Abstract
Aim
To investigate patterns of and factors associated with help-seeking behaviors among individuals with diabetes mellitus (DM) and/or serious psychological distress (SPD).
Methods
The analysis was conducted with the California Health Interview Survey (CHIS) 2011–2012 of 40,803 adults. Logistic regression was used to examine the associations between the multiple facilitating/preventing factors and outcome, guided by the Andersen’s Health Care Utilization Model.
Results
The prevalence of DM and SPD were 10.9% and 3.4%, respectively, among participants in the survey. The participants with DM were more likely to experience SPD than those without DM (OR 1.46, 95% CI=1.11–1.91, p=0.006). Participants with combined DM and SPD, the most underserved, were less likely to perceive the need for mental health services and less likely to seek help, compared to those with only SPD. Need factors (SPD status and perceived need) were significantly associated with help-seeking behaviors for mental health, along with predisposing factors (age, gender, obesity, race, and employment), and enabling factors (insurance, English proficiency).
Conclusions
Perceptions about need for seeking help seem to play an important role in receiving mental health services in addition to other predisposing or enabling factors. Identification of these factors may improve clinical outcomes related to DM and SPD.
Keywords: Diabetes mellitus, help-seeking behaviors, perceived needs, serious psychological distress
1. Introduction
The link between diabetes mellitus (DM) and serious psychological distress (SPD) continues to be of concern among healthcare providers in delivering quality of care for individuals with DM [1]. Individuals with DM have been found to be two times more likely to experience depressive symptoms than individuals without DM [2,3]. Besides depression, many individuals with DM are more likely to suffer from SPD caused by anxiety and other mood disorders [4,5]. The crude prevalence of SPD among U.S. adults with DM was twice as high as that among those without DM, according to the data of the Behavioral Factor Surveillance System [6].
The coexistence of DM and SPD results in an increased risk of DM complications [7], higher mortality rates [8,9], and an increased utilization of healthcare services [10]. Individuals with depression had more hospitalization and longer hospital stay which lead to higher healthcare cost [11,12]. Despite the importance of treating SPD in patients with DM, the recognition and treatment of SPD are less than satisfactory, with low detection of depression and other mood disorders [1]. Moreover, studies have reported significant deficiencies in receiving the monitoring and treatment for SPD among patients with DM, even in primary care settings where many of those individuals are treated [1, 13–14]. Additionally, there are many barriers to effective treatment of SPD among individuals with DM. These are reported to include stigma, poor recognition, suboptimal dosing, treatment discontinuation, insurability, financial constraints and fragmented clinical care [1, 4, 12].
To improve the quality of care for DM and comorbid SPD, it could be important to study the factors affecting help-seeking behaviors and identify the barriers in utilizing health services for SPD. Despite extensive research about psychological distress and DM, few studies have investigated factors associated with help-seeking behaviors for mental/emotional health among individuals with DM who experience SPD. The purpose of this study was to assess the prevalence of and factors related to help-seeking behaviors for mental/emotional health and use of alcohol or drugs among adults with DM and SPD. This study also aimed to compare perceived need, help-seeking patterns between individuals with DM and without DM when they experienced SPD.
2. Method
2.1. Study subjects
Our study utilized data from the California Health Interview Survey (CHIS) 2011–2012, a random-digit telephone survey designed to be representative of California’s non-institutionalized population [15]. CHIS were conducted across the two-year cycle and CHIS 2011–2012 was selected as the most recent survey at the initiation of this study. It includes supplemental samples of American Indian and Alaska Native residents of California to increase the representation of those subgroups. The Data Access Center secured the confidentiality of highly sensitive information (e.g., sexual behaviors, mental health treatment) without sharing it with users. Detailed information is available at http://healthpolicy.ucla.edu/chis.
The Andersen’s Health Care Utilization Model is the theoretical framework for this study. The model purports that healthcare utilization (help-seeking behaviors) is dependent on an individual’s propensity to use services (predisposing), ability to access service (enabling), and his/her illness level (need) [16,17].
2.2. Measurements
2.2.1. Outcome factors
Help-seeking behaviors were ascertained with the question, “Did you seek help for your mental/emotional health or for an alcohol/drug problem?” Help-seeking from non-mental health practitioners was determined from “Have you seen your primary care physician or general practitioner for problems with your mental health, emotions, nerves, or your use of alcohol or drugs?” Help-seeking from mental health practitioners was assessed with “Have you seen any other professional, such as a counselor, psychiatrist, or social worker for problems with your mental health, emotions, nerves, or your use of alcohol or drugs?”
Barriers in utilizing services for problems with mental health, emotions, nerves or use of alcohol or drugs were assessed based on the question, “What is the main reason you are no longer receiving treatment?” Reasons of not seeking help were listed as: 1) Concerned about the cost of treatment; 2) Not feel comfortable talking with a professional about your personal problems; 3) Concerned about what would happen if someone found out you had a problem; and 4) Had a hard time getting an appointment, and Yes/No was allowed for each question.
