Abstract
Background. Traditional Chinese medicine (TCM) has long been used to treat chronic atrophic gastritis (CAG). The aim of the present study was to evaluate the TCM syndrome characteristics of CAG and its core pathogenesis so as to promote optimization of treatment strategies. Methods. This study was based on a participant survey conducted in 4 hospitals in China. Patients diagnosed with CAG were recruited by simple random sampling. Exploratory factor analysis (EFA) was conducted on syndrome extraction. Results. Common factors extracted were assigned to six syndrome patterns: qi deficiency, qi stagnation, blood stasis, phlegm turbidity, heat, and yang deficiency. Distribution frequency of all syndrome patterns showed that qi deficiency, qi stagnation, blood stasis, phlegm turbidity, and heat excess were higher (76.7%–84.2%) compared with yang deficiency (42.5%). Distribution of main syndrome patterns showed that frequencies of qi deficiency, qi stagnation, phlegm turbidity, heat, and yang deficiency were higher (15.8%–20.8%) compared with blood stasis (8.3%). Conclusions. The core pathogenesis of CAG is combination of qi deficiency, qi stagnation, blood stasis, phlegm turbidity, heat, and yang deficiency. Therefore, treatment strategy of herbal prescriptions for CAG should include herbs that regulate qi, activate blood, resolve turbidity, clear heat, remove toxin, and warm yang.
1. Background
Chronic atrophic gastritis (CAG) is an inflammatory disease of the stomach from various etiologies [1–3]. Typical symptoms, when present, include epigastric pain, fullness, belching, anorexia, and other nonspecific symptoms [3]. CAG can lead to mucosal atrophy, intestinal metaplasia (IM), and gastric intraepithelial dysplasia (GED), also known as intraepithelial neoplasia, which is defined as the precancerous stage of gastric carcinoma [1, 4, 5]. Global cancer statistics for 2012 estimated that there were 951,600 new cases of stomach cancer worldwide [6]. The transition from chronic gastritis to gastric cancer is a typical disease model of uncontrolled inflammation leading to malignant transformation [7–10]. Active treatment of CAG arrests further malignant transformation, and thus prevents gastric cancer [11, 12].
Traditional Chinese medicine (TCM) has a long history in treating gastritis. Numerous basic and clinical studies have demonstrated that Chinese medicine can effectively treat CAG, including resolving mucosal inflammation and reversing glandular atrophy, as well as inhibiting or even reversing intestinal metaplasia and gastric epithelial dysplasia [13–24]. Modern-day TCM treatment of CAG remains based on the time-honored core principle of syndrome pattern differentiation to identify and treat the root of illness. When differentiating a patient's syndrome pattern, the TCM practitioner systematically collects comprehensive information about the presenting signs and symptoms, using the four diagnostic methods of looking, listening/smelling, asking, and palpating. The collocated information is then evaluated according to TCM theory and clinical experience to identify the physical condition and nature of pathologic changes during the current stage of the disease. Treatment is then applied in accordance with conclusions drawn from the pattern differentiation process.
Factor analysis (FA) is a statistical analytic method for reducing data, that is, the redundancy of variables, and to detect the structure (relationships) among the variables being measured. FA has been applied in TCM to develop usable dimensional taxonomies, by which large numbers of observed variables can be remodeled as linear combinations of a smaller number of the underlying factors. There are two modes of FA. Exploratory factor analysis (EFA) is an exploratory data-driven tool that generates solutions for developing theories. Its aim is to explore the relationships among the variables without a specific hypothesis or a priori fixed number of factors. Confirmatory factor analysis (CFA) is a method for theory testing that requires the researcher to have substantive knowledge and a firm idea about the number of factors that will be come upon during analysis. In the field of TCM, EFA is being used increasingly for data mining of measured variables such as clinical information obtained during syndrome pattern differentiation. Through EFA features of the distribution of syndromes can be ascertained.
Although various studies have demonstrated that TCM can effectively treat CAG [13–24], there has been a lack of consensus across studies on syndrome differentiation, treatment strategy, and elaboration of herbal prescriptions [25–27]. This is likely due to the complexity of CAG pathogenesis in TCM. Results of literature reviews have confirmed the lack of agreement in CAG syndrome features [28–33] with only a few studies focusing mainly on CAG. This situation is not conducive to standardization of syndrome differentiation and improvement in treatment efficacy of CAG. The present study explored syndrome pattern features and core TCM pathogenesis of CAG by applying EFA to provide evidence for establishment of TCM treatment principles and standardization of syndrome differentiation for chronic atrophic gastritis.
2. Methods
2.1. Study Design and Participants
This study was conducted between September 2010 and October 2012 based on participant survey. Outpatients and inpatients who visited the hospital for upper gastrointestinal endoscopy and were diagnosed with CAG were recruited by simple random sampling from medical centers in Beijing and Xiamen, China: Dongzhimen Hospital Affiliated to Beijing University of Chinese Medicine, Peking Union Medical College Hospital Affiliated to the Chinese Academy of Medical Sciences, Beijing Hospital Affiliated to the National Health and Family Planning Commission of China, and Xiamen Traditional Chinese Medicine Hospital. All participants signed consent forms. Ethics approval of the present study was given by the Medical Ethics Committee of Beijing University of Chinese Medicine.
2.2. Diagnostic Criteria
Diagnostic criteria of CAG were based on Chinese Society of Gastroenterology, Chinese Medical Association, guidelines [1].
2.3. Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (1) meeting the diagnostic criteria of CAG with detailed medical records and diagnostic reports, (2) age: 20–75 years old, (3) willing to participate in the investigation and sign informed consent, and (4) capable of completing the clinical observation questionnaire and responding to the investigator queries.
Exclusion criteria were as follows: (1) unclear diagnosis or not meeting the diagnostic criteria of CAG, (2) not meeting the age criteria; (3) cognitive difficulty such that four diagnostic methods cannot be completed accurately; (4) other digestive disease or neurologic, circulatory, respiratory, and endocrine disease.
2.4. Case Report Form Content and Administration
Content of the CAG case report form (CRF) was based on literature research, on expert advice, and on standard Chinese guidelines [34–37]. CRF content included general information (name, sex, and age), disease data (complaint, history of present illness, past medical history, family medical history, and endoscopy results), information from the four diagnoses (symptoms, physical signs, tongue appearance, and pulse reading), western medicine diagnosis, and TCM diagnosis.
Disease history and results of the four diagnostic methods were collected and recorded. Records that met the following criteria were deemed acceptable: all general information filled in except address and contact details and complete information for CAG and four diagnostic methods.
The study was carried out with strict quality control. All investigators were specialized in TCM or integrated Chinese and Western medicines and trained in standard operating procedures of the study. Each study participant was examined and followed up by at least two resident physicians or graduate students who filled in the CRFs. At least two senior staff physicians supervised the interview sessions to ensure consistency and authenticity of data collection to reduce measurement bias.
