal environment. One component of this microbicidal response is the acidification of the phagosome due to the recruitment of the vATPase proton pump to the mature phagosomal membrane [15]. Intracellular pathogens can survive these extreme conditions by arresting phagosomal maturation at an early non-microbicidal stage, developing resistance to the microbicidal arsenal of the phagolysosome, or escaping from the phagosome into the cytosol.
It is well established that Leishmania amastigotes are adapted to the acidic pH found in the parasitophorus vacuole and are able to proliferate under these conditions [16,17]. In contrast, it has been proposed that promastigotes, the parasite stage of the insect vector, delay phagosome maturation to avoid destruction before differentiation into amastigotes [18,19]. Although this hypothesis has been challenged by the observation that promastigote-containing parasitophorus vacuoles do fuse with lysosomes [20], the importance of acidic pH for controlling intracellular Leishmania growth is well recognized. Infection studies in Stat1 deficient mice for instance showed an increased Leishmania intracellular growth that was associated with an increase in phagosomal pH [21].
Our study demonstrated a naloxonazine-induced increased expression of the vATPase transporter as well as an increase of Lysotracker-positive intracellular compartments which was associated to an enhanced capacity of the host cell to control infection. Whether naloxonazine influences the pH of the parasitophorus vacuole or the amount of acidic vacuoles is unclear at this stage. Time-course analysis supported a naloxonazine anti-leishmanial effect at early stages of infection, in accordance with previous observations showing the importance of acidic compartments in the early steps of infection [18, 19]. The microarray analysis performed in this study also showed upregulation of actin and some actin-related genes in naloxonazine-treated cells. However, further investigation is required to assess the importance of actin for the anti-leishmanial activity of naloxonazine.
The molecular pathways affected by naloxonazine that lead to modification of the phagosome are yet to be determined. Naloxonazine is a MOR antagonist [22]; however, albeit such receptors are expressed by macrophages and more specifically by the THP-1 cell line, they could not be linked to Leishmania growth inhibition. Naloxone, β-funaltrexamine or CTOP, other MOR antagonists, were inactive against L. donovani and knock-down of MOR in THP-1 cells did not affect L. donovani intracellular growth. Moreover, naloxonazine is a very potent MOR antagonist (Kd < 2 nM) while its activity against L. donovani is in the micromolar range. These data suggest that the cellular target of naloxonazine in this case is independent of MOR.
Targeting phagolysosome acidification to fight against intracellular pathogens is a strategy that has previously been validated for Mycobacterium tuberculosis, a pathogen that infects macrophages through delayed phagosome maturation. Imatinib, an Abelson tyrosine kinase inhibitor used to treat early chronic myeloid leukemia, was shown to decrease the pH of intracellular compartments which in turn reduced M. tuberculosis intracellular growth in vitro and in vivo (14,23). Whether Abelson tyrosine kinases are involved in the naloxonazine-induced pH decrease of intracellular compartments deserves further investigation.
Host-directed therapies (HDT) are considered an innovative strategy for infectious diseases, given the concern over parasites evolving resistance to current treatments, combined with the recognition of the importance of host determinants for progression of infections. HDTs are receiving increasing attention in treatment of tuberculosis for instance, and are expected to improve treatment outcomes against drug-susceptible as well as multi-drug-resistant strains [24]. Examples of HDTs under evaluation for tuberculosis treatment include anti-inflammatory compounds, statins and imatinib [25]. In antiviral therapy, HDTs have also been raised as interesting alternatives and possible solutions for limiting the emergence of drug resistance [26].
Treatment against leishmaniasis is also jeopardized by increasing treatment failure and drug resistance. Of importance, treatment failure does not necessarily correlate with parasite drug resistance (at least against SSG or miltefosine), highlighting the importance of the host background for treatment outcome in this case [27]. This observation would therefore also argue in favor of HDTs against leishmaniasis. In this context, immunotherapy has received considerable interest in recent years, with the idea of modulating the immune system to achieve a protective response and parasite elimination [28,29]. Combination of immuno- and chemo-therapy is believed to be synergistic, allowing infection control while reducing the threat of drug resistance.
Whether HDTs would be less likely to induce resistance remains an interesting and important question, and for Leishmania at least, the example of SbV raises concern. Indeed, although SbV targets host cell defense pathways, SbV-R parasites have been isolated in the Indian subcontinent, and notably these parasites showed increased infectivity [30]. This ought to raise concern of possibly generating more virulent strains should parasites become resistant to immuno-therapy.