2.2.2. Factors/Covariates
Predisposing factors
Predisposing factors included age, gender, race, marital status, education and working status. Some of the categorical variables that occurred with small frequency were combined in regression analyses. Specifically, educational attainment was coded into four categories: less than high school graduate; high school graduate; some college or college degree; and more. Working status were categorized: full-time employment (21+ hrs/week); part-time (0–20 hrs/week); employed not at work; and unemployed. Height and weight with body mass index (BMI) variables were also included and classified as underweight (BMI<18.5); normal (BMI 18.5–24.9); overweight (BMI 25–29); or obese (BMI≥30).
Enabling factors
Financial factors such as income and insurance status are considered as conditions enabling services utilization [17]. English proficiency was also included.
Need factors
Need factors include perceived need (i.e., how people perceive and experience their own general health, function state, and illness symptoms) and evaluated need (i.e., professional assessments and objective measurements of health status) (16). The assessment of perceived need was ascertained with the question, “Was there ever a time during the past 12 months when you felt that you might need to see a professional because of problems with mental health, emotions, nerves, or your use of alcohol or drugs?”
Evaluated need includes status of DM and SPD. Participants’ DM status was determined by self-report. The question, “Has a doctor ever told you that you have diabetes or sugar diabetes?” was used for known/diagnosed Type-1 or 2 DM. Participants with gestational DM were not included in this study. The presence of SPD was determined by the Kessler-6 scale (K6), developed to monitor the prevalence of nonspecific SPD in general population [18]. SPD was assessed with “During the past 30 days, about how often did you feel psychological distress?” The K6 scale was derived from a series of questions: feeling nervous, hopeless, restless or fidgety, depressed, everything was an effort, or worthless. 5-point Likert scale was used to enumerate the frequency with which the participants experienced these symptoms: none, a little, some, most, and all of the time with 0–5, respectively. Total scores of K6 could range from 0 to 24 and was categorized into no/low (0–6); mild-moderate (7–12); and severe psychological distress (>13) [19].
2.2.3. Other factors/variables
Health risk behaviors such as past year drinking, current smoking, thoughts of suicide, and suicide attempt were observed. Alcohol use was assessed with “Over 12 months, did you have any kind of alcoholic drink?” Smoking cigarettes was assessed with “Do you now smoke cigarettes every day, some days or not at all?” Suicide ideations and attempts were assessed with these questions respectively, “Have you ever seriously thought about committing suicide?” and “Have you ever attempted suicide.” As a health benefit behavior, taking a prescription medication for mental health was assessed based on, “During the past 12 months, did you take any prescription medications, such as an antidepressant or sedative, almost daily for two weeks or more, for an emotional or personal problem?”
2.3. Data analysis
Descriptive statistics for participants classified by the presence of DM and SPD (4 subgroups) were reported. In addition, the descriptive statistics of help-seeking behavior for mental health and risk behaviors by DM status among those participants with SPD were computed. T-test was used for continuous variables and Pearson’s chi-squared test for categorical variables.
To test if predisposing, enabling or need factors are independently associated with help-seeking status (0/1) for SPD, simple and multiple logistic regression analyses were performed for unadjusted and adjusted analyses. Types of factors/confounders were qualitatively grouped as described above and included in the model sequentially; thus there was no attempt to develop a parsimonious model or do model/variable selection. For succinct presentation, we present unadjusted and fully adjusted analyses side-by-side, not each step of sequential adjustments. The regression analyses were summarized by the odds ratio (OR), 95% confidence interval (CI), and p-value.
Complex survey design was accounted for in the analyses. To analyze specific subpopulations, the Taylor series linearization method was used [15]. All statistical analyses were performed in SAS version 9.4.
3. Results
Of the total participants (unweighted N=40,803), the prevalence of DM (combined type-1 and 2 DM) and SPD were 10.9% (n=4,433) and 3.4% (n=1,396), respectively. The participants with DM are more likely to experience SPD than those without DM (OR: 1.46, 95% CI=1.11–1.91, p=0.006).
Table 1 summarizes the socio-demographic characteristics for 4 groups based on DM and SPD statuses (N=40,803). Participants with DM and SPD showed the lowest levels of education, English proficiency, employment and household income among the four groups. Participants who suffered from both DM and SPD were the least likely to be married and insured. They were more likely to be obese (56%), compared with the rest (46, 31, 22%).
Table 1.
