Abstract
Study Objective
To estimate Long-Acting Reversible Contraception (LARC) discontinuation rates. Secondary aims are to determine risk factors for discontinuation, describe reasons for discontinuation, evaluate complications related to placement, and estimate pregnancy rates after discontinuation.
Design
We conducted a retrospective cohort study of LARC method use through review of electronic medical record data.
Setting
Our program is housed in an academic primary care pediatric and adolescent clinic in Baltimore, Maryland.
Participants
160 women ages 12-24 who received an intrauterine device (IUD) or subdermal implant through our program between December 10, 2012 and December 10, 2015.
Interventions
None
Main Outcome Measures
Complications from LARC insertion, device discontinuation, reason(s) for discontinuation, pregnancies resulting from device failure, and occurrence of pregnancy within one year of discontinuation.
Results
Thirty-five women discontinued their LARC method. The six-month discontinuation rate was 11.3% and the 12-month rate was 21.9%. Discontinuation was associated with history of STI (adjusted hazard ratio (AHR) 3.21, 95% confidence interval (CI) 1.49-6.90). The most common reason for discontinuation was bleeding for the implant and expulsion for the IUD.
Conclusions
Our results support the safety and low discontinuation rates of LARC provision to adolescents and young adult women in a primary care setting. Discontinuation rates and reasons are consistent with those described by other studies.
Keywords: Adolescent, Contraception, LARC, Long-acting reversible contraception
Introduction
Despite recent declines, the United States’ teen pregnancy rate remains one of the highest among developed countries.1 Approximately 80% of teen pregnancies are unintended, a significantly higher proportion than the overall national rate of 50%, reflecting a substantial unmet need for contraception in this age group.2 Similarly, unintended pregnancies make up 60% of pregnancies in young adult women ages 20-24, who in turn have the highest pregnancy rates in the country.2 Health inequities are evident, with significantly higher pregnancy rates among black and Hispanic teen and young adult women.1 Significant geographic disparities exist as well. For example, Baltimore, Maryland has long had one of the highest rates of teen births in the United States, most recently at 43 per 1,000 girls ages 15-19, nearly twice the state and national rates.3 Baltimore garnered national attention over two decades ago when it became the first city in the United States to offer Norplant to students at public schools, a practice later discontinued due to community backlash.4 Efforts to enhance access to effective contraception were reinitiated in 2010 as part of a strategic plan by the Baltimore City Health Department to reduce teen pregnancy rates in the city.5 Baltimore remains a challenging setting for reducing teen pregnancy.
Local efforts were further bolstered by the support of professional organizations who agree that long-acting reversible contraception (LARC), namely intrauterine devices (IUDs) and subdermal implants, should be offered as safe, effective contraceptive choices for adolescents.6,7,8 Studies show low LARC discontinuation rates for adolescents and young adult women, comparable to rates for adult women, in contrast to the higher rates of discontinuation of short-acting contraception in this age group.9 However, pediatricians and adolescent medicine specialists, those most likely to see women in this age bracket, are not consistently trained in LARC provision as this is not a standard requirement for accredited training programs in the United States.10,11
Rates of LARC utilization remain low among adolescents and young adult women.12 The medical and public health communities have developed large-scale programs in recent years to try to decrease barriers to LARC use. For example, the Contraceptive CHOICE Project and the Colorado Family Planning Initiative (CFPI) increased LARC uptake with a subsequent decrease in pregnancy, birth, and abortion rates among adolescent and young adult women.13,14 While these projects have had a substantial impact, both received extensive private funding, which is not always available. More evidence is needed from small-scale, real-world programs and practice settings.
