Abstract
Purpose
Intraductal papilloma (IDP) is a benign breast disease with malignant potential, for which complete surgical excision is usually recommended. The aim of the present study was to investigate predictive factors for upgrading patients with a benign papillary lesion (BPL).
Methods
This study was an observational study using a prospectively collected cohort. In total, 13,049 patients who underwent a core needle biopsy (CNB) for a breast lesion between January 2009 and May 2015 were enrolled. We reviewed all patients with pathologically confirmed BPL from a CNB.
Results
Surgical treatment was performed for 363 out of a total of 592 lesions. According to the pathological differences, the lowest upgrade rate was shown in IDP without atypia (without atypia, 6.0%; with atypia, 26.8%; papillary neoplasm, 31.5%; p<0.001). The univariate analysis showed that, in IDP without atypia, the age at diagnosis, size of BPL on ultrasonography, and density on mammography were associated with upgrading. The multivariate analysis revealed that age >54 years and lesion size >1 cm were significantly associated with upgrade to malignancy (odds ratio [OR]=4.351, p=0.005 and OR=4.236, p=0.001, respectively).
Conclusion
The indications for surgical treatment can be defined as age >54 years and mass size >1 cm, even in IDP without atypia in the CNB results; this also includes cases of IDP with atypia or papillary neoplasm. Therefore, we suggest that close observation without surgery is sufficient for younger women with a small IDP without atypia.
Keywords: Atypia, Biopsy, Breast neoplasms, Intraductal papilloma, Large core needle
INTRODUCTION
Intraductal papilloma (IDP) is a relatively common benign tumor that forms in the breast and requires surgical treatment. When a core needle biopsy (CNB) of the breast identifies a papillary lesion (PL), surgical treatment is performed because of the malignant potency of these lesions [1,2,3].
Traditionally, a benign papillary lesion (BPL) is generally treated with a complete excision. However, doubts have been raised that surgical treatment is necessary for all patients with BPLs [4,5,6,7]. Many previous studies have attempted to determine the necessity of surgical treatment in patients with IDP [2,6,7,8]. In fact, the upgrade rate of BPLs is the most accurate way to compare the results before and after a surgical procedure. However, only a few studies fulfill the necessary conditions. In several small case studies comparing surgical results, 0% to 19% of BPLs were upgraded to malignancy [5,6,7,9].
Based on pathologic findings, PLs of the breast are divided into benign IDP, with or without atypia, and papillary carcinoma. In recent years, it has been argued that the potential for malignancy could be revealed using immunohistochemistry or several histopathological molecular biomarkers on the preoperative CNB from the PL [1,10,11,12,13]. Some studies have also analyzed several radiological characteristics to predict the malignant risk of a BPL [14,15,16]. Diagnostic accuracy and methods to determine the malignant potency of PLs are more accurate today than in the past. Therefore, surgical excision is not always necessary [2,7,16].
The present study investigated predictive factors for upgrading lesions in a large population of patients with BPLs from a single institution using a core biopsy.
METHODS
Patients
This study was an observational study using a prospectively collected cohort. In total, 13,049 patients who underwent a CNB for a breast lesion between January 2009 and May 2015 were enrolled. All patients had a pathologically confirmed BPL from a CNB and were surgically treated.
