Abstract
Background
Computerised cognitive–behavioural therapy (CCBT) helps improve mental health outcomes in White populations. However, no studies have examined whether CCBT is acceptable and beneficial for African Americans.
Aims
We studied differences in CCBT use and self-reported change in depression and anxiety symptoms among 91 African Americans and 499 White primary care patients aged 18–75, enrolled in a randomised clinical trial of collaborative care embedded with an online treatment for depression and anxiety.
Method
Patients with moderate levels of mood and/or anxiety symptoms (PHQ-9 or GAD-7≥10) were randomised to receive either care-manager-guided access to the proven-effective Beating the Blues® CCBT programme or usual care from their primary care doctor.
Results
Compared with White participants, African Americans were less likely to start the CCBT programme (P=0.01), and those who did completed fewer sessions and were less likely to complete the full programme (P=0.03). Despite lower engagement, however, African Americans who started the CCBT programme experienced a greater decrease in self-reported depressive symptoms (estimated 8-session change: −6.6 v. −5.5; P=0.06) and similar decrease in anxiety symptoms (−5.3 v. −5.6; P=0.80) compared with White participants.
Conclusions
CCBT may be an efficient and scalable first-step to improving minority mental health and reducing disparities in access to evidence-based healthcare.
Declaration of interest
None.
Copyright and usage
© The Royal College of Psychiatrists 2017. This is an open access article distributed under the terms of the Creative Commons Non-Commercial, No Derivatives (CC BY-NC-ND) license.
Depression and anxiety are common in the general population and a growing source of disability.1,2 There is limited access to evidence-based treatment, particularly among African Americans,3 who may be at increased risk for chronic depression and anxiety-related disorders.4,5 Further, disparities in mental healthcare are widened by the increased stigma surrounding mental illness that makes African Americans less likely to pursue treatment, even if it is through their primary care physician (PCP).6
As access to the internet has become more ubiquitous, online strategies for mental health treatment have emerged as an alternative to in-person psychotherapy. Internet-delivered computerised cognitive–behavioural therapy (CCBT) is one of the more common adjuvants or replacements for traditional face to face that has been proven effective in reducing depression and anxiety symptoms.7,8 These CCBT programmes are typically online multimedia programmes designed to teach users through a series of modules that can include narratives, video vignettes, interactive worksheets, the basic concepts of cognitive–behavioural therapy and the skills for managing their mental health symptoms. CCBT programmes used in clinical practice can be accompanied by some form of professional human support to encourage the user to complete the online session and reinforce the CBT skills learned through the programme. Adherence and efficacy of these CCBT programmes are higher when there is a human support component than in self-help formats that lack this support.9
Given CCBT’s strong evidence base, low cost and scalability, this type of internet intervention has the potential to increase access to high-quality mental health treatment, particularly for underserved populations; however, few CCBT trials include Black and minority ethnic participants,9 and no large trials have reported on racial differences in CCBT engagement or outcomes. To fill this gap in the literature, we examined differences in CCBT use and self-reported symptoms between African American and White primary care patients enrolled in a large comparative effectiveness trial.
Method
Participants in this study were part of the Online Treatment for Mood and Anxiety Disorders Trial, an NIMH-funded clinical trial approved by the University of Pittsburgh’s Institutional Review Board. This trial examined whether a collaborative care approach delivering CCBT, either alone or combined with an Internet Support Group (ISG), is effective for treating mental health in a primary care setting.
PCPs from 26 offices in the southwestern Pennsylvania region of the USA, all connected through an electronic medical record system, were notified of patients’ possible trial eligibility via an automated electronic message. The PCP then referred interested anxious and/or depressed patients aged 18–75, with reliable access to both the internet and telephone to the Online Treatment Trial. Study assessors contacted referred patients via telephone, and those who scored ≥10 on either the Patient Health Questionnaire (PHQ-9)10 or the Generalised Anxiety Disorder (GAD-7) Scale,11 signifying at least moderately elevated symptoms, and met all other eligibility criteria (e.g. no psychotic disorder; medically stable; not currently in mental health treatment) were mailed a consent form and telephoned within 1 week to review the form and obtain their consent on a recorded line. If so provided, we requested the patient to return the signed consent form and then administered our baseline assessment battery, which included socio-demographics, PRIME MD depression and anxiety modules,12 and use of pharmacotherapy.