2.5. Data Analysis
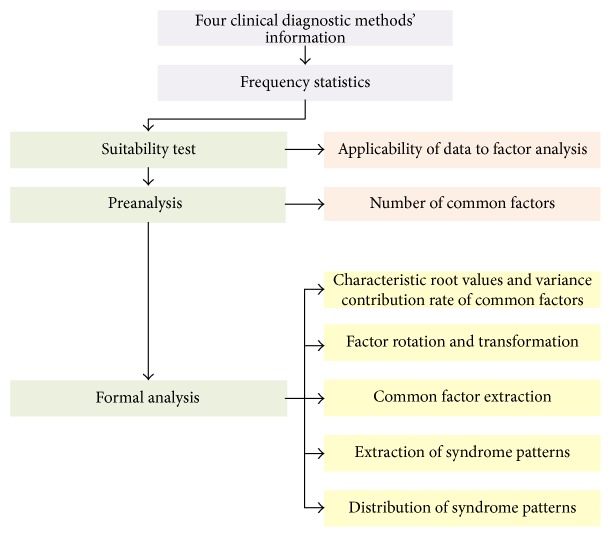
Frequency analysis was performed on data collected from the four diagnostic methods. Exploratory factor analysis (EFA) was performed on syndrome element extraction (Figure 1). All statistical analyses in this study were processed by SPSS software (version 17.0, SPSS Inc., Chicago, IL, USA).
Figure 1.
Flow chart of EFA based CAG syndrome patterns extraction.
3. Results
3.1. Characteristics of Participants
A total of 135 CRFs were distributed, and 131 were completed and returned, with a return rate of 97%. There were 120 forms, that is, patients, that were deemed eligible for the study after eliminating questionnaires with incomplete information, thus, with the acceptance rate of 92%. Among the participants, 62 were male and 58 were female, with an average age of 52.56 and a standard deviation of 12.45.
3.2. Distribution Characteristics of Results from the Four Diagnostic Methods
Information from the four diagnostic methods was collected and 53 entries with ≥10% frequency were tabulated based on the distribution frequency (Table 1).
Table 1.
Four diagnostic variables' frequency for chronic atrophic gastritis (N = 120).
| Frequency sequence | Four diagnostic variables | Distribution frequency (%) |
|---|---|---|
| 1 | Wiry pulse | 75.8 |
| 2 | Dark tongue | 65 |
| 3 | Distention and fullness of the stomach | 64.2 |
| 4 | Thin tongue coating | 61.7 |
| 5 | White tongue coating | 59.2 |
| 6 | Greasy tongue coating | 56.7 |
| 7 | Belching | 54.2 |
| 8 | Stomach aversion to cold | 54.2 |
| 9 | Acid regurgitation | 50 |
| 10 | Lack of strength | 50 |
| 11 | Dry mouth | 49.2 |
| 12 | Heartburn | 46.7 |
| 13 | Irritability | 45 |
| 14 | Bitter taste in the mouth | 45 |
| 15 | Yellow tongue coating | 44.2 |
| 16 | Red tongue | 39.2 |
| 17 | Insomnia | 35.8 |
| 18 | Pale red tongue | 34.2 |
| 19 | Loose stool | 33.3 |
| 20 | Profuse dreaming at night | 33.3 |
| 21 | Constipation | 32.5 |
| 22 | Enlarged tongue | 32.5 |
| 23 | Sensation of coldness of the body and limbs | 31.7 |
| 24 | Fetid mouth odor | 30 |
| 25 | Choppy pulse | 30 |
| 26 | Stifling sensation in the chest | 28.3 |
| 27 | Poor appetite | 28.3 |
| 28 | Night sweat | 28.3 |
| 29 | Thick tongue coating | 28.3 |
| 30 | Frequent sighing | 25.8 |
| 31 | Abdominal distention | 24.2 |
| 32 | Palpitations | 23.3 |
| 33 | Listlessness | 23.3 |
| 34 | Teeth-marked tongue | 23.3 |
| 35 | Fine pulse | 23.3 |
| 36 | Tinnitus | 22.5 |
| 37 | Sharp pain in stomach | 21.8 |
| 38 | Nausea | 21.8 |
| 39 | Tongue with petechiae | 21.8 |
| 40 | Slippery pulse | 21.8 |
| 41 | Sallow complexion | 21.8 |
| 42 | Hypochondriac pain | 20.8 |
| 43 | Dry stool | 20.8 |
| 44 | Hiccups | 20.8 |
| 45 | Rapid pulse | 20.8 |
| 46 | Distending pain in the stomach | 20 |
| 47 | Stomach noises (grumbling) | 20 |
| 48 | Thirst and desire to drink | 20 |
| 49 | Emotional upset | 19.2 |
| 50 | Reddish yellow urine | 19.2 |
| 51 | Feeling of heaviness of the body | 19.2 |
| 52 | Dull ache in the stomach | 18.3 |
| 53 | Distention and fullness in the hypochondriac region | 16.7 |
| 54 | Dark complexion | 16.7 |
| 55 | Shortness of breath | 15.8 |
| 56 | Borborygmus | 15.8 |
| 57 | Thin and shrunken tongue | 15 |
| 58 | Sticky mouth | 13.3 |
| 59 | Flatulence | 12.5 |
| 60 | Sunken pulse | 12.5 |
| 61 | Bland taste in the mouth | 10.8 |
Data were preanalyzed and ultimately 40 diagnostic variables with more than 21% frequency of occurrence were chosen to judge the applicability of the data for EFA, so as to determine the number of common factors to be extracted for formal analysis.
3.3. Suitability Test
KMO and Bartlett's test of sphericity were used to evaluate suitability of collocated diagnostic variables for EFA. The Kaiser-Meyer-Olkin (KMO) test assesses partial correlation between variables, and if the KMO value is >0.5, the variable will be more suitable for EFA. In addition, the closer the KMO value is to 1, the stronger the correlation is between variables. Bartlett's test of sphericity assesses the null hypothesis and whether the correlation matrix is rejected as a unit matrix. Only when variables are relatively nonindependent (P < 0.05) can they be used for EFA.
In this study, the KMO value of the partial correlation of variables was 0.549 > 0.5 (Table 2), indicating a certain degree of partial correlations between variables, such that EFA could be carried out. The approximate chi-square value of Bartlett's test of sphericity was 1589.24 and P < 0.001, indicating strong correlation between variables, rejection of the hypothesis of independence of variables, and that the variables could be applied to EFA.
Table 2.
KMO and Bartlett's test of sphericity.
| Kaiser-Meyer-Olkin measure of sampling adequacy | 0.549 |
|
| |
| Bartlett's test of sphericity | |
| Approx. chi-square | 1589.24 |
| df | 780 |
| Sig | 0.000 |
3.4. Assessment of Common Factors
Characteristic root value is an index to evaluate the influence of extracted common factors; that is, introduction of this common factor can explain and evaluate the information of the original variables. Variance contribution rate is the proportion of communality in all variances, and the value is positively correlated with carrying capacity of comprehensive information. The cumulative variance contribution rate is the accumulation of variance contribution rate of first N common factors, which represents the proportion of information of all variables whose first N common factors is covered. Results of characteristic root values and variance contribution rate of common factors were tabulated (Table 3). Principal component analysis was applied to extract common factors. Characteristic root values of the first 15 common factors were greater than 1, and their cumulative variance contribution rates reached 70.795, good overall data interpretation capability.
