Abstract
Background:
Epilepsy is a neurological disorder characterized by abnormal firing of nerve impulses in the brain.
Aim:
This study aims to investigate the frequency of appearance of pathological changes in conventional examination methods (electroencephalography–EEG, brain computerized tomography -CT or brain magnetic resonance imaging – MRI) in patients with epilepsy, and relationship between clinical manifestations and localization of changes in CT or MRI.
Methods:
In this study we have included 110 patients with focal epilepsy who fulfilled the inclusion criteria out of 557 initially diagnosed patients. Detailed clinical examination together with brain imaging (CT and MRI) and electroencephalography examination was performed. We have evaluated the accuracy of each diagnostic method to localize the epileptic focus. Diagnosis of epilepsy was determined by the ILAE (International League Against Epilepsy) criteria of the year 1989, and classification of epileptic seizures was made according to the ILAE classification 2010.
Results:
Electroencephalography presented changes in 60.9% of patients; brain CT in 42.1%, and MRI in 78% of the patients. The results of our study showed that clinical manifestations were not always conveyed with pathological changes in conventional examining methods performed. Of the total of 79 patients with changes in imaging (8 with changes in CT and 71 in MRI), 79.7% presented a clinical picture compatible with the region in which morphological changes were found, while in 20.3% of patients the presented morphological changes were not aligned with the clinical picture.
Conclusion:
In patients with epilepsy, conventional examination methods do not always find pathological changes, while clinical manifestations of epilepsy did not always coincide with the location of changes in imaging. Further studies are needed to see if there is clear border between focal and generalized epilepsy.
Keywords: Epilepsy, morphological changes, EEG, CT, MRI
1. INTRODUCTION
Abnormal electrical activity, which characterizes epilepsy, is the result of biochemical processes of hyperexcitability of nerve cells and neuronal hypersynchronization. However, a single neuron, although with abnormal discharge, is insufficient to produce an epileptic seizure, whichhappens only in the context of extensive neuronal networks. Cortical structures and some of the key subcortical areas are involved in the generation of a crisis (1). Cellular mechanisms of epileptogenesis are numerous and include loss of cells, gliosis, modification of neurogenesis and synaptogenesis (2). However, althoughthe causes of the disease remain difficult to define, it is know that the crisis itself is caused by malfunction of a large number of neurons. These last are linked with synapses and are organized into networks that facilitate the flow of action potentials (3).
Electroencephalography (EEG) has relatively low sensitivity regarding epilepsy, between 25-56% (4). Another study showed that the sensibility of EEG in detecting epileptiform changes is 62.7% in cases clinically suspicious for epilepsy (5). On the other hand, MRI presents a high sensitivity in detecting structural damage. Its superiority compared with computerized tomography was immediately recognizedafter its development. First generation computed tomography reveals only 3% of operable lesions (6). MRI, however, detects up to 80% of operable temporal lesions in patients who can benefit from a temporal lobotomy and up to 60% of frontal lesions in patients that can benefit from surgery of the frontal lobes (7, 8).
International League Against Epilepsy recommends performing an MRI in all patients with epilepsy, except for those with idiopathic generalized epilepsy (9). Crises originating from the back of the parietal lobe are most often clinically silent until they spread in the primary sensitive cortex or on other lobes, including frontal, temporal, or occipital (first of all, the temporal region and motor frontal supplementary region) (10). Somatic-sensitive disorder appears on the contralateral side of the seizure origin (11), but in some cases it can also occur on the same side (12).
2. METHODS
Patients’ selection
Data of 6846 patients with various neurological diseases, which were examined during the period June 2012–June 2014, in the Neurology Clinic of the University Clinical Center of Kosova, were analyzed. Of those, 805 (11.8%) presented with epilepsy and 6041 (88.2%) presented with other neurological pathologies. Out of 557 patients diagnosed with focal epilepsy, in this study we have included 110, mean age was 27.7±5.7 years, 47.3% were females. Conventional diagnostic methods used were: electroencephalography (EEG), brain computerized tomography (CT) and magnetic resonance imaging of the brain (MRI). Regular neurological consultations and examination with conventional diagnostic methods were criteria for inclusion of patients in the study. Patients that did not met these criteria were not included in the study (n=447).
Diagnosis of epilepsy was determined by means of the ILAE (International League Against Epilepsy) 1989 criteria, and epileptic seizures were classified according to the 2010ILAE classification.
Statistical analysis
Kappa values were calculated to determine the sensitivity for each diagnostic method. The comparison between accuracy of different diagnostic methods was performed using proportion Z-test with pre-selected significance level of p<0.05. We have used IBM SPSS statistics version 22 for the statistical analysis.