We randomised protocol-eligible patients in a 3:3:1 ratio to either (1) a CCBT-only group with 24/7 patient access to the ‘Beating the Blues’ CCBT programme provided under the guidance of a care manager, (2) a CCBT+ ISG with additional access to a password-protected and moderated ISG or (3) their PCP’s ‘usual care’.
Study setting
Computerised cognitive–behavioural therapy
Patients randomised to either of the two groups with access to CCBT received username and password for ‘Beating the Blues’, an internet-based programme that delivers simple and easily understood text, audio and audiovisual clips to maintain patient interest. It consists of eight 50-min interactive sessions and ‘homework’ to complete between weekly sessions (e.g. thought labelling, pleasurable activities and problem-solving worksheet). The participants were prompted to enter their mood symptoms using the PHQ-9 and their anxiety symptoms using the GAD-7 at the start of each CCBT session.
Care manager support
We selected two college-educated research assistants as our care managers. Participants in either of the CCBT arms were assigned to one of the care managers who telephoned each intervention patient after randomisation to conduct a structured mental health assessment that included their prior mental health history and current use and interest in pharmacotherapy. Afterwards, they guided patients in how to first log into the CCBT programme and answered any questions they had. For the following 6 months, the care manager encouraged the patient to complete a new session every 1–2 weeks and offered support that involved monitoring the participant’s progress via reports generated by the CCBT programme and emailing to congratulate them for successfully completing a session. In addition, our care managers recommended general lifestyle adjustments including promotion of social engagement, exercise, adequate sleep, nutrition, reducing alcohol and quitting tobacco. If the participant reported a worsening of symptoms, the care manager emailed or telephoned the at-risk individual to provide support and/or reinforce use of the learnt CBT skills. If a participant did not start or complete a session in more than 2 weeks, the care manager would email them to encourage them to continue with the programme. The care manager would telephone in the case of more complex psychosocial issues, suicidal ideation, changes in pharmacotherapy or technical problems. In most cases, however, the mode of contact was based on participant preference and/or reachability.
During weekly case-review meetings, care managers reviewed all new patients and those with elevated and/or unresponsive symptoms with the specialty team consisting of the psychiatrist (J.F.K.), psychologist (B.H.B.) and general practitioner (B.L.R.). The care managers also had an additional meeting once a week with the study psychologist to review difficult cases. We recorded the number of emails, telephone calls and total contacts to each participant.
Statistical analyses
In a previous report, we analysed improvements in mood and anxiety symptoms assessed by blinded research assistants at 6 months and found that although patients assigned to the CCBT-only and CCBT+ISG groups both reported significant improvements in their symptoms compared with those in their physician’s usual care, there were no significant differences in symptom improvements between the CCBT-only and CCBT+ISG groups.13 Therefore, for the current analyses, we combined participants randomised to CCBT-only and CCBT+ISG groups, but did not include the usual care group. Further, our analyses only included those who self-identified as African American or White (11 participants in the ‘other’ race/ethnic group were excluded). We compared socio-demographic factors, baseline symptoms and the number of CCBT sessions completed by racial group (African American v. White). All categorical variable P-values are based on a chi-squared test. Continuous variable P-values are based on a t-test or rank-sum test for two-group comparisons. We assessed changes in self-reported depression and anxiety symptoms using linear mixed models controlling for age, gender, education, baseline depression/anxiety and baseline pharmacotherapy use. We first evaluated whether the change in symptom outcome across the eight sessions differentiated by race (i.e. session-by-race interaction). Where interaction effects were non-significant, they were removed from the model and only the main effect reported. In order to assess whether the relationship between baseline PHQ-9 or GAD-7 and starting/completing the CCBT sessions varied by race, we modelled starting/completing CCBT in logistic regression models that included the main effect of baseline PHQ-9 or GAD-7 scores and their interaction with race. These models were adjusted for age, gender, education and baseline pharmacotherapy. All statistical analyses were performed using Stata® 14 software (College Station, TX).
Results
Of the 2884 patients PCPs referred, 954 met eligibility criteria, 704 consented and were randomised, and 601 were assigned to either of the two groups with CCBT access (91 African American, 499 White, 11 other). Compared with White people, African Americans were younger, had higher baseline PHQ-9 scores and were less likely to be using pharmacotherapy at study entry (76% v. 90%, P<0.01; Table 1).
