Abstract
Introduction Friedreich's ataxia is a neurodegenerative disease and progressive by nature. It has autosomal recessive inheritance and early onset in most cases. Nystagmus and hearing loss (in some cases) make up some of the common symptoms seen in this disorder.
Objective The objective of this study is to examine vestibular disorders in patients with Friedreich ataxia.
Methods We conducted a retrospective cross-sectional study. We evaluated 30 patients with ages ranging from six to 72 years (mean age of 38.6 ( ± 14.7). The patients underwent the following procedures: anamnesis, ENT, and vestibular evaluations.
Results Clinically, the patients commonly had symptoms of incoordination of movement (66.7%), gait disturbances (56.7%), and dizziness (50%). In vestibular testing, alterations were predominantly evident under caloric testing (73.4%), gaze nystagmus testing (50.1%), rotational chair testing (36.7%), and optokinetic nystagmus testing (33.4%). The presence of alterations occurred under examination in 90% of subjects, with the majority occurring in those with central vestibular dysfunction (70% of the examinations).
Conclusion The most evident neurotological symptoms were incoordination of movement, gait disturbances, and dizziness. Alterations in vestibular examinations occurred in 90% of patients, mostly in the caloric test, with a predominance of deficient central vestibular system dysfunction.
Keywords: spinocerebellar ataxias, ataxia, spinocerebellar degenerations
Introduction
Hereditary ataxias account for ∼10% of genetic diseases that affect the nervous system. Currently, more than 20 different types of autosomal recessive ataxias are mapped and classified according to their etiology.1 In this group of diseases, some are very rare and observed only in isolated populations, while others are found worldwide.2 Among them, is Friedreich's ataxia (FA), described initially by Nicholaus Friedreich in 1863, but only becoming well-known around 1882. It is a neurodegenerative disease, progressive in nature, autosomal recessive, and early onset in most cases.2 3 4
The first symptoms are usually observed in childhood or the early teens; however, in some cases, the diagnosis is made before the age of two years or after the age of twenty. The main features of the disease are: ataxia (impaired coordination) that initially affects the lower limbs and then the upper limbs, absence of tendon reflexes and weakness in the lower limbs, dysarthria, loss of distal deep sensitivity, and bilateral Babinski sign. Nerve conduction studies show axonal sensory neuropathy.5 6 7 Other main problems associated to the condition are: nystagmus, optic atrophy, hearing loss (which may be present), atrophy in hands and distal lower limbs, scoliosis, pes cavus, and claw toes.2 3 4 5 6 7 Diabetes is present in 10% of cases and cardiomyopathy occurs in approximately two-thirds of patients, making the latter the leading cause of death.7 8 9 There are significant variations in the average duration of the disease, from the onset of symptoms until death, which tends to occur around the fourth decade of life.5 6 8 10
The diagnosis of FA is performed by means of clinical and genetic data.
Spinocerebellar ataxias (SCAs) are part of a list of diseases that, by their manifestations and impairment areas, can lead to vestibular disorders. The vestibular evaluation is an important tool in confirmation of vestibular disorders and their relationship with the central nervous system. The tests that comprise the vestibular examination make it possible to assess balance and its relationship to the function of the posterior labyrinth, vestibular branches of cranial nerve VIII, vestibular nuclei at the floor of the fourth ventricle, vestibular pathways and, above all, vestibular-oculomotor, vestibulocerebellar, vestibulospinal, and vestibular and neck proprioceptive relationships.11
The aim of this study was to investigate the vestibular disorders in patients with Friedreich's ataxia.
Materials and Methods
This study was approved by the Institutional Ethics Committee under registration number 058/2008 and authorized by the patients' signing of a consent form.