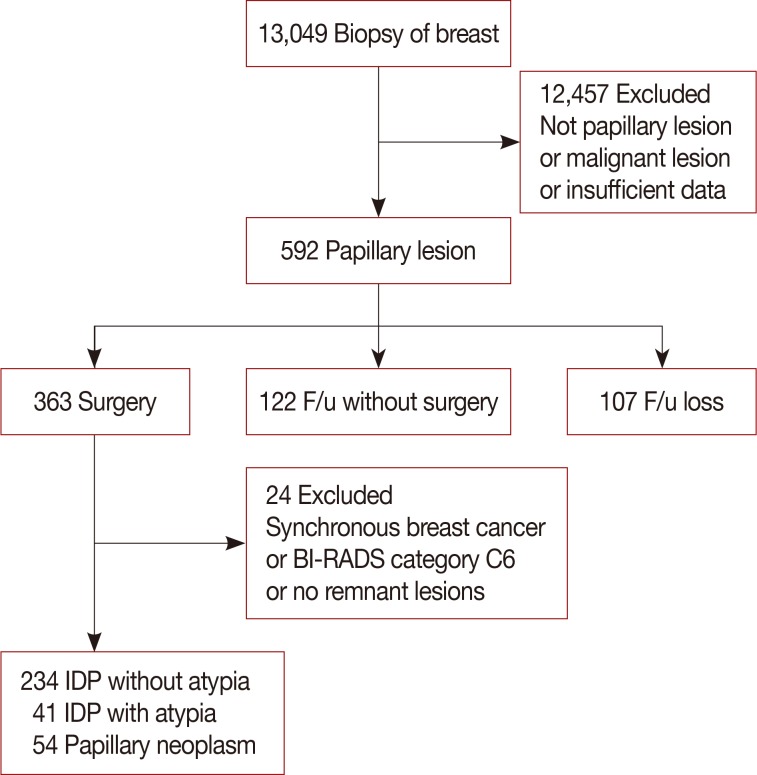
We analyzed data in detail, including patient symptoms at the time of diagnosis, past history, and information on family history of breast cancer for the 592 cases identified as BPL. All patients were evaluated using radiologic examinations (breast ultrasonography [USG] and mammography [MMG]) prior to surgery. We also reviewed several radiologic findings. Of the 592 cases, 363 cases underwent surgery; 122 cases were followed up without surgery; and 107 cases did not attend a follow-up appointment (Figure 1). Our study was approved by the Institutional Review Board (KC16RISI0471).
Figure 1. The schematic diagram outlines the process for selecting eligible cases for analysis.
F/u=follow-up; BI-RADS=Breast Imaging Reporting and Data System; IDP=intraductal papilloma.
Treatment and follow-up
All surgeries were performed by three experienced breast surgeons. All biopsies were performed by two experienced radiologists prior to surgery. We recommended surgery for all PLs that were diagnosed during the study period. However, if the size of the biopsy lesion was small, a follow-up breast USG was performed within 3 to 6 months and surgery was recommended if remnant lesions were observed. One of three types of surgical treatments was performed: excision, wide excision, or vacuum-assisted excision, based on each patient's preference. Predominantly, excision or vacuum-assisted excision was performed when resection margin status assessment was not required. If assessment of the surgical resection margin was required, a wide excision was considered. However, surgical treatment was not performed if the patient refused. When a patient was diagnosed with breast cancer at the same time, the surgery was performed for breast cancer treatment. In addition, further treatment for breast cancer was conducted properly when malignancy was confirmed with postoperative pathology.
All patients were followed-up from the date of diagnosis of the BPL until September 2015, when data were analyzed for this study.
Definitions
Mass size was defined as the longest diameter of the lesion as measured on breast USG before surgery and the Breast Imaging Reporting and Data System (BI-RADS) category was dependent on the breast USG results. A lesion located within 2 cm of the nipple was defined as a central location, and any location further away was defined as a peripheral location, on breast USG.
Surgery within 6 months after diagnosis was defined as a surgical treatment case. When a patient did not have any records related to the breast, including records in another department, after diagnosis, this was defined as follow-up loss.
Pathologically, papillary neoplasms include invasive papillary carcinoma, IDP, intraductal papillary carcinoma, and encapsulated papillary carcinoma, according to the World Health Organization classification, fourth edition. In fact, lesions are diagnosed as papillary neoplasms when an accurate diagnosis is impossible but papillary architecture is confirmed on CNB. If atypical epithelial proliferation was confirmed within the papilloma, it was defined as IDP with atypia or, if not, as IDP without atypia.
When postoperative pathologic results showed ductal carcinoma in situ (DCIS) or invasive cancer compared with the preoperative BPL results, it was defined as an upgrading lesion.