Table 1. Baseline socio-demographic and clinical characteristics and engagement in computerised cognitive–behavioural therapy programme.
| Characteristics | African American participants (N=91) | White participants (N=499) | P | Adjusted P |
|---|---|---|---|---|
| Age, mean (s.d.) | 39.9 (13.9) | 43.6 (14.2) | 0.02 | NA |
| Male, n (%) | 12 (13) | 110 (22) | 0.05 | NA |
| High school diploma or higher, n (%) | 70 (77) | 414 (83) | 0.17 | NA |
| Mental health diagnosis | 0.97 | NA | ||
| Depression only, n (%) | 38 (42) | 205 (41) | ||
| Anxiety only, n (%) | 6 (7) | 45 (9) | ||
| Depression and anxiety, n (%) | 45 (49) | 235 (47) | ||
| PHQ-9,a mean (s.d.) | 14.4 (4.5) | 13.1 (5.0) | 0.01 | NA |
| GAD-7,b mean (s.d.) | 13.2 (4.1) | 12.8 (4.4) | 0.63 | NA |
| Pharmacotherapy use, n (%) | 69 (76) | 449 (90) | <0.001 | NA |
| Started first session, n (%) | 68 (75) | 432 (87) | 0.01 | 0.01 |
| Completed all eight sessions, n (%) | 20 (29) | 186 (43) | 0.03 | 0.09 |
| Sessions completed, mean (s.d.) | ||||
| ≤3 months | 4.2 (2.8) | 4.8 (2.5) | 0.08 | 0.10 |
| ≤6 months | 4.7 (2.7) | 5.5 (2.7) | 0.03 | 0.07 |
PHQ-9 and GAD-7 scores were assessed by research assistants, blinded to patient randomisation status, over the telephone at baseline. The baseline assessor-administered PHQ-9 scores were highly correlated with self-entered PHQ-9 scores at session 1 (r=0.53; P<0.01). Race was self-reported. Primary Care Evaluation of Mental Disorders (PRIME-MD) was used to evaluate depression and anxiety diagnosis. Adjusted models controlled for age, gender, education, PHQ-9 and baseline pharmacotherapy use.
PHQ-9=Patient Health Questionnaire 9-item Scale, assessor-administered.
GAD-7=Generalised Anxiety Disorder 7-item Scale, assessor-administered.
Engagement measures
African Americans were less likely than White people to start session 1 of the CCBT programme (75% v. 87%; P=0.01). Among those who started the programme, compared with White people, African Americans completed slightly fewer sessions at 6 months (mean 4.7 v. 5.5; P=0.03). After adjusting for age, gender, education, pharmacotherapy and baseline PHQ-9 depression scores, African Americans still trended towards being less likely than White people to complete all eight sessions (Table 1). In the total sample, baseline-assessor-administered PHQ-9 depression and GAD-7 anxiety scores did not predict the likelihood of starting or completing the CCBT programme.
Mental health outcomes
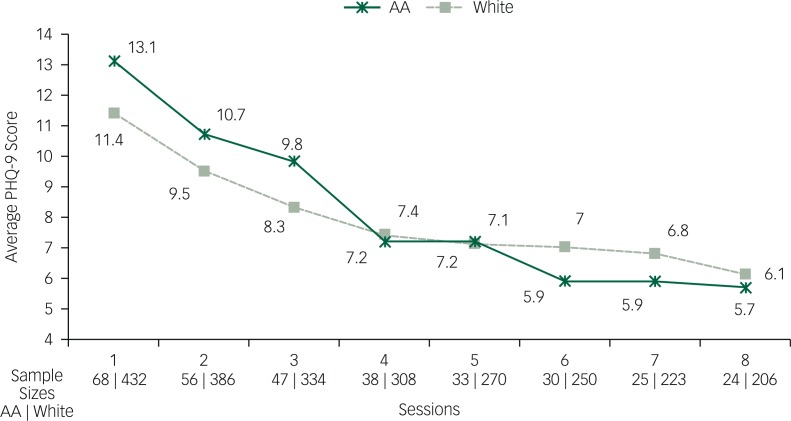
Of those participants who started the CCBT programme, African Americans trended towards a greater decrease in depressive symptoms compared with White people (estimated 8-session change: −6.6 v. −5.5; P=0.06) (Fig. 1) but similar decline in anxiety (estimated 8-session change: −5.3 v. −5.6; P=0.80) over the course of the eight CCBT sessions.