Table 3.
Characteristic root values and variance contribution rate of common factors.
| Common factor | Initial characteristic root value | Variance extraction load | Variance load after rotation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic root value | Variance contribution rate (%) | Cumulative variance contribution rate (%) | Characteristic root value | Variance contribution rate (%) | Cumulative variance contribution rate (%) | Characteristic root value | Variance contribution rate (%) | Cumulative variance contribution rate (%) | |
| 1 | 3.830 | 9.576 | 9.576 | 3.830 | 9.576 | 9.576 | 1.988 | 4.970 | 4.970 |
| 2 | 3.382 | 8.454 | 18.030 | 3.382 | 8.454 | 18.030 | 1.903 | 4.756 | 9.726 |
| 3 | 2.832 | 7.080 | 25.110 | 2.832 | 7.080 | 25.110 | 1.107 | 2.768 | 12.494 |
| 4 | 2.507 | 6.268 | 31.378 | 2.507 | 6.268 | 31.378 | 1.035 | 2.588 | 15.082 |
| 5 | 2.132 | 5.330 | 36.708 | 2.132 | 5.330 | 36.708 | 1.028 | 2.570 | 17.651 |
| 6 | 1.987 | 4.967 | 41.675 | 1.987 | 4.967 | 41.675 | 1.027 | 2.568 | 20.219 |
| 7 | 1.671 | 4.176 | 45.852 | 1.671 | 4.176 | 45.852 | 1.027 | 2.567 | 22.786 |
| 8 | 1.575 | 3.937 | 49.789 | 1.575 | 3.937 | 49.789 | 1.026 | 2.566 | 25.352 |
| 9 | 1.443 | 3.608 | 53.396 | 1.443 | 3.608 | 53.396 | 1.025 | 2.564 | 27.915 |
| 10 | 1.296 | 3.239 | 56.636 | 1.296 | 3.239 | 56.636 | 1.025 | 2.562 | 30.478 |
| 11 | 1.262 | 3.155 | 59.791 | 1.262 | 3.155 | 59.791 | 1.022 | 2.556 | 33.034 |
| 12 | 1.218 | 3.044 | 62.836 | 1.218 | 3.044 | 62.836 | 1.018 | 2.546 | 35.580 |
| 13 | 1.106 | 2.765 | 65.601 | 1.106 | 2.765 | 65.601 | 1.018 | 2.546 | 38.126 |
| 14 | 1.055 | 2.638 | 68.239 | 1.055 | 2.638 | 68.239 | 1.018 | 2.544 | 40.669 |
| 15 | 1.022 | 2.556 | 70.795 | 1.022 | 2.556 | 70.795 | 1.017 | 2.542 | 43.212 |
| 16 | .956 | 2.391 | 73.186 | .956 | 2.391 | 73.186 | 1.017 | 2.542 | 45.754 |
| 17 | .852 | 2.130 | 75.316 | .852 | 2.130 | 75.316 | 1.017 | 2.541 | 48.295 |
| 18 | .810 | 2.025 | 77.341 | .810 | 2.025 | 77.341 | 1.014 | 2.536 | 50.831 |
| 19 | .805 | 2.013 | 79.354 | .805 | 2.013 | 79.354 | 1.014 | 2.534 | 53.365 |
| 20 | .774 | 1.934 | 81.288 | .774 | 1.934 | 81.288 | 1.011 | 2.527 | 55.892 |
| 21 | .696 | 1.740 | 83.028 | .696 | 1.740 | 83.028 | 1.008 | 2.520 | 58.412 |
| 22 | .666 | 1.665 | 84.693 | .666 | 1.665 | 84.693 | 1.007 | 2.517 | 60.929 |
| 23 | .624 | 1.560 | 86.253 | .624 | 1.560 | 86.253 | 1.005 | 2.512 | 63.441 |
| 24 | .591 | 1.476 | 87.729 | .591 | 1.476 | 87.729 | 1.004 | 2.509 | 65.950 |
| 25 | .526 | 1.315 | 89.044 | .526 | 1.315 | 89.044 | 1.002 | 2.504 | 68.455 |
| 26 | .495 | 1.239 | 90.283 | .495 | 1.239 | 90.283 | 1.001 | 2.502 | 70.957 |
| 27 | .451 | 1.127 | 91.410 | .451 | 1.127 | 91.410 | 1.001 | 2.502 | 73.459 |
| 28 | .437 | 1.093 | 92.503 | .437 | 1.093 | 92.503 | .997 | 2.493 | 75.952 |
| 29 | .421 | 1.053 | 93.555 | .421 | 1.053 | 93.555 | .997 | 2.492 | 78.444 |
| 30 | .351 | .878 | 94.433 | .351 | .878 | 94.433 | .993 | 2.482 | 80.926 |
| 31 | .336 | .839 | 95.272 | .336 | .839 | 95.272 | .981 | 2.453 | 83.379 |
| 32 | .323 | .807 | 96.079 | .323 | .807 | 96.079 | .975 | 2.439 | 85.817 |
| 33 | .294 | .734 | 96.813 | .294 | .734 | 96.813 | .965 | 2.413 | 88.230 |
| 34 | .257 | .643 | 97.456 | .257 | .643 | 97.456 | .959 | 2.397 | 90.627 |
| 35 | .236 | .589 | 98.044 | .236 | .589 | 98.044 | .935 | 2.337 | 92.964 |
| 36 | .212 | .529 | 98.574 | .212 | .529 | 98.574 | .907 | 2.267 | 95.232 |
| 37 | .194 | .484 | 99.058 | .194 | .484 | 99.058 | .863 | 2.159 | 97.390 |
| 38 | .157 | .392 | 99.451 | .157 | .392 | 99.451 | .767 | 1.918 | 99.308 |
| 39 | .139 | .348 | 99.798 | .139 | .348 | 99.798 | .184 | .459 | 99.767 |
| 40 | .081 | .202 | 100.000 | .081 | .202 | 100.000 | .093 | .233 | 100.000 |
Note. Extraction method: principal component analysis. Rotation method: Kaiser standardized orthogonal. Rotation was converged after 20 iterations.
Scree plot displayed relevance of common factors and characteristic root values (Figure 2). The number of common factors was shown on the x-axis and the characteristic values on the y-axis. Scatter locations of first 15 common factors were steep, and characteristic root values of the last 25 common factors were small as revealed by the leveling off of the curve's slope. Thus, the number of extracted common factors in formal calculation was 15.
Figure 2.