Characteristics of participants by DM and SPD status (N=40,803)
| Characteristic | DM with SPD (N=254) | DM without SPD (N=4179) | No DM with SPD (N=1142) | No DM without SPD (N=35228) |
|---|---|---|---|---|
| Age, Mean (SE) | 56.4 (SE=1.04) | 60.1 (SE=0.38) | 43.3 (SE=0.66) | 43.8 (SE=0.05) |
|
| ||||
| Gender | ||||
| Female | 156 (61.4%) | 2144 (51.3%) | 723 (63.3%) | 20431 (58.0%) |
| Male | 98 (38.6%) | 2035 (48.7%) | 419 (36.7%) | 14797 (42.0%) |
|
| ||||
| Height, inches, Mean (SE) | 64.3 (SE=0.56) | 65.9 (SE=0.11) | 65.3 (SE=0.28) | 66.2 (SE=0.03) |
|
| ||||
| Weight, lbs, Mean (SE) | 191.1 (SE=3.85) | 189.7 (SE=1.88) | 167.6 (SE=1.86) | 166.5 (SE=0.31) |
|
| ||||
| BMI, kg/m2, Mean (SE) | 33.0 (SE=0.73) | 30.8 (SE=0.25) | 27.9 (SE=0.42) | 26.8 (SE=0.05) |
|
| ||||
| BMI Group | ||||
| Normal 18.5–24.99 | 37 (14.6%) | 826 (19.8%) | 388 (34.0%) | 14388 (40.8%) |
| Obese 30.0+ | 143 (56.3%) | 1925 (46.1%) | 357 (31.3%) | 7703 (21.9%) |
| Overweight 25.0–29.99 | 74 (29.1%) | 1400 (33.5%) | 366 (32.1%) | 12482 (35.4%) |
| Underweight 0–18.49 | 0 (0.0%) | 28 (0.7%) | 31 (2.7%) | 655 (1.9%) |
|
| ||||
| Race | ||||
| African American | 19 (7.5%) | 309 (7.4%) | 78 (6.8%) | 1678 (4.76%) |
| American Indian/Other | 7 (2.8%) | 97 (2.3%) | 21 (1.8%) | 382 (1.1%) |
| Asian/PI/Native Hawaii | 21 (8.3%) | 457 (10.9%) | 81 (7.1%) | 3498 (9.9%) |
| Hispanic | 55 (21.7%) | 504 (12.1%) | 178 (15.6%) | 3834 (10.9%) |
| White | 152 (59.8%) | 2812 (67.3%) | 784 (68.7%) | 25836 (73.3%) |
|
| ||||
| Marital Status | ||||
| Married/Living With Partner | 94 (37.0%) | 2164 (51.8%) | 426 (37.3%) | 19588 (55.6%) |
| Never Married | 43 (16.9%) | 439 (10.5%) | 299 (26.2%) | 6524 (18.5%) |
| Widowed/Separated/Divorced | 117 (46.1%) | 1576 (37.7%) | 417 (36.5%) | 9116 (25.9%) |
|
| ||||
| Education | ||||
| College Degree | 30 (11.8%) | 1051 (25.2%) | 222 (19.4%) | 11233 (31.9%) |
| High School | 112 (44.1%) | 1908 (45.7%) | 572 (50.1%) | 14565 (41.3%) |
| Less Than High School | 102 (40.2%) | 741 (17.7%) | 282 (24.7%) | 3559 (10.1%) |
| Professional Degree | 10 (3.9%) | 479 (11.5%) | 66 (5.8%) | 5871 (16.7%) |
|
| ||||
| Working Status | ||||
| Employed, Not At Work | n/a | 18 (0.4%) | 7 (0.6%) | 120 (0.3%) |
| Full-Time | 34 (13.4%) | 1037 (24.8%) | 263 (23.0%) | 15902 (45.1%) |
| Part-Time | 7 (2.8%) | 221 (5.3%) | 80 (7.0%) | 2940 (8.4%) |
| Unemployed | 210 (82.7%) | 2903 (69.5%) | 792 (69.4%) | 16266 (46.2%) |
|
| ||||
| Current insured | ||||
| Insured | 224 (88.2%) | 3899 (93.3%) | 923 (80.8%) | 30743 (87.3%) |
| Uninsured | 30 (11.8%) | 280 (6.7%) | 219 (19.2%) | 4485 (12.7%) |
|
| ||||
| English Use/Proficiency | ||||
| Not Well/Not At All | 85 (33.5%) | 697 (16.7%) | 211 (18.5%) | 3808 (10.8%) |
| Speak Only English | 139 (54.7%) | 2768 (66.2%) | 694 (60.8%) | 24399 (69.3%) |
| Very Well/Well | 30 (11.8%) | 714 (17.1%) | 237 (20.8%) | 7021 (19.9%) |
|
| ||||
| Household Income, US $, Mean (SE) | 30875 (SE=3575) | 57039 (SE=1332) | 39233 (SE=1926) | 77779 (SE=550) |
Abbreviations: BMI, body mass index; DM, diabetes mellitus; PI, Pacific Islander; SE, standard error; SPD, serious psychological distress
Table 2 presents comparisons of two groups (with SPD with DM vs. SPD without DM, n=1,396) in terms of degree of SPD, perceived need, help-seeking, medications, health risk behavior, and suicide ideation and attempts. SPD was categorized into SPD 13–18 and SPD 19–24 for the degree of SPD. Degree of SPD is not differential in the 2 groups of those who are already psychologically distressed (p=0.74).
Table 2.