A retrospective cross-sectional study was conducted. We evaluated 30 patients (10 female and 20 male) directed by the Department of Internal Medicine at the Hospital de Clinicas for evaluation by the Otoneurology Department of an educational institution in the same city, with a diagnosis of Friedreich's-type recessive SCA (FA). The diagnosis of ataxia was performed by means of genetic testing using Polymerase Chain Reaction (PCR) (Table 1).12 13 14 To measure the severity of cerebellar ataxia in an easier and more practical manner, Schmitz-Hübsch et al15 proposed a scale for the assessment and rating of ataxia (SARA) which was translated and validated in Brazilian Portuguese by Braga-Neto el al.16 The SARA has eight questions that yield a total score of 0 (no ataxia) to 40 (most severe ataxia); 1: gait (score 0 to 8), 2: stance (score 0 to 6), 3: sitting (score 0 to 4), 4: speech disturbance (score 0 to 6), 5: finger-chase test (score 0 to 4), 6: nose-finger test (score 0 to 4), 7: fast alternating hand movements (score 0 to 4), 8: heel-shin coordination test (score 0 to 4). Kinetic limb functions (items 5 to 8) are rated independently for both sides, and the arithmetic mean of both sides is included in the SARA total score.15 This scale has proven to be a valid and trustworthy measurement in SCA patients.
Table 1. Aspects of Friedreich's ataxia.
| CASE | AGE (years) | SEX | DISEASE DURATION (years) | SARA |
|---|---|---|---|---|
| 1 | 43 | M | 25 | 20 |
| 2 | 41 | M | 7 | 3,5 |
| 3 | 30 | F | 18 | 8 |
| 4 | 24 | M | 8 | 4 |
| 5 | 29 | M | 13 | 14 |
| 6 | 17 | M | 3 | 13 |
| 7 | 63 | F | 38 | 7 |
| 8 | 6 | F | 6 | 19 |
| 9 | 37 | F | 19 | 16 |
| 10 | 41 | F | 20 | 29,5 |
| 11 | 27 | F | 12 | 14 |
| 12 | 25 | F | 12 | 12 |
| 13 | 55 | F | 30 | 7 |
| 14 | 44 | M | 10 | 3,5 |
| 15 | 55 | M | 12 | 14 |
| 16 | 37 | M | 17 | 19 |
| 17 | 51 | M | 30 | 29 |
| 18 | 27 | M | 10 | 16 |
| 19 | 46 | M | 18 | 10 |
| 20 | 72 | M | 42 | 28 |
| 21 | 52 | F | 18 | 3 |
| 22 | 30 | M | 4 | 4,5 |
| 23 | 37 | M | 19 | 18 |
| 24 | 44 | M | 18 | 9,5 |
| 25 | 22 | M | 14 | 5 |
| 26 | 42 | F | 31 | 25 |
| 27 | 63 | M | 18 | 19 |
| 28 | 42 | M | 21 | 8 |
| 29 | 28 | M | 21 | 8 |
| 30 | 30 | M | 17 | 13 |
Abbreviations: F, female; M, male; SARA, scale for the assessment and rating of ataxia.
Excluded from the study were patients that presented with otological alterations or other abnormalities that prevented the completion of testing.
The following procedures were performed:
Anamnesis
A questionnaire was given focusing on otoneurological signs and symptoms (Fig. 1).
Fig. 1.
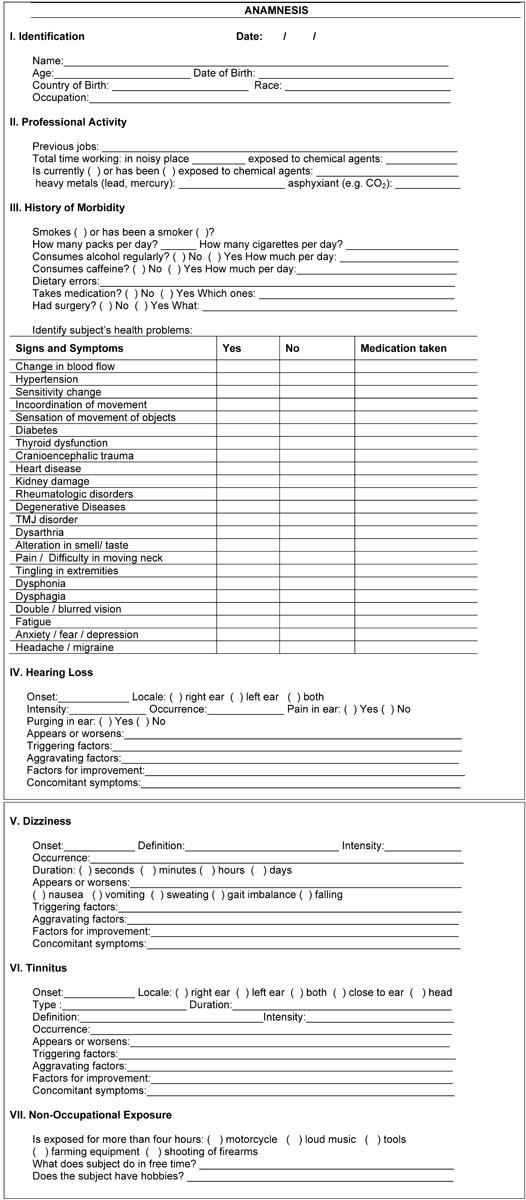
Anamnesis by Otoneurology Department.
