
Keywords: nerve regeneration, apolipoprotein E, genetic polymorphism, post-stroke depression, risk, regional resting-state cerebral blood flow, rs429358, rs7412, cerebral infarction, neural regeneration
Abstract
Recent reports have shown that apolipoprotein E (APOE) polymorphisms are involved in neurodegenerative disease. However, it is unclear whether APOE affects post-stroke depression. Accordingly, we hypothesized that APOE polymorphisms modify the risk of post-stroke depression. Here, we performed a hospital-based case-control study (including 76 cerebral infarction cases with post-stroke depression, 88 cerebral infarction cases without post-stroke depression, and 109 controls without any evidence of post-stroke depression or cerebral infarction) to determine possible association between APOE rs429358 and rs7412 polymorphisms and risk of post-stroke depression. Our findings show no difference among the groups with regards genotype distribution of the rs7412 polymorphism. In contrast, APOE genotypes with rs429358-C alleles increased the risk of post-stroke depression. Further, the rs429358 polymorphism was associated with significantly decreased regional cerebral blood flow values in the left temporal lobe of post-stroke depression cases. Additionally, the rs429358 polymorphism was not only associated with depression severity, but with increasing serum levels of total cholesterol. These results suggest that the APOE rs429358 polymorphism is associated with increased risk of developing post-stroke depression, and that APOE rs429358-C allele genotypes may be detrimental to recovery of nerve function after stoke. Indeed, these findings provide clinical data for future post-stroke depression gene interventions.
Introduction
As the third leading cause of death worldwide, and a major health issue in the elderly population, stroke not only results in physical impairments such as disability, but also leads to social nonparticipation and psychological disease (Robinson and Jorge, 2015; Weaver and Liu, 2015). Of these, post-stroke depression (PSD) is the most common neuropsychiatric impairment, and often accompanied by apathy, fatigue, feelings of worthlessness, sleep changes, and anhedonia. Indeed, PSD is the most significant factor in causing low quality of life in stroke patients (Dwyer Hollender, 2014; Eum and Yim, 2015; Robinson and Jorge, 2015). However, to date, PSD pathogenesis remains unclear. Studies show that PSD may be related to certain behavioral, neurobiological, and social factors (Robinson and Jorge, 2015). Additionally, molecular epidemiological studies suggest that genetic factors play an important role in PSD pathogenesis (Tang et al., 2013; Zhou et al., 2015; Zhao et al., 2016). Yet despite considerable efforts in past decades, PSD-related genes have not been identified.
Apolipoprotein E (APOE), a major chylomicron apoprotein, plays an important physiological role in regulation of overall lipid and lipoprotein homeostasis (Zhao et al., 2014). Further, APOE plays an important role in neuronal repair (Hatters et al., 2006; Zhang et al., 2013). Recently, studies have shown that two polymorphisms of the APOE gene (namely, rs429358 T > C and rs7412 C > T) may be associated with APOE dysfunction and increased risk of several neurological and cardiovascular diseases, including Alzheimer's disease (Cosentino et al., 2008; Jofre-Monseny et al., 2008; McGuinness et al., 2010; Seripa et al., 2011; Yi et al., 2014; Lagos et al., 2015; Yuan et al., 2015). However, association between these polymorphisms and PSD has not yet been investigated. In addition, their correlation with regional cerebral blood flow (rCBF), a valuable marker for brain function including neural regeneration and activity (Venkat et al., 2016), has not previously been performed. Thus, in this study, we hypothesized that APOE rs429358 and rs7412 polymorphisms modify PSD risk by disrupting recovery of brain function after stoke. Accordingly, we performed a hospital-based case-control study to determine the influence of these two polymorphisms on PSD risk and brain function.