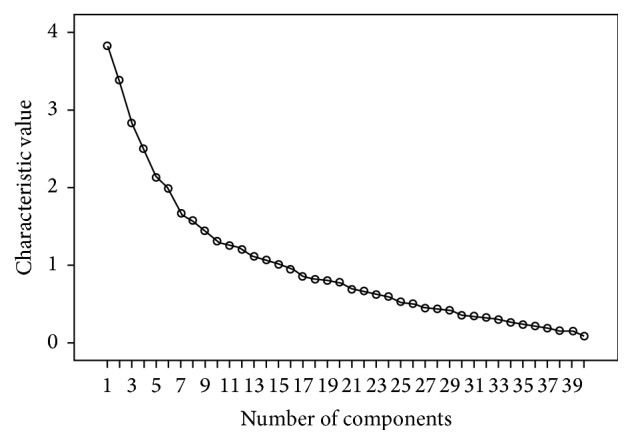
Scree plot of characteristic root value of common factors.
3.5. Factor Rotation and Transformation
Factor rotation was performed to allow the factor load absolute value of the new common factor for each of the four diagnostic results to polarize to 0 or 1 and thus more clearly display the load of all common factor variables, as well as maintaining the variance of all common factors in the corresponding row unchanged. This allows for a more reasonable explanation for the extraction of all common factors. Principal component analysis was used to extract 15 common factors, and the factor rotation method used was varimax rotation. Rotation was converged after 20 iterations and results of the factor load matrix after rotation transformation is shown in Table 4.
Table 4.
Factor load matrix after rotation transformation.
| Four diagnostic variables | Component | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
| Distention and fullness of the stomach | −.028 | .005 | .015 | .056 | .332 | −.026 | .121 | .024 | .160 | .694 | .093 | −.202 | .008 | −.053 | −.009 |
| Palpitations | .544 | .021 | .195 | .136 | .051 | .242 | .167 | −.057 | .046 | .026 | .029 | −.130 | −.321 | .359 | −.109 |
| Stifling sensation in the chest | .140 | .020 | .136 | .017 | .139 | .010 | .096 | −.019 | −.091 | .034 | .041 | −.021 | .056 | .833 | .072 |
| Loose stool | −.073 | .128 | −.047 | .416 | .113 | −.086 | .209 | −.075 | .449 | −.049 | .180 | .068 | .027 | .034 | .192 |
| Stomach tingling Sharp pain in stomach | −.095 | −.170 | .356 | .048 | −.014 | .201 | .478 | .214 | .041 | .185 | −.060 | .101 | −.341 | −.076 | .213 |
| Frequent sighing | .629 | −.281 | .050 | −.060 | −.121 | −.100 | .058 | .046 | .016 | .035 | .074 | .251 | .080 | .119 | .215 |
| Constipation | −.205 | −.081 | .089 | .502 | .145 | .026 | −.038 | −.195 | .133 | .324 | .142 | .141 | .363 | −.105 | .142 |
| Irritability | .017 | −.024 | .248 | .013 | −.118 | .590 | .164 | .079 | −.132 | −.327 | .136 | −.095 | .161 | −.141 | .101 |
| Bitter taste in the mouth | .047 | −.010 | .049 | .133 | .282 | .622 | −.074 | −.156 | −.056 | .094 | −.200 | .024 | .036 | −.061 | .195 |
| Poor appetite | −.050 | .013 | −.037 | .087 | −.253 | .095 | −.097 | −.065 | −.158 | .720 | −.014 | .008 | .024 | .064 | .035 |
| Abdominal distention | .060 | −.009 | −.027 | .142 | .101 | .235 | .195 | −.051 | .187 | .187 | .114 | .200 | .295 | .124 | .414 |
| Fetid mouth odor | .078 | .041 | −.075 | −.034 | .165 | .044 | .078 | .064 | −.007 | −.020 | −.054 | −.033 | −.054 | .039 | .814 |
| Belching | .142 | .009 | −.192 | .074 | .425 | −.027 | .065 | .016 | .018 | .172 | .131 | .458 | −.180 | .051 | .017 |
| Sallow complexion | .029 | .041 | .029 | .005 | −.057 | .005 | .116 | −.039 | .775 | −.024 | .007 | .010 | .032 | −.092 | −.046 |
| Acid regurgitation | .012 | −.098 | −.097 | .149 | .794 | .075 | .006 | .010 | .006 | −.112 | .027 | .041 | .050 | .131 | .143 |
| Stomach aversion to cold | .670 | .150 | −.146 | .000 | .208 | .074 | −.074 | .011 | .068 | −.139 | −.093 | .216 | −.064 | .008 | .056 |
| Heartburn | .065 | −.203 | .152 | −.143 | .702 | .183 | .126 | −.158 | −.052 | .106 | −.059 | −.004 | .090 | .013 | .070 |
| Listlessness | .388 | −.002 | −.032 | .730 | .024 | −.021 | .066 | .159 | .093 | −.035 | −.059 | .126 | −.175 | .040 | −.092 |
| Sensation of coldness of the body and limbs | .795 | .169 | −.088 | .125 | .068 | −.043 | .052 | .058 | −.047 | .022 | −.012 | −.096 | .191 | −.017 | −.055 |
| Nausea | .174 | .056 | .028 | .325 | .064 | −.181 | .050 | .213 | −.004 | −.061 | −.270 | .462 | .363 | .395 | .021 |
| Lack of strength | −.011 | .010 | .038 | .738 | −.005 | .190 | −.033 | .098 | −.047 | .166 | .014 | −.318 | −.044 | .037 | −.024 |
| Insomnia | −.163 | −.054 | −.079 | −.081 | .161 | .561 | −.129 | .088 | .426 | .035 | .353 | −.082 | .168 | .130 | −.072 |
| Profuse dreaming at night | .110 | −.112 | .020 | −.112 | .062 | .349 | −.112 | .004 | .068 | .040 | .027 | −.071 | .786 | .051 | −.031 |
| Dry mouth | .066 | .063 | .204 | .070 | .102 | .569 | .081 | −.068 | −.014 | .341 | −.129 | .173 | .161 | .175 | −.086 |
| Tinnitus | .395 | .082 | −.018 | .316 | −.135 | .032 | .345 | −.127 | −.315 | −.035 | .180 | .100 | .131 | .163 | .127 |
| Pale red tongue | .042 | −.122 | −.040 | .105 | −.117 | .045 | −.073 | .860 | .023 | .038 | .035 | .061 | .051 | −.081 | .011 |
| Red tongue | .015 | −.006 | .386 | −.015 | −.031 | .182 | −.034 | −.724 | .017 | .175 | −.131 | −.012 | .111 | −.133 | −.068 |
| Dark tongue | .099 | .170 | −.160 | −.082 | .088 | −.097 | .768 | −.033 | −.046 | −.190 | .045 | −.019 | .046 | .044 | .237 |
| Enlarged tongue | .100 | .160 | −.122 | .312 | −.126 | −.018 | −.083 | .251 | .479 | .014 | −.226 | −.138 | .016 | .000 | .293 |
| Tongue with petechiae | −.013 | −.069 | −.057 | .079 | .056 | .083 | .669 | −.058 | .266 | .180 | −.110 | .061 | −.180 | .153 | −.117 |
| Teeth-marked tongue | .258 | .296 | .080 | −.181 | .182 | −.279 | −.056 | .254 | .357 | .217 | −.072 | −.108 | .110 | −.187 | .112 |
| White tongue coating | .092 | −.035 | −.893 | −.074 | .052 | −.133 | .056 | .145 | .044 | .013 | −.039 | .047 | .089 | −.067 | .079 |
| Yellow tongue coating | −.037 | .100 | .895 | −.066 | .035 | .039 | −.094 | −.108 | .025 | −.024 | .036 | −.076 | .088 | .108 | −.033 |
| Thick tongue coating | .080 | .889 | −.043 | .044 | −.112 | −.016 | .002 | −.040 | −.053 | −.021 | −.005 | .001 | −.028 | .089 | .051 |
| Thin tongue coating | .014 | −.849 | −.095 | −.041 | .208 | −.083 | .006 | .074 | −.093 | −.015 | .000 | −.078 | .105 | −.096 | −.083 |
| Greasy tongue coating | .080 | .685 | .135 | −.076 | .083 | −.127 | .160 | −.014 | .178 | .035 | .132 | −.094 | .074 | −.333 | −.134 |
| Wiry pulse | −.463 | .059 | .156 | −.007 | .168 | −.036 | .177 | .096 | −.077 | .073 | −.532 | −.051 | .046 | −.100 | −.193 |
| Fine pulse | .085 | −.003 | −.055 | −.121 | −.010 | .063 | .001 | .034 | −.039 | −.127 | .139 | .794 | −.008 | −.047 | −.009 |
| Choppy pulse | .021 | .140 | −.117 | .196 | .166 | .020 | .450 | −.101 | .106 | −.129 | −.500 | −.162 | .113 | −.323 | −.085 |
| Slippery pulse | −.039 | .128 | .090 | .090 | .094 | −.055 | .051 | .121 | −.007 | .036 | .783 | .110 | .070 | −.068 | −.113 |
Note. Extraction method: principal component analysis. Rotation method: Kaiser standardized orthogonal. Rotation was converged after 20 iterations. Factor load values that were positive and larger or equal to 0.25 are depicted in bold.