Ear, Nose, and Throat (ENT) Evaluation
An ENT evaluation was performed to rule out any alterations that could affect the test.
Vestibular Assessment
Patients underwent the following tests that make up the vestibular examination. Initially, we checked vertigo and spontaneous and semi-spontaneous positional nystagmus.
Then, to analyze vectoelectronystagmography (VENG), we used a three-channel thermosensitive Berger VN316 model device along with a Ferrante swivel chair, a Neurograff Eletromedicina Ltda. model EV VEC visual stimulator, and a Neurograff ear calorimeter model NGR 05 (Vn 316 model, São Paulo, Brazil) for measuring air temperature.
Next, we conducted the eye and labyrinth VENG tests, according to criteria proposed by Mangabeira-Albernaz, Ganança, and Pontes.17
*Eye movement calibration – We verified spontaneous and semi-spontaneous nystagmus using pendular tracking, checking for pre- and post-rotatory plus pre- and post-caloric optokinetic nystagmus. We recorded the caloric stimulation time in each ear using air at 42°C and 18°C lasted 80 seconds for each temperature and responses with eyes closed and then with eyes open to observe the inhibitory effect of eye fixation (IEEF). The criteria used in the air caloric test were: absolute value between 2 and 24 degrees/ sec (<2 degrees/ sec (hyporeflexia), >24 degrees/ sec (hyperreflexia); relative values of labyrinth preponderance (LP) <41% and nystagmus directional preponderance (NDP) <36%.18
Statistical Analysis
We used a difference of proportions test to compare the results of the vestibular examination (analyzing normal and abnormal results) and to correlate FA with the most altered results from the vestibular examination (caloric, semi-spontaneous nystagmus, rotatory, and optokinetic tests) and below, with the most frequent otoneurological symptoms (incoordination of movement, imbalance of gait, and dizziness). Finally, we applied the Fisher test correlating the results of the vestibular examination with otoneurological symptoms of major occurrence. In all cases, we considered p < 0.05 to be statistically significant.
Results
The subjects' ages ranged from six to 72 years, with a mean age 38.6 years and a standard deviation of 14.7 years. The average duration of the disease was 17.7 years and the standard deviation was 9.4 years.
The most frequent complaints in the anamneses were incoordination of movement (66.7%), gait imbalance (56.7%), dizziness (50%), and dysarthria (46.7%), as shown in Table 2.
Table 2. Distribution in frequency of symptoms in 30 Friedreich's ataxia patients.
| SYMPTOMS | NUMBER OF PATIENTS | FREQUENCY (%) |
|---|---|---|
| Incoordination of movement | 20 | 66.7 |
| Gait imbalance | 17 | 56.7 |
| Dizziness | 15 | 50.0 |
| Dysarthria | 14 | 46.7 |
| Headache | 10 | 33.4 |
| Dysphagia | 9 | 30.0 |
| Diplopia | 9 | 30.0 |
| Falling | 8 | 26.7 |
| Tremors | 8 | 26.7 |
| Depression | 8 | 26.7 |
| Fatigue | 7 | 23.4 |
| Anxiety | 7 | 23.4 |
| Difficulty moving the neck | 6 | 20.0 |
| Pain radiating to the shoulder and arm | 5 | 16.7 |
| Tingling in extremities | 4 | 13.4 |
| Insomnia | 3 | 10.0 |
| Neck cracking | 3 | 10.0 |
| Hearing loss | 3 | 10.0 |
| Olfactory change | 2 | 6.7 |
| Gustative change | 2 | 6.7 |
| Dysphonia | 1 | 3.4 |
In assessing the vestibular function, the caloric test, spontaneous and semi-spontaneous, rotatory, optokinetic, and pendulum tracking showed alterations in FA, as shown in Table 3.
