Abstract
Background
Delays to definitive care are associated with poor outcomes after trauma and medical emergencies. It is unknown whether inter-hospital transfer delays affect outcomes for non-traumatic acute surgical conditions.
Methods
We performed a retrospective cohort study of patient transfers for acute surgical conditions within a regional transfer network from 2009-2013. Delay was defined as more than 24 hours from presentation to transfer request and categorized as 1 or 2+ days. The primary outcome was post-transfer death or hospice. Bivariate and multivariable logistic regression were performed.
Results
The cohort included 2,091 patient transfers. Delays of 2 or more days were associated with death or hospice in unadjusted analyses but there was no difference after adjustment. Predictors of post-transfer death or hospice included older age, higher comorbidity scores, and greater severity of illness.
Conclusions
Delays in transfer request were not associated with post-transfer mortality or discharge to hospice, suggesting effective triage of non-traumatic acute surgical patients.
Brief Summary
Delays in transfer worsen outcomes for trauma and some medical emergencies. This retrospective cohort study evaluated the impact of delay in transfer request for non-traumatic surgical emergencies, finding that increased time to transfer request was not associated with increased likelihood of post-transfer mortality or discharge to hospice.
Keywords: transfer, inter-hospital, acute care surgery, delay, quality, death, hospice
Introduction
Inter-hospital transfer of patients with acute non-traumatic surgical conditions occurs commonly, and can mitigate mismatches between patient needs and facility capabilities.1,2 Patients who are admitted in transfer have more comorbidities and greater physiologic and metabolic derangements than their counterparts who are directly admitted to the same hospitals.1,3,4 Prior work reveals that after risk-adjustment for patient and clinical factors, transferred patients have longer lengths of stay, incur greater charges, and are more likely to die in the hospital.5-7
It is unclear whether observed differences in outcomes after transfer versus direct admission are fully explained by selection of the most critically ill patients in a given region for transfer to higher levels of care, or if delayed inter-hospital transfer decisions and processes may also contribute to worse outcomes for this population. Transfer delays have been associated with worse outcomes after trauma, stroke, and acute myocardial infarction. In these patient populations, development of care algorithms and regional transfer networks have streamlined care and improved outcomes, including reduced mortality.8-12 By contrast, for most non-traumatic surgical conditions, decisions regarding indications for and timing of inter-hospital transfer still occur without clear guidelines or organization. These decisions occur at transferring facilities and are not well-captured in the current literature from academic medical centers. Pre-transfer care may expedite initial resuscitation and treatment, resulting in better ultimate outcomes. Or, it may delay definitive diagnosis and treatment, potentially worsening outcomes.
We sought to understand the role of pre-transfer duration of care on post-transfer outcomes. We hypothesized that patients with longer delays prior to transfer request would have increased post-transfer mortality and discharge to hospice.
Material and methods
We performed a retrospective cohort study of patient transfers from acute care hospitals to a tertiary referral center (accepting facility) in the Southeast United States, Vanderbilt University Medical Center (VUMC), from January 1, 2009 through December 31, 2013. We included adult patients who were admitted to the accepting facility's general surgery, thoracic surgery, urologic surgery, and vascular surgery services from another acute care facility. Patient transfers from non-acute care facilities, including rehabilitation hospitals and long term acute care facilities, were excluded (2% of patients). Patient transfers for a different problem than the initial problem on presentation, including transfers for a complication of referring facility care (6% of cohort), were not included as it was not feasible to determine the time of onset of the problem requiring transfer. Patients who were transferred to the accepting facility but not admitted were also excluded because it was not possible to determine whether the transfer was for care by one of the included surgical services. The study was approved by Vanderbilt University's Human Research Protection Program and Institutional Review Board.
Data sources included the accepting facility's administrative records, patient electronic medical records, and referring facility documents. Administrative data elements were obtained from VUMC's Enterprise Data Warehouse (EDW), which contains billing and clinical data for each patient encounter, as well as patient transfer documentation. Patient transfer requests are managed and documented by the Vanderbilt Access Center, which records the date and time of transfer request and obtains standardized information from referring facilities about patients being transferred. Referring facility records were consistently obtained by the Vanderbilt Access Center for the study duration. Data obtained from referring facility records were abstracted by manual chart review performed by a physician.