Subjects and Methods
Subjects
This study was a hospital-based retrospective case-control study (Figure 1). The procedures were performed in accordance with the Guidelines for Medical Research Projects Involving Human Samples, and the protocol was approved by the Medical Ethics Committee of the Affiliated Hospital of Youjiang Medical University for Nationalities, China (approved No. 2011016). Every patient with a newly diagnosed cerebral infarction was recruited at the Affiliated Hospital of Youjiang Medical University for Nationalities by Youjiang Cancer Institution staff members using a standard interviewer-administered questionnaire. The inclusion criteria for cases were: (1) cerebral infarction confirmed by magnetic resonance imaging (MRI) and/or computed tomography (CT) scanning, according to diagnostic criteria from the 4th Cerebral-Vascular Diseases Conference of China (Wu, 1997); (2) the study objective was understood and informed consent provided; (3) ability to complete the necessary investigations and questionnaires; (4) cases without a history of receiving blood cholesterol-lowering agents or antidepressants; (5) cases undergoing rCBF perfusion imaging examination; and (6) 6-month follow-up completed, and available blood samples and clinical data. The exclusion criteria were: (1) cases with depression but without cerebral infarction; (2) cases with a history of substance abuse, psychotic disorder, bipolar disorder, psychiatric illness, severe aphasia or dysarthria, intracranial hemorrhage, unconsciousness, severe infection, chronic inflammatory disease, tumors, hematologic disease, autoimmune disease, or severe heart, liver, or kidney damage; and (3) cases that died, dropped out, or had absent information during follow-up. Based on these inclusion and exclusion criteria, 164 patients with first-ever acute cerebral infarction were consecutively recruited within 7 days of stroke incidence from April 2013 to July 2014. All cases received subsequent stroke assessments by a single trained neurologist and psychiatrist, at both acute and chronic stages, specifically, approximately 2 weeks and 1, 3, and 6 months after stroke onset. Patients were screened and assessed for PSD using the 24-item Hamilton Depression Rating Scale (HAMD) questionnaire (Ning, 1986) and World Health Organisation Composite International Diagnostic Interview (Kessler and Üstün, 2004). Patients with cerebral infarction were included in the PSD group (n = 76) if they had both HAMD scores ≥ 8 and were diagnosed with depression. Alternatively, they were included in the non-PSD (NPSD) group (n = 88). During the same period, controls (n = 109) without any evidence of psychiatric disorder, mental illness, heart vessel disease, or other brain disorders, were randomly selected from a pool of healthy volunteers who had visited a general health check-up center at the same hospital for a routinely scheduled physical examination. Controls were frequently matched to cases with respect to age (± 5 years) and gender. Of those asked, 100% agreed to participate in this investigative study.
Figure 1.
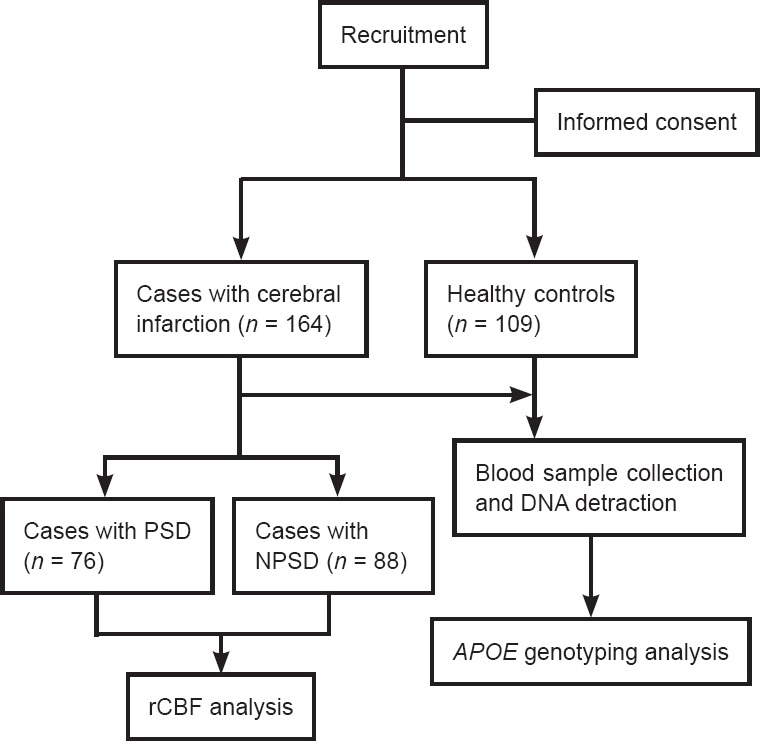
Study design.
PSD: Post-stroke depression; NPSD: non-post-stroke depression; rCBF: regional cerebral blood flow; APOE: apolipoprotein E.
After providing written consent, 4 mL peripheral blood samples were obtained from all participants at the Affiliated Hospital of Youjiang Medical University for Nationalities for APOE genotype analysis. Demographic information and clinical data were also collected at the same hospital using a standard interviewer-administered questionnaire and/or medical records.
rCBF perfusion imaging assay
All subjects underwent rCBF perfusion imaging to examine brain function one month after stoke. rCBF perfusion imaging analysis was performed using a Siemens Symbia T2 single-photon emission computed tomography (SPECT)/CT Dual Head System (Siemens, Munich, Germany) between 8:00 a.m. and 9:00 a.m. Subjects were orally treated with potassium perchlorate (400 mg), and with their heads in a head holder, were instructed to keep their eyes closed for 30 minutes. Subjects were then injected with 740 MBq (20 mCi) 99mTc- ethyl cysteinate dimer (99mTc-ECD, HTA Co., Ltd., Beijing, China). Fifteen minutes after injection, SPECT/CT data were acquired using a 128 × 128 matrix with a zoom of 1.23 and 15% symmetric energy window at 140 keV. Images were acquired at a rate of 35 s/frame by rotating the camera a total of 360° at 6° intervals. In total, 36 frames were collected. Data were analyzed using CBF perfusion imaging software (Brain Tomo PROC; Siemens) by two experienced nuclear medicine physicians that were blinded to the patients' clinical data. Relative rCBF (rrCBF) values in regions of interest were calculated by: average rCBF value in region of interest/average rCBF value in ipsilateral cerebellar cortex.