Our academic institution created a program to increase LARC access for adolescent and young adult women, housed in a pediatric primary care clinic. Multidisciplinary collaboration was used to train pediatric and adolescent providers in LARC provision and establish an on-site OB/GYN clinic in order to bypass outside referral and streamline service delivery. Program implementation is described in more detail elsewhere.15 The primary aim of this analysis is to estimate LARC discontinuation rates for women who received an IUD or implant through our program in its first three years. Continuation can serve as an indirect marker of effectiveness and patient satisfaction, and correlation has been shown between these measures.16 Secondary aims are to determine risk factors for discontinuation, describe reasons for discontinuation, evaluate complications related to placement, and estimate pregnancy rates after discontinuation.
Materials and Methods
Study Setting
This clinic is located in Baltimore City and provides continuity of care for approximately 8,000 patients from birth through age 25. The clinic receives Title X funding to provide reproductive health services to those who are uninsured or underinsured. No funding was received for our particular program. The Johns Hopkins Department of Pediatrics and Department of Gynecology and Obstetrics started collaboration in August 2011. The first device was placed in December 2012. The Johns Hopkins University School of Medicine Institutional Review Board approved this quality improvement program and analysis.
Study procedures
We conducted a retrospective cohort study of LARC method use initiated through our program. A database of patients who received LARC devices had been created prospectively as an IRB-approved quality control measure. This database included patient name, medical record number, referral date, reason for referral, current contraception, insurance type, race, consult appointment, provider, and insertion date. We reviewed electronic medical records of all patients who had IUDs and implants placed through the program from December 10, 2012 through December 10, 2015 and extracted supplementary information including missing data and additional variables, described below.
Measures
Extracted baseline data included demographics (age, race, and insurance), reproductive health history (parity, history of sexually transmitted infection (STI), and HIV status), LARC method choice, and LARC insertion date. History of STI and history of HIV were determined from provider notes and confirmed with laboratory results if available. Outcome variables collected included complications from LARC insertion, device discontinuation date, reason(s) for discontinuation, birth control plan at time of removal, pregnancies resulting from device failure, and occurrence of pregnancy within one year of discontinuation. Complications associated with device insertion were defined a priori as uterine perforation or pelvic inflammatory disease (PID) within one month of insertion for women who received an IUD, and hematoma, cellulitis, or allergic reaction for those who received an implant. Discontinuation was ascertained from documentation of removal, prior removal, or expulsion in the medical record, either recorded during a clinic visit or in a telephone note. Follow-up time for women with method discontinuation was the time between device insertion and discontinuation. For women with no documented discontinuation, follow-up time was defined as the time between device insertion and the last note in the medical record that documented the device was in use.
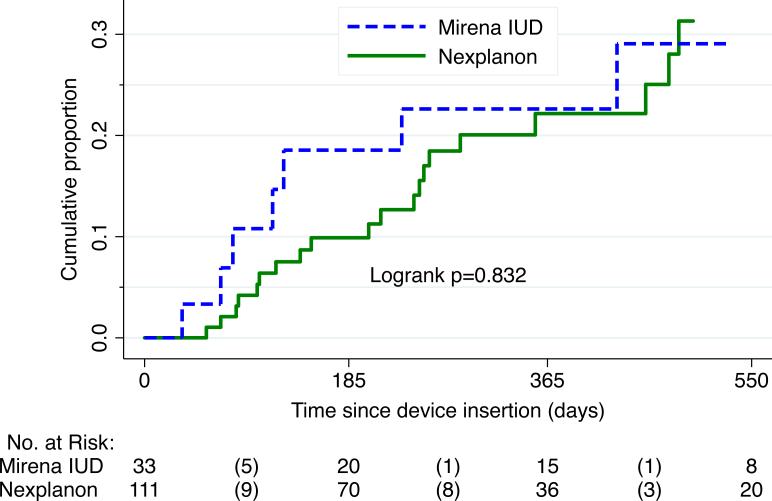
Data analysis
Descriptive analyses were used to evaluate the study population, complications associated with insertion, reasons for discontinuation, birth control plan after discontinuation, and pregnancy rates after discontinuation. Rates of cumulative discontinuation were estimated with life table analysis and plotted using the Kaplan-Meier survival function. The log-rank test was used to determine if there was a statistically significant difference in the overall discontinuation rates for implant versus IUD users. Given time to event data with varied follow-up time, Cox proportional hazards modeling was performed to evaluate the association of various patient characteristics with the risk of discontinuation. This method of analysis excludes any patients for whom no follow-up time is available. Model assumptions of proportional hazards were tested based on Schoenfeld residuals.17 Analyses were performed with Stata statistical software.18
Results
Participants
During this time period a total of 1242 women were seen in the primary care clinic for family planning visits. A total of 160 adolescent and young adult women received a LARC device through our program during the three-year study period, and thus 160 charts were reviewed. An overview of patient characteristics for women who received LARC is provided in Table 1. After contraceptive counseling, 119 (74%) women received an etonorgestrel subdermal implant and 41 (26%) selected a levonorgestrel IUD (LNG-IUS). No patient chose the copper IUD. Ninety-five percent of patients were black. Twenty percent reported a history of pregnancy, and 14% overall had previously given birth. History of STI's was common (34%), including 4% of patients with HIV positive status. Mean age at time of insertion was 17.5 years (range 12-24, standard deviation (SD) 2.5).