The analysis was performed at the level of the patient transfer, with each transfer evaluated as a unique encounter. The primary exposure was the duration of time under referring facility care from presentation to transfer request, i.e., time to request. Time to request was measured in both hours and days, and was categorized by days for the primary analysis (0-23 hours = 0 days, 24 to 47 hours = 1 day, 48 or more hours = 2+ days). Patients for whom the date of presentation was known, but the specific time of presentation was unknown (10%) were included, but time to request was conservatively rounded down to the nearest day.
The primary outcome was a composite of any of the following post-transfer events: in-hospital mortality, discharge to hospice, or mortality within 30 days of discharge. The outcome was determined based on VUMC records. Inpatient deaths were consistently documented in patient electronic medical records (EMRs). Discharge disposition, including discharge to hospice care, was documented in hospital administrative records. Post-discharge deaths were documented in one of two ways. Reports of death from patient providers and family members that were conveyed to VUMC personnel were documented in the EMR as clinical communications. This information was augmented by death reports from the United States Social Security Administration Death Master File, which were available for 2009 to 2011. Study follow-up began at the time of patient admission to an included VUMC surgical service and continued until development of the primary outcome, or 30 days post-discharge from the index hospitalization.
Estimates of effect were adjusted for relevant covariates that could potentially confound the association between time to transfer request and the post-transfer composite outcome. Covariates were selected a priori and included patient age, gender, race, insurance status, admitting surgical service, year of transfer request, comorbid conditions, severity of illness, whether the patient previously received care at the accepting facility for the transfer diagnosis, and whether the transfer was designated by the referring provider as an Emergency Medical Condition (EMC).
Patient comorbidities and severity of illness at the time of transfer were measured by calculating Elixhauser Comorbidity Scores and Acute Physiology Scores (APS) using previously published methods.13,14 Comorbidities were identified from the accepting facility's administrative records based on ICD-9 codes for the index admission, and reported as a single composite score for each patient. Acute Physiology Scores relied on the first set of laboratory tests and vital signs performed upon patient arrival to the accepting facility, as well as documentation of each patient's mental status on arrival according to the admitting service history and physical exam. Missing vital sign and basic laboratory values (3%) were coded as normal. Missing arterial blood gas values (76%) were also coded as normal, assuming that such tests would primarily be performed if there was clinical concern that they might be abnormal. This is consistent with assumptions made by the developers of the Acute Physiology Score in handling missing values.15
Descriptive statistics were provided for all study covariates. Continuous exposures were reported using means with standard deviations or medians with interquartile ranges where appropriate. Categorical variables were reported using frequencies and proportions. Covariates were compared for the primary exposure categories using chi squared tests for categorical variables and ANOVA and Kruskal-Wallis tests for parametric and non-parametric continuous variables, respectively. Bivariate logistic regression was used to compare the incidence of the death or hospice for relevant exposures. Multivariable logistic regression was performed to determine the adjusted association between transfer delay and death or hospice.
A separate model was created that did not include Acute Physiology Scores, theorizing that pre-transfer resuscitation might improve these scores which were measured upon arrival to the accepting facility. Other sensitivity analyses included measurement of transfer delay in hours rather than days, inclusion of travel intervals (times from transfer request to accepting facility admission) in measurement of transfer delays, and evaluation of variation in time to request for years with and without complete post-discharge death data as well as for individual components of the primary outcome (i.e. in-hospital mortality versus hospice discharge versus post-discharge mortality). All models were adjusted to account for within-subject correlation due to patients who had more than 1 eligible transfer during the study period (<10% of the sample).
A difference in referring center length of stay of 1 day was determined to be significant based on clinical factors. Using a student's t-test assuming independent events, a standard deviation of 5 days, and ratio of 1 event (death or hospice) per 10 encounters, an estimated 216 events were needed in order to reject the null hypothesis with a power of 0.8 at an alpha of 0.05.
Results
The study cohort included 2,091 patient transfers from 299 unique referring facilities. Patients were on average 57 ± 17 years old, 53% male, 86% white, and 33% commercially insured (Table 1). The median Elixhauser Comorbidity Score was 5 (interquartile range (IQR) 0-12) and median Acute Physiology Score was 3 (IQR 2-5). Most patients were admitted to a general surgical service at the accepting facility (60%). Forty-two percent previously received care at the accepting facility related to the transfer diagnosis. Most transfers were for a higher level of care (63%) and were designated as Emergency Medical Conditions (EMCs) (70.0%) (Table 1).