APOE genotyping
Genomic DNA was extracted from peripheral blood leukocytes. APOE rs429358 and rs7412 genotypes were determined by TaqMan polymerase chain reaction (TaqMan-PCR) using an iCycler iQ real-time PCR detection system (iQ5; Bio-Rad, Hercules, CA, USA). Each PCR was performed in 25 μL total volumes consisting of 1 × TaqMAN® Universal Master Mix II (cat#4440041; Applied Biosystems [ABI], Foster City, CA, USA), 0.2 μM each probe and each primer (cat# 4351379; ABI), and 50–100 ng genomic DNA. PCR programs had an initial denaturation of 10 minutes at 95°C, followed by 40 cycles of 15 seconds at 95°C and 1 minute at 60°C. Data analysis for allele discrimination was performed using iCycler iQ software (Bio-Rad). Controls were included in each run for quality control, and repeated genotyping of random 5% subsets yielded 100% identical genotypes. Additionally, sequencing analyses performed using the ABI 3730XL DNA Sequencing System with universal primers (5′-GGCGC GGACA TGGAG GAC-3′ and 5′-GCCCC GGCCT GGTAC ACT-3′) for both polymorphisms yielded 100% identical genotypes.
Statistical analysis
Results were analyzed using SPSS 18.0 software (SPSS Institute, Chicago, IL, USA). Comparison of variables among groups was performed using Student's t-test, one-way analysis of variance, chi-square test, or Fisher's exact test. Spearman r test was used to analyze correlation between genotypes and other variables. Using a frequently matched design, non-conditional logistical regression was performed to estimate odds ratios (OR) and 95% confidence intervals (CI) for PSD risk. Statistical significance was considered at α = 0.05.
Results
Characteristics of subjects
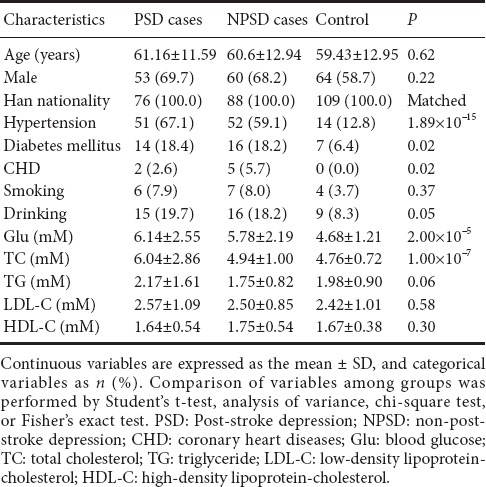
One hundred and sixty-four patients (113 males and 51 females; mean age 60.8 ± 11.9 years) completed the 6-month follow-up. Overall, 76 patients were ultimately diagnosed as PSD cases, producing an incidence of 46.3%. The remaining 88 cases were included as NPSD. Distribution of demographic and clinical characteristics (including age, sex, smoking and drinking status, and coronary heart disease, hypertension, and diabetes mellitus history) was not significantly different between PSD and NPSD cases (Table 1). However, compared with controls without cerebral infarction, cerebral infarction cases had a higher frequency of risk factors including hypertension, diabetes mellitus, and blood glucose (Table 1).
Table 1.
Participants demographic and clinical characteristics
APOE rs429358 polymorphism increases PSD risk
Analysis of APOE rs429358 and rs7412 polymorphisms in control individuals showed a genotype distribution consistent with Hardy-Weinberg equilibrium (P > 0.05). Meanwhile, logistic regression analysis indicated that only the rs429358 polymorphism significantly correlated with PSD risk (Table 2). Compared with rs429358-T allele homozygotes (rs429358-TT), rs429358-T and -C allele heterozygotes (rs429358-TC) had a higher risk of PSD (adjusted OR [95%CI], 2.93 [1.50–5.72] for PSD versus NPSD; 3.31 [1.27–8.64] for PSD versus controls; and 3.17 [1.42–7.05] for PSD versus combined NPSD and control groups). The corresponding OR (95%CI) for rs429358-C allele homozygotes (rs429358-CC) were 9.80 (1.95–49.24), 11.98 (1.60–89.44), and 11.24 (2.98–42.40), respectively. Altogether, these results show that PSD risk is associated with the number of rs429358-C alleles.
Table 2.