Table 1.
Overview of patient characteristics
| Characteristic | All patients (n=160) | Implant (n=119) | LNG-IUS (n=41) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age (years) | |||
| 12-17 | 86 (54) | 68 (57) | 18 (44) |
| 18-24 | 74 (46) | 51 (43) | 23 (56) |
| Race | |||
| Black | 152 (95) | 113 (95) | 39 (95) |
| White | 8 (5) | 6 (5) | 2 (5) |
| Insurance | |||
| Public | 130 (81) | 105 (88) | 25 (61) |
| Private | 20 (13) | 8 (7) | 12 (29) |
| None | 10 (6) | 6 (5) | 4 (10) |
| Parity | |||
| Never pregnant | 128 (80) | 94 (79) | 34 (83) |
| History of abortion§ | 10 (6) | 7 (6) | 3 (7) |
| Parous | 22 (14) | 18 (15) | 4 (10) |
| History of STI | |||
| Yes | 55 (34) | 37 (31) | 18 (44) |
| No | 105 (66) | 82 (69) | 23 (56) |
| HIV status | |||
| Yes | 7 (4) | 5 (4) | 2 (5) |
| No | 153 (96) | 114 (96) | 39 (95) |
induced or spontaneous
Discontinuation
Of 160 patients, 35 had their LARC device removed during the follow-up period: 27 of those with implants and eight of those with LNG-IUS. Sixteen patients were excluded from further analysis because no follow-up time was available. A sensitivity analysis showed that there was no difference between these patients and those remaining in terms of any of the baseline characteristics detailed in table 1. A total of 127 woman-years were analyzed. Median follow-up time for all patients was 784 days or approximately 2 years and 2 months. For those who had the device removed, median time to discontinuation was 244 days, or approximately 8 months. The rate of cumulative LARC discontinuation at six months was 11.3% (95% CI 6.9-18.3%). The rate at twelve months was 21.9% (95% CI 15.0-31.5%). Kaplan-Meier curves further depict time to discontinuation for each method, with log-rank testing demonstrating no difference in survival functions between the implant and LNG-IUS (p=0.832) (Figure 1).
Figure 1.
Cumulative proportion with LARC discontinuation
Table 2 presents the multivariate Cox proportional hazards analysis of predictors of LARC discontinuation. The following variables were included in the model: contraceptive method choice, age, insurance, parity, and documented history of any STI. Race and HIV status were excluded from the final analysis due to the low number of patients who were white or HIV positive. Patients with a history of STI had increased risk of discontinuation (AHR 3.21, 95% CI 1.49-6.90). Patients with private insurance had a decreased risk of discontinuation compared to those with public insurance (AHR 0.19, 95% CI 0.04-0.99). There were no differences based on LARC method or other demographic characteristics measured. A sensitivity analysis was performed excluding women with discontinuation due to IUD expulsion; these were accidental rather than requested removals so may differ. In this analysis, insurance type was no longer statistically significant (AHR 0.24, 95% CI 0.02-2.26). No other differences in the results were noted.