Degree of SPD, perceived need, help-seeking behaviors, prescription/alcohol/cigarettes use, and suicide thought/attempt among participants with SPD with and without DM (N=1,396)
| Characteristic | DM with SPD (N=254) | No DM with SPD (N=1142) | P value |
|---|---|---|---|
| Degree of SPD | 0.74 | ||
| SPD, 13–18 | 165 (65.0%) | 761 (66.6%) | |
| SPD, 19–24 | 89 (35.0%) | 381 (33.4%) | |
|
| |||
| Perceived Need | 0.03 | ||
| No | 115 (45.3%) | 368 (32.2%) | |
| Yes | 139 (54.7%) | 774 (67.8%) | |
|
| |||
| Help-seeking behavior | 0.66 | ||
| Inapplicable | 123 (48.4%) | 528 (46.2%) | |
| Yes | 131 (51.6%) | 614 (53.8%) | |
|
| |||
| Seeking help from GP/PCP | 0.46 | ||
| No | 159 (62.6%) | 692 (60.6%) | |
| Yes | 95 (37.4%) | 450 (39.4%) | |
|
| |||
| Seeking help from Mental health providers | 0.09 | ||
| No | 175 (68.9%) | 706 (61.8%) | |
| Yes | 79 (31.1%) | 436 (38.2%) | |
|
| |||
| Took a prescription medication for mental health | 0.12 | ||
| No | 107 (42.1%) | 528 (46.2%) | |
| Yes | 147 (57.9%) | 614 (53.8%) | |
|
| |||
| Had alcohol past 12 months | 0.003 | ||
| No | 148 (58.3%) | 475 (41.6%) | |
| Yes | 106 (41.7%) | 667 (58.4%) | |
|
| |||
| Suicide thought | 0.39 | ||
| No | 169 (66.5%) | 688 (60.3%) | |
| Yes | 85 (33.5%) | 454 (39.8%) | |
|
| |||
| Suicide attempt | 0.64 | ||
| No | 49 (19.3%) | 241 (21.1%) | |
| Refused/Don’t Know | 169 (66.5%) | 688 (60.3%) | |
| Yes | 36 (14.2%) | 213 (18.7%) | |
|
| |||
| Smoking cigarettes | 0.03 | ||
| Current Smoker | 61 (24.0%) | 365 (32.0%) | |
| Not Current Smoker | 193 (76.0%) | 777 (68.0%) | |
|
| |||
| How many days of excessive drinking? N, Mean (SE) | N=22, 13.7 (SE=8.1) | N=142, 53.9 (SE=12.1) | 0.008 |
Abbreviations: DM, diabetes mellitus; GP, general practitioner; PCP, primary care physician; SE, standard error; SPD, serious psychological distress
Among participants who experienced SPD, 51.6% with DM sought help for mental/emotional health or alcohol/drug use, while 53.8% without DM sought help. 37.4% with DM and SPD sought help from GP/PCP, while 31.1% did from mental health providers. Participants with both DM and SPD were less likely to perceive that they need to see a professional for mental/emotional health or alcohol/drug use, compared to those with SPD only (54.7% vs 67.8%, p=0.02). Interestingly, they were less likely to seek help from mental health providers, although they were more likely to take medication for mental health (57.9% vs 53.8%). Participants with SPD and without DM were more likely to smoke and binge drink. There was no significant difference between individuals with SPD and DM vs. those with only SPD on help-seeking behavior, seeking help from GP/PCP, and suicide ideation and attempts.
Among all participants, 5,849 (14.3%) sought help for mental or emotional health or alcohol/drug problem. In regression analysis (Table 3), among predisposing factors, age (younger), gender (female), race (white), BMI status (obese), education (higher education), and working status (unemployed) showed significant associations with help-seeking. Among enabling factors, participants who had insurance and English proficiency showed significant association with help-seeking. When adjusting for the factors jointly, the associations of help-seeking behavior with age, gender, obesity, race, working status, perceived need, insurance status, language proficiency, and presence of SPD were significant.
Table 3.