APOE rs429358 and rs7412 polymorphisms and PSD risk
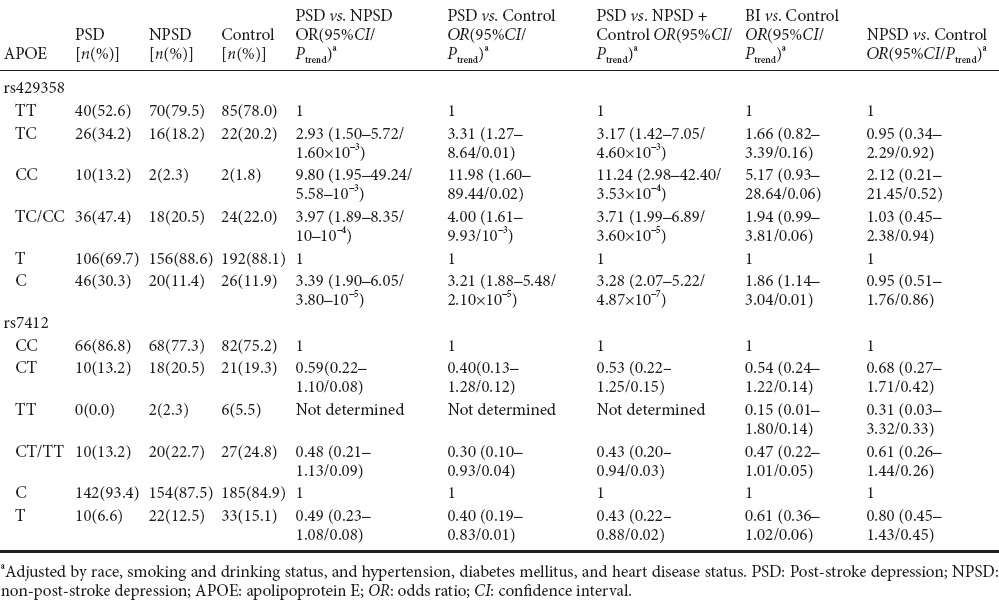
Indeed, a higher frequency of rs429358-C alleles was found in cerebral infarction cases compared with healthy controls (18.1% versus 11.9%). Logistic regression analysis showed that the risk of rs429358-C alleles for brain infarction was 1.86 (1.14–3.04). However, this risk was not significant after adjusting for other risk variables (including smoking and drinking, and hypertension, heart disease, and diabetes mellitus history) (P > 0.05; Table 2).
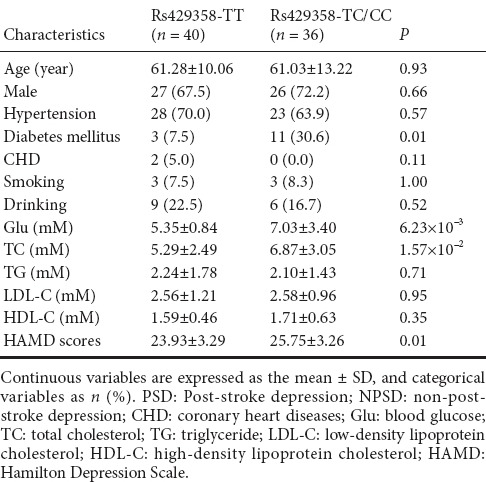
APOE rs429358 polymorphism correlates with clinical features of PSD cases
Next, we analyzed the effect of APOE rs429358 polymorphism on clinical features of PSD cases (Table 3). We found rs429358 was significantly related to increasing levels of serum glucose (rs429358-TC/CC versus rs429358-TT, 7.03 ± 3.40 versus 5.35 ± 0.84 mM; relative coefficient, 0.24), and also total cholesterol (6.87 ± 3.05 versus 5.29 ± 2.49 mM; relative coefficient, 0.37). Moreover, rs429358 affected the degree of depression for PSD cases (P = 0.01).
Table 3.
Association between APOE rs429358 polymorphism and clinical characteristics of PSD cases
Effect of APOE rs429358 polymorphism on rCBF in PSD cases
Previous studies have shown that rCBF positively correlates with brain function and depression (Paschali et al., 2009, 2010; Cantisani et al., 2015; Simpson et al., 2016). Therefore, to determine whether the APOE rs429358 polymorphism affects rCBF, we examined rCBF in regions of interest (including the frontal lobe, temporal lobe, parietal lobe, occipital lobe, basal ganglia, and thalamus) in all PSD and NPSD cases (Tables 4 and 5). Our results show lower rrCBF in the left temporal and parietal lobes compared with the corresponding right lobes among PSD cases (0.71 versus 0.77 for temporal lobe and 0.72 versus 0.80 for parietal lobe; P < 0.05), but not among NPSD cases. Furthermore, comparative analysis showed significantly decreasing rrCBF in the left temporal lobe of PSD and NPSD cases (P = 0.04) (Table 4).