Statistics
Statistical analyses were performed using the IBM SPSS version 20.0 software (IBM Corp., Armonk, USA). We used chi-square tests or t-tests to compare categorical and continuous variables, respectively, between the two groups. Similar statistics were applied to the three stratified groups. The results are described as the means±the standard deviations (SDs) as numbers (%) and were considered statistically significant at p<0.05. A multivariate binary logistic regression model was used to analyze variables found to be statistically significant (p<0.1) in univariate analyses. The results are represented as odds ratios (ORs) with 95% confidence intervals.
RESULTS
Of the 13,049 biopsies, a total of 592 cases (571 patients) were confirmed as a BPL by a core biopsy of the breast. Of these, a surgical treatment was performed for 363 lesions. Three hundred twenty-nine eligible cases remained after excluding 20 cases with synchronous breast cancer (including unilateral and/or contralateral) and/or BI-RADS category 6 lesions, and 14 cases in which there were no remnant lesions in the postoperative pathologic results (Figure 1).
Based on the pathologic results from the CNB prior to surgery, the BPLs were classified into three groups: IDP without atypia (n=234), IDP with atypia (n=41), or papillary neoplasm (n=54). After comparing the groups, the lowest upgrade rate was found in the IDP without atypia group (p<0.001) (Table 1).
Table 1. Upgrade rate of the papillary lesions according to the pathological differences.
| Upgrade | IDP without atypia (n = 234) No. (%) |
IDP with atypia (n = 41) No. (%) |
Papillary neoplasm (n = 54) No. (%) |
p-value |
|---|---|---|---|---|
| Not upgrade | 220 (94.0) | 30 (73.2) | 37 (68.5) | < 0.001 |
| Upgrade | 14 (6.0) | 11 (26.8) | 17 (31.5) |
IDP=intraductal papilloma.
Clinicoradiologic features according to upgrade status
Only 14 of the 234 cases were confirmed as upgrade to malignancy, including five cases of invasive cancer and nine cases of DCIS. The mean age at diagnosis in the upgrade group was 54.8±11.9 years, which was approximately 10 years older than the mean age of the not upgraded group (p<0.001). Based on the clinical age of menopause, we set the appropriate age cut-off value at 55 years. The age at diagnosis was also significantly different between the two groups (p=0.001).
Comparison between the preoperative radiologic results of the two groups revealed only two factors that were significantly different. Upgrade to malignancy was associated with a larger sized lesion on USG and lower density on MMG (p=0.002 and p<0.001, respectively). On the other hand, multifocality, BI-RADS category, and lesion location were not associated with an upgrade. There was approximately 95% concordance between radiologic and pathologic results in both groups, meaning that there was no significant difference in concordance (Table 2).
Table 2. Clinicoradiologic features depending on the upgrade in intraductal papilloma without atypia in the univariate analysis.
| Characteristic | Not upgrade (n = 220) No. (%) |
Upgrade (n = 14) No. (%) |
p-value |
|---|---|---|---|
| Age (yr) | |||
| Mean ± SD | 45.1 ± 10.2 | 54.8 ± 11.9 | < 0.001 |
| < 55 | 185 (84.1) | 7 (50.0) | 0.001 |
| ≥ 55 | 35 (15.9) | 7 (50.0) | |
| Mass size (cm) | |||
| Mean ± SD | 1.1 ± 1.2 | 1.6 ± 1.0 | 0.085 |
| ≤1 | 141 (64.1) | 4 (28.6) | 0.002 |
| >1 | 79 (35.9) | 10 (71.4) | |
| Multifocality | 0.630 | ||
| Negative | 159 (72.3) | 10 (71.4) | |
| Positive | 61 (27.7) | 4 (28.6) | |
| BI-RADS category | 0.528 | ||
