Abstract
Introduction
A woman’s health practices during pregnancy are associated with maternal and neonatal outcomes. Yet limited research has examined predictors of a woman’s engagement in favorable health practices, particularly in pregnant women at greatest risk for adverse outcomes. We examined the role of mental health on engagement in favorable health practices during pregnancy in a sample of pregnant, low-income, predominantly African American women.
Methods
A convenience sample of pregnant women was obtained from 3 obstetric clinics within a large Mid-Atlantic academic health system. Pregnant women (N = 166) completed measures of depression, social support, and engagement in favorable health practices during their second trimester. Six domains of health practices (ie, balance of rest and exercise, safety measures, nutrition, substance use, health care access, access to pregnancy-related information) were assessed by the Health Practices in Pregnancy Questionnaire-II. Multiple linear regression was used to examine predictors of engagement in favorable health practices.
Results
Fifty-nine percent of the study participants experienced depressive symptomatology during pregnancy. Multivariate linear regression modeling demonstrated that increased depressive symptoms, decreased social support, young age, and prepregnancy overweight or obesity were significant predictors of nonengagement in favorable health practices during pregnancy.
Discussion
Findings suggest that pregnant women with poor mental health (eg, depressive symptomatology, poor social support) and specific sociodemographic characteristics (eg, young age, prepregnancy overweight or obesity) were less likely to engage in favorable health practices during pregnancy. Health care providers are uniquely positioned to assess a woman’s mental health and related indicators to optimize pregnancy and neonatal outcomes.
Keywords: African American, antenatal depression, health practices, obesity, pregnancy, social support
INTRODUCTION
Pregnancy represents a critical time period during which maternal health practices contribute significantly to maternal, neonatal, and early childhood outcomes. Favorable health practices associated with positive outcomes include maintaining a health prepregnancy weight, gaining an appropriate amount of weight during pregnancy, consuming a variety of foods with adequate intake of specific nutrients, engaging in regular physical activity, limiting alcohol consumption, avoiding tobacco and illicit substance use, taking appropriate vitamin and mineral supplementation, and using safe food handling practices.1 Despite the recognition that a woman’s health practices during pregnancy are important for maternal and fetal health, as well as neonatal outcomes, there is limited research examining predictors of favorable health practices during pregnancy. It is important to better understand factors that influence a woman’s ability to engage in favorable health practices during pregnancy, particularly among women at highest risk for poor outcomes, in an effort to best support them in achieving a healthy pregnancy. Thus, the purpose of the current study was to examine predictors of a woman’s engagement in favorable health practices during pregnancy.
Perinatal depression affects an estimated 7% to 20% of women with rates as high as 35% to 40% in low-income and minority women.2,3 Limited research examining perinatal mental health and engagement in healthy practices has largely focused on specific health practices such as use of alcohol, tobacco use, and illicit substances. Depression in pregnancy has been associated with alcohol use, tobacco use, and substance use.1,4–6 In a study of low-income, predominantly African American women, depressive symptoms during pregnancy were associated with an increased risk of cigarette smoking.7 In addition, poor health practices such as smoking, substance use, or alcohol use may exacerbate depressive symptoms and vice versa.8–10 While an important contribution, knowledge of individual health practices limits our understanding of the contribution of mental health to a more comprehensive picture of a woman’s ability to engage in favorable health practices.
A growing body of research suggests there is a relationship between poor antenatal mental health and adverse maternal, neonatal, and early childhood outcomes.11,12 There are several plausible mechanisms by which depression may contribute to adverse perinatal outcomes. First, evidence supports depression as a stressor leading to changes in the hypothalamic-pituitary-adrenal (HPA) axis with resultant inflammation and dysregulation of cortisol. These changes may lead to early contractions and preterm birth.12,13 Maternal obesity also is associated with an increased risk of adverse maternal and fetal outcomes.14 Maternal obesity and depression are individually associated with an increased risk of poor pregnancy outcomes, and research suggests their combined presence has the greatest impact on the risk of adverse neonatal outcomes.15 A recent systematic review was conducted to summarize the relation between psychological factors and gestational weight gain. Synthesized results from 35 studies did not find an association between gestational weight gain and depressive symptoms. Findings were in contrast to evidence from studies of nonpregnant women, which supports an association between depression and weight,16,17 although many studies of this association have been underpowered.16 Importantly, studies examining the link between depression and gestational weight gain are limited by small sample sizes and participants with mild depressive symptomatology.18 Finally, limited research suggests depression is associated with an increase in tobacco use and illicit substance use during pregnancy; thus, the relation between depression and adverse neonatal outcomes may be mediated by harmful substance use.19
Pregnancy represents a critical time period in that poor health practices are clearly associated with short-term and long-term health consequences for both woman and child. There is a significant need for an enhanced understanding of predictors of health practices that extends beyond examining substance use. Illuminating these relationships is important not only to enhance our understanding of the factors that predict these behaviors but also to identify factors that might be amenable to interventions. Most pregnant women access health care during the perinatal period, making it an opportune time to assess facilitators and barriers to optimal health practices.