Table 1. Characteristics of Patient Transfers for Acute Surgical Conditions.
| Characteristic | Study Cohort N=2,091 |
|---|---|
|
| |
| Age (mean ± standard deviation) | 57 ± 17 |
|
| |
| Gender (N, %) | |
| Male | 1,106 (53) |
| Female | 985 (47) |
|
| |
| Race (N, %) | |
| White | 1,807 (86) |
| Non-White | 211 (10) |
| Unknown | 73 (4) |
|
| |
| Insurance Status (N, %) | |
| Private | 697 (33) |
| Medicare | 976 (47) |
| Medicaid/Uninsured | 418 (20) |
|
| |
| Surgical Service (N, %) | |
| General | 1,244 (60) |
| Vascular | 378 (18) |
| Thoracic | 221 (11) |
| Urologic | 248 (12) |
|
| |
| Elixhauser Comorbidity Score (median, IQRa) | 5 (0-12) |
|
| |
| Acute Physiology Score (median, IQRa) | 3 (2-5) |
|
| |
| Prior Accepting Facility Care for Transfer Diagnosis (N, %) | 881 (42) |
|
| |
| Year of Service (N, %) | |
| 2009 | 410 (20) |
| 2010 | 417 (20) |
| 2011 | 455 (22) |
| 2012 | 321 (15) |
| 2013 | 488 (23) |
|
| |
| Emergency Medical Condition (N, %) | 1,455 (70) |
|
| |
| Reason for Transfer (N, %) | |
| Higher Level of Care/Specialist Care | 1,311 (63) |
| Continuity of Care | 654 (31) |
| Patient/Family Request | 115 (6) |
| Other | 11 (<1) |
|
| |
| Pre-transfer Intervention (N, %) | 305 (15) |
|
| |
| Duration of Pre-Transfer and Transfer Processes | |
| Time to Transfer Request (days, median, IQRa) | 0 (0-1) |
| Time to Transfer Request (hours, median, IQRa) | 4 (2-27) |
| Transfer Request to Accepting Facility Admission (hours, median, IQRa) | 6 (4-10) |
IQR=Interquartile range
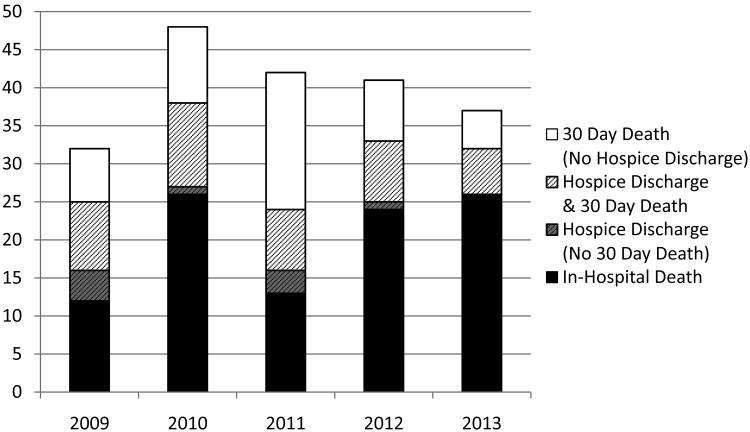
The composite outcome occurred in 10% of transfers (211 patients) (Figure 1). Approximately half were in-hospital deaths (101/211 patients). The majority of other events were deaths within 30 days of discharge (101/110). A lower proportion of non-hospice post-discharge deaths were captured in 2012 and 2013 relative to 2009-2011 due to unavailability of Social Security Administration death data after 2011 (p=0.02) (Figure 1).
Figure 1. Distribution of Components of Composite Outcome by Year of Transfer.
Patient transfers resulting in in-hospital death, discharge to hospice, or death within 30 days of discharge by year of transfer request (N=211).
Pre-transfer processes of care varied based on multiple factors. Longer times to request were observed for patients with Medicare insurance (p<0.01), more comorbid conditions (p<0.01), admission to Thoracic Surgery (p<0.01), transfers in earlier years of the study (p<0.01), and non-EMC transfers (Table 2). Times to request were shorter for patients admitted to Vascular surgery (p<0.01) (Table 2) and those who previously received care for the transfer diagnosis at the accepting facility (p<0.01) (Table 3). Pre-transfer interventions were performed less frequently in patient transfers that were designated as EMCs (10 versus 24%, p<0.01) and those with prior accepting facility care (6 versus 21%, p<0.01) (Table 3). Times to request did not vary based on year of transfer (p=0.34) or components of the composite outcome (p=0.52).
