Abstract
Data from approximately 140 articles and reports published since 2000 on drinking, alcohol use disorder (AUD), correlates of drinking and AUD, and treatment needs, access and utilization were critically examined and summarized. Epidemiological evidence demonstrates alcohol-related disparities across U.S. racial/ethnic groups. American Indians/Alaska Natives generally drink more and are disproportionately affected by alcohol problems, having some of the highest rates for AUD. In contrast, Asian Americans are less affected. Differences across Whites, Blacks and Hispanics are more nuanced. The diversity in drinking and problem rates that is observed across groups also exists within groups, particularly among Hispanics, Asian Americans, and American Indians/Alaska Natives. Research findings also suggests that acculturation to the U.S. and nativity affect drinking. Recent studies on ethnic drinking cultures uncover the possible influence that native countries’ cultural norms around consumption still have on immigrants’ alcohol use. The reasons for racial/ethnic disparities in drinking and AUD are complex and are associated with historically-rooted patterns of racial discrimination and persistent socioeconomic disadvantage. This disadvantage is present at both individual and environmental levels. Finally, these data indicate that admission to alcohol treatment is also complex and is dependent on the presence and severity of alcohol problems but also on a variety of other factors. These include individuals’ sociodemographic characteristics, the availability of appropriate services, factors that may trigger coercion into treatment by family, friends, employers and the legal system, and the overall organization of the treatment system. More research is needed to understand facilitators and barriers to treatment to improve access to services and support. Additional directions for future research are discussed.
Keywords: review, race/ethnicity, drinking, treatment access
Introduction
From 2006 through 2010, alcohol consumption ranked as the fourth leading preventable cause of death in the U.S., causing an estimated 88,129 deaths, representing 2,830,608 years of potential life lost for all age groups (0–65+ years; Centers for Disease Control, 2013). Research has shown differential alcohol-related social and health effects across U.S. racial/ethnic groups. The relationship of race/ethnicity to alcohol-related harms is attributed, in part to differences in patterns of drinking. Other individual, interpersonal, and environmental-level factors also play a role. For example, while some groups have higher rates of alcohol consumption, a risk factor for drinking-related harms, others experience harms from drinking despite having similar or lower rates of consumption (Mulia et al., 2009; Witbrodt et al., 2014).
In this critical review, we begin by describing the most current literature on drinking and alcohol use disorder (AUD) among major U.S. racial/ethnic groups: Whites, Blacks, Hispanics, Asian Americans/Pacific Islanders, and American Indians/Alaska Natives. We also provide a selective review of the literature addressing additional factors associated with drinking and AUD. In particular, the effects of nativity, acculturation, the “immigrant paradox,” and ethnic drinking cultures. Further consideration is given to the effects of discrimination, neighborhood disadvantage, residential segregation, and neighborhood ethnic density. Next, we describe alcohol treatment needs in relation to race/ethnicity and factors associated with access and utilization. We conclude this review with directions for future research.
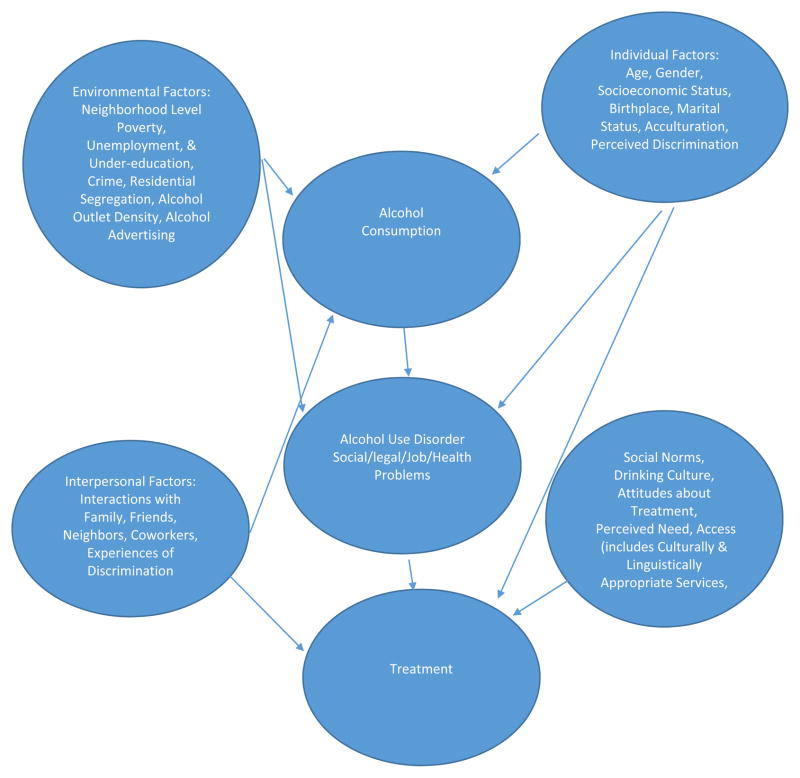
While we focus on different U.S. racial/ethnic groups, we acknowledge significant subgroup differences within these populations. These general categories introduce limitations since ethnicity encompasses a complex combination of factors including birthplace, national origin, language, tribe, and ancestry; any of which may have distinct associations with patterns of drinking and alcohol-related outcomes. Further, individuals of multiethnic backgrounds are not well represented by these categories. The very concept of race has been questioned too, in light of recent genomic discoveries (Foster & Sharp, 2004; Yudell et al., 2015). However, studies that examine race/ethnicity and alcohol-related outcomes serve to understand patterns of alcohol use and the development of AUD, and target at-risk groups for prevention, intervention, and treatment. Figure 1 shows the complexity of the domains that influence alcohol use/misuse and its consequences. However, an exhaustive discussion of all these factors is beyond the scope of this review.
Figure 1.
Conceptual Framework of Alcohol Consumption, Alcohol-Related Problems, and Treatment (adapted from Alegría et al., 2002).