3. RESULTS
Electroencephalography was conducted in all 110 patients, brain MRI was performed in 91 cases (82.7%), and brain CT in 19 cases (17.3%) and (Table 1). Specific epileptiform changes in EEG were presented in 67 out of 110 patients, resulting in a sensitivity of 60.9%.
Table 1.
Conventional diagnostic methods conducted

Out of 91 patients that underwent MRI, structural changes were presented (epileptiform foci) in 71 (78%) compared to 8 out of 19 (42.1%) patients who underwent brain CT. Changes on CT were mainly observed in cases with cerebrovascular disease and in cases with major brain morphological injuries. Brain MRI showed significantly higher sensitivity compared to electroencephalography 78% vs. 69.9 % (p=0.009) and brain CT 42.15% vs. 78% (p=0.001) (Figure 1). Even thought, electroencephalography showed higher sensitivity compared to brain CT 60.9% vs. 42.1%, the difference between these two methods was not significant (p=0.12).
Figure 1.
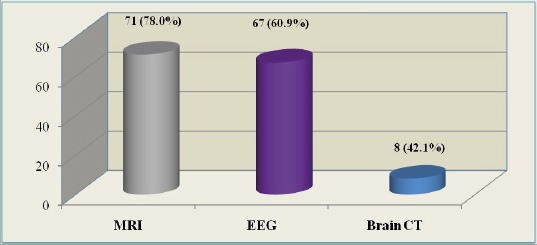
Cases with pathological changes presented on different examining methods
It has to be worth mentioned that clinical manifestations were not conveyed in all cases with pathological changes in the conventional examining methods usedin patients involved in the study.
In 31 patients (28.2%) out of 110 patients included in the study, no morphological changes were observed on the imaging methods performed (Figure 2).
Figure 2.

Cases with and without structural changes on imaging evaluations
Among 79 patients with changes in imaging (8 with changes in brain CT and 71 in brain MRI) 63 patients (79.7%) presented a clinical picture compatible with the region in which the morphological changes were found, whereas in 16 patients (20.3%) the morphological changes found were not compatible with the clinical picture (Table 2). In 27 patients (24%) who initially presented with generalized epileptiform changes, on the repeated EEG examination after one to three months of treatment with antiepileptic therapy we noticed focal changes on EEG.
Table 2.
Compatibility of morphological changes on imaging (CT, MRI) and electroencephalography with the clinical picture

4. DISCUSSION
EEG was confirmed as a highly specific method for epilepsy diagnosis (5), however, this method has some drawbacks regarding its low sensitivity (4). Brain MRI is a highly sensitive method for detection of structural changes. As compared to brain CT, MRI is much more accurate for detecting structural brain changes in patients with epilepsy (6-8).
In our study, EEG showed specific changes in 60.9% of epileptic patients, which is approximate to the results of other studies (4). Brain CT showed morphological changes compatible with epilepsy in 42.1% of patients compared to 78% of patients on MRI. Changes on brain CT were observed mainly in cases with cerebrovascular disease and those with major morphological brain injuries. Our results are closely similar to studies of many other authors who have dealt with this issue (4, 5, 7, 8, 13).
We realized that clinical manifestations were not conveyed in all cases with pathological changes in the conventional examination methods performed in patients included in the study. In 79.7% of cases a correlation between clinical manifestations and brain morphological changes was observed, compared with 20.3% of patients in whom such correlation was not observed. A possible reason for this incompatibility might be the spread of epileptic discharges toward other brain regions, or probably the co-existence of another epileptic focus not associated with brain structural change. Several other studies showed similar data on this issue (1-3, 10, 14, 15).
A characteristic worth mentioning, in terms of EEG changes, is that on a repeated EEG examination the foci were not localized always in the same region. Sometimes it happened that in the same patient the EEG focus has changed during the repeated examination.
Interestingly, we have observed that typical EEG changes for generalized epilepsy (such as the presence of 3.5 Hz spike-wave complexes) have been transformed to typical epileptiform changes of focal epilepsy months after treatment with antiepileptic drugs. This fact shows that there is no clear border between focal and generalized epilepsy. An important factor defining the appearance of epileptic seizures has been the presence of gliosis around the lesion detectable on imaging. We noticed that the higher pronounced gliosis were associated with a greater epileptogenicity of the lesions, especially when lesions involved in the generation of a seizure were located in the cortical and key subcortical regions.