Fig. 1. Decline in average PHQ-9 scores at each session by race. AA=African American; PHQ-9=9-item Patient Health Questionnaire. PHQ-9 scores were self-entered at the beginning of each CCBT session. Changes in depression and anxiety symptom outcomes were assessed using linear mixed models controlling for age, gender, education, baseline symptom and baseline pharmacotherapy use. We first evaluated whether the change in symptom outcome across the eight sessions differentiated by race (i.e. session-by-race interaction). Where interaction effects were non-significant, they were removed from the model and only the main effect reported.
Care manager process measures
The care managers made a median of 14 total contacts (inter-quartile range (IQR) 11–18) to participants. Although the total number of contacts did not differ between African American and White people, care managers telephoned African Americans more often than White participants (median (IQR)=5 (3–7) and 3 (2–5), respectively, P<0.001), but sent fewer email messages to African Americans than to White people (median (IQR)=9 (6–11) and 10 (7–14), respectively, P<0.001). However, the number of telephone contacts was not associated with change in PHQ (r=0.01; P=0.91) or GAD scores (r=0.05; P=0.31).
Pharmacotherapy use
The three-way interaction between session, race and baseline pharmacotherapy use was non-significant (P=0.7013). Thus, the effect of race (African American v. White) on PHQ-9 decline was not dependent on baseline pharma use. Further, baseline pharmacotherapy use was not a predictor of decline in PHQ-9 (P=0.7877) or GAD-7 (P=0.6713) scores.
Discussion
Both African American and White anxious and/or depressed primary care patients benefitted from an internet-delivered CCBT programme delivered via a collaborative care strategy. Although we observed that African Americans were less likely than White people to engage with our CCBT programme, African Americans who did so trended towards a greater benefit from the programme than their White counterparts.
To the best of our knowledge, this is the first study to specifically examine racial differences in the level of engagement and/or benefit derived from CCBT for mental health symptoms.9 Two studies testing CCBT programmes for substance use treatment found CCBT improved coping and duration of abstinence in adult samples with a majority of African American participants.14,15 Two paediatric studies examined CCBT as a treatment for depression16 and anxiety17 in cohorts that included Black and minority ethnic participants. Yet, none of these studies specifically tested for racial/ethnic differences in programme acceptance or outcomes. Thus, until this study, there has been no evidence on whether CCBT is a feasible and/or effective treatment for mental health conditions among minority populations.
There are several possible reasons for the racial differences in engagement with CCBT in our report. Compared with White people, African American participants in this study reported more severe depressive symptoms, which is a known contributor to dropout or non-participation in internet-based programmes.18 It should be noted, however, we did not find baseline depression scores to predict the likelihood of starting or completing CCBT. Thus, although African Americans reported more depressive symptoms at baseline than White people, the severity of their depressive symptoms did not explain their lower level of engagement.
Another barrier to CCBT engagement among African Americans may be that the Beating the Blues programme is a culturally generic treatment not tailored specifically for minority patients. Our African American participants may have felt the intervention content was less culturally relevant, engaging and helpful. To better understand minority engagement and how CCBT can be most effective to a more diverse population, future studies would benefit from qualitative data assessing minority participant’s perceptions of the programme and barriers to uptake.
Despite the lower engagement among our African American participants, the average number of sessions completed and the overall adherence to the programme were similar or better than that reported in previous studies testing online-based mental health treatments.18–20 High dropout and low completion rates are characteristic of most CCBT studies, even those that do not include any racial or ethnic minorities.21 Although African Americans appear to be at higher risk for attrition from CCBT programmes, there is a need for innovative efforts to improve engagement in CCBT programmes for all racial/ethnic groups. In fact, although this is a large-scale, adequately powered study, the population may not be representative. Future studies examining race and CCBT outcomes may find no racial differences in uptake; thus, the findings from this study will benefit from replication in other large-scale trials that cut across different, more diverse geographic regions.
