Abstract
Arsenic is a naturally occurring toxic element often concentrated in groundwater at levels unsafe for human consumption. Private well water in the United States is mostly unregulated by federal and state drinking water standards. It is the responsibility of the over 13 million U.S. households regularly depending on private wells for their water to ensure it is safe for drinking. There is a consistent graded association with health outcomes at all levels of socioeconomic status (SES) in the U.S. Differential exposure to environmental risk may be contributing to this persistent SES-health gradient. Environmental justice advocates cite overwhelming evidence that income and other SES measures are consistently inversely correlated with exposure to suboptimal environmental conditions including pollutants, toxins, and their impacts. Here we use private well household surveys from two states to investigate the association between SES and risks for arsenic exposure, examining the potentially cumulative effects of residential location, testing and treatment behavior, and psychological factors influencing behavior. We find that the distribution of natural arsenic hazard in the environment is socioeconomically random. There is no evidence that higher SES households are avoiding areas with arsenic or that lower SES groups are disproportionately residing in areas with arsenic. Instead, disparities in exposure arise from differing rates of protective action, primarily testing well water for arsenic, and secondly treating or avoiding contaminated water. We observe these SES disparities in behavior as well as in the psychological factors that are most favorable to these behaviors. Assessment of risk should not be limited to the spatial occurrence of arsenic alone. It is important that social vulnerability factors are incorporated into risk modeling and identifying priority areas for intervention, which should include strategies that specifically target socioeconomically vulnerable groups as well as all the conditions which cause these disparities in testing and treatment behavior.
Keywords: Private well, Arsenic, Drinking water, Socioeconomic status, Disparities, Environmental justice
GRAPHICAL ABSTRACT
1. Introduction
Arsenic (As) is a toxic element naturally occurring in the Earth's crust that can be released into groundwater at unsafe levels for human consumption. Chronic exposure to arsenic is associated with a range of chronic diseases and conditions (Naujokas et al., 2013); of particular concern is in utero and early-life exposure, which even at low concentrations is associated with impaired intellectual development and increased risks of adverse health effects later in life (Farzan et al., 2013; Smith et al., 2012). The U.S. EPA's 2001 Arsenic Rule lowered the federal drinking water standard for arsenic from 50 µg/L to 10 µg/L. Under the Safe Drinking Water Act public water systems and public wells serving at least 25 individuals were given until 2006 to comply with this new Maximum Contaminant Level (MCL) (United States Environmental Protection Agency (USEPA), 2001). The U.S. EPA estimates that by 2011, 5 years after the deadline, nearly 800 water systems serving 1.8 million people were still not in compliance (United States Environmental Protection Agency (USEPA), 2013). These were mostly small rural systems facing financial difficulties. An analysis of community water systems in California's San Joaquin Valley found that higher arsenic levels and higher odds of receiving an MCL violation were most common among systems serving predominantly socioeconomically disadvantaged communities, suggesting that lower socioeconomic status (SES) residents face greater exposure and compliance burdens (Balazs et al., 2012). Similarly in Oregon, community water systems exceeding the arsenic MCL were found to be serving customers with lower income levels (Stone et al., 2007). Although compliance of small community systems is still a challenge, over 13 million mostly rural U.S. households regularly depending on private wells for their drinking water are at risk of arsenic contamination (U.S. Census Bureau, 2015). The relationship between risk for arsenic exposure through well water and SES has not yet been studied.
USGS nationwide non-random sampling has found arsenic exceeding MCL in 10.6% of 7580 wells tested between 1986 and 2001 (Focazio et al., 2006), and 6.8% of 2167 wells tested between 1991 and 2004 (Desimone, 2009). Without a more systematic approach to monitoring the water quality of private wells it is difficult to estimate exactly how many households have arsenic above the MCL in their well water. Private well water in the U.S. is unregulated by federal and state drinking water standards. It is entirely the responsibility of the well owner to ensure that the water is safe to drink. Some state and local governments have taken steps to require well testing during specific occasions such as drilling new wells and real estate sales. For example, New Jersey's 2002 Private Well Testing Act (PWTA) requires wells to be tested during a real estate transaction and tests in the 12 northern counties of the state are required to include arsenic as a parameter. Based on our survey of randomly selected well households in northern New Jersey (NJ) areas affected by arsenic, 75% live in homes purchased before the PWTA came into effect (Flanagan et al., 2016a), and so remain in the same situation as private well owners in Maine and across the country where arsenic testing is not required.
Arsenic in drinking water cannot be seen, smelled, or tasted. Its presence can only be identified through a targeted test. Testing well water for arsenic is essential to identify the hazard so that necessary protective actions to reduce exposure can be taken, such as treating the water or avoiding the source for drinking and cooking. Arsenic is a naturally occurring toxicant; in the absence of outside influences all private well households in a given area, regardless of SES, should face equal risks for arsenic exposure and adverse health effects, but persistent associations between SES, numerous other environmental exposures, and health in the U.S. suggest that the arsenic situation may also be more complex (Evans and Kantrowitz, 2002; Adler and Newman, 2002).
Since private water quality is the responsibility of well owners, reducing risks from arsenic on a population level requires many individuals to take protective action on their own. Factors like perceived vulnerability to and severity of risks, perceived costs and benefits of action, perceived actions of others, and beliefs about self-efficacy and perceptions of control are commonly used to model the adoption of precautionary behavior towards health hazards (Weinstein, 1988; Mosler, 2012). However, the focus on psychological factors influencing behavior may obscure social patterns in the beliefs and behavior of individuals. SES may influence access to information, social, and economic resources and therefore contribute to how risks are perceived and interpreted (Fothergill and Peek, 2004; Vaughan, 1995). In general, the more socioeconomically advantaged individuals are, the better their health; this has generated considerable research interest in recent decades into how social processes might be affecting susceptibility to disease (Marmot, 2000). An individual's social environment of resources and support, experiences that influence psychological development and cognition, and health behavior are among the pathways contributing to this SES-health gradient (Adler et al., 1994). Another contribution to the persistent SES-health gradient may be differential exposure to physical environmental risk resulting from social vulnerability. Environmental justice advocates cite overwhelming evidence that income and other measures of SES are consistently inversely correlated with exposure to suboptimal environmental conditions including pollutants, toxins, noise, crowding, and their impacts. It is this accumulation of negative exposures across multiple dimensions which generates a cumulative vulnerability to adverse health impacts and provides a compelling explanation for the SES health gradient observed in epidemiological studies (Evans and Kantrowitz, 2002; Brulle and Pellow, 2006).
Here we examine private well arsenic exposure from the perspective of cumulative vulnerability. Through a series of household surveys in geographically and demographically different areas of central Maine and northern NJ we have identified significant predictors of well water testing and treatment behavior as well as persistent routes of arsenic exposure (Flanagan et al., 2015a, 2015b; Flanagan et al., 2016a, 2016b). In Maine we found that testing behavior can be significantly predicted in logistic regression by elements of risk knowledge, attitude, action knowledge, and norm beliefs, and observed that testing and mitigation behavior was significantly associated with education level and household income. In this paper we use our growing database of household surveys from both states to investigate the association between SES and risks for arsenic exposure, examining the potentially cumulative effects of residential location, testing and treatment behavior, and the psychological factors influencing behavior. Low SES households already face a cumulative burden of risks from many sources. Here we assess if exposure to naturally occurring arsenic contributes to this burden as well.