Table 3. Distribution in frequency of alterations in vestibular exam in 30 patients with Friedreich's ataxia.
| ALTERED EXAMS | FRIEDREICH'S ATAXIA | |
|---|---|---|
| N | % | |
| Bilateral labyrinthine hyporeflexia | 16 | 53.3 |
| Multiple semi-spontaneous nystagmus | 12 | 40.0 |
| Absent rotary nystagmus | 11 | 36.7 |
| Asymmetrical optokinetic nystagmus | 10 | 33.4 |
| Spontaneous nystagmus | 6 | 20.0 |
| Pendulum tracking alterations | 5 | 16.7 |
| Bilateral labyrinthine hyperreflexia | 5 | 16.7 |
| Bidirectional semi-spontaneous nystagmus | 2 | 6.7 |
| Unidirectional semi-spontaneous nystagmus | 1 | 3.4 |
| Unilateral labyrinthine hyperreflexia | 1 | 3.4 |
Abbreviations: %, frequency; N, number of patients.
Among the tests with alterations in FA, the highest prevalence occurred in: the caloric test (73.4%) with a predominance of hyporeflexia (53.3%); then, the test for semi-spontaneous nystagmus (50.1%), with a predominance of the multiple type (40%); next, the rotatory test (36.7%), which denotes a lack of response from lateral, anterior, and posterior semicircular canals; and optokinetic (33.4%), which shows a change in pursuit movements, as observed in Table 3.
The use of the difference of proportions test proves that there was significance in the correlation between FA with labyrinthine and eye tests that showed more alterations than the others, the caloric test with rotatory (p = 0.0065) and caloric with optokinetic (p = 0.0032).
Regarding the outcome of the vestibular examination, there was a higher incidence of central vestibular dysfunction (70%), as shown in Table 4.
Table 4. Frequency of results from vestibular exam in 30 patients with Friedreich's ataxia.
| VESTIBULAR EXAM RESULT | FRIEDREICH'S ATAXIA | |
|---|---|---|
| N | % | |
| Central vestibular disorder | 21 | 70.0 |
| Peripheral vestibular disorder | 6 | 20.0 |
| Normal vestibular exam | 3 | 10.0 |
| Total | 30 | 100.0 |
Abbreviations: N, number of patients; %, frequency.
The implementation of the difference of proportions test proves that there was a significant difference between the proportions of normal tests and those that showed alterations (p = 0.0000).
The correlation between FA and the three most frequent otoneurological symptoms, can be seen in Table 5.
Table 5. Correlation among most common otoneurological symptoms in 30 patients with Friedreich's ataxia.
| SYMPTOMOLOGY | FRIEDREICH'S ATAXIA | |
|---|---|---|
| N | % | |
| Incoordination of movement | 20 | 66.7 |
| Gait imbalance | 17 | 56.7 |
| Dizziness | 15 | 50.0 |
Abbreviations: N, number of patients; %, frequency.
The implementation of the difference of proportions test proves that there was no significant difference in the correlation between FA symptoms of incoordination of movement and gait imbalance (p = 0.42890), gait imbalance and dizziness (p = 0.6049), and dizziness and incoordination of movement (p = 0.1867).
The result of the vestibular examination and the most frequent otoneurological symptoms is shown in Table 6.
Table 6. Correlation between vestibular exam and most common otoneurological symptoms in 30 patients with Friedreich's ataxia.
| VESTIBULAR EXAM RESULT | INCOORDINATION OF MOVEMENT | GAIT IMBALANCE | DIZZINESS | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Normal vestibular exam | − | 0.0 | 1 | 3.4 | 1 | 3.4 |
| Altered vestibular exam | 20 | 66.7 | 16 | 53.3 | 14 | 46.6 |
| Total | 20 | 66.7 | 17 | 56.7 | 15 | 50.0 |
Abbreviations: N, number of patients; %, frequency.