Table 2. Patient Transfer Characteristics by Time to Transfer Request.
| Characteristic | 0 Days N=1,202 | 1 Day N=403 | 2+ Days N=486 | Test of Significance |
|---|---|---|---|---|
|
| ||||
| Age (years, mean±SDa) | 56±17 | 57±17 | 58±16 | 0.44 |
|
| ||||
| Gender (N, %) | 0.70 | |||
| Male | 641 (58) | 216 (20) | 249 (23) | |
| Female | 561 (47) | 187 (19) | 237 (24) | |
|
| ||||
| Race (N, %) | 0.07 | |||
| White | 1060 (59) | 342 (19) | 405 (22) | |
| Non-White | 107 (51) | 43 (20) | 61 (29) | |
| Unknown | 35 (48) | 18 (19) | 20 (27) | |
|
| ||||
| Insurance (N, %) | <0.01 | |||
| Private | 401 (58) | 133 (19) | 163 (23) | |
| Medicare | 539 (55) | 184 (19) | 253 (26) | |
| Medicaid/Uninsured | 262 (63) | 86 (21) | 70 (17) | |
|
| ||||
| Surgical Service (N, %) | <0.01 | |||
| General | 715 (57) | 254 (20) | 275 (22) | |
| Vascular | 266 (70) | 50 (13) | 62 (16) | |
| Thoracic | 91 (41) | 45 (20) | 85 (38) | |
| Urologic | 130 (52) | 54 (22) | 64 (26) | |
|
| ||||
| Year of Service (N, %) | 0.01 | |||
| 2009 | 214 (52) | 91 (22) | 105 (26) | |
| 2010 | 228 (55) | 81 (19) | 108 (26) | |
| 2011 | 267 (59) | 80 (18) | 108 (24) | |
| 2012 | 188 (59) | 52 (16) | 81 (25) | |
| 2013 | 305 (63) | 99 (20) | 84 (17) | |
|
| ||||
| Elixhauser Comorbidity Score (mean±SDa) | 7±8 | 7±8 | 10±10 | <0.01 |
|
| ||||
| Acute Physiology Score (median, IQRb) | 3 (2-6) | 3 (2-5) | 4 (2-6) | 0.14 |
|
| ||||
| Prior Accepting Facility Care for Transfer Diagnosis (N, %) | 554 (63) | 180 (20) | 147 (17) | <0.01 |
|
| ||||
| Emergency Medical Condition (N, %) | 982 (68) | 268 (18) | 205 (14) | <0.01 |
|
| ||||
| Transfer Request to Accepting Facility Admission (hours, median, IQRb) | 5 (3-8) | 6 (4-10) | 10 (5-25) | <0.01 |
Standard deviation
Interquartile range
Table 3. Pre-Transfer Care Processes by Elective versus Emergency Medical Condition Transfer and by Prior Accepting Center Treatment for the Transfer Diagnosis.