Method
We used several different strategies to identify papers for this review. First, we decided a priori, to report data from the most recently published reports on drinking and AUD in relation to race/ethnicity from federally funded surveys with large representative samples of the U.S. population: The Substance Abuse and Mental Health Services Administration’s (SAMSHA) 2014 National Survey on Drug Use and Health (NSDUH), the longitudinal 2001–2002 (Wave 1) National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), the 2012–2013 NESARC-III, and the cross-sectional NESARC-III. We discuss drinking and AUD among U.S. Hispanic national groups by reporting data from the 2010–2012 NSDUH and 2006 Hispanic Americans Baseline Alcohol Survey (HABLAS). Data on U.S. Asian national groups are reported from the 2002–2003 National Latino and Asian American Study (NLAAS). Data on the differences in drinking and AUD among American Indians by tribe and geographic region are reported from the American Indian-Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project (AI-SUPERPFP). We also decided that large treatment surveillance data sets would be included such as the Treatment Episode Data System (TEDS) which is a compilation of state-collected client-level data to monitor substance abuse treatment systems. Apart from the NSDUH, which includes 12+ year olds, we focus on studies of adults 18+ years of age.
Second, in our discussion of the literature addressing additional factors associated with drinking and AUD (i.e., acculturation, nativity, ethnic drinking cultures, discrimination and neighborhood), as well as factors associated with treatment access and utilization, we restricted our review to epidemiological research with adults (excluding college populations). We searched the English-language literature in PubMed beginning with the year 2000. These PubMed searches employed a combination of key words such as “drinking” and “alcohol” together with key words identifying the main racial/ethnic groups in the U.S. population (e.g., Hispanics, Blacks, American Indians, Asian Americans, Mexican Americans, Puerto Ricans, etc.).
We also searched our own Endnote database, which presently contains 3,443 references from our research and that of others on drinking among U.S. ethnic groups. We then selected papers for inclusion in this review based on a number of criteria: (1) national representativeness of the sample or sample coverage of a large geographical area or racial/ethnic group; (2) content related to one of the areas of focus in the review (e.g., acculturation); (3) comprehensiveness and effectiveness of the analyses (e.g., multivariate methods controlling for confounders); and (4) importance of the findings. We identified approximately 140 studies for inclusion, all of which are in this review.
Drinking across U.S. Racial/Ethnic Groups
Two high-risk consumption patterns that contribute to alcohol-related problems include binge and heavy drinking (Naimi et al., 2003; Rehm et al., 2003). The Substance Abuse and Mental Health Services Administration (SAMHSA; 2015a, 2015b) defined binge drinking in the NSDUH as the consumption of 5+ drinks on the same occasion (at the same time or within a few hours of each other) on at least one day in the previous month (a standard drink being 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor). Heavy drinking was defined as the consumption of 5+ drinks on the same occasion on 5+ days in the past month (SAMSHA 2015a). The 2014 NSDUH (Table 1) showed that rates of previous 30-day binge and heavy drinking were highest among American Indian/Alaska Natives and lowest among Asian Americans (SAMSHA, 2015a). Utilizing data from the 2001–2002 Wave 1 NESARC and the 2012–2013 NESARC-III, Dawson et al. (2015) reported increases in average daily ethanol intake over the decade across racial/ethnic groups (Table 1). Similar to the NSDUH findings in Table 1, in 2001–2002 and 2012–2013, American Indians had the highest average daily intake, while Asian Americans/Pacific Islanders had the lowest (Dawson et al., 2015).
Table 1.
2014 NSDUH:* Prevalence of binge and heavy drinking among persons 12+ years of age. The 2001–2002 Wave 1 NESARC and 2012–2013 NESARC III:** average daily intake and heavy episodic drinking among past year drinkers 18+ years of age.
| 2014 NSDUH | 2001 Wave 1 NESARC and 2012–2013 NESARC III | |||||
|---|---|---|---|---|---|---|
| Daily Intake, oz (se) | Heavy Episodic Drinking (%) | |||||
| Binge Drinking (%) | Heavy Drinking (%) | 2001–2002 | 2012–2013 | 2001–2002 | 2012–2013 | |
| White | 23.5 | 7.1 | 0.62 (0.015) | 0.73 (0.02) | 21.3 | 24.8 |
| Black | 21.6 | 4.5 | 0.75 (0.05) | 1.03 (0.05) | 19.0 | 27.7 |
| Hispanic | 24.7 | 5.1 | 0.59 (0.035) | 0.685 (0.03) | 25.9 | 31.6 |
| American Indian | 27.7 | 9.2 | 0.95 (0.13) | 1.09 (0.125) | 28.1 | 30.4 |
| Asian American | 14.5 | 2.0 | 0.435 (0.06) | 0.49 (0.04) | 15.3 | 17.2 |
| Native Hawaiian/Pacific Islander | 18.3 | 4.6 | - | - | - | - |
In the NSDUH, the American Indian category also included Alaska Natives; binge and heavy drinking were defined as the consumption of 5+ drinks on the same occasion (i.e., at the same time or within a few hours of each other) on at least one day in the previous month and the consumption of 5+ drinks on the same occasion on 5+ days in the past month, respectively.
In the NESARC Wave 1 and NESARC III, the Asian American and Pacific Islander categories were combined; daily intake refers to average daily ethanol intake, one fluid ounce is equivalent to approximately 23.3 g of ethanol. Figures in parentheses are standard errors of estimates; heavy episodic drinking was defined as the consumption of 5+ drinks (men)/4+ drinks (women) of any alcoholic beverage once or more per month.
Adapted from:
SAMHSA, Center for Behavioral Health Statistics and Quality (2015). 2014 National Survey on Drug Use and Health: Detailed Tables. SAMHSA. Rockville, MD. Table 2.42B
Dawson, DA, Goldstein RB, Saha TD, & Grant BF (2015) Changes in alcohol consumption: United States, 2001–2002 to 2012/2013. Drug and Alcohol Dependence 148:56–61.
Regarding the prevalence of heavy episodic drinking (HED; drinking 5+/men and 4+/women drinks of any alcoholic beverage once or more per month), increases across race/ethnicity over the decade were also observed. In the 2001/2002 Wave 1 survey, the proportion of American Indians who engaged in HED was greatest, followed by Hispanics (Dawson et al., 2015). In the 2012/2013 NESARC-III, however, the prevalence of HED among American Indians was slightly less than that of Hispanics, but higher than that of Whites, Blacks, and Asian Americans/Pacific Islanders (Dawson et al., 2015). An important limitation of the NESARC Wave 1 and NESARC-III analysis, however, is that Asian Americans were not differentiated from Pacific Islanders, presumably due to small sample sizes for these groups.