Targeting host-encoded functions unrelated to the immune response but important for parasite invasion or intracellular development provides additional options for HDTs for leishmaniasis and intracellular pathogens in general. This is exemplified by naloxonazine or imatinib and their interference with endocytic components of the host cell.
Although the potential of naloxonazine itself as a therapeutic anti-leishmanial drug is unproven, targeting pathways linked to phagosome acidification remains of great interest. In addition, naloxonazine was as potent against both SSG-R and SSG-S clinical isolates, highlighting the possible benefits of such a drug target for parasites resistant to classic chemotherapy.
Acknowledgments
We would like to thank John Coller and the staff of the Stanford Functional Genomics Facility for supplying us with the human cDNA microarrays used for this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Belgian Science Policy Office (TRIT P7/41 (BV, JCD) and Back-to-Belgium Return grant (GDM)) https://www.belspo.be/belspo/index_fr.stm; the Flemish Fund for Scientific Research (12Q8115N (GDM))www.fwo.be; and the Center for Discovery and Innovation in Parasitic Diseases. GC was supported by the EU/FP7 ERC starting grant (No.282312). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Haldar AK, Sen P, Roy S. Use of antimony in the treatment of leishmaniasis: current status and future directions. Mol Biol Int, 2011;2011:571242 10.4061/2011/571242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Croft SL, Olliaro P. Leishmaniasis chemotherapy-challenges and opportunities. Clin Microbiol Infect. 2011;17(10):1478–83. 10.1111/j.1469-0691.2011.03630.x [DOI] [PubMed] [Google Scholar]
- 3.Singh N, Kumar M, Singh RK. Leishmaniasis: Current status of available drugs and new potential drug targets. Asian Pac J Trop Med. Hainan Medical College; 2012;5(6):485–97. [DOI] [PubMed] [Google Scholar]
- 4.Luque-Ortega JR, Rivas L. Miltefosine (hexadecylphosphocholine) inhibits cytochrome c oxidase in Leishmania donovani promastigotes. Antimicrob Agents Chemother. 2007;51(4):1327–32. 10.1128/AAC.01415-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernández MM, Malchiodi EL, Algranati ID. Differential effects of paromomycin on ribosomes of Leishmania Mexicana and mammalian cells. Antimicrob Agents Chemother. 2011;55(1):86–93. 10.1128/AAC.00506-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pathak MK, Yi T. Sodium stibogluconate is a potent inhibitor of protein tyrosine phosphatases and augments cytokine responses in hemopoietic cell lines. J Immunol. 2001;167(6):3391–7. [DOI] [PubMed] [Google Scholar]
- 7.Jayaswal S, Kamal MA, Dua R, Gupta S, Majumdar T, Das G, et al. Identification of host-dependent survival factors for intracellular Mycobacterium tuberculosis through an siRNA screen. PLoS Pathog. 2010;6(4):e1000839 10.1371/journal.ppat.1000839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwegmann A, Brombacher F. Host-directed drug targeting of factors hijacked by pathogens. Sci Signal. 2008;1(29):re8 10.1126/scisignal.129re8 [DOI] [PubMed] [Google Scholar]
- 9.Peña I, Pilar Manzano M, Cantizani J, Kessler A, Alonso-Padilla J, Bardera AI, et al. New Compound Sets Identified from High Throughput Phenotypic Screening Against Three Kinetoplastid Parasites: An Open Resource. Sci Rep, 2015;5:8771 10.1038/srep08771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Muylder G, Ang KKH, Chen S, Arkin MR, Engel JC, McKerrow JH. A screen against leishmania intracellular amastigotes: Comparison to a promastigote screen and identification of a host cell-specific hit. PLoS Negl Trop Dis. 2011;5(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goyard S, Segawa H, Gordon J, Showalter M, Duncan R, Turco SJ, et al. An in vitro system for developmental and genetic studies of Leishmania donovani phosphoglycans. Mol Biochem Parasitol. 2003;130(1):31–42. [DOI] [PubMed] [Google Scholar]
- 12.Huang DW, Lempicki RA, Sherman BT. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4(1):44–57. 10.1038/nprot.2008.211 [DOI] [PubMed] [Google Scholar]