METHODS
Sample
A convenience sample of pregnant women was recruited from 3 obstetric clinics in Baltimore, Maryland. These clinics were affiliated with a major academic health system and served predominantly low-income, urban women. Eligibility requirements included English-speaking pregnant women aged 16 years and older and in their second trimester of pregnancy with a singleton pregnancy.
Institutional review board approval was received from Johns Hopkins Medical Institution prior to study recruitment.
Procedure
The study was discussed with eligible participants during their routine prenatal care appointments. After a complete description of the study, written informed consent was obtained and participants were interviewed in a private area within the clinic with only the researcher and the participant present. The study instruments were read aloud to the women and took approximately 30 minutes to complete. All study participants were compensated $15 for their time and expertise.
Measures
Study measures included a measure of demographics created by the study team, the Prenatal Psychosocial Profile (PPP),20 the Edinburgh Postnatal Depression Scale (EPDS),21 and the Health Practices in Pregnancy Questionnaire-II (HPQ-II).22
The PPP consists of 3 subscales that assess social support, stress, and self-esteem. For the purpose of this study, the 11-item social support subscale was used to measure each woman’s perceived social support. Using a Likert-type scale of 1 (“very dissatisfied”) to 6 (“very satisfied”), each woman was asked to rate her level of satisfaction with the support she received from her partner. Scores on the social support subscale range from 11 to 66, with higher scores indicative of a higher perception of social support. If the woman did not report contact with a partner, she completed the scale based on perceived support from a close family member. Sample items include: “Helps me out when I’m in a pinch,” and “Takes me seriously when I have concerns.” Validity and reliability of each subscale has been supported in several studies that have included ethnically diverse rural and urban women with reliability estimates of subscales ranging from .78 to .98.20 Adequate reliability was demonstrated in the current study (Cronbach’s α = .96).
Depressive symptomatology was measured using the EPDS, the well-validated and most widely utilized screening tool for depressive symptoms in the perinatal period.23 The EPDS contains 10 items and focuses less on somatic symptoms associated with depression making it particularly valuable during the perinatal period.24 Women are asked to rate their responses in a Likert-type format and represent how they’ve felt over the past 7 days. Sample items include, “I have been able to laugh and see the funny side of things,” and “I have felt sad or miserable.” Each item is scored 0 (eg, “not at all,” “never”) to 3 (eg, “most of the time,” “quite a lot”) and the total scale score ranges from 0 to 30 with higher scores indicative of higher depressive symptomatology. The EPDS has been used with racial and ethnic minority women, and several studies have supported its use during pregnancy.23,25 For this analysis, we used the most widely recommended cutoff score for depressive symptomatology during pregnancy (ie, > 12). Consistent with the participating clinics’ protocols, any woman with a positive response to item # 10 (“The thought of harming myself has occurred to me”) on the EPDS or scoring greater than 12 on the EPDS was referred to the clinic social worker and health care provider for further evaluation and treatment. A sensitivity rate of 82% with a specificity of 95% has been previously demonstrated with this cutoff point in a similar population.26 The Cronbach’s α for the current study was .91.
The HPQ-II contains 34 items that ask about health practices in 6 domains including balance of rest and exercise, safety measures, nutrition, substance use, health care access, and access to pregnancy-related information.22 Responses range from 1 (“never”) to 5 (“always” or “daily”) or a word or phrase that indicates the woman’s level of engagement in a specific activity (eg, 1—No alcoholic drinks while pregnant to 5—More than 3 alcoholic drinks at one sitting). Sample items include, “Since becoming pregnant, I have exercised regularly”; “Since becoming pregnant, I have taken herbal remedies other than those recommended to me by my doctor or midwife”; and “Since becoming pregnant, I have eaten 5 servings of fruits or vegetables in a day.” The total scale score ranges from 34 to 170, with a higher score indicative of greater engagement in favorable health practices. Consistent with scoring recommendations, this scale was analyzed as a continuous measure.22 Content validity was established by a diverse sample of pregnant women and maternal-child health experts,22,27 and Cronbach’s α for the current study was .90.