In the application of Fisher's test, there was no significant difference in the correlation between the results of the entrance examination with the symptoms of incoordination of movement and gait imbalance (p = 0.4595), incoordination of movement and dizziness (p = 0.4286), and gait imbalance and dizziness (p = 0.7258).
Discussion
The most commonly reported symptoms by patients were also observed in several other studies.19 20 21 22 Because of the illness' multidisciplinary clinical characteristics, various events may occur with disease progression.
Nacamagoe, Iwamoto, and Yoshida23 reported that the combination of vestibular dysfunction in the presence of cerebellar atrophy can contribute significantly to the appearance of gait instability, which is part of the initial symptomatology of SCAs.
In this study, the videonystagmography (VNG) examination showed a higher prevalence of vestibular dysfunction (53.3%), as well as altered multiple-type semi-spontaneous nystagmus (40%), rotatory (36.7%), and optokinetic (33.4%) tests. Cerebellar vermis lesions cause ataxia of the upper limbs, head wobbling, dysmetria, and trembling eye movements, which is the body part that manifests electrical activity along the length of the eye muscles and neck.24 The most common alterations in other studies11 22 24 were the presence of positional nystagmus, irregular eye movement calibration, spontaneous rebound nystagmus, bi- and multi-directional semi-spontaneous nystagmus, abolition of optokinetic nystagmus, pendular tracking type IV nystagmus, hyporeflexia, absence of inhibitory effect of eye fixation, and Aubry signs in the Barany test. Among the damaged neuronal structures, the occurrence of vestibular dysfunction is known, but little is known about when and why it occurs. Takegoshi and Murofushi25 report that spinocerebellar ataxia is one of the clinical entities in vestibular disorders.
Prim-Espada et al26 performed an eletrooculographic examination (EOG) on 51 patients diagnosed with genetic FA and observed alterations in saccadic movements for positional, spontaneous, and optokinetic nystagmus. The authors refer to suppression of the vestibular-ocular reflex (VOR) in all patients. Fahey et al27 evaluated 20 patients with FA and observed that, despite presenting normal saccadic speed, extended latency was present. In addition, vestibular disorders were found with a marked reduction in the increase of the VOR. For Hocking, Fielding, and Corben,28 altered saccadic latency can be useful as a marker of severity and progression in FA. Noval et al29 performed eye examinations on 23 patients with FA and observed that visual acuity may decrease with disease progression, based on a small proportion of the patients without citing the percentage.
Zeigelboim et al11 report that the loss of hair cells of the ampullary crests, as well as the decline in the number of nerve cells in the vestibular ganglion (Scarpa), degeneration of the otoliths, reduced labyrinthine blood flow, progressive depression of neural stability, and reduction in the compensation capacity of the vestibular-ocular and vestibulospinal reflexes all contribute to the reduction of speed in the eye tracking motion, as well as rotatory and caloric hyporeactivity in the vestibular system, both peripheral and central, present in SCAs.
In this study, the result of the vestibular exam had a significant predominance of central vestibular dysfunction in 70% of patients. Ito et al22 showed involvement of the central vestibular system and stressed the importance of vestibular evaluation in diseases affecting the posterior fossa. Prim-Espada et al26 observed central alterations in the EOG exam in 72.5% of patients and Monday and Lemieux,30 in 100% of cases via EOG exams. Fahey et al27 and Kirkham et al31 stressed that the range of alterations for eye movements suggest alterations in the brain stem, as well as the cortical and vestibular pathways.
In this study, we did not observe significance in the inter-correlation between the most evident symptoms (lack of coordination of movement, gait imbalance, and dizziness) for FA. We found no data that would challenge our findings.
It was evident that alterations in VNG are related to the severity of SCAs or the clinical stage of the disease.
The study emphasizes the importance of the vestibular evaluation for the topographic diagnosis of neurodegenerative diseases since, in most cases, the otoneurological symptoms present early and such information may aid in the choice of procedures to be performed in clinical and therapeutic monitoring.