- 13.Huang DW, Sherman BT, Lempicki R a. Bioinformatics enrichment tools: Paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009;37(1):1–13. 10.1093/nar/gkn923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bruns H, Stegelmann F, Fabri M, Dohner K, van Zandbergen G, Wagner M, et al. Abelson Tyrosine Kinase Controls Phagosomal Acidification Required for Killing of Mycobacterium tuberculosis in Human Macrophages. J Immunol, 2012;189(8):4069–78. 10.4049/jimmunol.1201538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huynh KK, Grinstein S. Regulation of vacuolar pH and its modulation by some microbial species. Microbiol Mol Biol Rev. 2007;71(3):452–62. 10.1128/MMBR.00003-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang KP, Dwyer DM. Leishmania donovani. Hamster macrophage interactions in vitro: cell entry, intracellular survival, and multiplication of amastigotes. J Exp Med. 1978;147:515–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saunders EC, Ng WW, Kloehn J, Chambers JM, Ng M, McConville MJ. Induction of a Stringent Metabolic Response in Intracellular Stages of Leishmania mexicana Leads to Increased Dependence on Mitochondrial Metabolism. PLoS Pathog. 2014;10(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Desjardins M, Descoteaux a. Inhibition of phagolysosomal biogenesis by the Leishmania lipophosphoglycan. J Exp Med. 1997;185(12):2061–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vinet AF, Fukuda M, Turco SJ, Descoteaux A. The Leishmania donovani lipophosphoglycan excludes the vesicular proton-ATPase from phagosomes by impairing the recruitment of Synaptotagmin V. PLoS Pathog. 2009;5(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forestier CL, MacHu C, Loussert C, Pescher P, Späth GF. Imaging host cell-leishmania interaction dynamics implicates parasite motility, lysosome recruitment, and host cell wounding in the infection process. Cell Host Microbe. 2011;9(4):319–30. 10.1016/j.chom.2011.03.011 [DOI] [PubMed] [Google Scholar]
- 21.Späth GF, Schlesinger P, Schreiber R, Beverley SM. A novel role for stat1 in phagosome acidification and natural host resistance to intracellular infection by leishmania majors. PLoS Pathog. 2009;5(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hahn EF, Pasternak GW. Naloxonazine, a potent, long-lasting inhibitor of opiate binding sites. Life Sci. 1982;31(12–13):1385–8. [DOI] [PubMed] [Google Scholar]
- 23.Napier RJ, Rafi W, Cheruvu M, Powell KR, Zaunbrecher MA, Bornmann W, et al. Imatinib-Sensitive Tyrosine Kinases Regulate Mycobacterial Pathogenesis and Represent Therapeutic Targets against Tuberculosis. Cell Host Microbe, Elsevier Inc.; 2011;10(5):475–85. 10.1016/j.chom.2011.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zumla A, Maeurer M. Host-Directed Therapies for Tackling Multi-Drug Resistant Tuberculosis: Learning From the Pasteur-Bechamp Debates: Table 1. Clin Infect Dis, 2015;61(9):1432–8. 10.1093/cid/civ631 [DOI] [PubMed] [Google Scholar]
- 25.Wallis RS, Hafner R. Advancing host-directed therapy for tuberculosis. Nat Rev Immunol, 2015;15(March):1–9. [DOI] [PubMed] [Google Scholar]
- 26.Prussia A, Thepchatri P, Snyder JP, Plemper RK. Systematic approaches towards the development of host-directed antiviral therapeutics. Int J Mol Sci. 2011;12(6):4027–52. 10.3390/ijms12064027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vanaerschot M, Dumetz F, Roy S, Ponte-Sucre A, Arevalo J DJ. Treatment failure in leishmaniasis: drug-resistance or another (epi-) phenotype? Expert Rev Anti Infect Ther [Internet]. 2014; [DOI] [PubMed] [Google Scholar]
- 28.Singh OP, Sundar S. Immunotherapy and targeted therapies in treatment of visceral leishmaniasis: Current status and future prospects. Front Immunol. 2014;5(June):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roatt BM, Aguiar-Soares RDDO, Coura-Vital W, Ker HG, Moreira NDD, Vitoriano-Souza J, et al. Immunotherapy and immunochemotherapy in visceral leishmaniasis: Promising treatments for this neglected disease. Front Immunol. 2014;5(June):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vanaerschot M, Decuypere S, Berg M, Roy S, Dujardin J-C. Drug-resistant microorganisms with a higher fitness–can medicines boost pathogens? Crit Rev Microbiol. 2012;39(July):1–11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.