Analysis
Data were analyzed using PASW Statistics 22, Release Version 22.0.0 (SPSS: An IBM Company). Data analysis began with descriptive and exploratory statistical analyses, and study variables were examined to assess distributions, to identify any outliers, and to determine the need for transformation. There were no missing data. A series of generalized linear models were conducted and included variables that had P values less than .15 in bivariate analyses or were deemed theoretically relevant.
RESULTS
Over a period of 6 months, 174 eligible women were approached to participate, and 166 (96%) completed the study instruments. The 8 women declining study participation reported time concerns. As depicted in Table 1, the majority of women identified as being African American (93%), single (54%), and unemployed (77%). Approximately 28% of the women were adolescents (defined in this study as 16 to 19 years of age) at the time of data collection. Two-thirds (66%) of the women reported less than a high school diploma, and nearly half of the women (46%) reported a total annual income of less than $10,000. Nearly two-thirds of the women had a body mass index (BMI) category that classified them as overweight or obese prepregnancy.
Table 1.
Participant Sociodemographic and Clinical Characteristics (N= 166)
| Characteristic | n (%) |
|---|---|
| Age, mean (range), y | 23.3 (16–39) |
| 16–19 | 46 (28) |
| 20–24 | 58 (35) |
| 25–29 | 35 (21) |
| 30–39 | 27 (16) |
| Race | |
| African American | 155 (93) |
| White non-Hispanic | 9 (5) |
| Other | 2 (2) |
| Education | |
| Less than high school | 110 (67) |
| High school graduate/GED | 45 (27) |
| Some college/trade school | 5 (3) |
| College/Trade school graduate | 6 (3) |
| Marital status | |
| Single | 90 (54) |
| Partnered/not married | 56 (34) |
| Married | 17 (10) |
| Divorced | 2 (1) |
| Widowed | 1 (1) |
| Employment status | |
| Unemployed | 127 (77) |
| Employed full-time | 25 (15) |
| Employed part-time | 14 (8) |
| Total household income | |
| Under $10,000 | 76 (46) |
| $10,001–$20,000 | 66 (40) |
| $20,001–$30,000 | 12 (7) |
| $30,001–$40,000 | 8 (5) |
| > $40,000 | 4 (2) |
| Gravidity | |
| Multiparous | 112 (68) |
| Primiparous | 54 (32) |
| Prepregnancy BMI classification, (kg/m2) | |
| Underweight (< 18.5) | 7 (5) |
| Normal (18.5–24.9) | 42 (26) |
| Overweight (25.9–29.9) | 60 (36) |
| Obese (30.0 and above) | 55 (33) |
Predictors of Health Practices During Pregnancy
Table 2 presents the mean scores and standard deviations (SDs) for all study measures. Scores are presented for adolescents and all other age groups. The mean score on the HPQ-II was 121.2 (SD, 19.6; range, 78–159), and the median was 122.0. An examination of HPQ-II scores by age group classification revealed significant differences with adolescents reporting lower levels of engagement in favorable health practices when compared to women in all other age categories (117.2 vs 123.4, P < .001). Specifically, adolescents were significantly less likely to report concerns about their health or questions about their pregnancies to a physician or midwife than women in all other age classifications. Further, adolescents were more likely to report using marijuana, sleeping less than 7 hours at night, and missing more than one prenatal appointment (all P < .001 with Bonferroni correction) than women in all other age classifications.
Table 2.
Participant Scores on Study Instruments (N= 166)
| Health Indicator (Score Range) | Adolescents (n = 46) Mean (SD) |
All Other Age Groups (n = 120) Mean (SD) |
P Value |
|---|---|---|---|
| Depressive symptomatologya | 13.7 (8.6) | 13.9 (7.6) | .21 |
| Social supportb | 34.1 (15.9) | 40.6 (16.8) | < 0.001 |
| Engagement in favorable health practicesc | 117.2 (21.9) | 123.4 (18.8) | < 0.001 |
Edinburgh Postnatal Depression Scale score range is 0–30.
Prenatal Psychosocial Profile score range is 11–66.
Health Practices in Pregnancy Questionnaire-II score range is 34–170.
Importantly, 59% (n = 98) of the participants exceeded the cutoff score of greater than 12 on the EPDS, indicative of depressive symptomatology, and there were no significant differences by age group classification. Finally, the mean score on the social support subscale was 38.5 (SD = 16.7, range 12–56), and adolescents reported significantly less social support than women in all other age groups (34.1 vs 40.6, P < .001).