Sociodemographic Correlates of Drinking
In addition to race/ethnicity, there are several additional factors associated with increased drinking. Men drink more than women, a common difference among most U.S. racial/ethnic groups (SAMHSA, 2015a; Dawson et al., 2015). Younger age is also a factor of risk (SAMHSA, 2015a; Dawson et al., 2015). U.S. cross-sectional and longitudinal data have shown an increase in drinking during the twenties followed by declines in the thirties that are sustained in older age groups (SAMHSA 2012a; Dawson et al., 2015). However, among Blacks and Hispanics consumption has been shown to decrease less dramatically with age (Ramisetty-Mikler et al., 2010). Other predictors of increased drinking include lower levels of education, unemployment, and single or divorced marital status (Caetano et al., 2010; Dawson et al., 2015).
Alcohol Use Disorder across U.S. Racial/Ethnic Groups
Cross-sectional data across racial/ethnic groups from the 2012–2013 NESARC-III showed any past 12-month Diagnostic and Statistical Manual (DSM-5) AUD (see https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-use-disorders) to be highest among American Indians, lowest among Asian Americans/Pacific Islanders, and similar among Whites, Blacks, and Hispanics (Table 2). The prevalence of lifetime AUD was also highest among American Indians, lowest among Asian Americans/Pacific Islanders, and was approximately 10% higher for Whites than for Blacks and Hispanics (Grant et al., 2015).
Table 2.
2013 NESARC III: Prevalence of any 12-month and lifetime DSM-5 alcohol use disorder (AUD) by race/ethnicity among persons 18+ years of age.
| Any 12-month AUD* (%) | Any Lifetime AUD** (%) | |
|---|---|---|
| White | 14.0 | 32.6 |
| Black | 14.4 | 22.0 |
| Hispanic | 13.6 | 22.9 |
| Native American | 19.2 | 43.4 |
| Asian American or Pacific Islander | 10.6 | 15.0 |
N=5,133
N=10,001
Adapted from: Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, & Hasin DS. Epidemiology of DSM-5 Alcohol Use Disorder. Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry (2015); 72(8):757–766.
Sociodemographic Correlates of Alcohol Use Disorder
AUD does not affect all individuals equally. Data from the 2012–2013 NESARC-III showed that the prevalence of any 12-month AUD was 17.6% (men) and 10.4% (women). In multivariate analyses, men were approximately twice as likely as women to have past 12-month AUD (Grant et al., 2015). Nationally representative data from the 2005–2010 National Alcohol Survey (NAS) have demonstrated how racial/ethnic disparities in alcohol dependence are also gender-specific. Compared to White women, Black women were at greater risk for dependence at all levels of heavy drinking. Black-White as well as Hispanic-White disparities were also seen among men: Blacks were at increased risk of dependence at no and low levels of heavy drinking whereas Hispanics were at increased risk at low and moderate levels of heavy drinking (Witbrodt et al., 2014). Like many telephone surveys, however, the NAS is limited by challenging response rates (i.e., in the 2000, 2005, and 2010 surveys, response rates ranged from 52% to 58%; Zemore et al., 2013).
The odds of developing an AUD have been shown to decrease with increasing age. For example, NESARC-III data showed that compared to 65+ year olds, the odds of developing any past 12-month AUD were 13.9 (99% CI: 11.57–16.67), 8.7 (99% CI: 7.11–10.57), and 4.8 (99% CI: 3.94–5.84) for 18–29, 30–44, and 45–64 year olds, respectively (Grant et al., 2015). Never married individuals and those who were separated, divorced, or widowed were also at greater risk (Grant et al., 2015). Studies have also shown that socioeconomic status (SES) is associated with AUD (see Collins, 2016 for a thorough review of this literature).
While informative, direct comparisons between the NSDUH and NESARC studies are limited. First, and importantly, the NESARC studies failed to provide data that differentiated between Asian Americans and Native Hawaiian/Pacific Islanders. In contrast, the NSDUH provided data separately for both groups. The NSDUH, however, combined data on American Indians and Alaska Natives. This is problematic because significant differences in drinking in relation to tribe and geographic region have been identified (Whitesell et al., 2012; O’Connell et al., 2005, Beals et al., 2005, Beals et al., 2003; Koss et al., 2003). A second hindrance is the way in which alcohol consumption was reported across studies. For example, the NSDUH reported on binge drinking (i.e., 5+ drinks on the same occasion at the same time or within a couple of hours of each other on ≥ 1 day in the previous 30 days). The NESARC studies, on the other hand, reported on HED (i.e., 5+/men and 4+/women) drinks once or more per month in the previous 12 months). Assessment of past-30 day intake is problematic because if large quantities of alcohol are consumed per occasion, but in an infrequent manner, the amount of drinking may be underestimated. Third, the NSDUH reported data for persons 12+ years of age whereas the NESARC included data from adults 18+ years of age.
Drinking and Alcohol Use Disorder among U.S. Hispanic National Groups
There are few publications utilizing nationally representative data examining differences in drinking and AUD among different U.S. Hispanic national groups. Examining such differences is important because of the diversity of this population. Utilizing 2010–2012 NSDUH data, Jetelina et al., (2016) found no statistically significant differences in binge drinking among Puerto Ricans (29%), Mexican Americans (27%), South/Central Americans (25%), and Cuban Americans (24%). There were, however, statistically significant differences in past 12-month DSM-IV alcohol dependence. The rate for Puerto Ricans was 7%, followed by South/Central Americans (6%), Puerto Ricans (4%), and Cuban Americans (3%; Jetelina et al., 2016). Other data on differences across Hispanic national groups are from the 2006 HABLAS. This study identified marked differences across groups. Puerto Rican and Mexican American men (Table 3) reported greater weekly consumption, more binge drinking (consumption of 5+ drinks within a 2-hour period), and higher rates of past 12-month DSM-IV alcohol abuse and dependence than South/Central and Cuban Americans (Caetano et al.,2009; Ramisetty-Mikler et al., 2010). Among women, Puerto Ricans drank more, binged (4+ drinks within a 2-hour period) more frequently, and had a higher prevalence of past 12-month DSM-IV alcohol dependence than women of other national groups (Caetano et al.,2009; Ramisetty-Mikler et al., 2010). A limitation of HABLAS is that data were collected in five metropolitan areas of the U.S., thus rural Hispanic populations were not represented.
Table 3.