Table 4.
rrCBF in PSD and NPSD cases
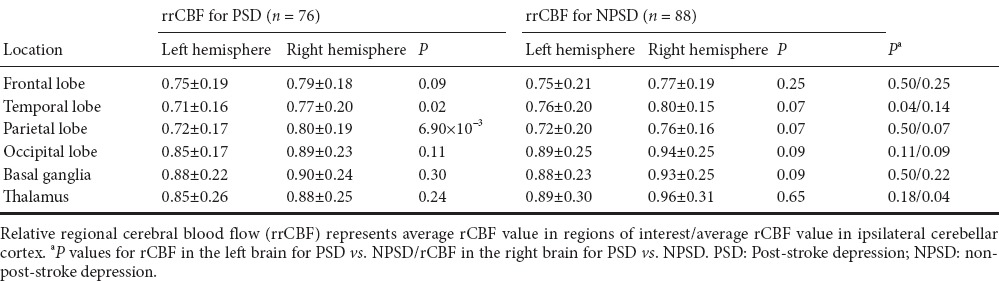
Table 5.
Effect of APOE rs429358 polymorphism on rrCBF in PSD cases
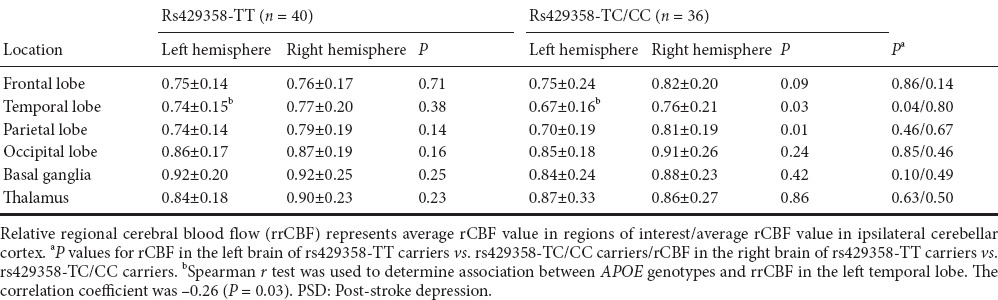
To further investigate the relationship between APOE rs429358 polymorphism and rCBF, we performed a stratified analysis (Table 5). Because of the small number of subjects with APOE rs429358-CC, genotypes, rs429358-CC and rs429358-TC were combined into a single group (i.e., rs429358-TC/CC), with APOE genotypes then divided into two strata. In PSD cases with APOE rs429358-TC/CC genotypes, decreasing rrCBF was still observed in the left temporal and parietal lobes, but not in those with rs429358-TT genotypes. Comparative analysis of cases with and without APOE rs429358-TC/CC showed that rs429358 polymorphism is significantly associated with rrCBF in the left temporal lobe (0.74 ± 0.15 for rs429358-TT and 0.67 ± 0.16 for rs429358-TC/CC, r = –0.26). Taken together, these findings suggest that the APOE rs429358 polymorphism may modify brain function.
Discussion
To date, no studies have examined the role of APOE polymorphism in PSD risk. Here, we examined association between APOE polymorphisms and PSD risk among the Guangxi population of China. Accordingly, we found that APOE genotypes with rs429358-C alleles are associated with increased PSD risk among this population (OR, 3.17 for rs429358-TC; 11.24, for rs429358-CC).
Stroke, such as cerebral infarction, is one of the leading causes of morbidity and long-term disability worldwide (Robinson and Jorge, 2015). Epidemiological studies have shown that approximately 40% of stroke patients develop PSD after acute stroke, and thus PSD is a common and serious psychiatric complication of stroke (Robinson and Jorge, 2015). Compared with stroke patients without depression, PSD typically leaves patients with severer deficits in daily living activities, a worsen functional outcome, severer cognitive deficits, and higher mortality (Fang and Cheng, 2009; Dwyer Hollender, 2014; Eum and Yim, 2015; Robinson and Jorge, 2015). In this study, approximately 46% of our cerebral infarction cases had depression and ultimately developed PSD. Furthermore, we found that PSD cases had higher levels of serum total cholesterol compared with NPSD cases, and that increasing serum total cholesterol levels increased both PSD and NPSD risk. These results suggest a strong biological relationship between PSD and stroke.
APOE is an important apolipoprotein gene located on chromosome 19q13.2. The protein encoded by APOE consists of 299 amino acid residues (relative molecular weight, 34 kDa), and contains amphipathic α-helical lipid-binding structural domains that enable APOE to interact with members of the low-density lipoprotein receptor family. Through this interaction, APOE displays a key role in lipid transport in both plasma and the central nervous system (Hatters et al., 2006). Accumulating evidence shows that dysregulation of APOE expression and genetic variance of APOE affects APOE function, and eventually leads to pathogenesis of certain nervous and cardiovascular diseases (Hatters et al., 2006; Cosentino et al., 2008; Jofre-Monseny et al., 2008; Lagos et al., 2015; Luckhoff et al., 2015; Yuan et al., 2015; Lu et al., 2016).