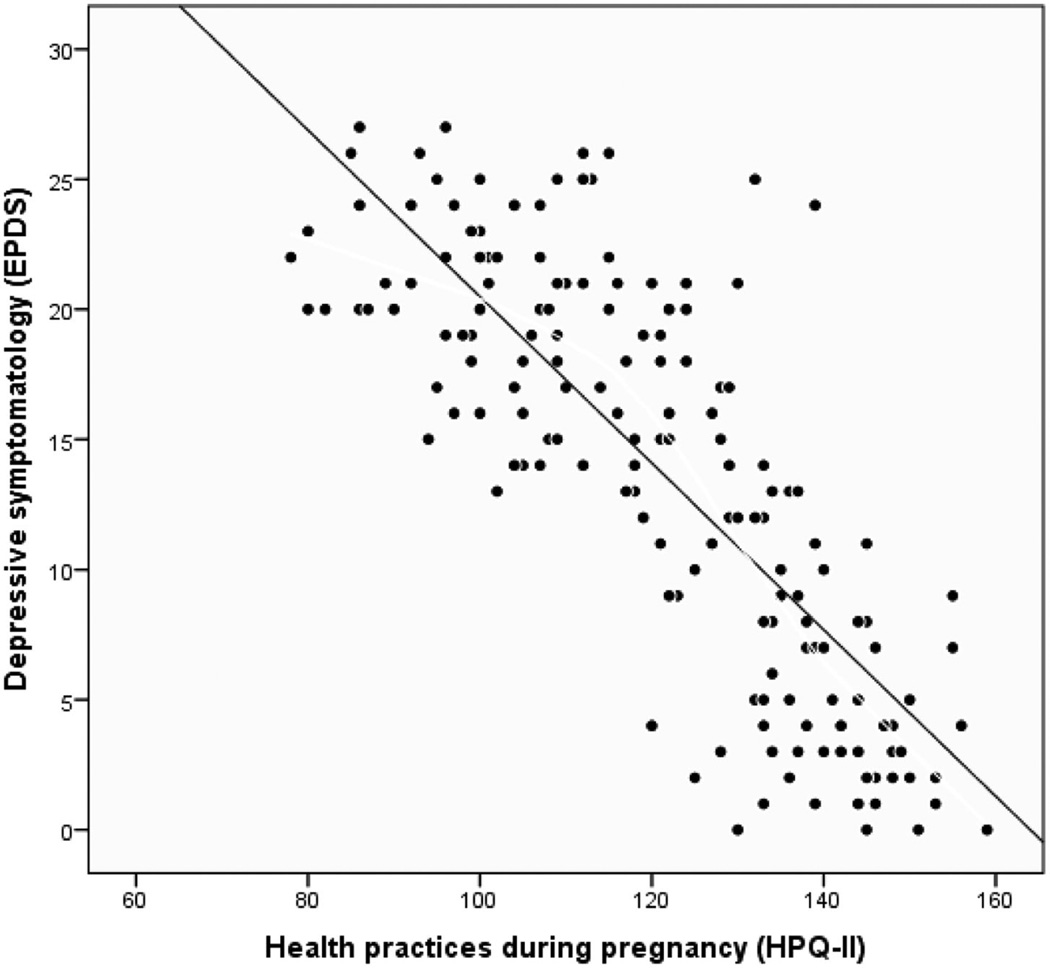
Participant scores on the HPQ-II and EPDS were strongly negatively correlated (r =−0.80; P < .001; Figure 1) suggesting that those participants with higher depressive symptomatology reported less engagement in favorable health practices. Engagement in favorable health practices during pregnancy was strongly positively correlated with social support (r = 0.75, P < .001), suggesting that those women who perceived greater social support reported engaging in more favorable health practices than those women who perceived less social support. With regard to sociodemographic indicators, engagement in favorable health practices during pregnancy was positively correlated with adolescent age (r = 0.28, P < .001), income (r = 0.31, P < .001), education (r = 0.47, P < .001), prepregnancy BMI classification of overweight or obese (r = 0.32, P < .001), and was not significantly associated with marital status or gravidity.
Figure 1. The Relation Between Engagement in Favorable Health Practices and Depressive Symptomatology.
Scatterplot of the relation between health practices during pregnancy and depressive symptomatology. Higher scores on the HPQ-II indicative of engagement in more favorable health practices. Higher scores on the EPDS indicative of greater depressive symptomatology.