2006 HABLAS: Number of drinks consumed per week, binge drinking,* and past 12-month DSM-IV abuse, and dependence, among men and women 18+ years and older by Hispanic national group (means and proportions).
| Hispanic National Group | Mean number of drinks per week (se) | Binge Drinking (%) | Past 12-month DSM-IV Abuse (%) | Past 12-month DSM-IV Dependence (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | |
| Puerto Ricans | 16.9 (1.6) | 9.5 (2.3) | 48.6 | 51.1 | 5.2 | 0.7 | 15.3 | 6.4 |
| Mexican Americans | 15.9 (1.7) | 3.0 (1.0) | 46.2 | 26.1 | 5.6 | 0.8 | 15.1 | 2.1 |
| Cuban Americans | 8.4 (0.9) | 3.4 (1.1) | 27.3 | 22.4 | 1.8 | 1.1 | 5.3 | 1.6 |
| South/Central Americans | 8.9 (0.8) | 3.8 (0.6) | 42.9 | 27.3 | 4.2 | 0.2 | 9.0 | 0.8 |
Binge drinking is defined as: consumption of 5 or more (men) or 4 or more (women) standard drinks within a 2-hour period.
Adapted from: Ramisetty-Mikler S, Caetano R, Rodriguez LA (2010). The Hispanic Americans Baseline Alcohol Survey (HABLAS): Alcohol consumption and sociodemographic predictors across Hispanic national groups. J Subst Use 15: 402–416.
Drinking and Alcohol Use Disorder among U.S. Asian National Groups
Data from the 2002–2008 NSDUH have demonstrated the heterogeneity of Asian Americans in drinking practices. Lee and colleagues (2013) found that the prevalence of past 30-day binge drinking was highest among Korean Americans (24.8%), followed by Filipino and Japanese Americans (14.5% and 14.2%, respectively), Asian Indian Americans (10.1%), and finally Chinese Americans (8.1%). They further showed that among past 30-day drinkers, Japanese Americans had the highest number of past-month drinking days (8.8), followed by Korean and Asian Indian Americans (7.1 and 6.9, respectively), then Chinese Americans (5.7) and Filipino Americans (5.1). On those drinking days, all groups consumed an average of just over 2 drinks per day (range of 1.7 for Chinese Americans to 2.6 for Korean Americans; Lee et al., 2013).
Chea and colleagues (2008) analyzed data on any lifetime DSM-IV AUD from the 2002–2003 NLAAS and found that prevalence rates varied widely across national groups. The lowest prevalence was among Vietnamese Americans at 2.5%. The rates among Chinese and Filipino Americans were 10.3% and 20.2%, respectively. “Other” Asian Americans had the highest rate at 39.3%. However, this “other” Asian American category included respondents representing 17 different national groups, with widely varying cultures and languages. Unfortunately, these NLAAS data are more than 10 years old and to our knowledge, no more recent data are available. Further research on drinking and AUD among Asian Americans is clearly needed to identify groups at greatest risk for culturally and linguistically appropriate targeted prevention and intervention efforts.
Drinking and Alcohol Use Disorder: Tribal and Regional Differences among American Indians
When viewed as a whole, American Indians appear to drink more and have higher rates of AUD compared to other racial/ethnic groups (SAMHSA, 2015a; Dawson et al., 2015). However, several American Indian/Alaska Native groups have lower rates of substance use than the U.S. general population, including higher rates of abstinence and lower rates of past 12-month alcohol dependence (Cunningham et al., 2016; Whitesell et al., 2012; Spicer et al., 2003; Beals et al., 2003). Drinking and AUD differ widely in relation to tribe and geographic region (Steele et al.,2008; O’Connell et al., 2005; Beals et al., 2005; Koss et al., 2003; Denny et al., 2003) which is not surprising since there are 566 federally recognized tribes and communities in the U.S. (Bureau of Indian Affairs, 2015).
The AI-SUPERPFP collected data from randomly selected American Indians in the Southwest and Northern Plains. Rates of heavy drinking (5+ drinks per day) were lower in the Southwest (men: 86.6% and women: 67.2%) than the Northern Plains (men: 92.5% and women: 87.1%; O’Connell et al., 2005). There were also differences in rates of DSM-IV AUD across regions. The rate of past 12-month abuse was lower among Southwest men and women (7.4% and 1.5%, respectively) than Northern Plains men and women (8.2% and 5.1%, respectively; Beals et al., 2005). Similar differences were observed for 12-month alcohol dependence (Southwestern tribe men and women, 8.9% and 1.1%, respectively and Northern Plains tribes men and women, 12.7% and 7.0%, respectively; Beals et al., 2005). Although informative, the AI-SUPERPFP results reported here are dated. Further epidemiological investigations that may serve to complement existing and ongoing qualitative and ethnographic studies among American Indians/Alaska Natives are warranted.
This previous section has described findings on drinking and AUD among U.S. racial/ethnic groups. This epidemiological evidence demonstrates the considerable alcohol-related disparities across U.S. racial/ethnic groups. American Indians/Alaska Natives generally drink more and are disproportionately affected by alcohol problems, having some of the highest rates for AUD. In contrast, Asian Americans are less affected. The diversity in drinking and problem rates that is observed across groups also exists within groups, particularly among Hispanics, Asian Americans, and American Indians/Alaska Natives.
There are several notable additional factors associated with drinking and AUD in relation to race/ethnicity. In the following section, the association between drinking and related outcomes are further discussed in relation to important findings in the research literature. These include acculturation, nativity, the “immigrant paradox,” and ethnic drinking cultures. The effects of discrimination, neighborhood disadvantage, residential segregation, and ethnic density are also discussed.
Acculturation and Nativity
There exists an expansive literature on the relationship between acculturation to the U.S. and behavioral and health outcomes. Acculturation refers to how immigrants adopt and adapt to the values, traditions, behaviors, and language of the new culture following their entry and settlement to the host country (Berry, 2005). Many acculturation scales are conceptually based on a view that acculturation takes place on a single continuum where the loss of attitudes, values, and behaviors of the culture of origin are replaced by adopting those of the host society. These measures place individuals on a continuum between highly acculturated to U.S. culture at one end to highly traditional to the heritage culture at the other.