3.6. Common Factor Extraction
In Table 4, the factor load value was the coefficient values of each common factor that were used to reflect the closeness between common factors and variables. The essence of factor load values was the correlation coefficient between them. A positive factor load value from the four diagnostic methods' information represents a positive correlation, and a negative factor load value represents a negative correlation. Correlation between them had a positive correlation with factor load value. Load coefficients that were positive and larger or equal to 0.25 of the four diagnostic methods' information were selected into the corresponding factors.
Through consultation with TCM gastroenterology experts throughout China, the diagnostic variables, nature of disease, and disease location obtained from the four diagnostic methods' information were assigned to 15 common factors (F) (Table 5).
Table 5.
Common factors and their corresponding four diagnostic variables, disease nature, and organ locations.
| Common factor | Four diagnostic variablesa | Syndrome pattern | Organ location of disease |
|---|---|---|---|
| F1 | Palpitations (.544); frequent sighing (.629); stomach aversion to cold, listlessness (.388); sensation of coldness of the body and limbs (.795); tinnitus (.395) | Yang deficiency | Spleen and stomach |
| F2 | Teeth-marked tongue (.258); thick tongue coating (.889); greasy tongue coating (.685) | Phlegm turbidity | Spleen and stomach |
| F3 | Severe stomach pain (.356); red tongue (.386); yellow tongue coating (.895) | Heat and blood stasis | Stomach |
| F4 | Loose stool (.416); constipation (.502); listlessness (.730); lack of strength (.738); tinnitus (.312); enlarged tongue (.312) | Qi deficiency | Spleen |
| F5 | Distention and fullness of the stomach (.332); bitter taste in the mouth (.282); belching (.425); acid regurgitation (.794); heartburn (.702) | Qi stagnation | Liver and stomach |
| F6 | Irritability (.590); bitter taste in the mouth (.622); insomnia (.561); profuse dreaming at night (.349); dry mouth (.569) | Heat | Liver |
| F7 | Sharp pain in stomach (.478); tinnitus (.345); dark tongue (.768); tongue with petechiae (.669); choppy pulse (.450); | Blood stasis | Stomach |
| F8 | pale red tongue (.860); enlarged tongue (.251); teeth-marked tongue (.254) | Qi deficiency | Spleen |
| F9 | Loose stool (.449); sallow complexion (.775); insomnia (.426); enlarged tongue (.479); tongue with petechiae (.266); teeth-marked tongue (.357) | Qi deficiency | Spleen |
| F10 | Distention and fullness in the stomach (.694); constipation (.324); poor appetite (.720); dry mouth (.341) | Qi stagnation | Spleen and stomach |
| F11 | Insomnia (.353); slippery pulse (.783) | Phlegm turbidity | Spleen and stomach |
| F12 | Frequent sighing (.251); abdominal distention (.200); belching (.458); nausea (.462); fine pulse (.794) | Qi stagnation | Liver and stomach |
| F13 | Constipation (.363); abdominal distention (.295); nausea (.363); profuse dreaming at night (.786) | Phlegm turbidity | Spleen |
| F14 | Palpitation (.759); stifling sensation in the chest (.833); nausea (.395) | Phlegm turbidity | Spleen and stomach |
| F15 | Abdominal distention (.414); fetid mouth odor (.814); enlarged tongue (.293) | Heat and qi stagnation | Spleen and stomach |
aValues in parentheses are results of factor load matrix after rotation transformation.
3.7. Extraction of Syndrome Patterns
Next, the 15 common factors were combined based on syndrome pattern and organ location. Ultimately, six syndrome patterns were established (Table 6).
Table 6.
Syndrome pattern and their corresponding common factors and four diagnostic variables.
| Syndrome pattern | Common factors | Four diagnostic variables | |
|---|---|---|---|
| Disease nature | Organ location | ||
| F1 (qi deficiency) | Spleen | F4, F8, F9 | Loose stool, constipation, listlessness, lack of strength, tinnitus, sallow complexion, insomnia, pale red tongue, enlarged tongue, teeth-marked tongue, tongue with petechiae |
| F2 (qi stagnation) | Liver Stomach |
F5, F10, F12 | Distention and fullness of the stomach, bitter taste in mouth, belching, acid regurgitation, heartburn, poor appetite, nausea, frequent sighing, abdominal distention, dry mouth, constipation, fine pulse |
| F3 (blood stasis) | Stomach | F3, F7 | Severe stomach pain, tinnitus, dark tongue, tongue with petechiae, choppy pulse, red tongue, yellow tongue coating |
| F4 (phlegm turbidity) | Spleen Stomach |
F2, F11, F13, F14 | Constipation, abdominal distention, nausea, stifling sensation in the chest, palpitation, insomnia, profuse dreaming at night, teeth-marked tongue, thick tongue coating, greasy tongue coating, slippery pulse |
| F5 (heat) | Spleen Liver Stomach |
F3, F6, F15 | Severe stomach pain, irritability, bitter taste in mouth, insomnia, profuse dreaming at night, abdominal distention, fetid mouth odor, dry mouth, red tongue, yellow tongue coating, enlarged tongue |
| F6 (yang deficiency) | Spleen Stomach |
F1 | Stomach aversion to cold, listlessness, sensation of coldness of the body and limbs, palpitation, frequent sighing, tinnitus, teeth-marked tongue |
3.8. Distribution of Syndrome Patterns
The corresponding common factor score of each participant's six syndrome patterns was calculated based on the factor score coefficient, according to which all syndrome patterns of each participant were estimated. Distribution of all syndrome patterns was tabulated (Figure 3).