| 0 | 1 (0.5) | 0 | |
| 1 | 1 (0.5) | 0 | |
| 2 | 2 (0.9) | 0 | |
| 3 | 36 (16.4) | 2 (14.3) | |
| 4 | 177 (80.5) | 12 (85.7) | |
| 5 | 3 (1.4) | 0 | |
| Breast density* | < 0.001 | ||
| 1 | 6 (2.7) | 0 | |
| 2 | 26 (12.0) | 7 (50.0) | |
| 3 | 107 (48.6) | 6 (42.9) | |
| 4 | 81 (36.8) | 1 (7.1) | |
| Location | 0.493 | ||
| Central | 119 (54.1) | 6 (42.9) | |
| Peripheral | 101 (45.9) | 8 (57.1) | |
| Concordance | 1.000 | ||
| Concord | 208 (94.5) | 13 (92.9) | |
| Discord | 12 (5.5) | 1 (7.1) | |
| Palpability | 0.092 | ||
| Negative | 188 (85.5) | 10 (71.4) | |
| Positive | 32 (14.5) | 4 (28.6) | |
| Nipple discharge | 0.085 | ||
| Negative | 155 (70.5) | 12 (85.7) | |
| Positive | 65 (29.5) | 2 (14.3) | |
| Hx. of benign breast disease | 0.852 | ||
| Negative | 194 (88.2) | 13 (92.9) | |
| Positive | 26 (11.8) | 1 (7.1) | |
| Hx. of breast cancer | 1.000 | ||
| Negative | 215 (97.7) | 14 (100) | |
| Positive | 5 (2.3) | 0 | |
| F/Hx. of breast cancer | 1.000 | ||
| Negative | 201 (91.4) | 13 (92.9) | |
| Positive | 19 (8.6) | 1 (7.1) |
BI-RADS =Breast Imaging Reporting and Data System; Hx. =history; F/Hx.=family history.
*Mammographic density by BI-RADS classification system (breast density: type 1, almost entirely fat, glandular tissue is less than 25%; type 2, scattered fibroglandular tissues, ranging from 25% to 50% of the breast; type 3, heterogeneously dense parenchyma, ranging 51% to 75% of the breast tissue; type 4, the breast contains greater than 75% glandular and fibrous tissue).
In addition, in the upgrade group, there was a trend towards a higher proportion of palpable masses and lower proportion of nipple discharge symptoms (including serous or bloody discharge) at diagnosis. However, these trends were not statistically significant (p=0.092 and p=0.085, respectively). A past history of benign breast disease, breast cancer, or a family history of breast cancer was not significantly different between the two groups.
The multivariate analysis revealed that age >54 years and lesion size >1 cm were significantly associated with upgrade to malignancy (OR=4.351, p=0.005 and OR=4.236, p=0.001, respectively) (Table 3).
Table 3. Factors influencing the upgrade to malignancy in intraductal papilloma without atypia in the multivariate analysis.
| Characteristic | OR | 95% CI | p-value |
|---|---|---|---|
| Age ≥ 55 yr | 4.351 | 1.576–12.071 | 0.005 |
| Size > 1 cm | 4.236 | 1.012–10.256 | 0.001 |
| Breast density* ( > 50%) | 0.481 | 0.133–1.529 | 0.107 |
| Palpable mass | 0.590 | 0.223–2.605 | 0.632 |
| Nipple discharge | 1.952 | 0.642–11.062 | 0.285 |
OR=odds ratio; CI=confidence interval.
*Mammographic density by Breast Imaging Reporting and Data System classification system (breast density: type 1, almost entirely fat, glandular tissue is less than 25%; type 2, scattered fibroglandular tissues, ranging from 25% to 50% of the breast; type 3, heterogeneously dense parenchyma, ranging 51% to 75% of the breast tissue; type 4, the breast contains greater than 75% glandular and fibrous tissue).
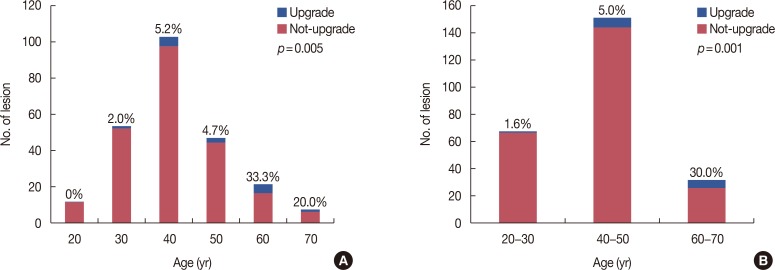
Upgrade rate according to the age-specific distribution
According to the age-specific distribution, IDP was most commonly diagnosed in patients in their 40s (41%). The upgrade rate increased in elderly patients. When age was divided into 10-year intervals, the highest upgrade rate was seen in patients in their 60s (33.3%, p=0.005). When the age was divided into 20-year intervals, the highest upgrade rate was observed in patients in their 60s and 70s (30.0%, p=0.001) (Figure 2).