Two hypotheses have been proposed in explaining the effect of acculturation to American society and increases in alcohol consumption among Hispanics (see Zemore, 2007 for a thorough review of this literature). The first is that the acculturation process is associated with more liberal and favorable drinking norms and attitudes, and thus, increased drinking. The second is that immigrants are thought to drink alcohol as a way to cope with acculturative stressors due to discrimination, language barriers, and family cultural conflicts. Past research supports the first hypothesis that more acculturated Hispanics have more liberal attitudes and positive norms toward drinking (Mills and Caetano, 2012; Zemore, 2005). Research findings on the association between acculturation stress and drinking outcomes have been less consistent. For example, Mills and Caetano (2012) found no support for acculturation stress serving as a mechanism to explain the relationship between acculturation and drinking. In contrast, Lee and colleagues (2013) found that greater acculturative stress was associated with alcohol problems but that acculturation alone was not. These same conceptual frameworks are also utilized to explain the increase in alcohol consumption among Asian Americans. (Park et al., 2014; Iwamoto et al., 2016).
Among Hispanics, acculturation effects on drinking behaviors among women are noteworthy and more consistent than those for men. Research evidence shows that acculturation among women is positively associated with increased probabilities of several drinking outcomes: current drinking status, higher average weekly/monthly consumption, frequency of drunkenness, binge drinking, drinking problems, and AUD (Vaeth et al., 2012; Zemore, 2007; Zemore, 2005; Caetano and Clark, 2003). Birthplace or foreign nativity also strongly impacts drinking and related outcomes, particularly among men (Vaeth et al., 2012; Mills and Caetano, 2012; Caetano et al., 2012; Szaflarski et al., 2011; Caetano et al., 2009; Borges et al., 2006; Grant et al., 2004; Vega et al., 2003).
Among Asian Americas, research on acculturation and foreign nativity on alcohol consumption patterns is more limited than investigations among Hispanics. A number of such studies use small convenience samples (largely among college students), rather than randomly selected general population samples. In general, acculturation has been shown to be associated with greater alcohol use among Asian immigrants (Park et al., 2014). Moreover, foreign-born Asians are less likely to drink in the past month, engage in binge and heavy drinking, and have a lower prevalence of AUD than U.S.-born Asians (Lee et al., 2013; Lo et al., 2014; Breslau and Chang, 2006). Longer length of U.S. residence is also associated with heavy drinking among immigrant Asians (Lo et al., 2014). In fact, Szaflarski and colleagues (2011) found that foreign-born Asians and their U.S.-born counterparts had the largest threefold difference in rates of excessive drinking compared to other groups, including Hispanics, Blacks, and Whites.
The “Immigrant Paradox”
A consistent finding in the research literature is that of the “immigrant paradox” whereby immigrant groups in the U.S. have better health indices, including substance use, than U.S. born generations (Alegria et al. 2006; Vega et al. 2009; Rios-Bedoya and Freile-Salinas, 2014a, 2014b). However, the reasons for the existence of this paradox are still debated. Many have proposed that immigrant groups are self-selected and as such, physically and psychologically healthier (Alegria et al., 2008; Salas-Wright et al., 2014a; Salas-Wright et al., 2014b). Others suggest that some immigrant groups possess protective characteristics such as family cohesion that may be lost in future generations of the U.S.-born (Marsiglia et al., 2009b; Rivera et al., 2008; Canino et al., 2008; Estrada-Martinez, et al., 2011). Some have suggested that the poorer health indices of subsequent U.S.-born members of immigrant groups are due to the frustration associated with difficulty in fulfilling ambitions of socioeconomic betterment due to segregation and discrimination, all factors of risk for increased involvement with substance use (Smedley et al., 2003; Mason et al., 2011; Cooper et al., 2007; Williams and Collins, 2001; Landrine and Klonoff, 2000; Gilbert and Zemore, 2016; Brondolo et al., 2009; Tran et al., 2010).
Ethnic Drinking Cultures
An increasing number of studies have examined the impact of ethnic drinking cultures on the drinking patterns of Hispanics and Asian Americas (Cook et al., 2015; Cook and Caetano, 2014; Cook et al, 2013; Cook et al., 2012). Ethnic drinking cultures refer to the cultural norms, values, and behavioral practices associated with drinking in an immigrant’s home country (Cook et al., 2012). The underlying premise of this construct is that immigrants often maintain ties with their native countries and preserve their cultural heritage so that the drinking practices in their countries of origin still influence their drinking in the U.S. (Cook et al., 2012). Cook et al., (2012) found that U.S. Asians from countries characterized by higher per capita alcohol consumption were more likely to be current drinkers, annually consume larger volumes of alcohol, and drink more frequently. In another study that examined the associations of ethnic drinking cultures on alcohol drinking patterns among Asian Americans and Hispanics, Cook and Caetano (2014) similarly found that for Asians in the U.S., per capita alcohol consumption in the countries of origin was significantly and positively associated with usual drinking quantity, frequency of heavy drinking, and the volume of past 12-month consumption. Per capita consumption level, however, was only associated with usual drinking quantity among Hispanics. The more prominent role of ethnic drinking cultures among Asian Americans than Hispanics may be due to the wider range of drinking patterns among Asian countries than among Latin American countries (Cook and Caetano, 2014).
Racial/Ethnic Discrimination
Two interrelated frameworks serve to explain the relationship between minority status in the U.S. and alcohol-related behaviors. One is a framework referring to social disadvantage, encompassing both racial discrimination and poverty (Mulia et al., 2008). With this model, considerations of discrimination and poverty are necessary to understand alcohol use and its consequences. A related framework, the minority stress model, emphasizes that discrimination and prejudices are stressors that may explain minority drinking behaviors (Keyes et al., 2012, Keyes et al., 2011). An additional framework, the social resistance framework, implies that the discrimination experienced by racial/ethnic minority groups, along with their low social status and sense of alienation from society, leads to active resistance which may include poor health behaviors such as alcohol misuse (Factor et al, 2013; Factor et al., 2011).