Conclusion
The most prevalent otoneurological symptoms were incoordination of movement, gait imbalance, and dizziness.
Alterations in the vestibular examination occurred in 90% of patients, located mainly in the caloric test, with a predominance of deficient central vestibular system dysfunction.
References
- 1.Fogel B L, Perlman S. Clinical features and molecular genetics of autosomal recessive cerebellar ataxias. Lancet Neurol. 2007;6(3):245–257. doi: 10.1016/S1474-4422(07)70054-6. [DOI] [PubMed] [Google Scholar]
- 2.Embiruçu E K, Martyn M L, Schlesinger D, Kok F. Autosomal recessive ataxias: 20 types, and counting. Arq Neuropsiquiatr. 2009;67(4):1143–1156. doi: 10.1590/s0004-282x2009000600036. [DOI] [PubMed] [Google Scholar]
- 3.Ell J, Prasher D, Rudge P. Neuro-otological abnormalities in Friedreich's ataxia. J Neurol Neurosurg Psychiatry. 1984;47(1):26–32. doi: 10.1136/jnnp.47.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rinaldi C, Tucci T, Maione S, Giunta A, De Michele G, Filla A. Low-dose idebenone treatment in Friedreich's ataxia with and without cardiac hypertrophy. J Neurol. 2009;256(9):1434–1437. doi: 10.1007/s00415-009-5130-6. [DOI] [PubMed] [Google Scholar]
- 5.Albano L MJ, Zatz M, Kim C A. et al. Friedreich's ataxia: clinical and molecular study of 25 Brazilian cases. Rev Hosp Clin Fac Med Sao Paulo. 2001;56(5):143–148. doi: 10.1590/s0041-87812001000500003. [DOI] [PubMed] [Google Scholar]
- 6.Alper G, Narayanan V. Friedreich's ataxia. Pediatr Neurol. 2003;28(5):335–341. doi: 10.1016/s0887-8994(03)00004-3. [DOI] [PubMed] [Google Scholar]
- 7.Pandolfo M. Friedreich ataxia. Arch Neurol. 2008;65(10):1296–1303. doi: 10.1001/archneur.65.10.1296. [DOI] [PubMed] [Google Scholar]
- 8.Fortuna F, Barboni P, Liguori R. et al. Visual system involvement in patients with Friedreich's ataxia. Brain. 2009;132(Pt 1):116–123. doi: 10.1093/brain/awn269. [DOI] [PubMed] [Google Scholar]
- 9.Melo M, Fagulha A, Barros L, Guimarães J, Carrilho F, Carvalheiro M. Friedreich ataxia and diabetes mellitus—family study. Acta Med Port. 2005;18(6):479–483. [PubMed] [Google Scholar]
- 10.Baloh R W, Konrad H R, Honrubia V. Vestibulo-ocular function in patients with cerebellar atrophy. Neurology. 1975;25(2):160–168. doi: 10.1212/wnl.25.2.160. [DOI] [PubMed] [Google Scholar]
- 11.Zeigelboim B S, Jurkiewicz A L, Fukuda Y, Mangabeira-Albernaz P L. Alterações vestibulares em doenças degenerativas do sistema nervoso central. Pró-Fono. 2001;13(2):263–270. [Google Scholar]
- 12.Dueñas A M, Goold R, Giunti P. Molecular pathogenesis of spinocerebellar ataxias. Brain. 2006;129(Pt 6):1357–1370. doi: 10.1093/brain/awl081. [DOI] [PubMed] [Google Scholar]
- 13.Schöls L, Bauer P, Schmidt T, Schulte T, Riess O. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol. 2004;3(5):291–304. doi: 10.1016/S1474-4422(04)00737-9. [DOI] [PubMed] [Google Scholar]
- 14.Pearson C E, Nichol Edamura K, Cleary J D. Repeat instability: mechanisms of dynamic mutations. Nat Rev Genet. 2005;6(10):729–742. doi: 10.1038/nrg1689. [DOI] [PubMed] [Google Scholar]