Figure 2. Distribution of intraductal papilloma depending on the age at the diagnosis. Patients age was divided into 10-year (A) or 20-year (B) intervals. Blue color represents upgrade to malignancy, and red color represents absence of upgrade, by comparing the pathologic results before and after surgery.
Upgrade rate and mass size changes in patients who did not undergo an initial surgery
There was confirmed available follow-up data for 122 cases of the 229 cases that did not undergo an initial surgery for BPL. During the mean follow-up period of 27.6±25.1 months, the mass size on the breast USG increased in only 19 cases (15.6 %); it did not increase (remained the same or decreased) in 103 cases. The mean size change on the breast USG was -0.18±0.45 cm. The value was different between the two groups “increase” group, +0.42±0.21 cm; “no increase” group, -0.29±0.70 cm. Eighteen cases underwent a surgical excision during the follow-up period, including eight cases (42.0%) in the “increase” group and 10 cases (10.0%) in the “no increase” group. Upgrade to malignancy was identified in only two cases, both in the “increase” group. In other words, the upgrade rate in the “increase” group was 25.0% and 0% in the “no increase” group. Additionally, atypical ductal hyperplasia was found in one case in each group (Table 4).
Table 4. Presentation and summary of the upgrade cases, including atypical ductal hyperplasia, in the follow-up cases.
| Initial | Postoperative | ||||||
|---|---|---|---|---|---|---|---|
| Date of Dx. (Age, yr) | Pathology | Size (cm) | Breast density* | Operation (date) | Size (cm)† | Final pathology | |
| Case 1 | 06/28/2009 (50) | IDP | 0.5 | 3 | WE c SLNB (09/28/2012) | 1.9 (+1.4) | IDC |
| Case 2 | 01/06/2012 (63) | PN | 1.9 | 3 | WE c SLNB (04/02/2013) | 3.4 (+1.5) | IDC |
| Case 3 | 10/05/2009 (38) | IDP | 0.5 | 4 | Excision (10/26/2010) | 0.5 (0) | ADH |
| Case 4 | 07/21/2011 (35) | IDP | 0.4 | 4 | Excision (10/13/2015) | 1.2 (+0.8) | ADH |
Dx.=diagnosis; IDP=intraductal papilloma; WE c SLNB=wide excision with sentinel lymph node biopsy; IDC=invasive ductal carcinoma; PN=papillary neoplasm; ADH=atypical ductal hyperplasia.
*Mammographic density by Breast Imaging Reporting and Data System classification system (breast density: type 1, almost entirely fat, glandular tissue is less than 25%; type 2, scattered fibroglandular tissues, ranging from 25% to 50% of the breast; type 3, heterogeneously dense parenchyma, ranging 51% to 75% of the breast tissue; type 4, the breast contains greater than 75% glandular and fibrous tissue); †Size change=the size of lesion at the time of operation–the size of lesion at the time of diagnosis.
DISCUSSION
In this study, we determined the upgrade rate for BPLs from CNB results and the predictive factors for upgrade to malignancy. Of the different BPL types, we determined that IDP with atypia and papillary neoplasms on a CNB should be treated with surgical excision to preclude the malignant potential; the confirmed upgrade rates were as high as 26.8% and 31.5%, respectively. On the other hand, IDP without atypia was considered to have a low malignant potential with an upgrade rate of 6.0%. Of the 234 cases of IDP without atypia diagnosed from a core biopsy that underwent surgical treatment, the significant upgrade-related factors were older age at diagnosis (>54 years) and greater mass size (>1 cm). Therefore, traditional surgical treatment should be performed when elderly patients present with larger masses, even in IDP without atypia. Surgical treatment may be omitted in younger woman with smaller IDP without atypia on CNB.