Table 2.
Multivariate Cox proportional hazards analysis of predictors of LARC discontinuation
| Characteristic | AHR (95% CI) | P value |
|---|---|---|
| Method chosen | ||
| Implant (ref) | 1.0 | |
| LNG-IUS | 1.27 (0.50-3.21) | 0.619 |
| Age (years) | ||
| 12-17 | 0.92 (0.41-2.03) | 0.828 |
| 18-24 (ref) | 1.0 | |
| Insurance | 0.047 | |
| Public (ref) | 1.0 | |
| Private | 0.19 (0.04-0.99)* | 0.048 |
| None | 2.05 (0.55-7.58) | 0.284 |
| Parity | 0.784 | |
| Never pregnant (ref) | 1.0 | |
| History of TAB/SAB* | 0.75 (0.17-3.28) | 0.701 |
| Parous | 1.31 (0.47-3.69) | 0.604 |
| History of STI | ||
| Yes | 3.21 (1.49-6.90)* | 0.003 |
| No (ref) | 1.0 | |
LNG-IUS, levonorgestrel intrauterine system; AHR, adjusted hazard ratio; CI, confidence interval; ref, reference
statistically significant finding
Pseudo R-squared .0689
Reasons for discontinuation are detailed in Table 3. Of those who had the implant removed, the most common reasons recorded in the medical chart included bleeding problems (59%), weight gain (22%), pelvic pain/cramping (15%), desire for pregnancy (15%), and mood changes (11%). LNG-IUS discontinuation was due to partial or complete expulsion (63%), vaginal discharge (25%), pelvic pain/cramping (13%), and vaginal bleeding (13%). The overall expulsion rate was 12%. Four of the five cases of expulsion were in nulliparous women, and although replacement was offered in all cases, the women declined. Twenty-three percent of patients had more than one recorded reason for LARC removal.
Table 3.
Reasons for discontinuation
| Reason for discontinuation | Implant (n=27) | LNG-IUS (n=8) |
|---|---|---|
| Bleeding problems | 16 (59%) | 1 (13%) |
| Weight gain | 6 (22%) | |
| Pelvic pain/cramping | 4 (15%) | 1 (13%) |
| Desire for pregnancy | 4 (15%) | |
| Mood changes | 3 (11%) | |
| Partial or complete expulsion | 5 (63%) | |
| Vaginal discharge | 2 (25%) |
Reasons included in this table were those that accounted for >10% of discontinuations
The percentages do not add up to 100 as more than one reason was often cited
Safety and Pregnancy
Only two complications related to insertion were documented. One of the patients who received an implant developed cellulitis, which was treated successfully with oral antibiotics, and the implant was left in place. Another patient was noted to have chlamydia from testing at time of IUD placement. When the patient was contacted for treatment, she complained of cramping and was therefore treated prophylactically for PID. The IUD was left in place. In addition, although this was not an a priori complication, the chart review revealed that two implants were placed in patients with very early pregnancy in the setting of a negative urine pregnancy test. One was removed when the patient found out she was pregnant, and she continued the pregnancy. Delivery information is not available, as she did not deliver in our hospital system. Inadvertent use of the implant during early pregnancy has not been associated with teratogenicity or adverse pregnancy outcomes.6 The other patient terminated the pregnancy and left the device in place.
There were no pregnancies as a result of method failures or unnoticed expulsions. Of 29 women who had their device removed for reasons other than desire for pregnancy, one switched to another LARC method, 24 (83%) chose a shorter acting hormonal method, and four (14%) chose to use condoms. The woman who switched to another LARC method did not become pregnant during the time of this analysis. Conversely, six (25%) of those who chose a shorter acting hormonal method and two (50%) of those using condoms became pregnant within one year of removal. Overall, 28% of the women who discontinued LARC for reasons other than desire for pregnancy became pregnant within one year.