All measured sociodemographic characteristics, prepregnancy obesity, depressive symptomatology, and social support were considered for inclusion in a multivariate linear regression model predicting engagement in favorable health practices during pregnancy. In the final model, age, prepregnancy obesity, depressive symptomatology, and social support were significant predictors. Specifically, younger age (ie, 16–19 years), prepregnancy obesity, increased depressive symptomatology, and decreased social support were all significant predictors of less favorable health practices during pregnancy (all P < .001). The final model accounted for 67.8% of the total variance in overall engagement in favorable health practices during pregnancy.
DISCUSSION
Findings from this study suggest that a woman’s mental health is strongly associated with her ability to engage in favorable health practices during pregnancy. In this sample, 59% of the women reported depressive symptomatology. Existing research demonstrates several sociodemographic characteristics associated with a higher risk of perinatal depression, including poverty, single marital status, lower levels of education, and young age.28–30 Findings from this study are similar to those of Lindgren who found that pregnant women with increased depressive symptoms were less likely to engage in favorable health practices.27 Importantly, the majority of the participants in the current study reported living in poverty which precludes comparisons across many study samples.
Research has demonstrated an association between depression and smoking in pregnancy,31,32 and results from the current study suggest that depressive symptoms are associated with less favorable health practices across multiple domains (ie, rest and exercise, safety measures, nutrition, substance use, health care access, access to pregnancy-related information) further highlighting the importance of screening for depression during pregnancy. Further studies with larger numbers of diverse adolescents in particular are needed to better understand the association between mental health and engagement in favorable health practices.
Extant research also supports a link between social support and perinatal depression. That is, women reporting the absence of a supportive partner are at significantly increased risk for perinatal depression.36 Social support is widely associated with positive health outcomes.37 In a sample of rural Hispanic women at risk for postpartum depression, social support from a significant other and family member were significant predictors of nutrition self-care.38
Perceived social support was lower in the women in this sample than in other studies.39,40 An important finding in the current study was that adolescents perceived less social support from a partner or close family member than women in all other age groups. Further, they were less likely to report asking a health care provider if they had questions related to the pregnancy or if there was something they didn’t understand. Research indicates that women who perceive more social support are more likely to seek health information than women who perceive less social support, yet this relationship in adolescents heretofore was largely unexplored.37 In the current study, there were not significant differences in depressive symptomatology between adolescents and other age groups, yet adolescents were less likely to engage in favorable health practices. A greater understanding of the role of social support and engagement in favorable health practices is an important area of continued inquiry, particularly for low-income women who have less formal support systems in place. Qualitative studies exploring how pregnant adolescents define social support, who they turn to for support, and what resources they are inclined to access for pregnancy-related information are needed to best address their unique needs.
Maternal obesity is a well-established risk factor for a number of adverse pregnancy, neonatal, and early childhood outcomes.41,42 Importantly, more than two-thirds of the women in this sample had a prepregnancy BMI classified as overweight or obese, and the presence of this classification was an independent predictor of lower engagement in favorable health practices during pregnancy. In a large sample of women trying to conceive, obese women were more likely to engage in unhealthy weight loss practices, including smoking.43 In a sample of low-income women, diet quality (assessed via 24-hour diet recall) was not significantly related to prepregnancy BMI, yet women with low dietary quality had significantly more depression and less social support.44 Importantly, the study was not powered to assess differences in dietary quality among depressed women of varied BMI classifications. Finally, a mixed-methods study conducted among a sample of low-income pregnant women, with a mean prepregnancy BMI of 28.0, demonstrated that excessive weight gain was common, nutritional knowledge was poor, and few women engaged in healthy behaviors.45 Taken together, this research suggests that low-income women with prepregnancy obesity are in need of additional supports to optimize healthy behaviors during pregnancy.
This study has several important limitations. First, study measures were collected via self-report in a cross-sectional manner precluding our ability to make inferences about their causal relationships. Also, as is true in many studies that rely on self-report, tobacco use and substance use may have been underreported. Further, we did not have access to accurate data on weight gain during pregnancy, which is an important consideration. Despite this, the final model explained a large amount of variance in health practices during pregnancy. Finally, study findings are based on a convenience sample and therefore cannot be generalized beyond this group of women. Nonetheless, this study provides compelling evidence of the important relations among social support, depressive symptomatology, and engagement in favorable health practices during pregnancy in a sample of low-income, predominantly African American women.
Clinical Implications
The American College of Obstetricians and Gynecologists recommends that health care providers screen women at least once during the perinatal period for depression and anxiety symptoms, acknowledging that perinatal depression often goes unrecognized because changes in sleep, energy, and appetite may be attributed to physiologic changes associated with pregnancy.33 Thus, it is particularly important that health care providers are assessing mental health early in the perinatal period, given its association with health practices as well as maternal and early childhood outcomes.