2. Methods
2.1. Data sources
2.1.1. Household surveys
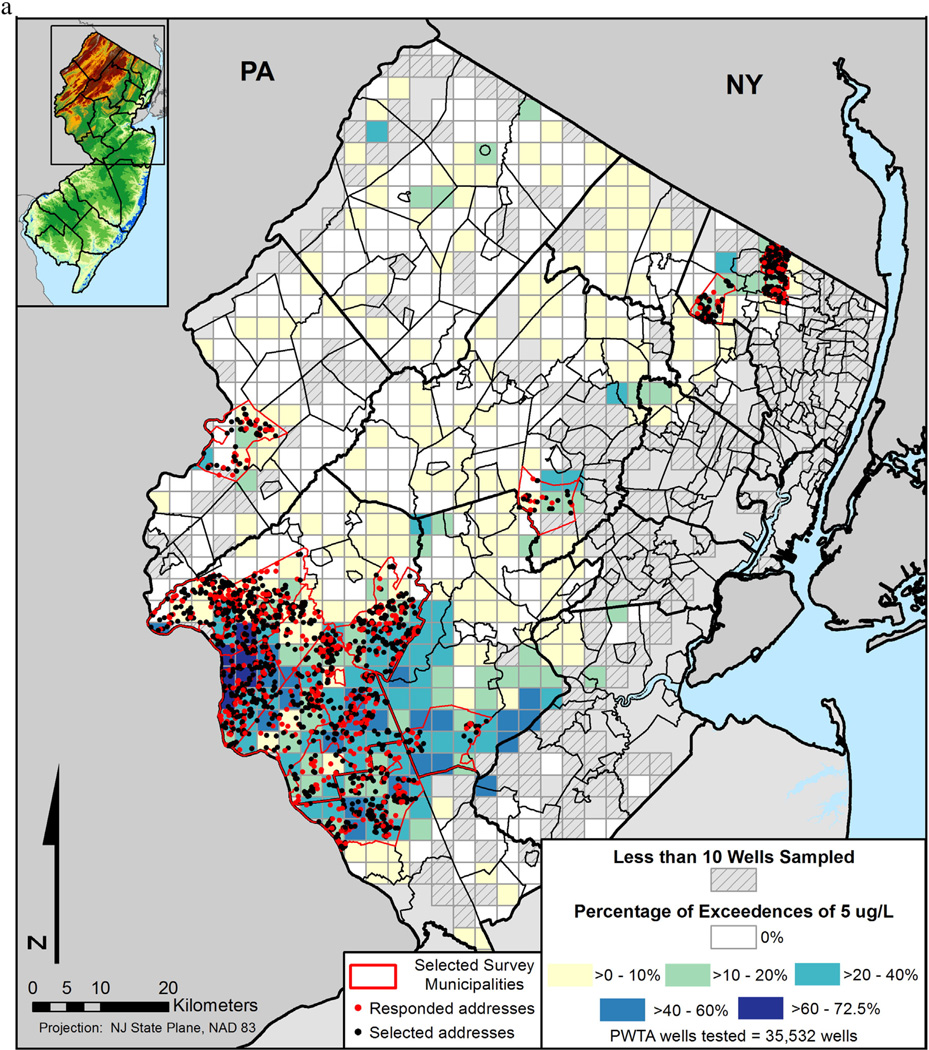
We have implemented two mailed household surveys of randomly selected addresses in arsenic-affected areas with high private well water use: a January 2013 survey of 617 well households in central Maine and a June 2014 survey of 670 well households in northern NJ (Fig. 1a and b). The study areas and survey implementation have been described elsewhere (Flanagan et al., 2015a; Flanagan et al., 2016a). The survey instruments were very similar, asking about water testing and treatment practices and opinions as well as basic demographic information. Household income was reported categorically on the surveys: <$25,000; $25,000–$50,000; >$50,000–$75,000; >$75,000–$100,000; >$100,000–$125,000; >$125,000–$150,000; and >$150,000 in New Jersey; and <$20,000; $20,000–$40,000; >$40,000–$60,000; >$60,000–$80,000; >$80,000–$100,000; and >$100,000 in Maine. Respondent's education was reported on the survey in a variety of categories but was coded as at least a bachelor's degree or less than a bachelor's degree for analyses in this paper. Each survey also included a section with questions designed to measure the risk, attitude, norms, ability, and self-regulation factors that may influence testing and treatment behavior, each phrased as a statement to which respondents indicated their agreement on a scale of 1 to 6 from strongly disagree to strongly agree.
Fig. 1.
a. Location of 2000 New Jersey addresses randomly selected from 17 towns for mailing surveys (all dots). Responses from 670 addresses (red dots) were included in the analyses. Arsenic exceedance rates are presented for 2 × 2 mile areas based on PWTA testing records through March 2014 (colored boxes). Areasnot covered by a box have no wells tested under the PWTA. b. Location of 1346 Maine addresses randomly selected from 15 towns for mailing surveys (all dots). Responses from 617 addresses (red dots) were included in the analyses. Arsenic exceedance rates are presented for 2 × 2 mile areas based on state testing records through 2013 (colored boxes). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
2.1.2. Spatial arsenic occurrence data
The NJ PWTA has resulted in the development of a database of fine-scale geocoded data for over 35,000 unique well tests during real estate transactions since 2002. The Maine Tracking Network brings together arsenic results from 47,000 wells tested by the State of Maine Health and Environmental Testing Laboratory since 1999, although only about 55% are available at fine-scale. Rates of exceedance are reported as percent of wells tested above state MCL for arsenic, 5 µg/L in NJ and 10 µg/L in Maine.
2.1.3. Population income data
Median household income and percent of population in poverty by town in each state were obtained from 2014 American Community Survey estimates (United States Census Bureau, 2015).
2.2. Analyses
Descriptive analysis and correlation and regression analyses were completed using STATA IC v14. All statistical tests were two-tailed and p values < 0.05 were considered significant. Completed surveys with partially missing data were only excluded from analyses requiring those variables of interest. Self-reported respondent's education level and household income are used as measures of SES, although 18% of households in Maine and 30% of households in NJ declined to provide income information thereby reducing the sample sizes for these analyses. Household income was the most commonly missing variable, sample sizes per survey statement in Tables 1–4 were further reduced by up to 5% due to missing responses.
Table 1.
Average marginal effect of household income and respondent education on agreement with survey statements about testing in New Jersey (n = 468).
| Beliefs on testing | Reference groupa agreement rate |
Household income ($50k increase) |
Bachelor's degree |
Significant term in adjusted model |
|---|---|---|---|---|
| Risk | ||||
| Area is at risk for well contamination | 38% | +5.7%* | +13%** | Education |
| Water quality can change over time | 72% | +4.5%** | +9.3%*** | Education |
| We can be exposed to arsenic in well water | 76% | +4%* | +10%*** | Education |
| Years of exposure increase arsenic risks | 83% | +3% | +7.4%** | Education |
| Arsenic-related health effects likely to be serious | 75% | +3% | +6.9%* | Neither |
| Health risks of arsenic exposure not overblown | 67% | +4%* | +9.1%* | Neither |
| Pregnant women and children are especially vulnerable to arsenic effects | 83% | +1.8% | +6.4%* | Education |
| Attitude | ||||
| Well testing helpful to protect my family | 81% | +3.2%** | +6%** | Income |
| Feel safer testing water in a lab | 70% | +4%** | +6.8%* | Income |
| Regularly testing water is not too expensive | 19% | +8.4%*** | +6.5% | Income |
| Norm | ||||
| Know someone with an arsenic problem | 0% | +3.5% | +13.2%*** | Education |
| Feel personally obligated to test water | 52% | +1.5% | +9.1%* | Neither |
| Ability | ||||
| Know who to contact to test well | 42% | +6.9%*** | +5% | Income |
| Confident can manage regularly testing | 65% | +4%* | +7.1%* | Neither |
| Self-regulation | ||||
| Have thought about testing before | 54% | +6.3%*** | +13.8%*** | Both |
| Have thought about testing for arsenic before | 52% | +5.1%* | +10%** | Neither |
| Committed to monitoring water quality | 44% | +5.7%* | +12.7%** | Education |
| Plan to test well in next year | 32% | +5.3%* | +9.7%* | Neither |
Only 18 statements (out of a total of 34) with agreement significantly predicted by income and/or education are shown.
Respondents with household income <$50,000 and less than bachelor's degree education.
p < 0.05.
p < 0.01.
p < 0.001.
Table 4.