Logistic regression of association between predisposing, enabling and need factors and help-seeking status (N= 40,803)
| Unadjusted Odds Ratio | 95% CI | P-value | Adjusted Odds Ratio | 95% CI | P-value | |||
|---|---|---|---|---|---|---|---|---|
| Predisposing factor | ||||||||
|
| ||||||||
| Age | 0.99 | 0.99 | 0.99 | <.001 | 0.99 | 0.99 | 1.00 | 0.004 |
|
| ||||||||
| Gender | ||||||||
| Female Vs Male | 1.68 | 1.51 | 1.87 | <.001 | 1.43 | 1.24 | 1.64 | <.001 |
|
| ||||||||
| BMI Group | ||||||||
| Obese vs. Underweight Or Normal | 1.34 | 1.19 | 1.52 | <.001 | 1.50 | 1.27 | 1.78 | <.001 |
| Overweight vs. Underweight Or Normal | 1.00 | 0.89 | 1.13 | 0.96 | 1.12 | 0.95 | 1.31 | 0.17 |
|
| ||||||||
| Race | ||||||||
| White Vs Other | 1.75 | 1.55 | 1.96 | <.001 | 1.51 | 1.27 | 1.78 | <.001 |
|
| ||||||||
| Marital Status | ||||||||
| Married/Living With Partner Vs Other | 0.71 | 0.64 | 0.79 | <.001 | 0.95 | 0.83 | 1.10 | 0.52 |
|
| ||||||||
| Education | ||||||||
| More Than High School Vs Other | 1.14 | 1.03 | 1.26 | 0.009 | 1.10 | 0.96 | 1.27 | 0.16 |
|
| ||||||||
| Working Status | ||||||||
| Employed Vs Unemployed | 0.69 | 0.63 | 0.77 | <.001 | 0.71 | 0.61 | 0.82 | <.001 |
|
| ||||||||
| Enabling factor | ||||||||
|
| ||||||||
| Current Insured | ||||||||
| Uninsured Vs Insured | 0.61 | 0.52 | 0.71 | <.001 | 0.51 | 0.41 | 0.63 | <.001 |
|
| ||||||||
| Income (Per 1 Level Increase On Ln Scale) | 0.97 | 0.94 | 1.00 | 0.038 | 0.98 | 0.94 | 1.04 | 0.55 |
|
| ||||||||
| English Use/Proficiency | ||||||||
| Not Well/Not At All Vs Speak Only English | 0.39 | 0.31 | 0.49 | <.001 | 0.56 | 0.41 | 0.76 | <.001 |
| Very Well/Well Vs Speak Only English | 0.73 | 0.64 | 0.82 | <.001 | 0.97 | 0.82 | 1.15 | 0.70 |
|
| ||||||||
| Need factor | ||||||||
|
| ||||||||
| Doctor Ever Told Have Diabetes | ||||||||
| Yes Vs No | 1.09 | 0.91 | 1.30 | 0.37 | 1.09 | 0.88 | 1.34 | 0.45 |
|
| ||||||||
| Serious Psychological Distress | ||||||||
| Mild To Moderate Vs No | 4.16 | 3.63 | 4.77 | <.001 | 1.57 | 1.27 | 1.94 | <.001 |
| Serious Vs No | 10.3 | 8.52 | 12.5 | <.001 | 2.31 | 1.75 | 3.05 | <.001 |
|
| ||||||||
| Perceived Need | ||||||||
| Yes Vs No | 32.0 | 28.1 | 36.4 | <.001 | 25.4 | 21.9 | 29.4 | <.001 |
Among need factors, participants who perceived need showed over 20 times larger odds to seek help for mental/emotional health, compared to those who did not perceive need. Participants who suffered from SPD showed 2.3 times of odds to seek help in the adjusted model (95% CI=1.75–3.05, p<0.001). In contrast, the presence of DM was not significantly associated with help-seeking (OR=1.09, 95% CI=0.88–1.34, p=0.45).
Figure 1 describes perceived barriers of 174 participants who did not seek help even when they thought they might need it. The largest proportion of participants were concerned about the cost of treatment (N=74). Some participants did not feel comfortable talking with a professional about their personal problems and some concerned about what would happen if someone found out they had a problem. Some reported that getting appointment is hard.
Figure 1.
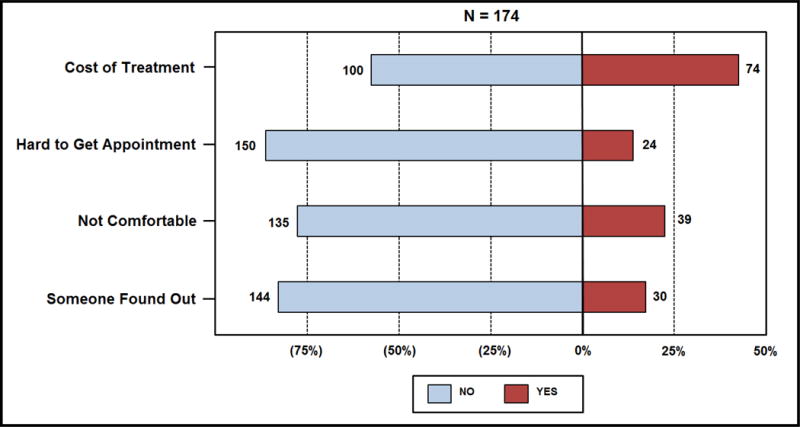
Perceived barriers among participants who did not seek help for emotional health/use of alcohol or drugs
Characteristics of participants with DM and SPD (n=254, as a small but the sickest and most disadvantaged subgroup) were compared further between those who sought help vs. those who did not (Table 4). Non-help-seekers tended to have even lower income ($24,917 vs. $37,497, p=0.06) and less insured (19.5% vs. 4.6%. p<0.001). Among participants who suffered from DM and SPD, race is not a significant factor in seeking help for mental/emotional or alcohol/drug problem while only “insurance” is significant (p<0.0001).
Table 4.