Low-income perinatal women, particularly adolescents, face many barriers to treatment for depression and its related sequelae.34 Health care providers are urged to provide critical linkages to gateway organizations, such as the local department of health, outpatient mental health programs, and community-based organizations that include mental health services as a component of care. Providing a referral to a local home visiting (HV) program is another important consideration in optimizing health outcomes. While mental health is not a primary focus of many home visiting programs, research supports that a positive relationship between the home visitor and the woman is beneficial to maternal mental health, particularly among adolescents.34,35
Policy Implications
The Patient Protection and Affordable Care Act46 expanded health care coverage for millions of women, yet there are many opportunities to further improve perinatal health, and these will be discussed in context of the current study’s findings. To optimize maternal health, experts have recommended that prenatal care be delivered within the context of a medical home and that every woman in the United States should be provided access to a medical home.47,48 This would eliminate the fragmented health care delivery that disproportionately impacts low-income women, allowing them to utilize the medical home before, during, and beyond pregnancies. Health care services should include primary and preventive care, family planning, health education, and social services.48 This would allow for higher levels of care coordination improving access to necessary supports. Further, greater attention could be given to the behavioral and psychosocial needs of each woman. In this model, the health educator is responsible for providing health promotion activities either individually or in a group setting (eg, Centering Pregnancy), and the activities are focused on nutritional counseling, weight management, stress reduction, and relevant behavioral modifications.48 Those women with, for example, significant dietary issues could be referred to a dietitian for further evaluation and treatment. This model better targets health promotion activities while capitalizing on each provider’s strengths (eg, obstetricians aren’t providing comprehensive nutritional counseling).48
CONCLUSION
Nearly two-thirds of the women in this sample reported depressive symptomatology, and depressive symptomatology was significantly associated with poor social support and less engagement in favorable health practices during pregnancy. Improving mental health care, particularly for low-income women who face unique barriers to care, has significant implications for the well-being of women, children, and families. As the work on health care reform continues, maternal-child health care providers are urged to play an active role in further elucidating what should constitute essential services for women’s health. Health care providers, researchers, policymakers, and health plan administrators must work together if we are to realize improvements in maternal and childhood outcomes during the perinatal period.
Quick Points.
-
✦
Pregnancy represents a critical time period during which maternal health practices contribute significantly to maternal, neonatal, and early childhood outcomes.
-
✦
It is important to better understand factors that influence a woman’s ability to engage in favorable health practices during pregnancy, particularly among women at highest risk for poor outcomes in an effort to best support them in achieving optimal pregnancy outcomes.
-
✦
Most pregnant women access health care during the perinatal period, making it an opportune time to assess facilitators and barriers to favorable health practices.
-
✦
Findings from this study suggest that a woman’smental health is strongly associated with her ability to engage in favorable health practices during pregnancy.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
Contributor Information
Jeanne L. Alhusen, School of Nursing at Johns Hopkins University..
Lauren Ayres, School of Nursing at Johns Hopkins University..
Kelli DePriest, School of Nursing at Johns Hopkins University..
REFERENCES
- 1.Lindgren K. A comparison of pregnancy health practices of women in inner-city and small urban communities. J Obstet Gynecol Neonatal Nurs. 2003;32:313–321. doi: 10.1177/0884217503253442. [DOI] [PubMed] [Google Scholar]