Figure 3.
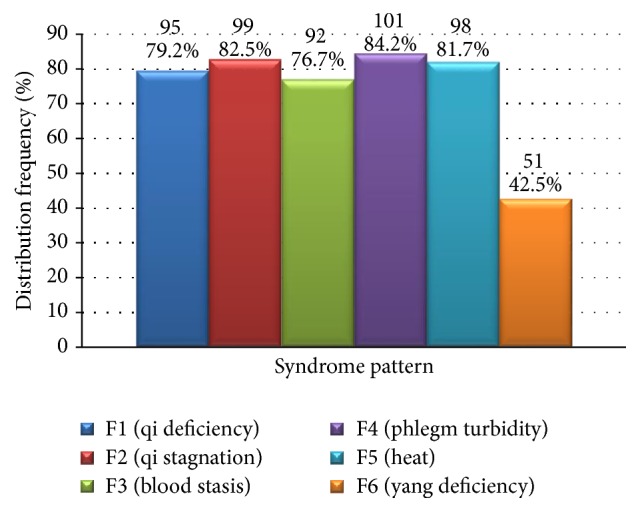
Distribution of all syndrome patterns (N = 120).
Factor load after rotation and transformation yielded a syndrome pattern with the highest score, which was taken as the primary syndrome pattern. Distribution of primary syndrome patterns was shown in Figure 4.
Figure 4.
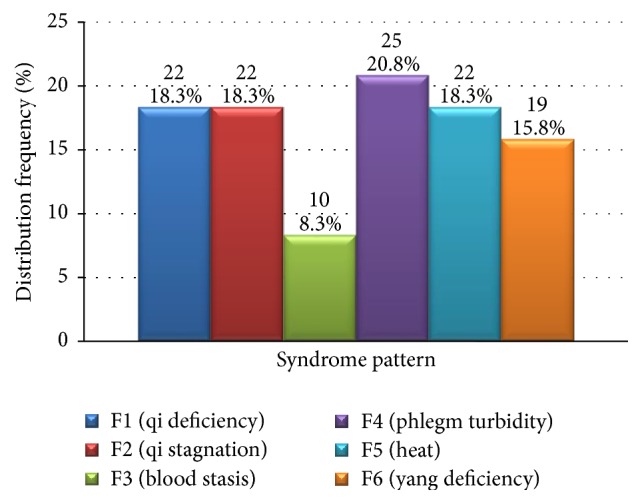
Distribution of primary syndrome patterns (N = 120).
4. Discussion
EFA is a multivariate statistical analytic method to explain original variable correlation with potential variables from the perspective of original variable correlation information. The fundamental concept is to project high-dimensional information onto a lower plain to explore internal structure and essential characteristics through dimensionality reduction. EFA applies principal component analysis to extract common factors. Constant factor variance and difference maximization (relative load of squares) are achieved by factor rotation. Finally, complex original data set information is summarized to a limited number of unmeasurable latent variables (common factors) to describe information of most variables. Based on this, the relationship where original measured variables are governed by a small number of independent factors is explored, and the nature of the original variables is clarified by a linear combination of common factors [38–42].
The holistic theory that TCM is based on determines the complex multivariate nonlinear, that is, multicollinear, relationship of the variables of the four diagnostic methods' information. In this study using EFA to assess TCM syndrome characteristics of CAG the four diagnostic variables were the original variables and had significantly higher dimensional characteristics. The syndrome patterns and other syndrome information were extracted from the common factors (four diagnostic variables with specific combination of features), which were the governing correlations of the four diagnostic variables, so as to achieve dimensionality reduction and elimination of multicollinearity.
The four diagnostic methods' information that were detected with high frequency were further assessed to rule out any noise interference after frequency statistics. EFA was applied to extract the syndrome patterns, organ location, and other common factors related to the four diagnostic methods' information. All information the common factors belonged to was appraised based on professional knowledge to extract the syndrome patterns. The distribution features of all syndrome patterns and their corresponding primary syndrome patterns were determined. Thus, EFA showed a total of 15 extracted common factors comprised 6 syndrome patterns (qi deficiency, qi stagnation, blood stasis, phlegm turbidity, heat, and yang deficiency) as well as disease location in the liver, spleen, or stomach.
In TCM, the syndrome pattern is the basic pathogenetic unit for evaluating a disease [43, 44]. Extraction of the aforementioned 6 syndrome patterns suggests that they form the core pathogenesis of CAG and should thus be the fundamental diagnostic elements taken into account during differentiation of CAG. It follows that, when formulating a prescription to treat CAG, the 6 strategies that should be considered depending on the presenting syndrome pattern are regulating qi (tonification of qi and moving of qi), activating blood, resolving turbidity, clearing heat, removing toxin, and warming yang. Furthermore, target organs of treatment should be the liver, spleen, and stomach.
In this study, EFA results indicated that the syndrome pattern blood stasis was highly associated with qi deficiency, qi stagnation, phlegm turbidity, and heat, whereas association of yang deficiency with the same syndrome patterns was significantly lower. However, in terms of distribution of the primary syndrome pattern, the detected frequency was significantly lower than that of qi deficiency, qi stagnation, phlegm turbidity, blood stasis, and yang deficiency. Thus, from two seemingly contradictory results, it can be inferred that blood stasis, similar to qi deficiency, qi stagnation, phlegm turbidity, and heat, has a wide distribution as a fundamental syndrome pattern and has a high frequency of detection even in patients who have mild blood stasis. For this reason, of all the syndrome patterns, blood stasis had the lowest distribution frequency. This suggests that, in terms of treatment of CAG, formulation of prescriptions should focus on the combination of tonification and moving of qi, activating blood and resolving stasis, clearing phlegm to resolve turbidity, clearing heat and removing toxin, and activating blood to resolve stasis. However, herbs that activate blood to resolve stasis should be prescribed in lesser amounts.
Interestingly, analysis of all syndrome patterns showed that frequency of yang deficiency was significantly lower than that of qi deficiency, qi stagnation, phlegm turbidity, and heat. EFA of primary syndrome patterns indicated that distribution frequency of yang deficiency was similar to that of qi deficiency, qi stagnation, phlegm turbidity, and heat, and was significantly higher than that of blood stasis. Thus, unlike qi deficiency, qi stagnation, phlegm turbidity, and heat, yang deficiency was not widely detected in CAG patients as a fundamental syndrome pattern. Although overall distribution was narrow, once yang deficiency took hold in the body, its presence was intense and detectable, thus occupying a considerable proportion of the primary syndrome distribution. Therefore, in formulating a prescription, in the early stage of yang deficiency type CAG, herbs that tonify yang should receive less prominence than herbs that focus on tonifying and regulating qi, activating blood, resolving phlegm turbidity, clearing heat, and removing toxin. If yang deficiency persists, yang-tonifying herbs should be used to some extent.