Characteristics for participants with DM and SPD who sought help and those who did not seek help for mental/emotional health or alcohol/drug problem (N=254)
| Characteristic | No (N=123) | Yes (N=131) | P value |
|---|---|---|---|
| Age | 55.9 (SE=1.5) | 56.9 (SE=1.2) | 0.59 |
|
| |||
| BMI, kg/m2 | 33.2 (SE=1.1) | 32.8 (SE=0.97) | 0.79 |
|
| |||
| Height, inches | 63.5 (SE=0.96) | 65.2 (SE=0.64) | 0.17 |
| Weight, lbs | 184.9 (SE=5.6) | 198.0 (SE=6.0) | 0.13 |
|
| |||
| Gender | 0.27 | ||
| Female | 73 (59.4%) | 83 (63.4%) | |
| Male | 50 (40.7%) | 48 (36.6%) | |
|
| |||
| Race | 0.51 | ||
| White | 67 (54.5%) | 85 (64.9%) | |
| Other | 56 (45.5%) | 46 (35.1%) | |
|
| |||
| Marital Status | 0.26 | ||
| Married/Living With Partner | 43 (35.0%) | 51 (38.9%) | |
| Other | 80 (65.0%) | 80 (61.1%) | |
|
| |||
| Education | 0.88 | ||
| More Than High School | 19 (15.5%) | 21 (16.0%) | |
| Other | 104 (84.6%) | 110 (84.0%) | |
|
| |||
| Working Status | 0.65 | ||
| Employed | 25 (20.3%) | 19 (14.5%) | |
| Unemployed | 98 (79.7%) | 112 (85.5%) | |
|
| |||
| Current insured | <.001 | ||
| Insured | 99 (80.5%) | 125 (95.4%) | |
| Uninsured | 24 (19.5%) | 6 (4.6%) | |
|
| |||
| English Use/Proficiency | 0.65 | ||
| Not Well/Not At All | 51 (41.5%) | 34 (26.0%) | |
| Speak Only English | 60 (48.8%) | 79 (60.3%) | |
| Very Well/Well | 12 (9.8%) | 18 (13.7%) | |
|
| |||
| Household Income, US $ | 24917 (SE=3682) | 37497 (SE=5580) | 0.06 |
Abbreviations: BMI, body mass index; DM, diabetes mellitus; PI, Pacific Islander; SE, standard error; SPD, serious psychological distress
4. Discussion
This population-based study demonstrated that among participants with diagnosed DM and SPD, the prevalence of help-seeking behaviors for mental/emotional health and alcohol/drug problem is still low (51.6%). In addition, those with DM and SPD were less likely to seek help from mental health providers for psychological distress than those with only SPD. The present study suggests that need factors played the strongest role in seeking help for mental/emotional health. Particularly, perceived need is the strongest predictor of seeking help − stronger than SPD itself − (OR=32 vs. 10 in the unadjusted models and 25 vs. 2.3 in the adjusted model, all p’s<0.001), while the presence of DM was a weaker or not predictor.
Compared with previous findings [20], the prevalence of diagnosed DM in California has increased from 6.9% to 10.9% of CHIS 2007 vs. 2011–2012, and the prevalence of SPD among participants with DM is 5.9%, almost double that among participants without DM (3.1%). This confirms that the prevalence of DM has been rising rapidly and SPD is more common among people with DM. However, our findings indicated that participants with SPD and DM were less likely to perceive that they needed a mental health professional’s help, whereas they tended to take a prescription medication for mental health more than those with only SPD.
Perceived need among individuals with DM who experience SPD is not fully understood. Our study showed that women, white, younger age, being obese, higher education, and English proficiency are significantly associated with perceived need for emotional help, in addition to SPD whose strongest association with the outcome is apparent (all p-values <0.001) based on the logistic regression analysis. Self-recognition of need for care has been known to influence the decision to seek help for distress [21, 22, 23]. In the population surveys conducted in Europe, participants who suffered from mental disorder had a higher likelihood of perceiving need for mental healthcare than participants without. Moreover, those who perceived a need for mental healthcare were more likely to use it [24]. Edlund et al [25] also found a correlation between the perceived need and receiving alcohol, drug, and mental health treatment. Our results demonstrated that individuals who perceived a need for mental health services were much more likely to seek help, even after adjusting for many other variables.
Although need factors were the main determinants in help-seeking behaviors, several predisposing or enabling factors showed significant associations. Studies showed associations between age and utilization of healthcare services [26, 27]. In our study, younger participants were more likely to seek help. We found that females were more likely to seek help for SPD, which has also been observed in other studies. The sex difference has been explained by the cultural values and expectations associated with social role as male/female [28]. Among enabling factors, insurance and English proficiency were associated with help-seeking behaviors.
While participants with DM are at risk for SPD, participants with DM did not show higher risk of suicidal ideations or attempt than those without DM. Some other studies, however, found that DM was a significant risk factor for suicidal ideations. A study from Korea (where the prevalence of suicide is relatively high) found that suicidal thoughts were reported by 20.7% of patients with DM and 15.3% of controls (p<0.001) and suicidal attempts by 1.3% of patients with DM and 0.8% of controls (p=0.006) [29]. Another study from Korea also reported that patients with only DM showed a significantly increased risk of suicidal ideations after adjusting for age and sex among four groups based on DM and depression [30].