Care manager support was a critical component of the delivered intervention. Several studies have found that computerised self-help programme is only effective when the treatment is professionally supported.22 Care managers in this study were supervised research assistants with a college level education, who provided support to participants and made on average 14 telephone and email contacts with each participant. This is particularly important given that participants’ perceived absence of support has been noted as a primary reason for poor adherence and treatment dropout.23 In a recent large-scale pragmatic trial, Gilbody et al 20 compared CCBT (Beating the Blues and MoodGYM) to usual care; CCBT for depression showed no benefit over usual care; however, the intervention lacked a structured psychological support and guidance by a clinician or someone trained in psychology. Instead, participants received telephone technical support and general encouragement to continue the programme.20 Participants in their trial reported this level of support to be inadequate,23 and as a potential consequence, one-quarter of the participants had dropped out of the study by 4 months.20
In this study, care manager support was not correlated with improvements in depression or anxiety symptoms which may support evidence suggesting that some patients require support whereas others appreciate the anonymity that CCBT offers.23 In addition, a care manager contacted those participants more often who were in need of the most support. Participants who progressed through the programme and showed improvements with little intervention were less likely to receive frequent contacts. It should also be noted that, although there were no racial group differences in total contacts, African Americans received more telephone contacts and fewer email contacts than White people. These racial differences in mode of contact could be due to participant’s expressed preference for a particular mode of contact or it may be an indication of particular support needs. This potentially interesting finding was unexpected and will need to be replicated and explored further in future studies.
African Americans in this study were less likely to report using pharmacotherapy than White people. This finding is consistent with data that suggest African Americans are less likely to receive guideline-concordant depression care than White people24 and may partially account for the higher baseline depressive symptoms among African Americans. The group differences in pharmacotherapy could be explained by African Americans’ reluctance towards seeking treatment, their increased risk of pharmacotherapy-related side-effects or lack of access to specialised psychiatric care.25 Indeed, if findings from this study are replicated, CCBT may be a potential mechanism for improving disparities in mental healthcare.
Limitations
Two main features of this study limit its generalisability. First, our trial was conducted within single geographic region and health system in the USA. Still, we enrolled patients from over two dozen primary care sites located across rural, suburban and urban southwest Pennsylvania. Second, we required participants to have email address and internet access from a desk computer; the CCBT programme was not accessible via mobile device. As a result, we may have excluded some lower-income patients who could have benefited from CCBT but lacked internet access. Internet interventions that can be accessed via mobile phone may be more effective for reaching lower-income patients. Nevertheless, our cohort was socio-economically diverse with over 18% of participants being African American and 1 out of 5 participants having less than a high school education.
Other limitations of this study include our inability to adequately account for the effect of pharmacotherapy use on outcomes. Although our statistical models controlled for baseline pharmacotherapy use (yes or no), we currently do not have data on adherence or change in pharmacotherapy use over the course of the study. Further, we were not able to include a control group in our analyses, as patients randomised to the usual care group (not reported here) did not have access to the online self-report depression and anxiety measures that were part of the CCBT programme. Finally, owing to this being a pragmatic trial, the frequency of care manager contacts varied among patients depending on their specific needs and may have confounded our findings. Although the number of contacts was not statistically associated with change in depression or anxiety symptoms, it is difficult to determine the specific impact of care coach support on outcomes without having a comparison group that received CCBT without care coach support.
To date, this is the largest sample of minority patients included in a clinical trial testing CCBT for depression and/or anxiety and the first to our knowledge to test racial differences in engagement and benefit of an internet-delivered mental health programme. The widespread deployment of CCBT into primary care could become an efficient and widely replicable first step to providing effective evidence-based mental healthcare to diverse populations. Improving engagement, particularly among minority populations, however, will be the major challenge to the future implementation of CCBT as an effective mental health intervention. Opportunities to improve user adherence may include fostering community and collaboration such as is possible with ISGs,9 programmes that are customised and adapt to the user and their behaviour, and the inclusion of more culturally relevant material.26 Whatever the methods for increasing engagement, guidance from a professionally trained care manager or clinician who provides psychological support is an important component of an effective CCBT intervention.