Average marginal effect of household income and respondent education on agreement with survey statements about treatment in Maine (n = 504).
| Beliefs on treatment | Reference groupa agreement rate |
Household income ($40k increase) |
Bachelor's degree |
Significant term in adjusted model |
|---|---|---|---|---|
| Attitude | ||||
| Treating water is not too much of a hassle | 51% | +4.7% | +10.7%* | Education |
| Treating water is not too expensive | 31% | +7.8%** | +14.7%*** | Education |
| Ability | ||||
| Know where to go to find information on treatment options | 56% | +10.8%*** | +9.6%* | Income |
| Confident can choose a treatment system | 77% | +6.3%* | −2.9% | Income |
| Know how to find a company to install treatment | 62% | +9.4%** | +3.6% | Income |
| Confident can maintain a treatment system | 57% | +13.2%*** | +12.3%** | Income |
Only 6 statements (out of a total 14) with agreement significantly predicted by income and/or education are shown.
Respondents with household income b$40,000 and less than bachelor's degree education.
p < 0.05.
p < 0.01.
p < 0.001.
2.2.1. Spatial analysis of arsenic hazard
First, Spearman correlation analysis was conducted at the municipal level to test the association between town-level well arsenic exceedance rates and income measures, specifically town median income and percent of population below poverty level. Then arsenic exceedance rates over the MCL within 2 × 2 mile (3.2 × 3.2 km) grid areas were calculated in each state and the addresses of survey participants matched to their respective grid area for a fine-scale spatial analysis. Our surveyed NJ addresses were located within 128 2 × 2 mile areas; however, three were excluded for having less than ten wells sampled from the area. The NJ Department of Environmental Protection (NJDEP) suppresses the PWTA data in grids with less than ten wells tested in an effort to protect the confidentiality of homeowner data. The number of sampled wells per NJ grid ranged from 10 to 400. Surveyed addresses in Maine were located in 146 2 × 2 mile areas; however, 36 were excluded for having less than ten wells sampled from the area. The number of sampled wells per Maine grid ranged from 10 to 69. Spearman correlation tested the association between local arsenic rate and survey-reported household incomes. Kruskal-Wallis tests were performed to detect differences in distribution of reported household income by local arsenic rates (areas grouped into high, medium, and low categories).
2.2.2. Analysis of SES and behavior
Surveyed households in each state were categorized by income -low (<$40,000 in Maine, <$50,000 in NJ), medium ($40,000–80,000 in Maine, $50,000–100,000 in NJ), and high (>$80,000 in Maine, >$100,000 in NJ), and respondent's education - at least a bachelor's degree or less than a bachelor's degree for the charts in Fig. 2. Income was treated as a continuous variable in univariate logistic regressions predicting binary behavior outcomes and to calculate average marginal effects on the likelihood of behavior. Analyses of testing behavior were limited in NJ to respondents with education and income data (n = 344) who purchased their homes prior to the commencement of the PWTA in late 2002 and thus have not faced a state requirement to test their water for arsenic. A well was considered to be “ever tested” if the respondent reported that their water has been tested by a lab at some point for any parameter, not necessarily arsenic. “Any treatment” was considered in use if a well owner reported treating or filtering their water in any way, not necessarily for arsenic.
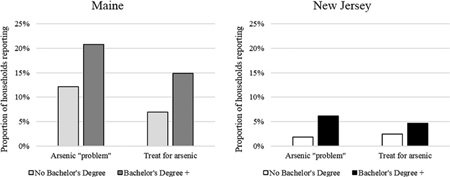
Fig. 2.
Top: Association between town-level arsenic exceedance rate (% >5 µg/L) and median household income (ρ = 0.206, p < 0.05) (left) and population below the poverty line (right) (ρ = −0.222, p < 0.01) for 134 NJ towns with at least 10 wells tested. Below: Association between town-level arsenic exceedance rate (% >10 µg/L) and median household income (ρ = 0.079, p = 0.15) (left) and population below the poverty line (right) (ρ = −0.001, p = 0.99) for 341 Maine towns with at least 20 wells tested. Kendall-Theil robust lines are shown.
2.2.3. Analysis of SES and psychological factors
Responses to the series of survey statements meant to explore the risk beliefs, attitudes, norms, ability beliefs, and self-regulation factors that may influence testing and treatment behavior were dichotomized into either agreeing (strongly, moderately, slightly) or disagreeing. The significance of income (as a continuous variable) and education (binary variable) as predictors of agreement with each statement was first tested by univariate logistic regression to calculate the average marginal effects of each on likelihood of agreement, followed by multivariate regression to identify which predictor remained significant in an adjusted model (Tables 1 through 4).
3. Results
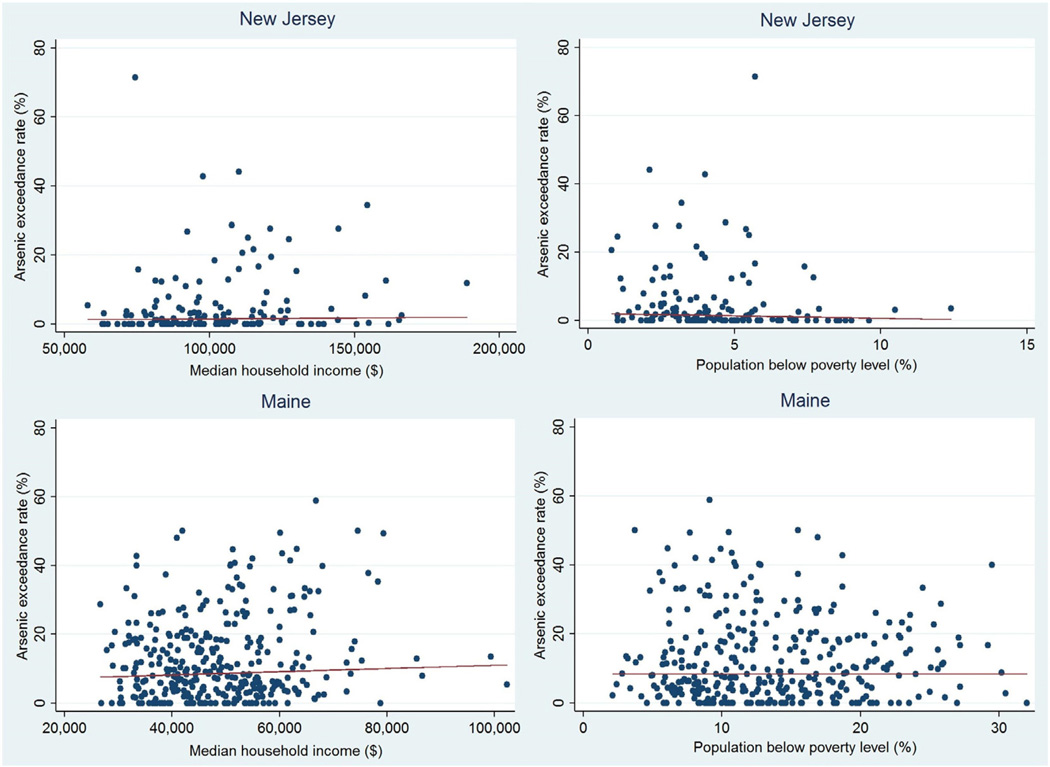
3.1. Distribution of arsenic hazard is socioeconomically random
When arsenic occurrence and median incomes are compared at the administrative level using towns as the unit of spatial analysis, we see a slight positive association (p < 0.05) between household income and arsenic occurrence in NJ only (Fig. 2). When arsenic occurrence and percent of population below poverty level are compared, the association is slightly negative and still significant only in NJ (p < 0.01).