| Care Process | Elective N=636 | EMCa N=1,455 | Test of Significance | Prior Careb N=881 | No Prior Care N=1210 | Test of Significance |
|---|---|---|---|---|---|---|
| Pre-Transfer Interventionc (N, %) | 155 (24) | 150 (10) | <0.01 | 49 (6%) | 256 (21%) | <0.01 |
| Time to Requestd (days, median, IQRf) | 1 (0-4) | 0 (0-1) | <0.01 | 0 (0-1) | 0 (0-2) | <0.01 |
| Time to Requestd (hours, median, IQRf) | 24 (3-83) | 3 (1-8) | <0.01 | 3 (1-15) | 5 (2-43) | <0.01 |
| Transfer Request to Accepting Facility Admission (hours, median, IQRf) | 7 (4-20) | 5 (4-8) | <0.01 | 6 (4-10) | 5 (3-9) | <0.01 |
EMC = Emergency Medical Condition
Prior Care included previous treatment at the accepting facility for the transfer diagnosis
Pre-Transfer Intervention included operative, endoscopic, radiologic, and critical care procedures
Time to Request = time from referring center presentation to transfer request
IQR = interquartile range
On unadjusted analysis, transfers with times to request of two or more days were more likely to result in death or discharge to hospice relative to transfer requests made on the day of presentation (OR 1.77, 95% CI 1.27-2.44) (Table 4). Patient transfers that resulted in the composite outcome were also older, had higher Elixhauser Comorbidity and Acute Physiology Scores, were more likely insured by Medicare relative to a Commercial payer, more likely admitted to Vascular Surgery, and more likely transferred in 2010 or 2012 relative to 2009. After adjustment for relevant covariates, time to request was not significantly associated with death or discharge to hospice (OR 1.18, 95% CI 0.74-1.87 for 1 day relative to 0 days and OR 1.26, 95% CI 0.81-1.96 for 2+ days relative to 0 days). Older age (OR 1.07, 95% CI 1.05-1.08), higher Elixhauser Comorbidity Scores (OR 1.10, 95% CI 1.08-1.13), higher Acute Physiology Scores (OR 1.14, 95% CI 1.10-1.18) and transfers in 2012 (OR 2.07, 95% CI 1.13-3.80) remained predictive of the composite outcome, while Medicare insurance (OR 0.60, 95% CI 0.37-0.97) and Urology admission (OR 0.53, 95% CI 0.29-0.95) were protective against death or hospice in the adjusted model (Table 4).
Table 4. Association of Patient Transfer Characteristics with Death or Discharge to Hospice.
| Characteristic | Unadjusted Odds (95% CI) | Adjusted Odds (95% CI) |
|---|---|---|
|
| ||
| Age | 1.05 (1.04-1.06) | 1.07 (1.05-1.08) |
|
| ||
| Female Gender | 0.82 (0.61-1.10) | 0.99 (0.70-1.40) |
|
| ||
| Race | ||
| White | REF | REF |
| Non-white | 1.39 (0.90-2.14) | 1.64 (0.96-2.82) |
| Unknown | 1.68 (0.86-3.25) | 1.33 (0.56-3.16) |
|
| ||
| Elixhauser Comorbidity Score | 1.13 (1.11-1.14) | 1.10 (1.08-1.13) |
|
| ||
| Acute Physiology Score | 1.17 (1.13-1.20) | 1.14 (1.10-1.18) |
|
| ||
| Insurance Status | ||
| Private | REF | REF |
| Medicare | 2.02 (1.43-2.87) | 0.60 (0.37-0.97) |
| Medicaid/None | 0.96 (0.60-1.56) | 1.43 (0.79-2.56) |
|
| ||
| Surgical Service | ||
|
| ||
| General | REF | REF |
| Vascular | 1.57 (1.10-2.24) | 1.33 (0.84-2.10) |
| Thoracic | 1.42 (0.91-2.22) | 1.30 (0.74-2.27) |
| Urologic | 0.68 (0.39-1.17) | 0.53 (0.29-0.95) |
|
| ||
| Year of Service | ||
| 2009 | REF | REF |
| 2010 | 1.61 (0.99-2.60) | 1.66 (0.92-2.98) |
| 2011 | 1.36 (0.84-2.20) | 1.50 (0.83-2.73) |
| 2012 | 1.83 (1.12-2.99) | 2.07 (1.13-3.80) |
| 2013 | 1.03 (0.63-1.68) | 1.17 (0.63-2.19) |
|
| ||
| Prior Accepting Facility Care for Transfer Diagnosis | 0.88 (0.66-1.18) | 1.38 (0.96-1.99) |
|
| ||
| Emergency Medical Condition | 0.91 (0.67-1.23) | 0.87 (0.58-1.29) |
|
| ||
| Time to Transfer Request (Days) | ||
| Zero Days | REF | REF |
| 1 Day | 1.14 (0.78-1.68) | 1.18 (0.74-1.87) |
| 2+ Days | 1.77 (1.27-2.44) | 1.26 (0.81-1.96) |
Sensitivity analyses supported primary findings. Limiting the cohort to patients with exact dates and times of presentation, times to transfer request of 2 or more days remained associated with an increased likelihood of the composite outcome relative to 0 days in unadjusted tests (OR 1.77, 95% CI 1.24-2.54), but there was no difference observed in the adjusted model (OR1.30, 95% CI 0.81-2.08). Measurement of the exposure in hours rather than days using restricted cubic splines to model the non-linear function did not improve model performance and yielded similar results. Re-defining the exposure as the total time from presentation at the referring facility to admission at the accepting facility (including travel time) also yielded similar results (for 2+ days unadjusted OR 1.55, 95% CI 1.14-2.12, adjusted OR 1.24, 95% CI 0.81-1.89). There was no significant difference in time to request for transfers resulting in in-hospital mortality versus those resulting in hospice discharge or post-discharge death (p=0.20). Times to request also did not vary for 2009-2011 versus 2012-2013 in patients with an event (p=0.34). Removal of the Acute Physiology Score from the model did not influence the outcome, demonstrating that the lack of association was not due to adjustment for theoretically improved physiology after a duration of pre-transfer resuscitation (adjusted OR 1.25, 95% CI 0.81-1.92 for 2+ days relative to 0 days).