- 15.Schmitz-Hübsch T, du Montcel S T, Baliko L. et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–1720. doi: 10.1212/01.wnl.0000219042.60538.92. [DOI] [PubMed] [Google Scholar]
- 16.Braga-Neto P, Godeiro-Junior C, Dutra L A, Pedroso J L, Barsottini O GP. Translation and validation into Brazilian version of the scale of the assessment and rating of ataxia (SARA) Arq Neuropsiquiatr. 2010;68(2):228–230. doi: 10.1590/s0004-282x2010000200014. [DOI] [PubMed] [Google Scholar]
- 17.Mangabeira-Albernaz P L, Ganança M M, Pontes P AL. São Paulo: Moderna; 1976. Modelo operacional do aparelho vestibular; pp. 29–36. [Google Scholar]
- 18.Costa K CF, Silva S MR, Ganança C F. Estudo das provas oculomotoras e vestibulares por meio da vectonistagmografia. Distúrb Comum. 2005;17:315–322. [Google Scholar]
- 19.Teive H AG. Spinocerebellar ataxias. Arq Neuropsiquiatr. 2009;67(4):1133–1142. [PubMed] [Google Scholar]
- 20.Zeigelboim B S, Ghizoni Teive H A, Sampaio R. et al. Otoneurological findings in spinocerebellar ataxia. Int Tinnitus J. 2011;16(2):161–167. [PubMed] [Google Scholar]
- 21.Klockgether T. Recent advances in degenerative ataxias. Curr Opin Neurol. 2000;13(4):451–455. doi: 10.1097/00019052-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Ito Y I, Mizrahi E I, Zeigelboim B S, Suzuki M R. Síndrome de Friedreich. Acta AWHO. 1993;12(1):39–41. [Google Scholar]
- 23.Nakamagoe K, Iwamoto Y, Yoshida K. Evidence for brainstem structures participating in oculomotor integration. Science. 2000;288(5467):857–859. doi: 10.1126/science.288.5467.857. [DOI] [PubMed] [Google Scholar]
- 24.Cogan D G, Chu F C, Reingold D B. Ocular signs of cerebellar disease. Arch Ophthalmol. 1982;100(5):755–760. doi: 10.1001/archopht.1982.01030030759007. [DOI] [PubMed] [Google Scholar]
- 25.Takegoshi H, Murofushi T. Vestibular evoked myogenic potentials in patients with spinocerebellar degeneration. Acta Otolaryngol. 2000;120(7):821–824. doi: 10.1080/000164800750061660. [DOI] [PubMed] [Google Scholar]
- 26.Prim-Espada M P, de Diego-Sastre J I, Martínez-Salio A, de Sarriá-Lucas M J. [Electrooculography findings in Friedreich's ataxia] Rev Neurol. 2005;40(2):78–80. [PubMed] [Google Scholar]
- 27.Fahey M C, Cremer P D, Aw S T. et al. Vestibular, saccadic and fixation abnormalities in genetically confirmed Friedreich ataxia. Brain. 2008;131(Pt 4):1035–1045. doi: 10.1093/brain/awm323. [DOI] [PubMed] [Google Scholar]
- 28.Hocking D R, Fielding J, Corben L A. et al. Ocular motor fixation deficits in Friedreich ataxia. Cerebellum. 2010;9(3):411–418. doi: 10.1007/s12311-010-0178-5. [DOI] [PubMed] [Google Scholar]
- 29.Noval S, Contreras I, Sanz-Gallego I, Manrique R K, Arpa J. Ophthalmic features of Friedreich ataxia. Eye (Lond) 2012;26(2):315–320. doi: 10.1038/eye.2011.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monday L A, Lemieux B. [Audiovestibular study in Friedreich's ataxia] J Otolaryngol. 1978;7(5):415–423. [PubMed] [Google Scholar]
- 31.Kirkham T H, Guitton D, Katsarkas A, Kline L B, Andermann E. Oculomotor abnormalities in Friedreich's ataxia. Can J Neurol Sci. 1979;6(2):167–172. doi: 10.1017/s0317167100119584. [DOI] [PubMed] [Google Scholar]