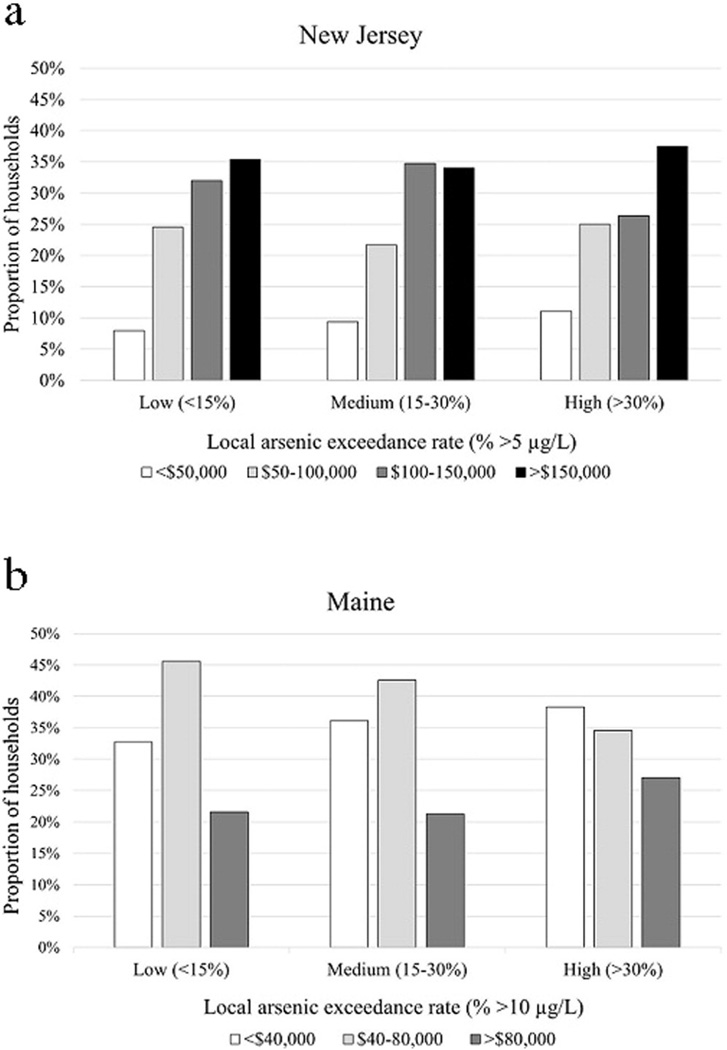
Although survey participants are self-selected and there may be a response bias in favor of higher income households participating (Flanagan et al., 2016a), we find that with geospatial data on arsenic occurrence down to a local 2 × 2 mile area, the household income distribution of respondents in both states is no different whether respondents live in a high, medium, or low arsenic occurrence area based on Kruskal-Wallis tests (NJ p = 0.967, Maine p = 0.694) (Fig. 3a and b). The spearman associations between categorical household income and local arsenic exceedance rates are also not significant (ρ = −0.019, p = 0.685 in NJ; ρ = 0.028, p = 0.575 in Maine). There is similarly no significant association between respondent's education and arsenic occurrence.
Fig. 3.
a. Distribution of NJ survey participants' household income (n = 457) by arsenic exceedance rate in their respective 2 × 2 mile area, low (<15% wells with arsenic >5 µg/L), medium (15–30% wells with arsenic >5 µg/L), and high (>30% wells with arsenic >5 µg/L). Arsenic exceedance is independent of income based on Kruskal-Wallis test, p = 0.967. b. Distribution of Maine survey participants' household income (n = 504) by arsenic exceedance rate in their respective 2 × 2 mile area, low (<15% wells with arsenic >10 µg/L), medium (15–30% wells with arsenic >10 µg/L), and high (>30% wells with arsenic >10 µg/L). Arsenic exceedance is independent of income based on Kruskal-Wallis test, p = 0.690. There is no change to the observed associations when the NJ MCL of 5 µg/L is used to determine exceedance rate.
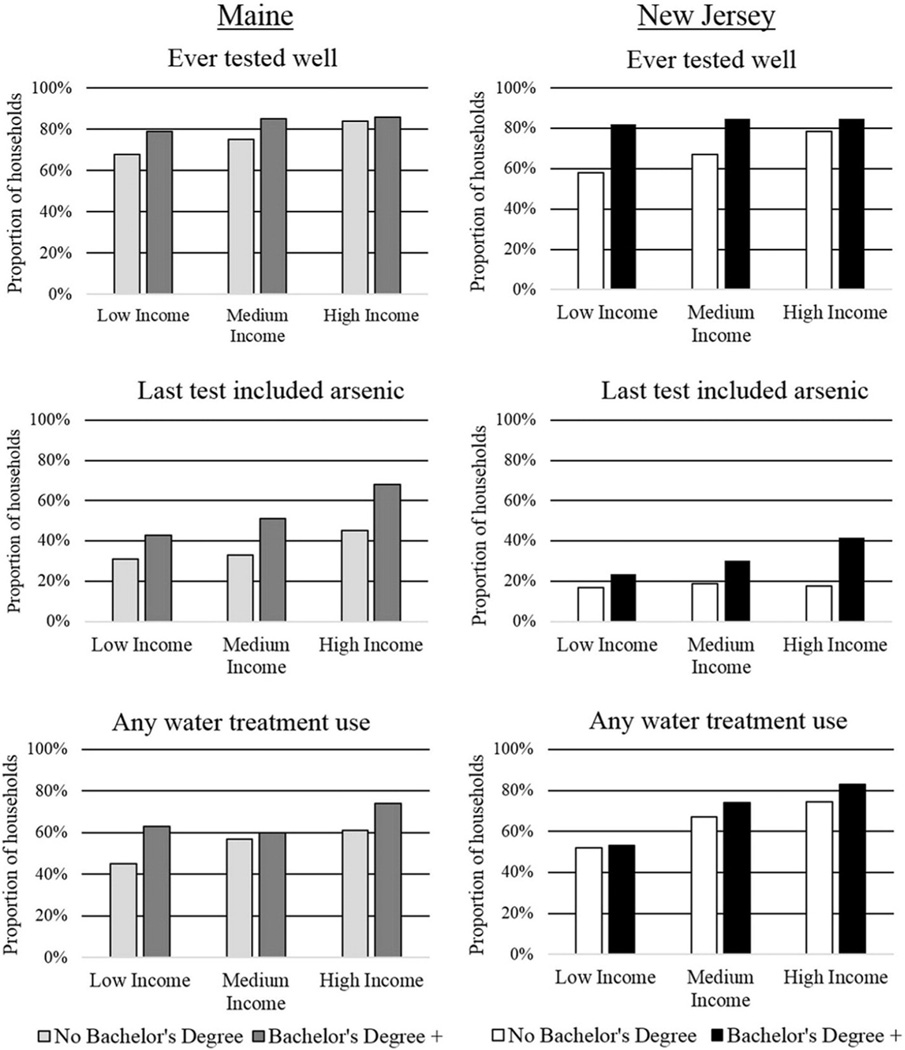
3.2. Socioeconomically vulnerable groups have lower rates of protective behavior
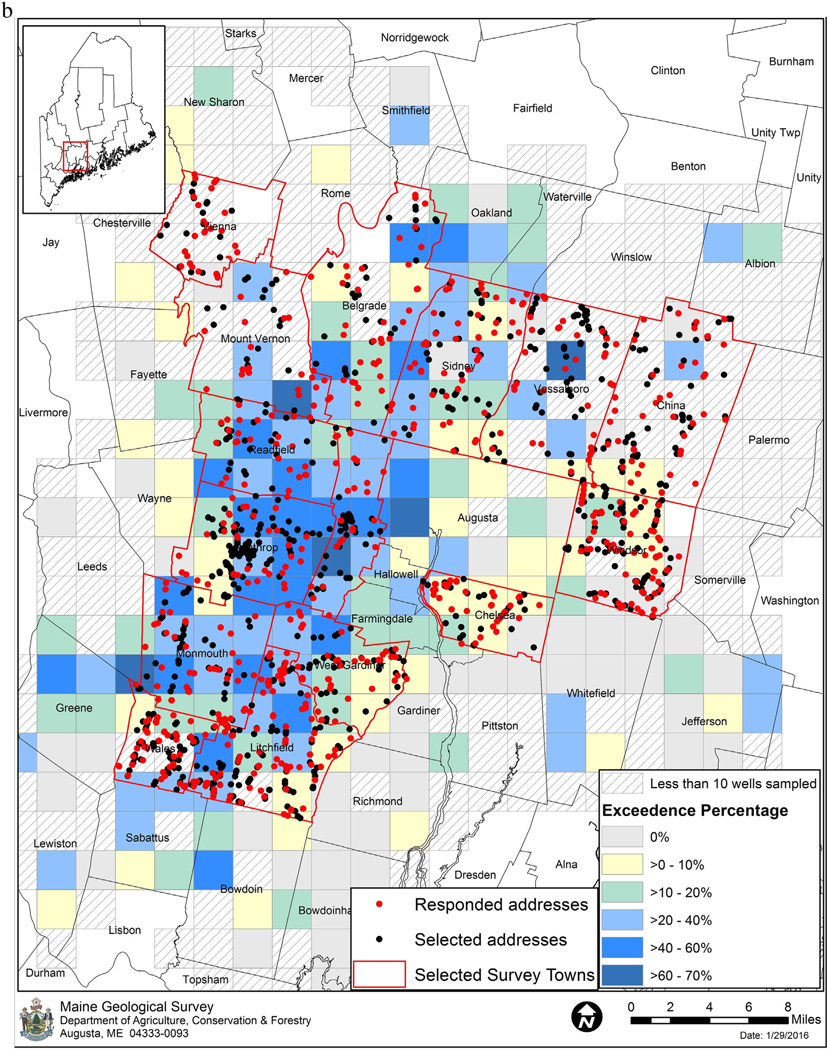
Our NJ survey sample represents a population with higher household income and education than our Maine survey sample (see supplementary information), but we observe the same SES gradient for testing and treatment behavior (Fig. 4). Ever testing a well and testing for arsenic on the last test are both significantly predicted (p < 0.05) by income and education in both states. Although the rate of including arsenic is overall higher in Maine (42%) than in NJ (32%), the influence of income and education on protective behavior is greater in Maine than in NJ; in NJ each increase of $25,000 in household income is associated with an average 4% increase in probability of having tested for arsenic, in Maine each increase of $20,000 in household income is associated with a 7% increase (p < 0.05). Having at least a bachelor's degree in NJ is associated with an average 15% increase in probability of having tested for arsenic, in Maine it is a 23% increase (p < 0.05). Use of any treatment is also significantly predicted by income in both states, while use of a system capable of removing arsenic from the water (Flanagan et al., 2016a) is significantly predicted by both income and education (p < 0.05).