Discussion
In this population of patients transferred to a non-trauma surgical service at a tertiary care facility, delays in transfer request were not associated with post-transfer mortality or hospice discharge after adjustment for patient severity of illness. With respect to the primary outcome, this suggests time-appropriate triage of non-traumatic acute surgical patients requiring transfer.
The study finding augments prior work in smaller samples of general surgical patients, which demonstrated that efficiency of other pre-transfer processes, including transportation mode, designated level of urgency, and time from transfer request to patient arrival at accepting facilities, did not influence post-transfer mortality.1,7 However, our findings in this non-trauma population differ from the known impact of pre-transfer delays in other patient populations. Delays in transfer to major trauma centers for traumatic surgical emergencies are associated with increased mortality.8-10 Transfer delays have also been implicated in higher orchiectomy rates for testicular torsion in pediatric patients and delayed reperfusion and increased mortality in patients with ST-elevation myocardial infarction.11,12,16 Further, within-facility delays in patient transfer from Emergency Departments to same-hospital ICUs have also been found to increase mortality.17
The finding that patients with older age and more significant comorbid conditions were more likely to experience the composite outcome was expected; however, it was surprising that patients with longest times to transfer request were older and had higher Elixhauser Comorbidity Scores. The reason and significance of this are unclear. Despite the lack of overall impact of transfer delay on death or hospice in the study population, future research is needed in this high risk sub-population, for whom greater guidance and decision support may be needed to inform timely patient selection for transfer.
We found that patients with prior accepting facility care for the transfer diagnosis had shorter times to transfer request and underwent fewer pre-transfer interventions. In discussing challenges of transfer, referring providers have previously cited difficulty determining when transfer is indicated for non-protocolized conditions, identifying an appropriate accepting facility, and negotiating the transfer.18 For patients who are established in care at another center, all three challenges may be significantly mitigated.
We also found that EMC transfers were more readily requested and accomplished, which suggests overall effectiveness of the Emergency Medical Treatment and Active Labor Act (EMTALA) in expediting transfer for patients who are perceived to have more emergent conditions.19 Greater variation existed in time to request and time from request to accepting facility admission for elective transfers, which may reflect challenging decision-making with respect to whether transfer is indicated as well as administrative issues such as bed availability, which may delay transfer once patients are accepted.
The primary outcome of mortality or hospice discharge is clearly relevant to patients and health systems; however, other outcomes that are important to patients may be more sensitive to the impact of transfer delays. For example, delays in care transitions that increase patient morbidity or debilitation could increase the likelihood that patients must be discharged to a higher level of care than their pre-admission location of residence (e.g. transitioning from functional independence at home to functional dependence in a skilled nursing facility). It will be important to investigate the impact of transfer delays other common patient-centric outcomes.
There are a number of strengths to our study. Data collection methods were robust, involving manual abstraction of date and timestamps as well as presenting and transfer diagnoses from referring facility records. This level of detailed temporal information and integration across multiple care settings at more than one institution cannot typically be obtained from large datasets, but is essential to understanding how pre-transfer processes impact post-transfer outcomes.