Study limitations: An important limitation of this study is the low number of patients included; particularly those who underwent brain CT. This might affect the results of comparisons between brain CT and other methods sensitivity. Because all of patients included in the study were diagnosed with focal epilepsy, evaluation of specificity, positive and negative predictive value analysis for each diagnostic method was not possible.
5. CONCLUSION
Although the conventional examination methods EEG, MRI and brain CT, were sensitive in detection of epileptic foci, the level of sensitivity was not the same. The clinical manifestations of focal epilepsy do not always coincide with the location of changes in imaging. Our study results raise the question if seizures are primarily generalized, or they begin as focal and become generalized immediately after they start.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Stafstrom CE, Carmant L, et al. Seizures and epilepsy: an overview for neuroscientists. Cold Spring Harb Perspect Med. 2015 Jun 1;5(6):a022426. doi: 10.1101/cshperspect.a022426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lascheta J, Louvela J, Kurcewicza I, et al. Cellular mechanisms of the epilepsies: In vitro studies on human tissue. Neurochirurgie. 2008;54:141–7. doi: 10.1016/j.neuchi.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Bartolomei F, et al. Neural networks involving the medial temporal structures in temporal lobe epilepsy. Clin Neurophysiol. 2001 Sep;112(9):1746–60. doi: 10.1016/s1388-2457(01)00591-0. [DOI] [PubMed] [Google Scholar]
- 4.Smith SJM. EEG in the diagnosis, classification, and management of patients with epilepsy. J Neurol Neurosurg Psychiatry. 2005 Jun;76(Suppl 2):ii2–7. doi: 10.1136/jnnp.2005.069245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajib NayanChowdhury, et al. Interictal EEG changes in patients with seizure disorder: experience in Bangladesh. Springerplus. 2013;2:27. doi: 10.1186/2193-1801-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilner AN, Sharma BK, Thompson A, et al. Diagnoses, procedures, drug utilization, comorbidities, and cost of health care for people with epilepsy in 2012. Epilepsy Behav. 2014 Dec; 41:83–90. doi: 10.1016/j.yebeh.2014.08.131. [DOI] [PubMed] [Google Scholar]
- 7.Berkovic SF, McIntosh AM, Kalnins RM, et al. Preoperative MRI predicts outcome of temporal lobectomy: an acturarial analysis. Neurology. 1995;45:1358–63. doi: 10.1212/wnl.45.7.1358. [DOI] [PubMed] [Google Scholar]
- 8.Mosewich RK, So EL, O'Brien TJ, et al. Factors predictive of the outcome of frontal epilepsy surgery. Epilepsia. 2000;41:843–9. doi: 10.1111/j.1528-1157.2000.tb00251.x. [DOI] [PubMed] [Google Scholar]
- 9.Wilmshurst JM, Gaillard WD, Vinayan KP, et al. Summary of recommendations for the management of infantile seizures: Task Force Report for the ILAE Commission of Pediatrics. Epilepsia. 2015 Aug;56(8):1185–97. doi: 10.1111/epi.13057. [DOI] [PubMed] [Google Scholar]
- 10.Siegel AM. Parietal lobe epilepsy. Adv Neurol. 2003;93:335–45. [PubMed] [Google Scholar]
- 11.Salanova V. Parietal lobe epilepsy. J Clin Neurophysiol. 2012 Oct;29(5):392–6. doi: 10.1097/WNP.0b013e31826c9ebc. [DOI] [PubMed] [Google Scholar]
- 12.Schoenberg MR, Frontera AT, Bozorg A, et al. An update on epilepsy. Expert Rev Neurother. 2011 May;11(5):639–45. doi: 10.1586/ern.11.50. [DOI] [PubMed] [Google Scholar]
- 13.Xiao F, An D, Chen S, et al. Clinical and Electroencephalographic (EEG) Features Associated With Refractoriness in Benign Childhood Epilepsy With Centrotemporal Spikes. J Child Neurol. 2015 Oct;30(12):1591–7. doi: 10.1177/0883073815575367. [DOI] [PubMed] [Google Scholar]
- 14.Vlaicu M. B, Epileptogenèse et pathologie post-traumatique cérébrale, Service de Neurologie et Neurovasculaire, Hôpital Saint- Joseph;Service de Neurochirurgie, Pitié-Salpétrière;UniversitéRenéDescartes, Paris-Neurologies, Décembre. 2011;14:143. [Google Scholar]
- 15.Nguyen DK, Mbacfou MT, Nguyen DB, et al. Prevalence of nonlesional focal epilepsy in an adult epilepsy clinic. Can J Neurol Sci. 2013 Mar;40(2):198–202. doi: 10.1017/s0317167100013731. [DOI] [PubMed] [Google Scholar]