Fig. 4.
Rates of testing and treatment behavior in Maine (left) and NJ (right) by education, Bachelor's degree or higher (Bachelor's Degree+) vs. no Bachelor's degree, and household income level, low (<$40,000 in Maine, <$50,000 in NJ), medium ($40,000–80,000 in Maine, $50,000–100,000 in NJ), and high (>$80,000 in Maine, >$100,000 in NJ). Education and income are significant predictors (p< 0.05) of each behavior in both states based on univariate logistic regression models. Maine n = 504, NJ n = 468. Testing behaviors in NJ were based only on households purchased prior to the start of the PWTA (n = 344). A well was considered to be “ever tested” if the respondent reported that their water has been tested by a lab at some point for any parameter, not necessarily arsenic. “Any treatment” was considered in use if a well owner reported treating or filtering their water in any way, not necessarily for arsenic.
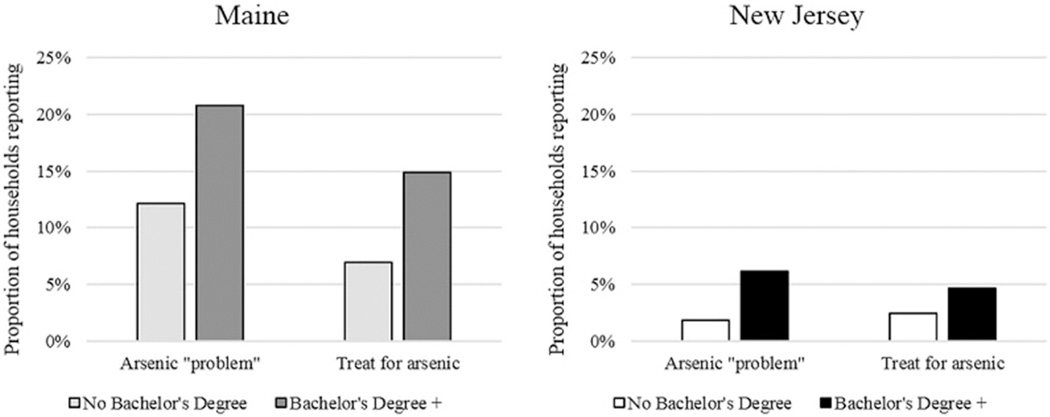
Socioeconomic disparities in testing are reflected in rates of identifying arsenic problems and treating for them (Fig. 5). Although in both NJ and Maine we have found that household income and education are independent of local arsenic occurrence, a well owner with a bachelor's degree in Maine has nearly twice the odds of reporting having an arsenic problem (95% CI = 1.20–3.00) and 2.3 times the odds of treating for arsenic (95% CI = 1.34–4.03) than one with less education. This difference is mostly due to the observed disparities in testing, as without first testing for arsenic a well household cannot be aware of a problem nor treating for it. A Sobel-Goodman test of mediation reveals that 92% of the total effect of education on reporting an arsenic problem in Maine is due to whether arsenic was included on the last well test. In NJ there have been very few arsenic problems identified in wells of homes purchased before the PWTA required tests, but those that have been found were mostly reported by higher educated and income households due to higher rates of testing. Among pre-PWTA households, a well owner with a bachelor's degree has 3.5 times the odds of reporting having an arsenic problem (95% CI = 1.01–11.80) than one with less education. Among post-PWTA households which have all faced the same requirement to test, there is no difference in the rate of reporting an arsenic problem by education.
Fig. 5.
Rates of reported arsenic “problems” (concentration not specified by well owner) and arsenic given as reason for current water treatment by respondent's education, in Maine (left) (n = 589), and NJ (right) (n = 486) for households purchased prior to the start of the PWTA only. Education level is categorized by those without a bachelor's degree and those with a bachelor's degree or higher (Bachelor's Degree +). Approximately 33% of wells in this area of Maine and 21% of wells in this area of NJ are estimated to exceed the state MCL for arsenic.
3.3. Psychological factors influencing testing and treatment behavior patterned by SES
We find that the beliefs and factors that are most favorable to testing and treatment behavior are consistently more prevalent among those with higher income and education (Tables 1–4). Statistical analysis reveals that the observed effects of SES on testing and treatment behavior (Fig. 4) are at least partially mediated by these psychological factors. For example, higher SES households perceive their water to be of worse quality than lower SES households. Income and education are both significantly inversely associated with agreement with the statements “the overall quality of my untreated water is good,” “ I like my untreated well water (e.g. taste, smell, looks),” and “my untreated well water is perfectly safe to drink” (p < 0.05).
The average marginal effects of income and education on likelihood of agreement with survey statements on testing are shown in Table 1 for NJ and Table 2 for Maine. Having thought previously about well testing and arsenic testing are significantly predicted by higher income and education. A well owner with a bachelor's degree in NJ has 2.2 times the odds of having thought about testing (95% CI = 1.50–3.21) and 1.6 times the odds (95% CI = 1.14–2.35) of having thought about arsenic testing specifically than one without a degree, while a well owner with household income over $100,000 has 1.71 (95% CI = 1.11–2.64) and 1.8 times the odds (95% CI = 1.16–2.63), respectively, compared to one with household income below $100,000. In Maine a well owner with a bachelor's degree has 3.4 times the odds of having ever thought about well testing than one without (95% CI = 2.17–5.43). Knowledge of well water as a source of arsenic exposure and that water quality can change over time are also significantly predicted by income and education in both NJ and Maine. Perceptions of arsenic risk severity are stronger among those with a bachelor's degree than without in both states. Even feelings about the usefulness of testing and feelings of safety from tests, although strong overall, are stronger among those with higher income and a college degree. Social factors like knowing someone else with an arsenic problem are significantly more common among those with a bachelor's degree than without. Odds of knowing someone with a problem are 2.5 times higher among those with a bachelor's degree in NJ (95% CI = 1.45–4.26). Confidence in ability to manage regularly testing and knowing who to contact for a well test are both significantly predicted by income; in NJ their likelihoods increase on average by 4% and 7% respectively with each increase of $50,000 in household income, and by 8% and 6% with each increase of $40,000 in Maine (p < 0.05).