Other investigations have not been consistent on TCM syndrome patterns and disease site of CAG [28–32]. For example, Gan and colleagues' [28] conclusion regarding disease site (stomach, spleen, and liver) concurred with our findings. However, their results on primary syndrome patterns of CAG (combined deficiency and excess and combined cold and heat) differed from our results of six patterns. Literature reviews have also confirmed the lack of agreement among TCM authors regarding disease site and primary syndrome patterns of CAG [30, 31], indicating the complexities of both the disease nature and progression of CAG as well as the differentiation of its syndrome patterns. Thus, our study applied EFA in an attempt to describe the network of relationships among the four diagnostic variables in order to understand the main syndrome patterns and thus disease sites of CAG.
There are some limitations of this study. Selection bias may exist because all data were derived from participants in hospitals in only two cities with a relatively small sample and therefore are likely not representative of the four diagnostic variables in CAG patients in the rest of China. Future multicentered study which includes large samples is required to verify the conclusions of the present study. In terms of data mining methodology, in EFA each variable or common factor has only one chance to be included in a single category, which means multiple correspondence between variables and categories cannot be created. These flaws may result in an inability to accurately describe the internal property or external relevance of TCM variables from a multidimensional and multilinear perspective to some extent. So in this process, multicollinearity is eliminated by reducing the dimension, from which information may be lost by the so-called dimension effect. It should be noted that Bartlett's test of sphericity approximate chi-square value of EFA was 1589.243 (P < 0.001) and the KMO value was 0.549 > 0.5, indicating that EFA was acceptable. However, the degree of perfection was not satisfactory such that the results need to be validated with other supervised data mining methods.
5. Conclusions
EFA is a valuable methodology for developing usable dimensional taxonomies in TCM, by which observed syndrome-related variables can be remodeled as linear combinations of the underlying factors. Application of EFA can provide evidence for treatment principles and standardization of syndrome differentiation of chronic atrophic gastritis. Results of this study found that the core pathogenesis of CAG is a combination of qi deficiency, qi stagnation, blood stasis, phlegm turbidity, and heat and yang deficiency. TCM treatment of CAG should therefore focus on regulating qi, activating blood, resolving turbidity, clearing heat and removing toxin, and warming yang.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (nos. 91129714, 81270466, 81173424, and 81373796), Science Research Foundation of Beijing University of Chinese Medicine (no. 2014-JYBZZ-XS-134), National Undergraduates Innovating Experimentation Project of the China Ministry of Education (no. 081002609), and Specialized Research Fund for the Doctoral Program of Higher Education of China (no. 20120013110014). The authors thank Professor Wenpeng Zhang of the China Academy of Chinese Medical Sciences for his helpful discussions during the course of this study and his critical review of this manuscript. The authors are grateful to Nissi S. Wang, M.S., for the reviewing and the developmental editing of the manuscript.
Abbreviations
- CAG:
Chronic atrophic gastritis
- TCM:
Traditional Chinese medicine
- EFA:
Exploratory factor analysis.
Competing Interests
The authors declare that they have no competing interests.
Authors' Contributions
Xia Ding and Yin Zhang conceived, designed, and coordinated the study. Yin Zhang and Yue Liu designed the case report form and trained investigators at each medical center on standard operating procedures of this study. Yin Zhang, Ying Zhao, Leilei Sun, and Ajian Zhou performed the data analysis. Yin Zhang, Ajian Zhou, Ying Zhao, and Yue Liu wrote the manuscript with contributions from all other authors. All authors carried out the clinical investigation and approved the final manuscript. Yin Zhang, Ajian Zhou, Yue Liu, and Ying Zhao contributed equally to this work; they are the co-first authors.
References
- 1.Fang J. Y., Liu W. Z., Li Z. S., et al. Consensus on chronic gastritis in China (9-10 November 2012 Shanghai) American Journal of Digestive Disease. 2014;1(1):3–21. [Google Scholar]
- 2.Weck M. N., Brenner H. Prevalence of chronic atrophic gastritis in different parts of the world. Cancer Epidemiology Biomarkers and Prevention. 2006;15(6):1083–1094. doi: 10.1158/1055-9965.EPI-05-0931. [DOI] [PubMed] [Google Scholar]
- 3.Feldman M., Lee E. L. Gastritis. In: Feldman M., editor. Sleisinger and Fordtran's Gastrointestinal and Liver Disease. 10th. chapter 52. Philadelphia, Pa, USA: Elsevier Saunders; 2016. pp. 870–872. [Google Scholar]
- 4.Nathan C., Ding A. Nonresolving Inflammation. Cell. 2010;140(6):871–882. doi: 10.1016/j.cell.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 5.Misdraji J., Lauwers G. Y. Gastric epithelial dysplasia. Seminars in Diagnostic Pathology. 2002;19(1):20–30. [PubMed] [Google Scholar]
- 6.Torre L. A., Bray F., Siegel R. L., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA: Cancer Journal for Clinicians. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 7.Krajcovic M., Johnson N. B., Sun Q., et al. A non-genetic route to aneuploidy in human cancers. Nature Cell Biology. 2011;13(3):324–330. doi: 10.1038/ncb2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Correa P., Piazuelo M. B. The gastric precancerous cascade. Journal of Digestive Diseases. 2012;13(1):2–9. doi: 10.1111/j.1751-2980.2011.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chao C., Hellmich M. R. Gastrin, inflammation, and carcinogenesis. Current Opinion in Endocrinology, Diabetes and Obesity. 2010;17(1):33–39. doi: 10.1097/MED.0b013e328333faf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kundu J. K., Surh Y.-J. Inflammation: gearing the journey to cancer. Mutation Research/Reviews in Mutation Research. 2008;659(1-2):15–30. doi: 10.1016/j.mrrev.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Nobili S., Bruno L., Landini I., et al. Genomic and genetic alterations influence the progression of gastric cancer. World Journal of Gastroenterology. 2011;17(3):290–299. doi: 10.3748/wjg.v17.i3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conteduca V., Sansonno D., Lauletta G., Russi S., Ingravallo G., Dammacco F. H. pylori infection and gastric cancer: state of the art (review) International Journal of Oncology. 2013;42(1):5–18. doi: 10.3892/ijo.2012.1701. [DOI] [PubMed] [Google Scholar]