With regards genetic variance, more than 5,000 single-nucleotide polymorphisms in APOE have been identified. Two of these (namely rs429358 and rs7412) influence functional and structural properties of the APOE protein, and are associated with development of neurodegenerative disease (Cosentino et al., 2008; Agarwal and Tripathi, 2014; Giau et al., 2015; Luckhoff et al., 2015), coronary heart disease (Chouinard-Watkins and Plourde, 2014; Yousuf and Iqbal, 2015), and liver disease (Shen et al., 2015). For example, Cosentino et al. (2008) investigated the effect of APOE polymorphisms on Alzheimer's disease development, and found that the ε4 allele (which is derived from a combination of rs429358 and rs7412) is a risk biomarker for Alzheimer's disease. APOE rs429358 and rs7412 polymorphisms also affect antioxidant and anti-inflammatory properties of APOE, and the ε4 allele is associated with relatively higher oxidative stress and a higher pro-inflammatory state (Jofre-Monseny et al., 2008; Yuan et al., 2015). In this study, the APOE rs429358 polymorphism was associated not only with increased PSD risk, but also more severe depression in PSD cases. Interestingly, our results also show that patients with more severe deficits are more likely to develop PSD. Supporting our results, several recent reports have shown that differential functional status of APOE (resulting from genetic polymorphic status and expression levels) is related to cognitive performance (Zhang et al., 2012; Rajan et al., 2014; Wang et al., 2014; Feng et al., 2015) and PSD pathogenesis (Zhang et al., 2013).
To investigate the effect of APOE rs429358 polymorphism on PSD risk, rCBF in stroke cases was examined. This was mainly performed as rCBF is a valuable marker for brain function, including neural regeneration and activity (Venkat et al., 2016), therefore any disruption in rCBF may affect neural repair after stoke and impact upon PSD pathogenesis. Recent evidence has shown that rCBF significantly correlates with depressive disorder, and may reflect pathological-psychological change in PSD (Cantisani et al., 2015). Here, we found a decreasing rCBF score in the left temporal lobe of PSD cases that was modified by APOE rs429358 polymorphism. Additionally, rs429358 was associated with increasing serum glucose and total cholesterol levels. Consistent with these results, a recent meta-analysis found that the APOE rs429358 polymorphism is associated with lipid profile changes and increased serum total cholesterol levels (Lu et al., 2016). Collectively, these results suggest that rs429358 may modulate PSD risk by modifying brain function and lipid profiles. Hence, APOE screening may be helpful for identifying PSD patients from those with abnormal brain function, or glucose and lipid profiles.
There are several limitations to our study. First, despite analyzing two polymorphisms, we did not examine any other APOE polymorphisms. Second, a potential selection bias may have occurred through selection of hospital-based control subjects. Third, the risk value of the rs429358 polymorphism may be underestimated because stroke risk is slightly associated with this polymorphism, and stroke as a variable might be a potential confounding factor. Fourth, our findings are based on a relatively small number of subjects, and limited further by the small number of stratified subjects. Finally, although we investigated the effect of APOE rs429358 polymorphism on clinical features, with rCBF as a brain function marker of PSD, the underlying mechanism(s) remain largely unknown. Therefore, additional functional analyses based on larger samples and combining APOE and brain function (including neural regeneration and repair) are required.
In conclusion, this is the first report to investigate association between APOE polymorphisms and PSD risk in the Guangxi population of China. Further, our findings provide evidence that the rs429358 polymorphism of APOE is essential to PSD etiology. Similarly, our findings support the hypothesis that APOE polymorphisms contribute to PSD risk. Understanding different genetic and clinical values in individual patients will allow more informed counseling with regards screening, prevention, treatment options, follow-up plans, and secondary prevention approaches. Therefore, in combination with information on functional neural regeneration during stoke, our findings may improve identification of high-risk populations of PSD.
Footnotes
Funding: This study was supported in part by the National Natural Science Foundation of China, No. 81160146.
Declaration of patient consent: The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest: None declared.
Plagiarism check: This paper was screened twice using CrossCheck to verify originality before publication.
Peer review: This paper was double-blinded and stringently reviewed by international expert reviewers.