IDP is a benign breast disease with a variety of clinical presentations. Common symptoms include nipple discharge (spontaneous or persistent, or serous or bloody) or a palpable mass. It is also not uncommon for an asymptomatic case to be diagnosed during a radiological screening examination. The relationship between these clinical symptoms and the BPL upgrade rate has been debated in the literature [3,17,18]. The present study analyzed the correlation between clinical symptoms and upgrade to malignancy after collecting information on nipple discharge and palpable masses for IDP without atypia. In the univariate analysis, the upgrade group exhibited a trend toward a higher incidence of palpable masses and lower rate of nipple discharge at diagnosis. However, these trends were not significant in the multivariate analysis.
Papillary breast lesions are divided into benign IDP without atypia, benign IDP with atypia, and malignancy (noninvasive carcinoma and invasive carcinoma) that appears as a broad spectrum pathologically. There is no disagreement that IDP with atypia has a high upgrade rate and high malignancy risk. However, the upgrade rate has been variably reported in IDP without atypia, and the best method to effectively treat IDP without atypia is still uncertain [1,6,7,8,19]. Nakhlis et al. [7] reported an upgrade rate of 6%, and based on this, they suggested that surgical treatment may not be necessary for IDP without atypia. They argued that careful observation may be sufficient if a patient had neither a palpable mass nor radiologic-pathologic discordance. A meta-analysis published in 2013 described the risk factors associated with the underestimation of PL, such as atypia and positive mammographic findings [20].
In recent years, histopathological efforts to differentiate between benign or malignant PLs prior to surgery have been reported. These methods included immunohistochemistry for several molecular biomarkers and cell cycle markers (such as cytokeratin 5/6, p63, and Ki-67) and resulted in a more accurate diagnosis [1,10,12,13,21,22]. In addition, these studies reported that features such as microcalcification or high density on MMG, larger mass size on USG, radiologic-pathologic discordance, and older age, could predict the malignant risk of BPL. As a result, the number of recommendations for surgical excision for PL was significantly reduced. The accuracy of image-guided large core biopsies has improved with higher sensitivity and specificity. However, in order to omit a surgical excision, radiologic-pathologic concordance and an accurate biopsy to obtain sufficient tissue prior to surgery is necessary. In addition, these earlier studies had several imitations, including relatively small study sizes or unconfirmed pathological results from surgery for many cases. Future research with larger studies and sufficient surgical outcomes will be necessary to address these limitations [14,15,16,17,20,23,24].
The awareness of IDP is changing; therefore, changes must be made to the diagnostic and treatment approaches. Surgical treatment is still needed to rule out malignant potential in a PL, although the importance of surgery has been reduced. Therefore, it is important to properly select patients for whom surgical treatment is necessary. According to the current study, elderly patients with larger lesions are encouraged to consider surgical treatment, even if the BPL is diagnosed as IDP without atypia.
In the follow-up data for the patients who did not undergo an initial surgery, increased mass size was shown in some patients (15.6%), but the upgrade rate was only 1.6% (2/122 patients). Two upgrading patients with confirmed malignancy after surgery were elderly and belonged to the group with increased tumor size. Although the follow-up period was inadequate, the results showed that close observation without surgery is safe because of the very low upgrade rate.
There were a number of limitations in this study. The number of patients lost to follow-up was substantial (n=107). However, we also followed-up and analyzed a large number of patients (n=122). Additionally, we used a well-organized prospective data collection that included a wealth of information. The analysis was performed to target a large number of cases for which the surgical results were available in a single institution.
We proposed highly selective criteria for surgical excision because we analyzed the biopsy results from patients with IDP without atypia in detail. These patients were then classified into three groups. Additionally, this is the first report that included the follow-up data for patients who did not undergo an initial surgery to confirm that the upgrade rate in BPL is not high. The results of this study suggest that our criteria have utility in selecting patients for surgical treatment.