- 2.Alhusen JL, Gross D, Hayat MJ, Rose L, Sharps P. The role of mental health on maternal-fetal attachment in low-income women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E71–E81. doi: 10.1111/j.1552-6909.2012.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Witt WP, DeLeire T, Hagen EW, et al. The prevalence and determinants of antepartum mental health problems among women in the USA: a nationally representative population-based study. Arch Womens Ment Health. 2010;13(5):425–437. doi: 10.1007/s00737-010-0176-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haskins A, Bertone-Johnson E, Pekow P, Carbone E, Chasan-Taber L. Correlates of smoking cessation at pregnancy onset among Hispanic women in Massachusetts. Am J Health Promot. 2010;25(2):100–108. doi: 10.4278/ajhp.090223-QUAN-77. [DOI] [PubMed] [Google Scholar]
- 5.Skagerstrom J, Chang G, Nilsen P. Predictors of drinking during pregnancy: a systematic review. J Womens Health (Larchmt) 2011;20(6):901–913. doi: 10.1089/jwh.2010.2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powers JR, McDermott LJ, Loxton DJ, Chojenta CL. A prospective study of prevalence and predictors of concurrent alcohol and tobacco use during pregnancy. Matern Child Health J. 2013;17(1):76–84. doi: 10.1007/s10995-012-0949-3. [DOI] [PubMed] [Google Scholar]
- 7.Neggers Y, Goldenberg R, Cliver S, Hauth J. The relationship between psychosocial profile, health practices, and pregnancy outcomes. Acta Obstet Gynecol Scand. 2006;85(3):277–285. doi: 10.1080/00016340600566121. [DOI] [PubMed] [Google Scholar]
- 8.Forray A, Gotman N, Kershaw T, Yonkers KA. Perinatal smoking and depression in women with concurrent substance use. Addict Behav. 2014;39(4):749–756. doi: 10.1016/j.addbeh.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhusen JL, Ray E, Sharps P, Bullock L. Intimate partner violence during pregnancy: Maternal and neonatal outcomes. Journal of Women’s Health. 2015;24:100–106. doi: 10.1089/jwh.2014.4872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connelly CD, Hazen AL, Baker-Ericzen MJ, Landsverk J, Horwitz SM. Is screening for depression in the perinatal period enough? The co-occurrence of depression, substance abuse, and intimate partner violence in culturally diverse pregnant women. J Womens Health (Larchmt) 2013;22(10):844–852. doi: 10.1089/jwh.2012.4121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20(3):189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- 13.Goedhart G, Snijders AC, Hesselink AE, van Poppel MN, Bonsel GJ, Vrijkotte TG. Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a large multiethnic cohort study. Psychosom Med. 2010;72(8):769–776. doi: 10.1097/PSY.0b013e3181ee4a62. [DOI] [PubMed] [Google Scholar]
- 14.Lutsiv O, Mah J, Beyene J, McDonald SD. The effects of morbid obesity on maternal and neonatal health outcomes: a systematic review and meta-analyses. Obes Rev. 2015;16(7):531–546. doi: 10.1111/obr.12283. [DOI] [PubMed] [Google Scholar]
- 15.McDonald SD, McKinney B, Foster G, Taylor V, Lutsiv O, Pullenayegum E. The combined effects of maternal depression and excess weight on neonatal outcomes. Int J Obes (Lond) 2015;39(7):1033–1040. doi: 10.1038/ijo.2015.44. [DOI] [PubMed] [Google Scholar]
- 16.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 17.Zhao G, Ford ES, Dhingra S, Li C, Strine TW, Mokdad AH. Depression and anxiety among US adults: associations with body mass index. Int J Obes (Lond) 2009;33(2):257–266. doi: 10.1038/ijo.2008.268. [DOI] [PubMed] [Google Scholar]
- 18.Kapadia MZ, Gaston A, Van Blyderveen S, et al. Psychological antecedents of excess gestational weight gain: a systematic review. BMC Pregnancy Childbirth. 2015;15(1):107. doi: 10.1186/s12884-015-0535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 20.Curry MA, Campbell RA, Christian M. Validity and reliability testing of the prenatal psychosocial profile. Res Nurs Health. 1994;17:127–135. doi: 10.1002/nur.4770170208. [DOI] [PubMed] [Google Scholar]
- 21.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 22.Lindgren K. Testing the health practices in pregnancy questionnaire-II. J Obstet Gynecol Neonatal Nurs. 2005;34:465–472. doi: 10.1177/0884217505276308. [DOI] [PubMed] [Google Scholar]
- 23.Davis K, Pearlstein T, Stuart S, O’Hara M, Zlotnick C. Analysis of brief screening tools for the detection of postpartum depression: comparisons of the PRAMS 6-item instrument, PHQ-9, and structured interviews. Arch Womens Ment Health. 2013;16(4):271–277. doi: 10.1007/s00737-013-0345-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan D, Milis L, Misri N. Depression during pregnancy. Can Fam Physician. 2005;51(8):1087–1093. [PMC free article] [PubMed] [Google Scholar]
- 25.Alhusen JL, Gross D, Hayat MJ, Rose L, Sharps P. The role of mental health on maternal-fetal attachment in low-income women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E71–E81. doi: 10.1111/j.1552-6909.2012.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tandon SD, Cluxton-Keller F, Leis J, Le HN, Perry DF. A comparison of three screening tools to identify perinatal depression among low-income African American women. J Affect Disord. 2012;136(1–2):155–162. doi: 10.1016/j.jad.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindgren K. Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health. 2001;24:203–217. doi: 10.1002/nur.1023. [DOI] [PubMed] [Google Scholar]