Table 2.
Average marginal effect of household income and respondent education on agreement with survey statements about testing in Maine (n = 504).
| Beliefs on testing | Reference groupa agreement rate |
Household income ($40k increase) |
Bachelor's degree |
Significant term in adjusted model |
|---|---|---|---|---|
| Risk | ||||
| Area is at risk for well contamination | 55% | +2.4% | +19.7%*** | Education |
| Water quality can change over time | 74% | +8.8%*** | +7.8%* | Income |
| We can be exposed to arsenic in well water | 82% | +5.1%* | +7.5%* | Neither |
| Years of exposure increase arsenic risks | 90% | +1.1% | +9.3%** | Education |
| Adverse health effects from well water not overblown | 60% | +4.5% | +14.5%*** | Education |
| Health risks of arsenic exposure not overblown | 72% | +2.9% | +12.1%** | Education |
| Our family is at risk for drinking contaminated water | 33% | +6.7%* | +3.1% | Income |
| Attitude | ||||
| Well testing helpful to protect my family | 92% | +4.1%** | +3.9% | Income |
| Concerned despite drinking water a long time with no problem | 45% | +3.8% | +15.5%*** | Education |
| Regularly testing water is not too expensive | 26% | +9.8%*** | +16.1%*** | Both |
| Not concerned a bad test result could hurt property value | 64% | −7.6%* | −9.4%* | Income |
| Norm | ||||
| It is my responsibility to have my water tested | 79% | +4.9%* | +2.2% | Neither |
| Ability | ||||
| Know who to contact to test well | 59% | +5.7%* | +10.2%* | Education |
| Confident can manage regularly testing | 62% | +8.4%** | +7.9% | Income |
| Something can be done about arsenic level in well water | 76% | +7.9%*** | +7.5%* | Income |
| Self-regulation | ||||
| Have thought about testing before | 63% | +6.9%*** | +23.5%* | Education |
Only 16 statements (out of a total of 34) with agreement significantly predicted by income and/or education are shown.
Respondents with household income <$40,000 and less than bachelor's degree education.
p < 0.05.
p < 0.01.
p < 0.001.
Similar to testing, factors that are most favorable to water treatment such as knowing where to go to find information about options, how to find a company to install treatment, and confidence in ability to maintain treatment are more common among well owners with higher income and education (Tables 3 and 4). For example, a well owner in Maine with a bachelor's degree and household income >$80,000 has 7.3 times greater odds of feeling confident about their ability to maintain a treatment system compared to a well owner with less education and income <$40,000 (95% CI = 2.96–18.09).
Table 3.
Average marginal effect of household income and respondent education on agreement with survey statements about treatment in New Jersey (n = 468).
| Beliefs on treatment | Reference groupa agreement rate |
Household income ($50k increase) |
Bachelor's degree |
Significant term in adjusted model |
|---|---|---|---|---|
| Attitude | ||||
| Treating my water is good for my health | 70% | +5.5%*** | +4% | Income |
| Treating well water reduces risk for disease | 74% | +3.4%* | +9.1%* | Education |
| I feel safer drinking treated water | 69% | +5.2%* | +10.2%** | Neither |
| Treating water is not too expensive | 19% | +5.2%* | +11.1%* | Neither |
| Norm | ||||
| I believe some neighbors treat their well water | 35% | +6.4%** | +19.8%*** | Education |
| Neighbors would expect me to treat if my water did not meet safety standards | 55% | +2.1% | +11.6%** | Education |
| If my well did not meet water standards I would feel a personal obligation to treat | 85% | +2.9%** | +5.8%** | Income |
| Ability | ||||
| Know where to go to find information on treatment options | 44% | +5.7%** | +4.6% | Income |
| Confident can choose a treatment system | 58% | +1.9% | +6.7%* | Neither |
| Know how to find a company to install treatment | 54% | +5.0%** | +8.8%* | Neither |
| Confident can maintain a treatment system | 65% | +6.1%*** | +8.3%** | Income |
Only 11 statements (out of a total 14) with agreement significantly predicted by income and/or education are shown.
Respondents with household income <$50,000 and less than bachelor's degree education.
p < 0.05.
p < 0.01.
p < 0.001.
4. Discussion
4.1. Cumulative risks for arsenic exposure: natural hazard, social and psychological vulnerability
Here we examined survey and arsenic occurrence data to investigate whether lower SES households are at greater risk of arsenic exposure from private well water. We found that while risk for arsenic contamination of wells is generally independent of socioeconomic measures, disparities in arsenic exposure likely result from differing rates of protective action and differences in beliefs about these actions. Exposure to arsenic can only be avoided through first testing the well to identify the hazard, secondly avoiding the water or treating the water to remove the arsenic, and third ongoing maintenance and monitoring of the treatment system to ensure continued drinking water quality. At each of these action steps there is the potential for disadvantaged groups to fall behind, ultimately resulting in disparities in arsenic exposure and health impact.
4.2. Naturally-occurring arsenic risk independent of SES
In most cases the disparate burden of environmental risk borne by lower SES households begins with greater likelihood of residential location in proximity to hazards (Evans and Kantrowitz, 2002). However, using town level data we find no association between arsenic occurrence and median income or poverty rate in Maine, and only a slight positive association between arsenic occurrence and median income and negative association between arsenic occurrence and poverty rate in NJ (Fig. 2). This suggests that higher income households are not disproportionately avoiding arsenic hazards and that poor households are not disproportionately residing in areas of high arsenic hazard. Using available fine-scale geocoded well testing data we find again that there is no association between local rates of arsenic occurrence and the household incomes or education of surveyed residents in either state, suggesting that at the local level the SES of residents is independent of arsenic occurrence and lending further support to the idea that geographical proximity to the natural arsenic hazard is not dictated by socioeconomic advantage. In this sense well water arsenic is unlike environmental exposures from hazardous waste sites, air pollution, and housing quality where higher SES families may have the knowledge, resources, and support to avoid negative environmental conditions. Naturally-occurring arsenic contamination of groundwater is not a widely known hazard, arsenic contamination of wells at the local level appears to be spatially random due to the underlying geology, and personal exposure cannot be determined except through a well water test. Furthermore, testing may not have been the normin affected areas until recent years, if at all. As more wells are tested and maps of high arsenic regions become available, it is possible that this situation will change. The initial finding of arsenic in two towns of Mainein 1993 and the consequent media attention led to significant decreases in property prices, but only temporarily over a two year period, much shorter than the price effect observed for Superfund sites (Boyle et al., 2010). It was unclear whether the short duration of depressed prices reflected arsenic contamination being a treatable problem or that perceived risks changed without continued media coverage.
4.3. Arsenic exposure results from inaction
Since arsenic is naturally occurring and appears to be spatially random and independent of SES at the local level, exposure to this toxic element can only be avoided through protective behaviors, primarily testing well water for arsenic, and secondly treating or consistently avoiding contaminated water. We find that well testing and arsenic testing are both significantly associated with household income and education in Maine and NJ (Fig. 4). We have observed that as testing rates increase with community engagement and raised awareness, SES disparities in testing may grow (Flanagan et al. 2016b, in press). In Maine the rate of including arsenic on a well test is overall higher (42%) than among pre-PWTA NJ wells (32%) but the associations of testing with income and education are stronger in Maine.
The state-wide Maine Behavior Risk Factor Surveillance System (BRFSS) includes a survey question on whether or not private wells have been tested for arsenic. The 2012 data (unpublished) shows significant relationships between education, income, and arsenic testing (p < 0.001) that support the SES trends we have observed in our more local survey area, also allowing for comparisons at lower ranges of income and education. While 50% of 4-year college graduates report a well tested for arsenic, only 16% of those with less than a high school education have. Households with incomes ≥$50,000 have an arsenic testing rate of 56%, while households earning less than $15,000 have a testing rate of 33%. Interestingly this rate is slightly higher than the 28% testing rate of households in Maine earning $15,000–$35,000, which may reflect a state policy to pay for free water tests for the indigent. Such policies to support low-income households with private wells could help to counteract strong SES-disparities in testing behavior if residents are made aware and actively encouraged to take advantage of them. Additionally, requiring arsenic testing for everyone at a certain time point, such as during real estate transaction, can help prevent these disparities from arising in new households (Flanagan et al. 2016b, in press).