In conclusion, surgical treatment for BPL should be carefully determined. Indications for surgical treatment include age >54 year and mass size >1 cm, even in IDP without atypia; this also includes IDP with atypia or papillary neoplasm in the core biopsy results. Therefore, we suggest that close observation without surgery is sufficient for younger woman with smaller IDP without atypia. Of course, surgical excision should be considered when the mass size increases in elderly patients during the observation.
Footnotes
CONFLICT OF INTEREST: The authors declare that they have no competing interests.
References
- 1.Shamonki J, Chung A, Huynh KT, Sim MS, Kinnaird M, Giuliano A. Management of papillary lesions of the breast: can larger core needle biopsy samples identify patients who may avoid surgical excision? Ann Surg Oncol. 2013;20:4137–4144. doi: 10.1245/s10434-013-3191-3. [DOI] [PubMed] [Google Scholar]
- 2.Nayak A, Carkaci S, Gilcrease MZ, Liu P, Middleton LP, Bassett RL, Jr, et al. Benign papillomas without atypia diagnosed on core needle biopsy: experience from a single institution and proposed criteria for excision. Clin Breast Cancer. 2013;13:439–449. doi: 10.1016/j.clbc.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rizzo M, Linebarger J, Lowe MC, Pan L, Gabram SG, Vasquez L, et al. Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up. J Am Coll Surg. 2012;214:280–287. doi: 10.1016/j.jamcollsurg.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Mercado CL, Hamele-Bena D, Oken SM, Singer CI, Cangiarella J. Papillary lesions of the breast at percutaneous core-needle biopsy. Radiology. 2006;238:801–808. doi: 10.1148/radiol.2382041839. [DOI] [PubMed] [Google Scholar]
- 5.Skandarajah AR, Field L, Yuen Larn Mou A, Buchanan M, Evans J, Hart S, et al. Benign papilloma on core biopsy requires surgical excision. Ann Surg Oncol. 2008;15:2272–2277. doi: 10.1245/s10434-008-9962-6. [DOI] [PubMed] [Google Scholar]
- 6.Ahmadiyeh N, Stoleru MA, Raza S, Lester SC, Golshan M. Management of intraductal papillomas of the breast: an analysis of 129 cases and their outcome. Ann Surg Oncol. 2009;16:2264–2269. doi: 10.1245/s10434-009-0534-1. [DOI] [PubMed] [Google Scholar]
- 7.Nakhlis F, Ahmadiyeh N, Lester S, Raza S, Lotfi P, Golshan M. Papilloma on core biopsy: excision vs. observation. Ann Surg Oncol. 2015;22:1479–1482. doi: 10.1245/s10434-014-4091-x. [DOI] [PubMed] [Google Scholar]
- 8.Renshaw AA, Derhagopian RP, Tizol-Blanco DM, Gould EW. Papillomas and atypical papillomas in breast core needle biopsy specimens: risk of carcinoma in subsequent excision. Am J Clin Pathol. 2004;122:217–221. doi: 10.1309/K1BN-JXET-EY3H-06UL. [DOI] [PubMed] [Google Scholar]
- 9.Jaffer S, Nagi C, Bleiweiss IJ. Excision is indicated for intraductal papilloma of the breast diagnosed on core needle biopsy. Cancer. 2009;115:2837–2843. doi: 10.1002/cncr.24321. [DOI] [PubMed] [Google Scholar]
- 10.Yang Y, Suzuki K, Abe E, Li C, Uno M, Akiyama F, et al. The significance of combined CK5/6 and p63 immunohistochemistry in predicting the risks of subsequent carcinoma development in intraductal papilloma of the breast. Pathol Int. 2015;65:81–88. doi: 10.1111/pin.12248. [DOI] [PubMed] [Google Scholar]
- 11.Rakha EA. Morphogenesis of the papillary lesions of the breast: phenotypic observation. J Clin Pathol. 2016;69:64–69. doi: 10.1136/jclinpath-2015-203191. [DOI] [PubMed] [Google Scholar]