Research findings have generally demonstrated a positive association between experiences of racial/ethnic discrimination, drinking and alcohol-related consequences among minorities (Martin et al., 2003, Gee et al., 2007; Mulia et al., 2008, Chae et al., 2008, Mulia et al., 2009; Tran et al., 2010; Borrell et al., 2010; Zemore el al., 2011; Mulia and Zemore, 2012; Borrell et al., 2013; Otiniano Verissimo et al., 2014; Zemore et al., 2016; Gilbert and Zemore, 2016). For example, Martin et al. (2003) found that among a national sample of Blacks, reports of discrimination more than doubled the odds of problem drinking. In another study, high levels of awareness of racial/ethnic stigma among Blacks and Hispanics were associated with a 2-fold greater risk of problem drinking compared to those who reported low levels of stigma (Mulia et al., 2008). Borrell et al. (2010) found that Hispanics who self-reported experiences of racial/ethnic discrimination had a 62% greater odds of drinking heavily. Among Asian Americans with low levels of ethnic identification, racial/ethnic discrimination was associated with an increased likelihood of past-year AUD (Chae et al., 2008). In a recent literature review of 97 scientific articles on the association between discrimination and alcohol outcomes, 71 of which specifically focused on racial/ethnic discrimination, Gilbert and Zemore (2016) concluded that the research generally affirms that experiences of discrimination are positively linked to alcohol misuse and related consequences. However, they note that the quality of research in this area varies widely and that the literature primarily focuses on Blacks with an under-representation of research on other U.S. racial/ethnic minority groups.
Neighborhood Effects: Residential Segregation Disadvantage, and Ethnic Density
Beyond the individual-level effects from personal experiences of racial discrimination on drinking, institutionalized discrimination creates racially segregated neighborhoods (Borrell et al., 2013) that may also impact alcohol use. Racial residential segregation is especially severe among Blacks compared to Hispanics and Asian Americans (Massey, 2001a); and among Hispanics, Puerto Ricans are more segregated than other national groups (Iceland et al., 2008; Wahl et al., 2007). Research suggests that these highly segregated neighborhoods negatively impact the health and substance use behaviors of residents and this is particularly so in predominantly Black neighborhoods (Mason et al., 2011; Cooper et al., 2007; Williams and Collins, 2001; Acevedo-Garcia etal., 2003).
These segregated neighborhoods are generally characterized by concentrated poverty, violence, and crime (Massey, 2001b). Moreover, disadvantaged minority communities are often heavily targeted by alcohol advertisers (Hackbarth et al., 2001; Kwate, 2007; Kwate and Lee, 2007), and disproportionately bear higher densities of retail alcohol outlets (Berke et al., 2010; Romley et al., 2007). Research has consistently demonstrated that residing in disadvantaged neighborhoods is associated with poorer physical and mental health, above and beyond individual sociodemographic characteristics (Galea et al., 2007; Matheson et al., 2006; Truong and Ma, 2006; Pickett and Pearl, 2001). Although, there is some inconsistency across studies (Karriker-Jaffe, 2011), neighborhood disadvantage also appears to influence substance use/misuse (Karriker-Jaffe et al., 2016; Brenner et al., 2015; Karriker-Jaffe et al., 2012; Mulia and Karriker-Jaffe, 2012; Cerdá et al., 2010; Karriker-Jaffe, 2013; Bernstein et al., 2007; Jason et al., 2001).
In contrast to research showing that racial residential segregation results in health disparities, especially for African Americans, other research findings indicate that there may be an “ethnic density effect” whereby racial/ethnic minorities are healthier when they live in areas with high concentrations of people of the same ethnicity and this appears to be particularly evident among Hispanics: notably, older Mexican Americans (Bécares et al., 2012; Alvarez and Levy, 2012; Alba et al., 2014; Lee et al., 2007; Ostir, et al., 2003; Patel et al., 2003). With regard to alcohol use/misuse, research indicates that for Hispanics, as the neighborhood composition of co-ethnics increases, the risk of heavy/problem drinking and AUD decreases (Stroope et al., 2015; Molina et al., 2012; Markides et al., 2012). Although Markides et al., (2012) found this to be the case for Mexican American women, but not men. Hypothesized mechanisms by which ethnic density leads to health and well-being include enhanced social cohesion (Hong et al., 2014), social support (Shell et al., 2013), community participation or civic engagement (Stafford et al., 2010; Bécares et al., 2009), and collective efficacy (Frank et al., 2007; Vega et al., 2011). In addition, ethnic density may buffer the effects of discrimination (Bécares et al., 2009), and the stigma of both disadvantaged and minority status (Pickett and Wilkinson, 2008).
In summary, research suggests that acculturation to the U.S. increases alcohol consumption among Hispanic and Asian immigrants through adopting more liberal attitudes and norms toward drinking or to cope with stress from adjusting to life in the host country. At the same time, however, recent immigration or less acculturation among Hispanics and Asian Americans may be associated with protective factors, such as family cohesion. Recent studies on ethnic drinking cultures uncover the possible influence that native countries’ cultural norms around consumption still have on immigrants’ alcohol use. Understanding the degree to which immigrants adopt the drinking norms and attitudes of the U.S. or continue to adhere to the norms and attitudes of their country of origin that are gender-specific, may lead to a deeper explanation of immigrants’ alcohol consumption patterns.
The reasons for racial/ethnic disparities in drinking and AUD are complex and are associated with historically-rooted patterns of racial discrimination and persistent socioeconomic disadvantage. This disadvantage is present at the individual level with regard to fewer opportunities for higher education, professional training, secure employment, and access to health care. Socioeconomic disadvantage at the neighborhood level also affects the health and well-being of residents. These disadvantaged neighborhoods are frequently in inner city areas, which are racially and economically segregated and characterized by substandard housing, poor schools, high crime, excessive alcohol advertising and alcohol outlets, and general social disorganization.
Race/Ethnicity and Treatment Access and Utilization
Given the levels of drinking and in some cases, racially/ethnically-specific factors of risk identified in the sections above, there is clearly a need for appropriate and adequate access to alcohol treatment programs for racial/ethnic minority groups. The following section examines the extent to which racial/ethnic minorities have access to and utilize these treatment programs.
Treatment for alcohol and other SUDs is a cornerstone of a comprehensive policy to address alcohol and drug problems worldwide (Babor et al., 2010). However, treatment utilization is not only determined by need, as defined by the prevalence of AUD in a particular racial/ethnic group and the severity of disease, but also by a number of other factors which may or may not be connected with such need. For instance, substance use treatment is frequently triggered by pressures from family, friends, employers, and the legal system (Weisner and Schmidt, 2001; Weisner et al., 2002). Therefore, those who have jobs, family, or friends are more likely to be led to or coerced into treatment than those who do not.