Testing disparities in turn contribute to disparities in treatment use. In NJ we find that 81% of household with incomes >$100,000 treat their well water in some way, while only 52% of respondents with household incomes <$50,000 do (Fig. 4). If considering only treatment methods that are capable of removing arsenic from the water, then the rates of use are 17% and 9%, respectively. A recent study of private well owners in Arizona similarly found that household income and education were significant predictors of water treatment (Lothrop et al., 2015). For arsenic specifically we have previously found that while taking any mitigation action was not associated with SES, choice of mitigation action is significantly associated with income and education. Higher income and educated households are more likely to install arsenic removal treatment, while lower income and less educated households are more likely to switch to drinking bottled water to avoid arsenic exposure (Flanagan et al., 2015b). This is likely because the upfront costs of installation (average $700–2740) (Spayd, 2007) can be prohibitive for lower income households, yet for a household of more than one person treating water is more cost effective in the long run than purchasing bottled water (Sargent-Michaud et al., 2006). However, mitigation choices cannot be made without first testing and identifying the arsenic problem. When higher SES households are more likely to test their wells, they are also more likely to be aware of an arsenic problem and therefore take action to avoid it as we have seen in our surveys (Fig. 5). Disparities in arsenic testing mean that lower SES families are more likely to be unaware of and unprotected from the arsenic hazard in their well water.
4.4. SES differences in behavior-influencing psychological factors
These effects of SES on testing are at least partially mediated by psychological factors that can favor or hinder the protective behavior. Previously we have found that testing behavior can be significantly predicted by elements of risk knowledge, attitude, action knowledge, and norm beliefs (Flanagan et al., 2015a). Here we find that these psychological factors are also significantly associated with education level and household income. Higher-income well owners perceive their untreated water to be of worse quality and less safe than lower-income well owners. They are also more likely to have thought about testing before, express greater awareness of the risks for water contamination in their area, and are more knowledgeable about well water as a potential route for arsenic exposure. Income is associated with greater appreciation for testing as a means to protect the health of one's family and stronger feelings of safety from having water tested. Social norms like knowing others who have tested and found arsenic problems are stronger among higher educated households. Higher-income well owners are more likely to know who to contact for well testing and be confident in their ability to manage regularly testing and monitoring of water quality. Although the majority of private well households in both states believe that regularly testing well water is too expensive, there is a clear gradient in this belief by household income. Through our own direct mail testing intervention in NJ we found that even when providing well owners who have never tested for arsenic a clear and convenient opportunity to test, a $40 charge can reduce testing participation rates by over 70% (Flanagan et al. 2016b, in press).
Income is also associated with the psychological factors most favorable to treatment behavior, such as knowing where to find information on treatment options or a company to install a system, and confidence in one's ability to maintain a treatment system. Feeling confident about being able to maintain treatment was a significant predictor of choosing treatment as a mitigation strategy among households faced with arsenic problems in Maine (Flanagan et al., 2015b). Concerns about the expense of treatment are also more common among the low SES households studied here.
4.5. Implications
In the absence of private well policies that require water testing and treatment, it is important that public outreach efforts to motivate these protective behaviors take into account existing socioeconomic disparities and attempt to address the conditions which contribute to them. This will be an ongoing challenge; we have found that community testing promotion can actually exacerbate SES disparities if higher SES households are more likely to respond to risk messaging or take advantage of program testing opportunities (Flanagan et al. 2016b, in press).
Differential exposure to environmental risk and an accumulation of negative exposures across multiple dimensions are contributing to a persistent SES-health gradient (Evans and Kantrowitz, 2002; Brulle and Pellow, 2006). Income and other measures of SES are consistently inversely correlated with exposure to adverse environmental conditions. Here we find that arsenic exposure through drinking water may fit the same pattern, although primarily due to differences in behavior rather than proximity to the natural hazard. This finding is important with regards to cumulative vulnerability to adverse health outcomes. Growing epidemiologic evidence suggests that psychological stressors from the social environment such as poverty, discrimination, and crime, can alter susceptibility to exposures in the physical environment such as air pollution (Clougherty and Kubzansky, 2009). Chronic activation of the stress system is believed to lead to increased allostatic load, the physiological burden or “wear and tear” imposed by stress on the body (McEwen, 1998) that can cause illness by weakening its ability to defend against external challenges (Gee and Payne-Sturges, 2004), by enhancing general susceptibility, and by enhancing responsivity to environmental toxicants (Clougherty and Kubzansky, 2009). Through this pathway environmental hazard exposures and chronic social stressors may interact as a form of “double jeopardy” that shapes persistent economic disparities in health (Morello-Frosch and Shenassa, 2006). Yet risk assessment tends to focus on protection from single risks at a time, mostly chemical exposure, without consideration for special vulnerability in cumulative risk situations (Morello-Frosch et al., 2011).
For this reason the inclusion of psychologic and social factors as an integral component of cumulative risk assessment and environmental policy has been advocated (DeFur et al., 2007; Morello-Frosch et al., 2011; Sexton and Linder, 2010). We believe it is important to consider private well arsenic exposure in a cumulative risk context as well; it is just one of a range of physical and social environmental stressors that can accumulate for disadvantaged populations, leaving them especially vulnerable to adverse health effects. Here, as with other environmental hazards, we find the risks for arsenic exposure are patterned by social and psychological vulnerabilities. This finding is consistent across two geographically and demographically different private well communities. It is important that cumulative risk assessments and well water policy take into account the social and psychological factors that make certain groups more at risk of arsenic exposure and more vulnerable to the health impacts from that exposure.
4.6. Limitations
We are limited by our survey sample size and coverage of only two arsenic-affected areas in the northeastern United States. Although our findings are consistent in these two different populations, they may not be generalizable to other regions or countries. Second, testing and treatment behavior were all self-reported in surveys and so subject to recall bias. Furthermore, a sizeable number of surveyed households declined to provide income information which further limited our sample sizes for analyses of association with SES, and the selective non-response may have introduced bias into our findings. However, there were no significant differences in the reported rates of testing and treatment behaviors between households who reported income information and those who were excluded from these analyses for not providing income.
5. Conclusion
Research finds the probability of arsenic occurrence at regional and local scale is governed by a set of hydrogeochemical factors and can increasingly be predicted by geostatistical modeling (Ayotte et al., 2006; Yang et al., 2012). As more private wells are tested across the country contributing to databases like those of the NJ PWTA and the Maine Tracking Network, there is potential to continuously fine-tune modeling to help target private well populations at higher risk of exposure to elevated geogenic arsenic. Yet any assessment of risk should not be limited to the spatial occurrence of arsenic alone. Socially vulnerable groups already face increased health risks through multiple pathways linking SES, psychosocial stress, and environmental exposures to health outcomes, leaving them potentially more susceptible to the adverse effects of chronic arsenic exposure. Since our findings suggest likely SES disparities in arsenic exposure resulting from disparities in protective actions taken and the psychological factors favoring them, it is important that these vulnerability factors are incorporated into risk modeling and identifying priority areas for intervention. Efforts to reduce arsenic exposure in the private well population would benefit from strategies that specifically target socioeconomically vulnerable groups, not because they are currently more likely to have arsenic contaminated well water, but because when they do they exposure is often not discovered or mitigated.
Supplementary Material
HIGHLIGHTS.
Unequal exposure to environmental risk contributes to the SES-health gradient.
We examine survey data for associations between SES and arsenic exposure risk.
Environmental distribution of the arsenic hazard is socioeconomically random.
SES exposure disparities arise from differing rates of arsenic testing/treatment.
Social vulnerability factors should be incorporated into arsenic risk modeling.