Some limitations must also be acknowledged. Data were derived from patient transfers to a single academic medical center, which limits generalizability to other centers, particularly non-academic referral facilities. The study population is relatively heterogeneous, encompassing four surgical disciplines. This may increase the generalizability of our findings, but limits our ability to make diagnosis-specific conclusions or recommendations. The study sample size and relatively rare primary outcome limited the number of allowable model covariates. As a result we were unable to adjust for specific diagnoses or referring hospital size or type. While the proposed model remains robust with adjustment for patient comorbid conditions as well as acute physiology, we are unable to account for other predictors of mortality in surgical patients, such as frailty.20
Patient mortalities that occurred prior to transfer were not captured in this population, so there was a theoretical selection bias toward patients who were less likely to experience the outcome. Based on data for the entire transfer population at the accepting facility, we estimate that we may have failed to capture 2-4 additional deaths in the study cohort. There is also potential for incomplete capture of post-discharge death based on discontinuation of Social Security Association (SSA) death reporting after 2011.21 Given that there was no significant variation in times to request for patient transfers in 2009-2011 versus 2012-2013 or for components of the primary outcome, we would not expect capture of additional post-discharge deaths to alter the study findings.
We also were unable to capture patients who were transferred to the accepting facility for surgical care but who were discharged from the Emergency Department without admission to an included surgical service. Based on data from our institution, this occurs in approximately 10% of all transfers. We cannot determine times to request for this population, but recognize that they are probably less likely to experience death or discharge to hospice given their conditions did not warrant inpatient admission. Finally, we are unable to determine specific reasons for delays in transfer request. Given the significant variation demonstrated in this study, further research is needed to understand how transfer decision-making and processes may contribute to delays in definitive care.
Conclusions
In this population of non-traumatic surgical transfers, duration of referring facility care prior to transfer request did not impact post-transfer mortality or discharge to hospice. This suggests effective triage of high risk patients, and permits time to determine transfer appropriateness for lower risk patients taking into consideration patient needs and available resources. Further work is needed to determine the impact of other transfer process measures on this outcome and to understand whether time to request influences other important outcomes besides death and hospice discharge.
Acknowledgments
Dr. Kummerow Broman is supported by the Office of Academic Affiliations (OAA), Department of Veterans Affairs, VA National Quality Scholars Program and uses facilities at VA Tennessee Valley Healthcare System, Nashville Tennessee. Dr. Vasilevskis was supported by the National Institute on Aging of the National Institutes of Health under Award Number K23AG040157 and the Veterans Affairs Clinical Research Center of Excellence, the Geriatric Research, Education, and Clinical Center (GRECC). The project was also supported by the National Center for Research resources, Grant UL1RR024975-01, and is now at the National Center for Advancing Translational Sciences, Grant 2UL1 TR000445-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs. Neither funder served any role in study design, data collection, analysis, or interpretation, writing of the manuscript, or the decision to submit the article for publication.
Footnotes
Author Contributions: Kummerow Broman – conception and design; acquisition, analysis, and interpretation of data; drafting of the manuscript, critical revision of the manuscript for important intellectual content
Hayes – conception and design; acquisition and interpretation of data; critical revision of the manuscript for important intellectual content
Kripalani – conception and design; interpretation of data; critical revision of the manuscript for important intellectual content
Vasilevskis - conception and design; interpretation of data; critical revision of the manuscript for important intellectual content
Phillips - conception and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content
Ehrenfeld -conception and design; acquisition and interpretation of data; critical revision of the manuscript for important intellectual content
Holzman – conception and design; interpretation of data; critical revision of the manuscript for important intellectual content
Sharp – conception and design; interpretation of data; critical revision of the manuscript for important intellectual content
Pierce - conception and design; interpretation of data; critical revision of the manuscript for important intellectual content
Nealon – conception and design; interpretation of data; critical revision of the manuscript for important intellectual content
Poulose – conception and design; acquisition and interpretation of data; critical revision of the manuscript for important intellectual content
Dr. Kummerow had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author Disclosures: Drs. Kummerow, Hayes, Ehrenfeld, Holzman, Sharp, Kripalani, Pierce, and Nealon, and Mrs. Phillips have no conflicts of interest to disclose. Dr. Poulose received research support from Bard-Davol and is a consultant to Ariste Medical and Pfizer.