Treatment utilization can also be affected by proximity of services to one’s home and by potential barriers such as inability to cover treatment costs, loss of income while in treatment, or child care and transportation availability/expenses. Interestingly, medical insurance does not seem to be associated with treatment utilization when the influence sociodemographic factors are taken into account (Weisner et al., 2002), perhaps due to the availability of public programs for SUD treatment.
The availability of culturally and linguistically appropriate services is also important. For example, evidence suggests that American Indians/Alaska Natives are more comfortable with services that integrate tribal customs, traditions, and spirituality (Venner et al., 2016; Novins et al., 2011 Spicer et al., 2007). Among Asian Americans, fear of shame or losing face has been identified as a barrier to treatment receipt (Masson et al., 2013).
Receipt of Treatment
Data by race/ethnicity from the 2014 NSDUH show that a slightly higher percentage of Whites (21.9%) than Blacks (19.1%) and Hispanics (19.3%) who were in need of treatment actually received it (SAMHSA, 2015a). Proportions for American Indians/Alaskan Natives, Native Hawaiians/Pacific Islanders, and Asians were not reported due to low precision in the estimates. Combined 2003–2010 NSDUH data comparing Hispanics and non-Hispanics indicated that among those 12+ years of age who met criteria for substance abuse or dependence, 9% of Hispanics versus 10.5% of non-Hispanics received treatment (SAMHSA, 2012b). Treatment was considered only if it occurred in drug or alcohol rehabilitation facilities, hospitals, and mental health centers. The majority of Hispanics (94.4%) and non-Hispanics (94.8%) with a positive diagnosis of DSM-IV abuse or dependence, did not feel they needed treatment.
SAMHSA’s TEDS provides trend data by race/ethnicity from 2002–2012 (SAMHSA, 2014b). The racial/ethnic composition of these admissions did not change much during that time period (Table 4). White admissions increased slightly and Black admissions decreased by nearly 5%, comprising about a fifth of all admissions in 2012. Hispanic admissions were basically stable, representing a little over a tenth of all admissions from 2002 to 2012. Admission for American Indians/Alaskan Natives, Asians/Pacific Islanders, and “other” were also relatively stable throughout the period and comprised between 4% and 6.1% of all admissions. Compared to the U.S. population (Table 4), Whites and American Asians/Pacific Islanders were underrepresented in admissions, while Blacks and Native Americans were overrepresented. Hispanic representation in admissions was similar to their proportion in the population. However, given that the prevalence of AUD varies across these groups, their representation in treatment should not necessarily be equal to their proportion in the population.
Table 4.
Admissions aged 12 and older by race and ethnicity: 2002 to 2012 and U.S. population 12 years of age and older.
[Based on administrative data reported to TEDS by all reporting states and jurisdictions (excl. Puerto Rico).]
| Race/ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | U.S. pop.(000s)1
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Number
|
||||||||||||
| No. of admissions | 1,874,278 | 1,847,737 | 1,793,533 | 1,871,558 | 1,946,923 | 1,941,589 | 2,014,888 | 1,975,194 | 1,910,439 | 1,915,333 | 1,736,926 | 254,306 |
|
| ||||||||||||
|
Percent distribution
|
||||||||||||
| White (non-Hispanic) | 58.5 | 58.6 | 59.6 | 59.2 | 59.9 | 60.2 | 60.2 | 60.2 | 60.8 | 60.9 | 61.0 | 69.1 |
| Black (non-Hispanic) | 24.3 | 24.0 | 22.8 | 22.4 | 21.6 | 21.1 | 21.1 | 21.1 | 20.5 | 20.5 | 19.6 | 12.1 |
| Hispanic origin | 12.8 | 12.8 | 12.8 | 13.6 | 13.3 | 13.2 | 13.2 | 13.1 | 12.7 | 12.7 | 13.3 | 12.8 |
| Mexican | 5.2 | 5.2 | 5.3 | 5.4 | 5.5 | 5.6 | 5.5 | 5.4 | 4.3 | 4.0 | 4.5 | n/a |
| Puerto Rican | 4.4 | 4.1 | 3.9 | 4.0 | 3.6 | 3.5 | 3.5 | 3.5 | 3.4 | 3.5 | 3.6 | n/a |
| Cuban | 0.3 | 0.4 | 0.3 | 0.5 | 0.4 | 0.2 | 0.2 | 0.2 | 0.2 | 0.3 | 0.3 | n/a |
| Other/not specified | 2.9 | 3.1 | 3.3 | 3.8 | 3.8 | 3.9 | 3.9 | 4.0 | 4.8 | 4.8 | 4.9 | n/a |
| Other | 4.4 | 4.5 | 4.8 | 4.8 | 5.2 | 5.5 | 5.6 | 5.6 | 6.0 | 5.9 | 6.1 | 6.1 |
| American Indian/Alaska Native | 2.1 | 1.9 | 2.0 | 2.1 | 2.2 | 2.3 | 2.2 | 2.2 | 2.3 | 2.2 | 2.4 | 0.7 |
| Asian/Pacific Islander | 0.9 | 1.0 | 0.9 | 1.0 | 1.0 | 0.9 | 0.9 | 0.9 | 1.0 | 1.0 | 1.0 | 4.9 |
| Other | 1.4 | 1.7 | 1.9 | 1.7 | 2.1 | 2.3 | 2.4 | 2.4 | 2.7 | 2.7 | 2.7 | 0.4 |
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
U.S. Bureau of Census, for population projections by state, age, gender, race.
n/a Not applicable.
SOURCE: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Treatment Episode Data Set (TEDS). Data received through 10.17.13. Population: U.S. Bureau of the Census. Population projections by state, age, gender, race. 2000–2050.
TEDS data also indicate that there is variation in the primary substance used at admission across race/ethnicity (Table 5). Among all racial/ethnic groups, the majority of admissions were due to alcohol alone or in combination with a secondary drug. Opiates constituted the second most common drug at admission among Whites and Hispanics. Among American Indians/Alaska Natives, both opiates and marijuana/hashish were the second most common drug. Marijuana/hashish was also the second most common drug among Blacks and Asian Americans/Pacific Islanders. The third most common drug at admission was marijuana/hashish for Whites and Hispanics, cocaine for Blacks, and methamphetamine/amphetamines for American Indians/Alaska Natives and Asian Americans/Pacific Islanders.
Table 5.