Our study showed that the subgroup with combined DM and SPD was most vulnerable, with the lowest levels of education, English proficiency, employment, income, and perceived need. Moreover, patients with both SPD and DM who did not seek help are more likely to live in poverty without insurance. These findings highlight the need for intervention that could not only improve the perception of psychological distress among those suffering from DM and SPD but also identify better and easier ways to seek help when they need it. In addition, more attention may be needed in adults with DM and SPD who are non-white, elderly, less educated, and/or unemployed.
This study has several limitations. First, CHIS is a cross-sectional survey so we cannot address causality. Second, all data are based on participants’ self-report. Third, our data do not permit distinction between type-1 and 2 DM, which we hope future studies to address. Finally, CHIS does not ask cultural beliefs, religiosity or spirituality, and perception toward healthcare providers. A better understanding of these factors (normally unavailable in large surveys) may provide crucial information in improving treatment and intervention programs for high at-risk and vulnerable populations. The strengths of our study include: It is a state survey with a large sample size which includes many ethnic groups and weighed samples of Californian with high generalization. We included sensitive data on seeking help for SPD by utilizing confidential data, not commonly available in community settings.
In conclusion, not being able to perceive need for mental health services could be a potential barrier for individuals with DM who are suffering from SPD in obtaining needed services. In addition, perceived need of individuals could be improved through screening and education about SPD and options of treatment and delivery, particularly, the most underserved, harder-to-reach population. Therefore, collaboration between primary care physicians and mental health specialists may improve clinical outcomes and patient-centered approach by helping individuals with DM receive appropriate mental health services in a timely and convenient manner. Primary care physicians and general practitioners need to be more attentive in screening and treating SPD in patients with DM. Improved knowledge of help-seeking behaviors and the associated factors may guide the development of effective prevention and intervention for individuals who are suffering from DM and SPD, who may need help most urgently.
Highlights.
This research utilized confidential data in the California Health Interview Survey (CHIS).
Perceived need is the strongest predictor of seeking help for mental health in this study
Identification of factors affecting help-seeking behaviors may improve clinical outcomes.
Acknowledgments
We thank Ms. Sheryl Ramer, and Ms. Barbara Gugluizza, at Elmhurst Hospital Center for their skillful assistance in conducting the study. We also thank participants, investigators and staff on the CHIS for their important contributions to health research.
Funding
H. Bang was partly supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR000002.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Jinah K. Shin, Psychiatric Department at Elmhurst Hospital in New York, 79-01, Broadway, Elmhurst, NY 11373, USA.
Eduard Poltavskiy, Graduate Group of Epidemiology, Department of Public Health Sciences, School of Medicine, University of California at Davis, Davis, CA, USA.
Tae Nyun Kim, Division of Endocrinology & Metabolism, Department of Internal Medicine, Haeundae Paik Hospital, Inje University School of Medicine, Busan, S. Korea.
Abdullah Hasan, Psychiatric Department at Elmhurst Hospital in New York 79-01, Broadway, Elmhurst, NY 11373, USA.
Heejung Bang, Division of Biostatistics, Department of Public Health Sciences, School of Medicine, University of California at Davis, Davis, CA, USA.
References
- 1.Egede LE, Ellis C. Diabetes and depression: Global perspectives. Diabetes Res Clin Pract. 2010;87:302–312. doi: 10.1016/j.diabres.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 2.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23:1165–1173. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 3.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 4.Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Prevalence of anxiety in adults with diabetes. J Psychosomat Res. 2002;53:1053–1060. doi: 10.1016/s0022-3999(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 5.Huang CJ, Chiu HC, Lee MH, Wang SY. Prevalence and incidence of anxiety disorders in diabetic patients: a national population-based cohort study. Gen Hosp Psychiatry. 2011;33:8–15. doi: 10.1016/j.genhosppsych.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Li C, Ford ES, Zhao G, Strine TW, Dhingra S, Barker L, et al. Association between diagnosed diabetes and serious psychological distress among U.S. adults: the Behavioral Risk Factor Surveillance System, 2007. Int J Public Health. 2009;54:43–51. doi: 10.1007/s00038-009-0006-1. [DOI] [PubMed] [Google Scholar]