- 12.Hoshikawa S, Sano T, Hirato J, Oyama T, Fukuda T. Immunocytochemical analysis of p63 and 34betaE12 in fine needle aspiration cytology specimens for breast lesions: a potentially useful discriminatory marker between intraductal papilloma and ductal carcinoma in situ. Cytopathology. 2016;27:108–114. doi: 10.1111/cyt.12244. [DOI] [PubMed] [Google Scholar]
- 13.Pathmanathan N, Albertini AF, Provan PJ, Milliken JS, Salisbury EL, Bilous AM, et al. Diagnostic evaluation of papillary lesions of the breast on core biopsy. Mod Pathol. 2010;23:1021–1028. doi: 10.1038/modpathol.2010.81. [DOI] [PubMed] [Google Scholar]
- 14.Jagmohan P, Pool FJ, Putti TC, Wong J. Papillary lesions of the breast: imaging findings and diagnostic challenges. Diagn Interv Radiol. 2013;19:471–478. doi: 10.5152/dir.2013.13041. [DOI] [PubMed] [Google Scholar]
- 15.Carder PJ, Garvican J, Haigh I, Liston JC. Needle core biopsy can reliably distinguish between benign and malignant papillary lesions of the breast. Histopathology. 2005;46:320–327. doi: 10.1111/j.1365-2559.2005.02082.x. [DOI] [PubMed] [Google Scholar]
- 16.Puglisi F, Zuiani C, Bazzocchi M, Valent F, Aprile G, Pertoldi B, et al. Role of mammography, ultrasound and large core biopsy in the diagnostic evaluation of papillary breast lesions. Oncology. 2003;65:311–315. doi: 10.1159/000074643. [DOI] [PubMed] [Google Scholar]
- 17.Patel BK, Falcon S, Drukteinis J. Management of nipple discharge and the associated imaging findings. Am J Med. 2015;128:353–360. doi: 10.1016/j.amjmed.2014.09.031. [DOI] [PubMed] [Google Scholar]
- 18.Cheng TY, Chen CM, Lee MY, Lin KJ, Hung CF, Yang PS, et al. Risk factors associated with conversion from nonmalignant to malignant diagnosis after surgical excision of breast papillary lesions. Ann Surg Oncol. 2009;16:3375–3379. doi: 10.1245/s10434-009-0637-8. [DOI] [PubMed] [Google Scholar]
- 19.Shiino S, Tsuda H, Yoshida M, Jimbo K, Asaga S, Hojo T, et al. Intraductal papillomas on core biopsy can be upgraded to malignancy on subsequent excisional biopsy regardless of the presence of atypical features. Pathol Int. 2015;65:293–300. doi: 10.1111/pin.12285. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs TW, Connolly JL, Schnitt SJ. Nonmalignant lesions in breast core needle biopsies: to excise or not to excise? Am J Surg Pathol. 2002;26:1095–1110. doi: 10.1097/00000478-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Loh SF, Cooper C, Selinger CI, Barnes EH, Chan C, Carmalt H, et al. Cell cycle marker expression in benign and malignant intraductal papillary lesions of the breast. J Clin Pathol. 2015;68:187–191. doi: 10.1136/jclinpath-2014-202331. [DOI] [PubMed] [Google Scholar]
- 22.Lin CH, Liu CH, Wen CH, Ko PL, Chai CY. Differential CD133 expression distinguishes malignant from benign papillary lesions of the breast. Virchows Arch. 2015;466:177–184. doi: 10.1007/s00428-014-1695-2. [DOI] [PubMed] [Google Scholar]
- 23.Weisman PS, Sutton BJ, Siziopikou KP, Hansen N, Khan SA, Neuschler EI, et al. Non-mass-associated intraductal papillomas: is excision necessary? Hum Pathol. 2014;45:583–588. doi: 10.1016/j.humpath.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 24.Mosier AD, Keylock J, Smith DV. Benign papillomas diagnosed on large-gauge vacuum-assisted core needle biopsy which span <1.5 cm do not need surgical excision. Breast J. 2013;19:611–617. doi: 10.1111/tbj.12180. [DOI] [PubMed] [Google Scholar]