References
- 1.Santry HP, Janjua S, Chang Y, et al. Interhospital transfers of acute care surgery patients: should care for nontraumatic surgical emergencies be regionalized? World Journal of Surgery. 2011 Dec;35(12):2660–2667. doi: 10.1007/s00268-011-1292-3. [DOI] [PubMed] [Google Scholar]
- 2.Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Critical Care Medicine. 2012 Aug;40(8):2470–2478. doi: 10.1097/CCM.0b013e318254516f. [DOI] [PubMed] [Google Scholar]
- 3.Rymer MM, Armstrong EP, et al. Analysis of a coordinated stroke center and regional stroke network on access to acute therapy and clinical outcomes. Stroke; a Journal of Cerebral Circulation. 2013 Jan;44(1):132–137. doi: 10.1161/STROKEAHA.112.666578. [DOI] [PubMed] [Google Scholar]
- 4.Gordon HS, Rosenthal GE. Impact of interhospital transfers on outcomes in an academic medical center. Implications for profiling hospital quality. Medical Care. 1996 Apr;34(4):295–309. doi: 10.1097/00005650-199604000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg AL, Hofer TP, Strachan C, et al. Accepting critically ill transfer patients: adverse effect on a referral center's outcome and benchmark measures. Annals of Internal Medicine. 2003 Jun 3;138(11):882–890. doi: 10.7326/0003-4819-138-11-200306030-00009. [DOI] [PubMed] [Google Scholar]
- 6.Durairaj L, Will JG, Torner JC, Doebbeling BN. Prognostic factors for mortality following interhospital transfers to the medical intensive care unit of a tertiary referral center. Critical Care Medicine. 2003 Jul;31(7):1981–1986. doi: 10.1097/01.CCM.0000069730.02769.16. [DOI] [PubMed] [Google Scholar]
- 7.Arthur KR, Kelz RR, Mills AM, et al. Interhospital transfer: an independent risk factor for mortality in the surgical intensive care unit. The American Surgeon. 2013 Sep;79(9):909–913. doi: 10.1177/000313481307900929. [DOI] [PubMed] [Google Scholar]
- 8.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. The New England Journal of Medicine. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 9.Nirula R, Maier R, Moore E, et al. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer's effect on mortality. The Journal of Trauma. 2010 Sep;69(3):595–599. doi: 10.1097/TA.0b013e3181ee6e32. discussion 599-601. [DOI] [PubMed] [Google Scholar]
- 10.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. The Journal of Trauma. 1999 Apr;46(4):565–579. doi: 10.1097/00005373-199904000-00004. discussion 579-581. [DOI] [PubMed] [Google Scholar]
- 11.Wang TY, Nallamothu BK, Krumholz HM, et al. Association of door-in to door-out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA : the Journal of the American Medical Association. 2011 Jun 22;305(24):2540–2547. doi: 10.1001/jama.2011.862. [DOI] [PubMed] [Google Scholar]
- 12.Vora AN, Holmes DN, Rokos I, et al. Fibrinolysis Use Among Patients Requiring Interhospital Transfer for ST-Segment Elevation Myocardial Infarction Care: A Report From the US National Cardiovascular Data Registry. JAMA Internal Medicine. 2014 Dec 8; doi: 10.1001/jamainternmed.2014.6573. [DOI] [PubMed] [Google Scholar]
- 13.van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical Care. 2009 Jun;47(6):626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 14.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Critical Care Medicine. 1985 Oct;13(10):818–829. [PubMed] [Google Scholar]
- 15.Knaus WA, Zimmerman JE, Wagner DP, et al. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Critical Care Medicine. 1981 Aug;9(8):591–597. doi: 10.1097/00003246-198108000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Bayne AP, Madden-Fuentes RJ, Jones EA, et al. Factors associated with delayed treatment of acute testicular torsion-do demographics or interhospital transfer matter? The Journal of Urology. 2010 Oct;184(4 Suppl):1743–1747. doi: 10.1016/j.juro.2010.03.073. [DOI] [PubMed] [Google Scholar]
- 17.Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Critical Care Medicine. 2007 Jun;35(6):1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 18.Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Medical Care. 2011 Jun;49(6):592–598. doi: 10.1097/MLR.0b013e31820fb71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bitterman RA. Transferring and Accepting Patients under EMTALA. In: Aghababian R, editor. Essentials of Emergency Medicine. Third. Burlington, MA: Jones and Bartlett; 2010. [Google Scholar]
- 20.Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. The Journal of Trauma and Acute Care Surgery. 2012 Jun;72(6):1526–1530. doi: 10.1097/TA.0b013e3182542fab. discussion 1530-1521. [DOI] [PubMed] [Google Scholar]
- 21.Service NTI. Change in Public Death Master File Records. [Accessed March 10, 2015];2011 http://www.ntis.gov/assets/pdf/import-change-dmf.pdf. 2015.