Acknowledgments
This research was supported by the U.S. National Institute of Environmental Health Sciences (NIEHS) Superfund Research Program 3 P42 ES10349 and NIEHS grant P30 ES009089. Funding for this study was provided in part through the NJ Department of Health (NJDOH) and the NJ Department of Environmental Protection (NJDEP) Environmental Pubic Health Tracking (EPHT) Cooperative Agreement Number 5U38EH000948-05 from the Centers for Disease Control and Prevention. This report's contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention, NJDOH or NJDEP. We also thank Judy Louis of NJDEP for assistance during survey planning and other NJDEP staff and interns for assistance with survey implementation. This is LDEO contribution 7990.
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.scitotenv.2016.03.217.
References
- Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff. (Millwood) 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health. The challenge of the gradient. Am. Psychol. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Ayotte JD, Nolan BT, Nuckols JR, et al. Modeling the probability of arsenic in groundwater in New England as a tool for exposure assessment. Environ. Sci. Technol. 2006;40(11):3578–3585. doi: 10.1021/es051972f. [DOI] [PubMed] [Google Scholar]
- Balazs CL, Morello-Frosch R, Hubbard AE, Ray I. Environmental justice implications of arsenic contamination in California's San Joaquin Valley: a cross-sectional, cluster-design examining exposure and compliance in community drinking water systems. Environ. Health. 2012;11:84. doi: 10.1186/1476-069X-11-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle KJ, Kuminoff NV, Zhang CW, Devanney M, Bell KP. Does a property-specific environmental health risk create a “neighborhood” housing price stigma? Arsenic in private well water. Water Resour. Res. 2010;46 [Google Scholar]
- Brulle RJ, Pellow DN. Environmental justice: human health and environmental inequalities. Annu. Rev. Public Health. 2006;27:103–124. doi: 10.1146/annurev.publhealth.27.021405.102124. [DOI] [PubMed] [Google Scholar]
- Clougherty J, Kubzansky L. A framework for examining social stress and susceptibility to air pollution in respiratory health. Environ. Health Perspect. 2009;117:1351–1358. doi: 10.1289/ehp.0900612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFur PL, Evans GW, Cohen Hubal EA, Kyle AD, Morello-Frosch RA, Williams DR. Vulnerability as a function of individual and group resources in cumulative risk assessment. Environ. Health Perspect. 2007;115(5):817–824. doi: 10.1289/ehp.9332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desimone LA. National Water-Quality Assessment Program (U.S.). Quality of Water From Domestic Wells in Principal Aquifers of the United States, 1991–2004. Reston, Va: U.S. Dept of the Interior, U.S. Geological Survey; 2009. [Google Scholar]
- Evans G, Kantrowitz E. Socioeconomic status and health: the potential role of environmental risk exposure. Annu. Rev. Public Health. 2002;23:303–331. doi: 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- Farzan SF, Karagas MR, Chen Y. In utero and early life arsenic exposure in relation to long-term health and disease. Toxicol. Appl. Pharmacol. 2013;272(2):384–390. doi: 10.1016/j.taap.2013.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan S, Marvinney R, Zheng Y. Influences on domestic well water testing behavior in a Central Maine area with frequent groundwater arsenic occurrence. Sci. Total Environ. 2015a;505:1274–1281. doi: 10.1016/j.scitotenv.2014.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan S, Marvinney R, Johnston R, Yang Q, Zheng Y. Dissemination of well water arsenic results to homeowners in Central Maine: influences on mitigation behavior and continued risks for exposure. Sci. Total Environ. 2015b;505:1282–1290. doi: 10.1016/j.scitotenv.2014.03.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan S, Spayd S, Procopio N, Chillrud S, Braman S, Zheng Y. Arsenic in private well water part 1 of 3: impact of the New Jersey Private Well Testing Act on household testing and mitigation behaviors. Science of the Total Environment. 2016a doi: 10.1016/j.scitotenv.2016.03.196. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan S, Spayd S, Procopio N, et al. Arsenic in private well water part 2 of 3: who benefits most from traditional testing promotion? Science of the Total Environment. 2016b doi: 10.1016/j.scitotenv.2016.03.199. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Focazio MJ, Tipton D, Dunkle Shapiro S, Geiger LH. The chemical quality of self-supplied domestic well water in the United States. Groundw. Monit Remediat. 2006;26(3):92–104. [Google Scholar]
- Fothergill A, Peek L. Poverty and disasters in the United States: a review of recent sociological findings. Nat Hazards. 2004;32:89–110. [Google Scholar]
- Gee G, Payne-Sturges D. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ. Health Perspect. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lothrop N, Wilkinson ST, Verhougstraete M, et al. Home water treatment habits and effectiveness in a rural Arizona community. Water. 2015;7(3):1217–1231. doi: 10.3390/w7031217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. Multilevel approaches to understanding social determinants. In: Berkman L, editor. Social Epidemiology. New York: Oxford University Press; 2000. [Google Scholar]
- McEwen B. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa E. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ. Health Perspect. 2006;114:1150–1153. doi: 10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff. 2011;30(5):879–887. doi: 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- Mosler HJ. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: a conceptual model, a review, and a guideline. Int J. Environ. Health Res. 2012;22(5):431–449. doi: 10.1080/09603123.2011.650156. [DOI] [PubMed] [Google Scholar]
- Naujokas MF, Anderson B, Ahsan H, et al. The broad scope of health effects from chronic arsenic exposure: update on a worldwide public health problem. Environ. Health Perspect. 2013;121(3):295–302. doi: 10.1289/ehp.1205875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent-Michaud J, Boyle K, Smith A. Cost effective arsenic reductions in private well water in Maine. J. Am. Water Resour. Assoc. 2006;42(5):1237–1245. [Google Scholar]
- Sexton K, Linder SH. The role of cumulative risk assessment in decisions about environmental justice. Int. J. Environ. Res. Public Health. 2010;7(11):4037–4049. doi: 10.3390/ijerph7114037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A, Marshall G, Liaw J, Yuan Y, Ferreccio C, Steinmaus C. Mortality in young adults following in utero and childhood exposure to arsenic in drinking water. Environ. Health Perspect. 2012;120(11):1527–1531. doi: 10.1289/ehp.1104867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spayd S. Arsenic Water Treatment for Residential Wells in New Jersey. Trenton, NJ: State of New Jersey Department of Environmental Protection, New Jersey Geological Survey; 2007. http://www.nj.gov/dep/pwta/Arsenic_Treatment.pdf. [Google Scholar]
- Stone D, Sherman J, Hofeld E. Arsenic in Oregon community water systems: demography matters. Sci. Total Environ. 2007;382(1):52–58. doi: 10.1016/j.scitotenv.2007.04.020. [DOI] [PubMed] [Google Scholar]
- United States Environmental Protection Agency (USEPA) [Accessed June, 2013];National primary drinking water regulations: arsenic and clarifications to compliance and new source contaminants monitoring. 2001 http://www.epa.gov/fedrgstr/EPA-WATER/2001/January/Day-22/w1668.htm.
- United States Environmental Protection Agency (USEPA) [Accessed June 2013];Fiscal year 2011: drinking water and ground water statistics. Office of Water (4606M) EPA 816-R-13-003. 2013 http://water.epa.gov/scitech/datait/databases/drink/sdwisfed/upload/epa816r13003.pdf.
- United States Census Bureau. 2010–2014 american community survey. U.S. Census Bureau's American Community Survey Office; 2015. http://factfinder2.census.gov. [Google Scholar]
- U.S. Census Bureau. 2013 Housing Profile: United States AHS/13–1. Washington, D.C.: 2015. [Google Scholar]
- Vaughan E. The significance of socioeconomic and ethnic diversity for the risk communication process. Risk Anal. 1995;15(2):169–180. [Google Scholar]
- Weinstein ND. The precaution adoption process. Health Psychol. 1988;7(4):355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- Yang Q, Jung HB, Marvinney RG, Culbertson CW, Zheng Y. Can arsenic occurrence rates in bedrock aquifers be predicted? Environ. Sci. Technol. 2012;46(4):2080–2087. doi: 10.1021/es203793x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.