- 7.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of Depression and Diabetes Complications: A Meta-Analysis. Psychosomatic Medicine. 2001;63:619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Norris SL, Gregg EW, Cheng YJ, Gregg EW, Cheng YJ, et al. Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol. 2005;161:652–660. doi: 10.1093/aje/kwi089. [DOI] [PubMed] [Google Scholar]
- 10.Subramaniam M, Sum CF, Pek E, Stahl D, Verma S, Liow PH, et al. Comorbid depression and increased health care utilisation in individuals with diabetes. Gen Hosp Psychiatry. 2009;31:220–224. doi: 10.1016/j.genhosppsych.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Dismuke CE, Egede LE. Association of serious psychological distress with health services expenditures and utilization in a national sample of US adults. Gen Hosp Psychiatry. 2011;33:311–317. doi: 10.1016/j.genhosppsych.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Egede LE, Zheng D, Simpson K. Comorbid Depression is Associated With Increased Health Care Use and Expenditures in Individuals With Diabetes. Diabetes Care. 2002;25:464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 13.Li C, Ford ES, Zhao G, Balluz LS, Berry JT, Mokdad AH. Undertreatment of Mental Health Problems in Adults With Diagnosed Diabetes and Serious Psychological Distress: The Behavioral Risk Factor Surveillance System, 2007. Diabetes Care. 2010;33:1061–1064. doi: 10.2337/dc09-1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vamos EP, Mucsi I, Keszei A, Kopp MS, Novak M. Comorbid depression is associated with increased healthcare utilization and lost productivity in persons with diabetes: A large nationally representative Hungarian population survey. Psychosomatic Medicine. 2009;71:501–507. doi: 10.1097/PSY.0b013e3181a5a7ad. [DOI] [PubMed] [Google Scholar]
- 15.California Health Interview Survey. CHIS 2011–2012 methodology report series: data collection methods. 2014 http://healthpolicy.ucla.edu/chis/design/documents/chis2011-2012_method-1_2014-06-09.pdf (accessed February 1, 2014)
- 16.Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter. J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 17.Andersen RM. Improving access to care in America: individual and contextual indicators. In: Davidson PL, editor. Changing the US Health Care System: Key Issues in Health Services, Policy, and Management. Jossey-Bass; San Francisco, CA: 2001. pp. 3–30. [Google Scholar]
- 18.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for Serious Mental Illness in the General Population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 20.Shin JK, Chiu YL, Choi S, Cho S, Bang H. Serious psychological distress, health risk behaviors, and diabetes care among adults with type 2 diabetes: The California Health Interview Survey 2007. Diabetes Research And Clinical Practice. 2012;95:406–414. doi: 10.1016/j.diabres.2011.10.043. [DOI] [PubMed] [Google Scholar]
- 21.Meadows G, Burgess P, Bobevski I, Fossey E, Harvey C, Liaw ST. Perceived need for mental health care: influences of diagnosis, demography and disability. Psychol Med. 2002;32:299–309. doi: 10.1017/s0033291701004913. [DOI] [PubMed] [Google Scholar]
- 22.Mojtabai MR, Olfson M, Mechanic D. Perceived Need and Help-Seeking in Adults With Mood, Anxiety, or Substance Use Disorders. Arch Gen Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 23.Mechanic D. Removing Barriers To Care Among Persons With Psychiatric Symptoms. Health Aff. 2002;21:137–147. doi: 10.1377/hlthaff.21.3.137. [DOI] [PubMed] [Google Scholar]
- 24.Codony M, Alonso J, Almansa J, Bernert S, Girolamo GD, Graaf RD, et al. Perceived Need for Mental Health Care and Service Use Among Adults in Western Europe: Results of the ESEMeD Project. Psychiatric Services. 2009;60:1051–1058. doi: 10.1176/ps.2009.60.8.1051. [DOI] [PubMed] [Google Scholar]
- 25.Edlund MJ, Unützer J, Curran GM. Perceived need for alcohol, drug, and mental health treatment. Soc Psychiat Epidemiol. 2006;41:480–487. doi: 10.1007/s00127-006-0047-1. [DOI] [PubMed] [Google Scholar]
- 26.Hochhausen L, Le HN, Perry DF. Community-Based Mental Health Service Utilization Among Low-Income Latina Immigrants. Community Ment Health J. 2009;47:14–23. doi: 10.1007/s10597-009-9253-0. [DOI] [PubMed] [Google Scholar]
- 27.Surood S, Lai DW. Impact of culture on use of Western health services by older South Asian Canadians. Can J Public Health. 2010;101:176–180. doi: 10.1007/BF03404367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dhingra S, Zack M, Strine T, Pearson W, Balluz L. Determining Prevalence and Correlates of Psychiatric Treatment With Andersen’s Behavioral Model of Health Services Use. Psychiatr Serv. 2010;61:524–28. doi: 10.1176/ps.2010.61.5.524. [DOI] [PubMed] [Google Scholar]
- 29.Chung JH, Moon K, Kim DH, Min JW, Kim TH, Hwang HJ. Suicidal ideation and suicide attempts among diabetes mellitus: The Korea National Health and Nutrition Examination Survey (KNHANES IV, V) from 2007 to 2012. J Psychosom Res. 2014;77:457–461. doi: 10.1016/j.jpsychores.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 30.Han SJ, Kim HJ, Choi YJ, Lee KW, Kim DJ. Increased risk of suicidal ideation in Korean adults with both diabetes and depression. Diabetes Res Clin Pract. 2013;101:e14–e17. doi: 10.1016/j.diabres.2013.06.012. [DOI] [PubMed] [Google Scholar]