Copyedited by James R, Yajima W, Yu J, Li CH, Qiu Y, Song LP, Zhao M
References
- Agarwal R, Tripathi CB. Association of apolipoprotein E genetic variation in Alzheimer's disease in Indian population: a meta-analysis. Am J Alzheimers Dis Other Demen. 2014;29:575–582. doi: 10.1177/1533317514531443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantisani A, Koenig T, Stegmayer K, Federspiel A, Horn H, Müller TJ, Wiest R, Strik W, Walther S. EEG marker of inhibitory brain activity correlates with resting-state cerebral blood flow in the reward system in major depression. Eur Arch Psychiatry Clin Neurosci. 2015 doi: 10.1007/s00406-015-0652-7. doi:10.1007/s00406-015-0652-7. [DOI] [PubMed] [Google Scholar]
- Chouinard-Watkins R, Plourde M. Fatty acid metabolism in carriers of apolipoprotein E epsilon 4 allele: is it contributing to higher risk of cognitive decline and coronary heart disease? Nutrients. 2014;6:4452–4471. doi: 10.3390/nu6104452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosentino S, Scarmeas N, Helzner E, Glymour MM, Brandt J, Albert M, Blacker D, Stern Y. APOE ε4 allele predicts faster cognitive decline in mild Alzheimer's disease. Neurology. 2008;70:1842–1849. doi: 10.1212/01.wnl.0000304038.37421.cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer Hollender K. Screening, diagnosis, and treatment of post-stroke depression. J Neurosci Nurs. 2014;46:135–141. doi: 10.1097/JNN.0000000000000047. [DOI] [PubMed] [Google Scholar]
- Eum Y, Yim J. Literature and art therapy in post-stroke psychological disorders. Tohoku J Exp Med. 2015;235:17–23. doi: 10.1620/tjem.235.17. [DOI] [PubMed] [Google Scholar]
- Fang J, Cheng Q. Etiological mechanisms of post-stroke depression: a review. Neurol Res. 2009;31:904–909. doi: 10.1179/174313209X385752. [DOI] [PubMed] [Google Scholar]
- Feng F, Lu SS, Hu CY, Gong FF, Qian ZZ, Yang HY, Wu YL, Zhao YY, Bi P, Sun YH. Association between apolipoprotein E gene polymorphism and depression. J Clin Neurosci. 2015;22:1232–1238. doi: 10.1016/j.jocn.2015.02.012. [DOI] [PubMed] [Google Scholar]
- Giau VV, Bagyinszky E, An SS, Kim SY. Role of apolipoprotein E in neurodegenerative diseases. Neuropsychiatr Dis Treat. 2015;11:1723–1737. doi: 10.2147/NDT.S84266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatters DM, Peters-Libeu CA, Weisgraber KH. Apolipoprotein E structure: insights into function. Trends Biochem Sci. 2006;31:445–454. doi: 10.1016/j.tibs.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Jofre-Monseny L, Minihane AM, Rimbach G. Impact of APOE genotype on oxidative stress, inflammation and disease risk. Mol Nutr Food Res. 2008;52:131–145. doi: 10.1002/mnfr.200700322. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Üstün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagos J, Zambrano T, Rosales A, Salazar LA. APOE polymorphisms contribute to reduced atorvastatin response in Chilean Amerindian subjects. Int J Mol Sci. 2015;16:7890–7899. doi: 10.3390/ijms16047890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Z, Wu X, Jin X, Peng F, Lin J. Apolipoprotein E ε2/ε3/ε4 variant in association with obstructive sleep apnoea and lipid profile: A meta-analysis. J Int Med Res. 2016;44:3–14. doi: 10.1177/0300060515611539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luckhoff HK, Brand T, van Velden DP, Kidd M, Fisher LR, van Rensburg SJ, Kotze MJ. Clinical relevance of apolipoprotein E genotyping based on a family history of Alzheimer's disease. Curr Alzheimer Res. 2015;12:210–217. doi: 10.2174/1567205012666150302154354. [DOI] [PubMed] [Google Scholar]
- McGuinness B, Carson R, Barrett SL, Craig D, Passmore AP. Apolipoprotein epsilon4 and neuropsychological performance in Alzheimer's disease and vascular dementia. Neurosci Lett. 2010;483:62–66. doi: 10.1016/j.neulet.2010.07.063. [DOI] [PubMed] [Google Scholar]
- Ning G. A application of Hamilton anxiety scale in Chinese neurasthenia. Zhonghua Shenjing Jingshen Ke Zazhi. 1986;32:342–344. [Google Scholar]
- Paschali A, Messinis L, Lyros E, Constantoyannis C, Kefalopoulou Z, Lakiotis V, Papathanasopoulos P, Vassilakos P. Neuropsychological functions and rCBF SPECT in Parkinson's disease patients considered candidates for deep brain stimulation. Eur J Nucl Med Mol Imaging. 2009;36:1851–1858. doi: 10.1007/s00259-009-1168-z. [DOI] [PubMed] [Google Scholar]
- Paschali A, Messinis L, Kargiotis O, Lakiotis V, Kefalopoulou Z, Constantoyannis C, Papathanasopoulos P, Vassilakos P. SPECT neuroimaging and neuropsychological functions in different stages of Parkinson's disease. Eur J Nucl Med Mol Imaging. 2010;37:1128–1140. doi: 10.1007/s00259-010-1381-9. [DOI] [PubMed] [Google Scholar]