Discussion
Rates of LARC method discontinuation in adolescents and young adult women are low in this clinical setting and comparable to those noted in other studies.16,19,20,21 This further supports the acceptability of our program. The pregnancy rate within one year of LARC discontinuation is high in our cohort, despite the vast majority starting another hormonal method. Furthermore, pregnancy rates are a conservative estimate given that not all patients had follow-up available for a full year after method discontinuation.
Other studies have shown a similar, although weaker, association between history of STI and increased risk of LARC discontinuation.19,22 One possible reason for this correlation is that these women may have ambivalence towards pregnancy and therefore practice more unprotected sex. Pregnancy ambivalence refers to contradictory or varying attitudes regarding pregnancy that do not fit neatly into an intended versus unintended dichotomy. It has been associated with reduced odds of using contraception or condoms and increased likelihood of pregnancy.23-27 Ambivalent attitudes have also been shown to be more likely in black and Latina adolescents, those from single parent families, and those with mothers with lower levels of educational attainment, features that many of our patients share.26 Thus ambivalence may mediate the association between these demographic characteristics and risk of unintended pregnancy. Research is needed regarding whether there is an association between pregnancy ambivalence and early LARC discontinuation. In addition, providers and/or parents may see women with a history of STI as being at high risk for unintended pregnancy and may counsel them differently. Further provider training in contraceptive counseling and reproductive life planning discussions may be beneficial.
Data regarding reasons for LARC discontinuation in this specific age group are limited.20, 28, 29 Consistent with prior studies as well as data from older women, abnormal bleeding was the most common reason given for implant removal.19,30,31,32 One interesting finding was the relatively high percentage of women who discontinued the implant due to perceived weight gain. Data on actual weight gain were not collected in this analysis due to the retrospective design and are limited in general.33 The proportion of women who discontinued the implant due to desire for pregnancy was also surprisingly high. In another study, only 3% of women of reproductive age who requested removal before six months did so due to desire for pregnancy.19 Perhaps this difference is a further reflection of the dynamic reproductive life plans or pregnancy ambivalence in this patient population.27 For IUD users, expulsion was the most common reason for discontinuation. The expulsion rate was within the 5-22% range for this age group described by other studies.34,35
In general, more adolescent and young adult women in this program received implants than IUDs with no one choosing the copper IUD. Reasons for this are unclear given the retrospective nature of the analysis but results are consistent with other findings that suggest that adolescents may prefer the implant to the IUD, in contrast to the general population.36 One hypothesis is that many of these women had never had a pelvic exam so IUD insertion may be more frightening than implant insertion. A practical issue is that more providers were trained to place implants than IUDs so more women who desired IUDs may have been referred to another clinic due to scheduling constraints, or women may have chosen the more accessible option. Training more providers in IUD placement may further increase access and choice.
Overall, our results support the safety of provision of LARC to adolescents and young adult women in a primary care setting. A strength of this study is that it reflects real-world experience in an urban primary care clinic with patients at high risk of unintended pregnancy. As the Affordable Care Act mitigates barriers related to cost, access issues related to provider training and convenience for patients will move to the forefront. Our program combats these obstacles. The completeness of the data available was excellent due to meticulous charting and prospective collection of initial data by the clinic nurse case manager. Use of a Cox model strengthened the analysis because it is a semi-parametric model that does not assume a constant hazard over time.
A limitation is that this program has only been in place for three years, although long-term follow-up is planned. This meant that our sample size was small and many women were not followed for more than two years. However, the data analysis plan accounted for this. With survival data, an assumption is made that subjects are censored for reasons independent from the event of interest. So although uncommon for this clinic population, if patients were lost to follow-up because they sought care elsewhere for LARC removal, this would bias our data. The unique economic and political context of the clinical setting may also limit generalizability to other settings. Lastly, the retrospective nature of this study and the fact that data were obtained from the medical record introduce potential information bias. These methods also limit our ability to explain some of our findings such as reason for choosing a particular LARC method.