- 28.Liu CH, Tronick E. Rates and predictors of postpartum depression by race and ethnicity: results from the 2004 to 2007 New York City PRAMS survey (pregnancy risk assessment monitoring system) Matern Child Health J. 2013;17(9):1599–1610. doi: 10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- 29.Koleva H, Stuart S. Risk factors for depressive symptoms in adolescent pregnancy in a late-teen subsample. Arch Womens Ment Health. 2014;17(2):155–158. doi: 10.1007/s00737-013-0393-4. [DOI] [PubMed] [Google Scholar]
- 30.Tzilos GK, Zlotnick C, Raker C, Kuo C, Phipps MG. Psychosocial factors associated with depression severity in pregnant adolescents. Arch Womens Ment Health. 2012;15(5):397–401. doi: 10.1007/s00737-012-0296-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: A systematic review. Am J Obstet Gynecol. 2010;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alhusen JL, Lucea MB, Bullock L, Sharps P. Intimate partner violence, substance use, adverse neonatal outcomes among urban women. J Pediatr. 2013;163:471–476. doi: 10.1016/j.jpeds.2013.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American College of Obstetricians and Gynecologists. Screening for perinatal depression. Committee opinion no. 630. Obstet Gynecol. 2015;125:1268–1271. doi: 10.1097/01.AOG.0000465192.34779.dc. [DOI] [PubMed] [Google Scholar]
- 34.Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics. 2014;133(1):114–122. doi: 10.1542/peds.2013-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Howard KS, Brooks-Gunn J. The role of home-visiting programs in preventing child abuse and neglect. Future Child. 2009;19(2):119–146. doi: 10.1353/foc.0.0032. [DOI] [PubMed] [Google Scholar]
- 36.Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guillory J, Niederdeppe J, Kim H, et al. Does social support predict pregnant mothers’ information seeking behaviors on an educational website? Matern Child Health J. 2014;18(9):2218–2225. doi: 10.1007/s10995-014-1471-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim Y. The Self-Care Ability for Health Practices in Rural Hispanic Women Experiencing Depressive Symptoms During Postpartum. Azusa, CA: Azusa Pacific University; 2014. [Google Scholar]
- 39.Jesse DE, Walcott-McQuigg J, Mariella A, Swanson MS. Risks and protective factors associated with symptoms of depresison in low-income African American and Caucasian women during pregnancy. J Midwifery Womens Health. 2005;50:405–410. doi: 10.1016/j.jmwh.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 40.Bloom T, Curry MA, Durham L. Abuse and psychosocial stress as factors in high utilization of medical services during pregnancy. Issues Ment Health Nurs. 2007;28(8):849–866. doi: 10.1080/01612840701493212. [DOI] [PubMed] [Google Scholar]
- 41.Aviram A, Hod M, Yogev Y. Maternal obesity: implications for pregnancy outcome and long-term risks—a link to maternal nutrition. Int J Gynaecol Obstet. 2011;115(Suppl 1):S6–S10. doi: 10.1016/S0020-7292(11)60004-0. [DOI] [PubMed] [Google Scholar]
- 42.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202(4):335–343. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berenson AB, Pohlmeier AM, Laz TH, Rahman M, McGrath CJ. Nutritional and weight management behaviors in low-income women trying to conceive. Obstet Gynecol. 2014;124(3):579–584. doi: 10.1097/AOG.0000000000000416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fowles ER, Stang J, Bryant M, Kim S. Stress, depression, social support, and eating habits reduce diet quality in the first trimester in low-income women: a pilot study. J Acad Nutr Diet. 2012;112(10):1619–1625. doi: 10.1016/j.jand.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hackley B, Kennedy HP, Berry DC, Melkus GD. A mixed-methods study on factors influencing prenatal weight gain in ethnic-minority women. J Midwifery Womens Health. 2014;59(4):388–398. doi: 10.1111/jmwh.12170. [DOI] [PubMed] [Google Scholar]
- 46.Mar 23, The Patient Protection and Affordable Care Act (PPACA) 2010 Pub. L. No. 111–148, 124 Stat. [Google Scholar]
- 47.Pies C, Kotelchuck M. Bringing the MCH life course perspective to life. Matern Child Health J. 2014;18(2):335–338. doi: 10.1007/s10995-013-1408-5. [DOI] [PubMed] [Google Scholar]
- 48.Lu MC. Healthcare reform and women’s health: a life-course perspective. Curr Opin Obstet Gynecol. 2010;22(6):487–491. doi: 10.1097/GCO.0b013e328340fffa. [DOI] [PubMed] [Google Scholar]