Funding
This project was supported by grant numbers MH093501 (PI: Rollman) from the National Institute of Mental Health and K12HS022989 from the Agency for Healthcare Research and Quality (C.J.). ClinicalTrials.gov Identifier: NCT01482806.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 593–602. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3: e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995–2005. Med Care 2008; 46: 668–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Himle JA, Baser RE, Taylor RJ, Campbell RD, Jackson JS. Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. J Anxiety Disord 2009; 23: 578–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry 2007; 64: 305–15. [DOI] [PubMed] [Google Scholar]
- 6.Neighbors HW, Caldwell C, Williams DR, Nesse R, Taylor RJ, Bullard KM, et al. Race, ethnicity, and the use of services for mental disorders: results from the National Survey of American Life. Arch Gen Psychiatry 2007; 64: 485–94. [DOI] [PubMed] [Google Scholar]
- 7.Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One 2010; 5: e13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adelman CB, Panza KE, Bartley CA, Bontempo A, Bloch MH. A meta-analysis of computerized cognitive-behavioral therapy for the treatment of DSM-5 anxiety disorders. J Clin Psychiatry 2014; 75: e695–704. [DOI] [PubMed] [Google Scholar]
- 9.Knowles SE, Toms G, Sanders C, Bee P, Lovell K, Rennick-Egglestone S, et al. Qualitative meta-synthesis of user experience of computerised therapy for depression and anxiety. PLoS One 2014; 9: e84323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–7. [DOI] [PubMed] [Google Scholar]
- 12.Spitzer RL, Williams JBW, Kroenke K, Linzer M, deGruy FV 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA 1994; 272: 1749–56. [PubMed] [Google Scholar]
- 13.Rollman BL, Belnap BH, Rothenberger SD, Abebe K, Rotondi AJ, Karp JF. Online treatments for mood and anxiety disorders in primary care: a randomized controlled trial. J Gen Intern Med 2016; 31: S316. [Google Scholar]
- 14.Kiluk BD, Nich C, Babuscio T, Carroll KM. Quality versus quantity: acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction 2010; 105: 2120–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Budney AJ, Stanger C, Tilford J, Scherer EB, Brown PC, Li Z, et al. Computer-assisted behavioral therapy and contingency management for cannabis use disorder. Psychol Addict Behav 2015; 29: 501–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iloabachie C, Wells C, Goodwin B, Baldwin M, Vanderplough-Booth K, Gladstone T, et al. Adolescent and parent experiences with a primary care/Internet-based depression prevention intervention (CATCH-IT). Gen Hosp Psychiatry 2011; 33: 543–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khanna MS, Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: results of a randomized clinical trial. J Consult Clin Psychol 2010; 78: 737–45. [DOI] [PubMed] [Google Scholar]
- 18.Kaltenthaler E, Sutcliffe P, Parry G, Beverley C, Rees A, Ferriter M. The acceptability to patients of computerized cognitive behaviour therapy for depression: a systematic review. Psychol Med 2008; 38: 1521–30. [DOI] [PubMed] [Google Scholar]
- 19.So M, Yamaguchi S, Hashimoto S, Sado M, Furukawa TA, McCrone P. Is computerised CBT really helpful for adult depression? A meta-analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. BMC Psychiatry 2013; 13: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbody S, Littlewood E, Hewitt C, Brierley G, Tharmanathan P, Araya R, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 2015; 351: h5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waller R, Gilbody S. Barriers to the uptake of computerized cognitive behavioural therapy: a systematic review of the quantitative and qualitative evidence. Psychol Med 2009; 39: 705–12. [DOI] [PubMed] [Google Scholar]
- 22.Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther 2009; 38: 196–205. [DOI] [PubMed] [Google Scholar]
- 23.Knowles SE, Lovell K, Bower P, Gilbody S, Littlewood E, Lester H. Patient experience of computerised therapy for depression in primary care. BMJ Open 2015; 5: e008581.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agyemang AA, Mezuk B, Perrin P, Rybarczyk B. Quality of depression treatment in Black Americans with major depression and comorbid medical illness. Gen Hosp Psychiatry 2014; 36: 431–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lawson WB. Clinical issues in the pharmacotherapy of African-Americans. Psychopharmacol Bull 1996; 32: 275–81. [PubMed] [Google Scholar]
- 26.Griner D, Smith TB. Culturally adapted mental health intervention: a meta-analytic review. Psychotherapy (Chic) 2006; 43: 531–48. [DOI] [PubMed] [Google Scholar]