In summary, our experience indicates that LARC provision in a primary care pediatric setting with adequate provider training and multidisciplinary collaboration is associated with low contraceptive discontinuation. This kind of program could easily be replicated in similar settings without need for outside funding and supports the expansion of training adolescent and pediatric providers in LARC provision.
Acknowledgements
There was no internal or external funding for the implementation of the project. The evaluation of this project was supported in part by federal funds (P20MD000198) from the National Institute of Minority Health & Health Disparities, National Institute of Child Health and Human Development (T23HD52459), and the Health Resources & Services Administration (T71MC08054). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Those who have contributed significantly to the work are listed as authors above.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Martinez G, Copen CE, Abma JC. Teenagers in the United States: sexual activity, contraceptive use, and childbearing, 2006-2010 national survey of family growth. Vital Health Stat. 2011 Oct 23;(31):1–35. 31. [PubMed] [Google Scholar]
- 2.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006 Jun;38(2):90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 3.Cohn M, McDaniels AK. Teen pregnancies in Baltimore drop by a third. [June 22, 2016];Baltimore Sun. 2015 Feb 24; Available at: http://www.baltimoresun.com/health/maryland-health/bs-hs-teen-pregnancy-20150224-story.html.
- 4.Beilenson PL, Miola ES, Farmer M. Politics and practice: introducing Norplant into a school-based health center in Baltimore. Am J Public Health. 1995 Mar;85(3):309–11. doi: 10.2105/ajph.85.3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baltimore City Health Department [June 22, 2016];Teen Pregnancy Prevention. Available at: http://health.baltimorecity.gov/node/170.
- 6.Committee on Adolescence American Academy of Pediatrics. Contraception for adolescents. Pediatrics. 2014 Oct;134(4):e1244–56. doi: 10.1542/peds.2014-2299. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group, The American College of Obstetricians and Gynecologists Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2012 Oct;120(4):983–8. doi: 10.1097/AOG.0b013e3182723b7d. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention US selected practice recommendations for contraceptive use, 2013: adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use. MMWR Recomm Rep. (2nd Edition.) 2013;62(RR-5):1–60. [PubMed] [Google Scholar]
- 9.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012 Dec;120(6):1298–305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. [June 22, 2016];ACGME Program Requirements for Graduate Medical Education in Pediatrics. 2015 Jul 1; Available at: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/320_pediatrics_07012015.pdf.
- 11. [June 22, 2016];ACGME Program Requirements for Graduate Medical Education in Adolescent Medicine. 2013 Jul 1; Available at: http://www.acgme.org/Portals/0/PFAssets/2013-PR-FAQ PIF/321_adolescent_med_peds_07012013.pdf.
- 12.Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15-44. NCHS Data Brief. 2015 Feb;(188):1–8. [PubMed] [Google Scholar]
- 13.Secura GM, Madden T, McNicholas C, Mullersman J, Buckel CM, Zhao Q, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med. 2014 Oct 2;371(14):1316–23. doi: 10.1056/NEJMoa1400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014 Sep;46(3):125–32. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 15. Onyewuchi et. al., unpublished work.