- Rajan KB, Wilson RS, Skarupski KA, de Leon CM, Evans DA. Gene-behavior interaction of depressive symptoms and the apolipoprotein E {varepsilon}4 allele on cognitive decline. Psychosom Med. 2014;76:101–108. doi: 10.1097/PSY.0000000000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson RG, Jorge RE. Post-stroke depression: A review. Am J Psychiatry. 2015;173:221–231. doi: 10.1176/appi.ajp.2015.15030363. [DOI] [PubMed] [Google Scholar]
- Seripa D, D'Onofrio G, Panza F, Cascavilla L, Masullo C, Pilotto A. The genetics of the human APOE polymorphism. Rejuvenation Res. 2011;14:491–500. doi: 10.1089/rej.2011.1169. [DOI] [PubMed] [Google Scholar]
- Shen Y, li M, Ye X, Bi Q. Association of apolipoprotein E with the progression of hepatitis B virus-related liver disease. Int J Clin Exp Pathol. 2015;8:14749–14756. [PMC free article] [PubMed] [Google Scholar]
- Simpson BN, Kim M, Chuang Y-F, Beason-Held L, Kitner-Triolo M, Kraut M, Lirette ST, Windham BG, Griswold ME, Legido-Quigley C, Thambisetty M. Blood metabolite markers of cognitive performance and brain function in aging. J Cereb Blood Flow Metab. 2016;36:1212–1223. doi: 10.1177/0271678X15611678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang WK, Tang N, Liao CD, Liang HJ, Mok VC, Ungvari GS, Wong KS. Serotonin receptor 2C gene polymorphism associated with post-stroke depression in Chinese patients. Genet Mol Res. 2013;12:1546–1553. doi: 10.4238/2013.May.13.8. [DOI] [PubMed] [Google Scholar]
- Venkat P, Chopp M, Chen J. New insights into coupling and uncoupling of cerebral blood flow and metabolism in the brain. Croat Med J. 2016;57:223–228. doi: 10.3325/cmj.2016.57.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Ma W, Rong Y, Liu L. The association between apolipoprotein E gene polymorphism and mild cognitive impairment among different ethnic minority groups in China. Int J Alzheimers Dis. 2014;2014:150628. doi: 10.1155/2014/150628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver J, Liu KJ. Does normobaric hyperoxia increase oxidative stress in acute ischemic stroke? A critical review of the literature. Med Gas Res. 2015;5:11. doi: 10.1186/s13618-015-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X. The fourth Chinese conference proceedings about cerebrovascular diseases. Cuzhong he Naoxueguan Jibing. 1997;4:51–55. [Google Scholar]
- Yi L, Wu T, Luo W, Zhou W, Wu J. A non-invasive, rapid method to genotype late-onset Alzheimer's disease-related apolipoprotein E gene polymorphisms. Neural Regen Res. 2014;9:69–75. doi: 10.4103/1673-5374.125332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousuf FA, Iqbal MP. Review: Apolipoprotein E (Apo E) gene polymorphism and coronary heart disease in Asian populations. Pak J Pharm Sci. 2015;28:1439–1444. [PubMed] [Google Scholar]
- Yuan L, Liu J, Dong L, Cai C, Wang S, Wang B, Xiao R. Effects of APOE rs429358, rs7412 and GSTM1/GSTT1 polymorphism on plasma and erythrocyte antioxidant parameters and cognition in old Chinese adults. Nutrients. 2015;7:8261–8273. doi: 10.3390/nu7105391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Shen XH, Qian MC, Sun JS, Zhong H, Yang JH, Lin M, Li L. Effects of apolipoprotein E genetic polymorphism on susceptibility of depression and efficacy of antidepressants. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2012;34:595–600. doi: 10.3881/j.issn.1000-503X.2012.06.011. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Mu J, Li J, Li W, Song J. Aberrant apolipoprotein E expression and cognitive dysfunction in patients with poststroke depression. Genet Test Mol Biomarkers. 2013;17:47–51. doi: 10.1089/gtmb.2012.0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Q, Guo Y, Yang D, Yang T, Meng X. Serotonin Transporter gene 5-httlpr polymorphism as a protective factor against the progression of post-stroke depression. Mol Neurobiol. 2016;53:1699–1705. doi: 10.1007/s12035-015-9120-7. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Li J, Tang Q, Gao J, Chen C, Jing L, Zhang P, Li S. Apolipoprotein E mimetic peptide protects against diffuse brain injury. Neural Regen Res. 2014;9:463–473. doi: 10.4103/1673-5374.130060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z, Ding X, Yang Q, Hu J, Shang X, Huang X, Ge L, Zhou T. Association between single-nucleotide polymorphisms of the tyrosine kinase receptor B (TrkB) and post-stroke depression in China. PLoS One. 2015;10:e0144301. doi: 10.1371/journal.pone.0144301. [DOI] [PMC free article] [PubMed] [Google Scholar]