- 13.Zhang W. D., Chen Z. S., Wei B. H. Treatment plan for integrated traditional Chinese medicine and western medicine on chronic gastritis. World Chinese Journal of Digestology. 2004;12(11):2697–2700. [Google Scholar]
- 14.Yang J. M., Zhu F. S., Xu T. T., et al. Yiqi Huoxue Decoction in the treatment of 31 cases of chronic atrophic gastritis. Jiangsu Journal of Traditional Chinese Medicine. 2014;46(12):16–18. [Google Scholar]
- 15.Teng L. P. Yiqi Huoxue Decoction in the treatment of 40 cases of chronic atrophic gastritis. Yunnan Journal of Traditional Chinese Medicine and Materia Medica. 2011;32(6):56–57. [Google Scholar]
- 16.Niu X. D., Niu K. M., Xu M. H., et al. Regulating qi, invigorating blood, resolving toxicity strategy in treatment of 30 cases of atrophic gastritis with intestinal metaplasia atypical hyperplasia. Journal of Medicine & Pharmacy of Chinese Minorities. 2009;23(12):8–10. [Google Scholar]
- 17.Liu X. F., Li D. G., Wang S. P., et al. Huazhuo Jiedu Formula for treatment of chronic atrophic gastritis with intestinal metaplasia. Hebei Journal of Traditional Chinese Medicine. 2011;33(8):1139–1141. [Google Scholar]
- 18.Gao S. F., Li D. G., Cui J. Efficacy of Huazhuo Jiedu Hewei Decoction in the treatment of chronic atrophic gastritis precancerous lesions. Chinese Journal of Gerontology. 2010;30(4):460–462. [Google Scholar]
- 19.Gu C. Y., Liu J. J., Liu X. B., et al. Efficacy of Yiqi Huoxue Formula for treatment of chronic atrophic gastritis. Hebei Journal of Traditional Chinese Medicine. 2012;34(1):14–16. [Google Scholar]
- 20.Yan H., Sun D. J., Wang S., et al. Jianpi Huoxue Qudu Decoction in treatment of H. pylori chronic atrophic gastritis. Shandong Medical Journal. 2014;54(42):79–81. [Google Scholar]
- 21.Bai H. Y., Guo L. F., Du Y. R. Jiedu Huoxue Decoction in the treatment of chronic atrophic gastritis with mild to moderate intestinal metaplasia. Shanghai Journal of Traditional Chinese Medicine. 2007;41(6):37–38. [Google Scholar]
- 22.Wei M., Yang J. X., Yang H. M., et al. Effect of benefiting qi, transforming stasis, relieving toxicity strategy in the rat model of chronic atrophic gastritis with dysplasia. Chinese Journal of Gastroenterology and Hepatology. 2011;21(10):916–919. [Google Scholar]
- 23.Zhao J., Meng J., Yang J. X. Effect of Xiaopi Granules on proliferation and apoptosis in the gastric mucosa of chronic atrophic gastritis rats with atypical hyperplasia. Journal of Traditional Chinese Medicine. 2012;53(24):2118–2121. [Google Scholar]
- 24.Li J. Q., Li C., Liu X., Wang J., Sun J. N. Improvement in gastric mucosal lesions in the rat model of chronic atrophic gastritis following administration of Shenqi Xiaopi Granules. Jiangsu Journal of Traditional Chinese Medicine. 2013;45(5):69–71. [Google Scholar]
- 25.Zhang S. S., Li Q. G., Tang X. D., et al. Consensus on Chinese medicine diagnosis and treatment of chronic atrophic gastritis (2009 Shenzhen) Chinese Journal of Integrated Traditional and Western Medicine on Digestion. 2010;18(5):345–349. [Google Scholar]
- 26.Zhang W. D., Li J. X., Chen Z. S., et al. Consensus on integrated Chinese and Western medicine diagnosis and treatment of chronic gastritis (2011 Tianjin) Modern Digestion & Intervention. 2011;17(3):172–177. [Google Scholar]
- 27.Tang X. D., Li Z. H., Li B. S., et al. Guideline of treatment and diagnosis of chronic gastritis. Chinese Modern Distance Education of China. 2011;9(10):123–125. [Google Scholar]
- 28.Gan H. J., Liang L. L., Han M. L., Guo S. R., Lin X. J. Relationship between syndrome distribution and sex in chronic atrophic gastritis. China Journal of Traditional Chinese Medicine and Pharmacy. 2015;30(7):2456–2459. [Google Scholar]
- 29.Lin W. G., Liang L. L., Han M. L., Guo S. R., Lin X. J. Association between syndrome element qi stagnation and disease site in chronic gastritis. China Journal of Traditional Chinese Medicine and Pharmacy. 2015;11(30):4074–4076. [Google Scholar]
- 30.Han M. L., Lin X. J., Gan H. J., Gao S. Literature review of Chinese medicine syndrome distribution rules of chronic gastritis. China Journal of Traditional Chinese Medicine and Pharmacy. 2014;29(3):900–903. [Google Scholar]
- 31.Li P. C., Ding X., Guo Q., Su Z. Q. Literature review of Chinese medicine syndromes and syndrome element distribution features of chronic gastritis. Liaoning Journal of Traditional Chinese Medicine. 2014;41(12):2532–2534. [Google Scholar]
- 32.Chen R. H., Zhang G., Su Z. Q., Zong X. Y., Li P. C., Ding X. Chinese medicine syndrome classification of Helicobacter pylori associated gastritis. Journal of Beijing University of Traditional Chinese Medicine. 2014;37(3):156–159. [Google Scholar]
- 33.Su Z. Q., Li P. C., Guo Q., et al. Syndrome pattern transformation in chronic gastritis. Journal of Beijing University of Traditional Chinese Medicine. 2015;38(11):762–771. [Google Scholar]
- 34.Zheng X. Y. Clinical Guideline of New Drugs for Traditional Chinese Medicine (Trial) China Medical Science Press; 1997 (Chinese) [Google Scholar]
- 35.State Bureau of Technical Supervision. Consensus Statement on Chronic Gastritis. China Medical Science Press; 1997 (Chinese) [Google Scholar]
- 36.Spleen and Stomach Disease Association of China Association of Chinese Medicine. Consensus statement on traditional Chinese treatment of chronic atrophic gastritis. Journal of Traditional Chinese Medicine. 2010;51(8):749–753. [Google Scholar]
- 37.Tian D. L. Traditional Chinese Internal Medicine. Beijing, China: Chinese Medicine Press; 2005 (Chinese) [Google Scholar]
- 38.Reise S. P., Waller N. G., Comrey A. L. Factor analysis and scale revision. Psychological Assessment. 2000;12(3):287–297. doi: 10.1037//1040-3590.12.3.287. [DOI] [PubMed] [Google Scholar]
- 39.Kelton M. L., LeardMann C. A., Smith B., et al. Exploratory factor analysis of self-reported symptoms in a large, population-based military cohort. BMC Medical Research Methodology. 2010;10(1, article 94) doi: 10.1186/1471-2288-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wirth R. J., Edwards M. C. Item factor analysis: current approaches and future directions. Psychological Methods. 2007;12(1):58–79. doi: 10.1037/1082-989x.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Der Eijk C., Rose J. Risky business: factor analysis of survey data—assessing the probability of incorrect dimensionalisation. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0118900.e0118900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scheier R. L. Finding pearls in an ocean of data. Computerworld. 2001;35(30):49–50. [Google Scholar]
- 43.Guo L., Wang Y. Y., Zhang Z. B. Annotations on the concept of syndrome. Journal of Beijing University of Chinese Medicine. 2003;26(2):5–8. [Google Scholar]
- 44.Li Y. H. Syndrome factors and formula factors. China Journal of Traditional Chinese Medicine and Pharmacy. 2009;24(2):117–121. [Google Scholar]