- 16.Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011 May;117(5):1105–13. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–41. [Google Scholar]
- 18.StataCorp. Stata Statistical Software: Release 13. StataCorp LP.; College Station, TX: 2013. [Google Scholar]
- 19.Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet Gynecol. 2013 Dec;122(6):1214–21. doi: 10.1097/01.AOG.0000435452.86108.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Obijuru L, Bumpus S, Auinger P, Baldwin CD. Etonogestrel Implants in Adolescents: Experience, Satisfaction, and Continuation. J Adolesc Health. 2016 Mar;58(3):284–9. doi: 10.1016/j.jadohealth.2015.10.254. [DOI] [PubMed] [Google Scholar]
- 21.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O'neil-Callahan M, Peipert JF, Zhao Q, Madden T, Secura G. Twenty-four-month continuation of reversible contraception. Obstet Gynecol. 2013 Nov;122(5):1083–91. doi: 10.1097/AOG.0b013e3182a91f45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bruckner H, Martin A, Bearman PS. Ambivalence and pregnancy: Adolescents’ attitudes, contraceptive use and pregnancy. Perspect Sex Reprod Health. 2004;36:248e57. doi: 10.1363/psrh.36.248.04. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz A. Defining new categories of pregnancy intention in African-American women. Women's health issues. 2010;20:371e9. doi: 10.1016/j.whi.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Crosby RA, Diclemente RJ, Wingood GM, et al. Adolescents’ ambivalence about becoming pregnant predicts infrequent contraceptive use: A prospective analysis of nonpregnant African American females. Am J Obstet Gynecol. 2002;186:251e2. doi: 10.1067/mob.2002.120081. [DOI] [PubMed] [Google Scholar]
- 26.Jaccard J, Dodge T, Dittus P. Do adolescents want to avoid pregnancy? Attitudes toward pregnancy as predictors of pregnancy. J Adolesc Health. 2003 Aug;33(2):79–83. doi: 10.1016/s1054-139x(03)00134-4. [DOI] [PubMed] [Google Scholar]
- 27.Miller WB, Trent M, Chung SE. Ambivalent childbearing motivations: predicting condom use by urban, African-American, female youth. J Pediatr Adolesc Gynecol. 2014 Jun;27(3):151–60. doi: 10.1016/j.jpag.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 28.Harel Z, Frank M, Kollar L, Rauh J. Adolescents’ reasons for and experience after discontinuation of the long-acting contraceptives Depo-Provera and Norplant. J Adolesc Health. 1996;19:118–23. doi: 10.1016/1054-139X(95)00322-J. [DOI] [PubMed] [Google Scholar]
- 29.Lara-Torre E, Spotswood L, Correia N, Weiss PM. Intrauterine contraception in adolescents and young women: a descriptive study of use, side effects, and compliance. J Pediatr Adolesc Gynecol. 2011 Feb;24(1):39–41. doi: 10.1016/j.jpag.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 30.Berenson AB, Tan A, Hirth JM. Complications and continuation rates associated with 2 types of long-acting contraception. Am J Obstet Gynecol. 2015 Jun;212(6):761.e1, 761.e8. doi: 10.1016/j.ajog.2014.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong RC, Bell RJ, Thunuguntla K, McNamee K, Vollenhoven B. Implanon users are less likely to be satisfied with their contraception after 6 months than IUD users. Contraception. 2009 Nov;80(5):452–6. doi: 10.1016/j.contraception.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 32.Harvey C, Seib C, Lucke J. Continuation rates and reasons for removal among Implanon users accessing two family planning clinics in Queensland, Australia. Contraception. 2009 Dec;80(6):527–32. doi: 10.1016/j.contraception.2009.05.132. [DOI] [PubMed] [Google Scholar]
- 33.Lopez LM, Edelman A, Chen M, Otterness C, Trussell J, Helmerhorst FM. Progestin-only contraceptives: effects on weight. Cochrane Database Syst Rev. 2013 Jul 2;7:CD008815. doi: 10.1002/14651858.CD008815.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deans EI, Grimes DA. Intrauterine devices for adolescents: a systematic review. Contraception. 2009;79:418–23. doi: 10.1016/j.contraception.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Lyus R, Lohr P, Prager S. Use of the Mirena LNG-IUS and Paragard CuT380A intrauterine devices in nulliparous women. Board of the Society of Family Planning. Contraception. 2010;81:367–71. doi: 10.1016/j.contraception.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 36.Mestad R, Secura G, Allsworth JE, Madden T, Zhao Q, Peipert JF. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the Contraceptive CHOICE Project. Contraception. 2011;84:493–8. doi: 10.1016/j.contraception.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]