Admission aged 12 and older, by race/ethnicity according to primary substance of abuse: 2012
[Based on administrative data reported to TEDS by all reporting states and jurisdictions.]
| Race/ethnicity | All admis- sions |
Primary substance at admission
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alcohol | Opiates | Cocaine | Mari- juana/ hashish |
Metham- phetamine/ amphet- amines |
Tran- quil- izers |
Seda- tives |
Hallu- cino- gens |
PCP | Inhal- ants |
Other/ none speci- fied |
||||||
|
| ||||||||||||||||
| Alcohol only | With secondary drug | Heroin | Other opiates | Smoked cocaine | Other route | |||||||||||
| No. of admissions | 1,739,977 | 373,293 | 305,709 | 284,678 | 169,220 | 82,871 | 37,799 | 304,110 | 123,922 | 17,353 | 3,289 | 2,023 | 5,718 | 1,102 | 28,890 | |
|
| ||||||||||||||||
| Row percent distribution | Total | |||||||||||||||
|
|
||||||||||||||||
| All admissions | 1,739,977 | 21.5 | 17.6 | 16.4 | 9.7 | 4.8 | 2.2 | 17.5 | 7.1 | 1.0 | 0.2 | 0.1 | 0.3 | 0.1 | 1.7 | 100.0 |
| White (non-Hispanic) | 1,060,065 | 23.4 | 16.8 | 17.4 | 13.8 | 2.6 | 1.6 | 12.7 | 8.1 | 1.3 | 0.2 | 0.1 | 0.1 | 0.1 | 1.8 | 100.0 |
| Black (non-Hispanic) | 339,920 | 14.8 | 20.9 | 12.6 | 2.1 | 13.6 | 3.5 | 28.2 | 1.3 | 0.3 | 0.1 | 0.1 | 1.1 | * | 1.6 | 100.0 |
| Hispanic origin | 234,204 | 20.1 | 15.6 | 19.9 | 3.8 | 2.9 | 3.1 | 22.8 | 9.4 | 0.7 | 0.1 | 0.1 | 0.5 | 0.1 | 1.0 | 100.0 |
| Mexican | 77,723 | 23.2 | 15.0 | 10.4 | 3.1 | 1.5 | 1.5 | 25.9 | 18.4 | 0.2 | 0.1 | 0.1 | 0.2 | 0.1 | 0.5 | 100.0 |
| Puerto Rican | 66,325 | 12.7 | 16.2 | 39.1 | 3.2 | 4.2 | 4.0 | 16.4 | 0.7 | 1.1 | 0.1 | 0.1 | 1.0 | 0.1 | 1.3 | 100.0 |
| Cuban | 4,870 | 31.3 | 16.3 | 13.6 | 5.2 | 4.4 | 4.7 | 17.4 | 3.4 | 0.9 | 0.1 | 0.2 | 0.4 | 0.1 | 2.0 | 100.0 |
| Other/not specified | 85,286 | 22.4 | 15.8 | 13.8 | 4.8 | 3.3 | 3.7 | 25.3 | 8.2 | 0.8 | 0.2 | 0.1 | 0.4 | 0.1 | 1.2 | 100.0 |
| Other | 105,788 | 26.3 | 19.2 | 10.2 | 6.7 | 2.6 | 1.4 | 19.5 | 11.3 | 0.5 | 0.2 | 0.1 | 0.2 | 0.1 | 1.6 | 100.0 |
| American Indian/Alaska Native | 41,147 | 35.9 | 26.0 | 5.7 | 7.5 | 1.6 | 0.8 | 13.2 | 7.6 | 0.3 | 0.1 | 0.1 | 0.1 | 0.2 | 1.0 | 100.0 |
| Asian/Pacific Islander | 17,515 | 23.1 | 13.6 | 8.4 | 5.3 | 2.6 | 1.4 | 21.2 | 20.3 | 0.6 | 0.2 | 0.1 | 0.1 | * | 2.9 | 100.0 |
| Other | 47,126 | 19.2 | 15.4 | 14.7 | 6.4 | 3.4 | 2.0 | 24.4 | 11.3 | 0.7 | 0.1 | 0.2 | 0.4 | 0.1 | 1.6 | 100.0 |
Less than 0.05 percent.
SOURCE: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Treatment Episode Data Set (TEDS). Data received through 10.17.13.
Other Literature on Access and Utilization
Apart from the federal data discussed above, there is also a peer-reviewed literature on alcohol treatment access and utilization by U.S. racial/ethnic minority groups (e.g., see Chartier and Caetano, 2010). Research findings on need and utilization of treatment by racial/ethnic groups are sometimes contradictory. Utilizing NAS data, Schmidt et al., (2007) reported no major differences in the rate of lifetime treatment utilization across Whites (15.8%), Blacks (14.7%), and Hispanics (16.3%) with a lifetime diagnosis of alcohol abuse or dependence. Further, Blacks and Hispanics with higher problem severity were less likely than Whites to receive treatment. Among individuals with an AUD, Hispanics were less likely than Whites to use alcohol/drug treatment programs or receive help from health professionals (physician, psychiatrist, psychologist, or social worker). At higher levels of severity, Blacks and Hispanics with an AUD were also less likely to use certain types of services (mental health, self-help). Contradictorily, Keyes et al. (2008), found no evidence of differential treatment utilization of alcohol treatment services between Whites and Blacks.
Zemore et al., (2014) reported on data from the NAS on the effects of both race/ethnicity and gender on alcohol treatment utilization among Whites, Blacks, and Hispanics with a lifetime AUD. Among men, Hispanics less likely to use specialty treatment and Alcoholics Anonymous (AA) than Whites. Among women, Blacks and Hispanics utilized any services, specialty treatment, and AA less than Whites. Weisner et al. (2002) analyzed data from a Northern California county and reported that compared to Whites, Blacks were almost three times more likely to have received treatment and Hispanics were half as likely. Oleski et al. (2010) also reported that Blacks and Hispanics with a lifetime AUD were about 1.7 times more likely than Whites to seek help. In contrast, Alvanzo et al. (2010) reported null findings for differences in time between first drink and alcohol-related service use across Whites, Blacks, and Hispanics. With regard to Hispanics, Zemore et al. (2009) reported a rate of lifetime utilization among individuals with a lifetime AUD of 19.2%, but most included utilization of self-help groups and not specialty treatment. Hispanics who were less acculturated were less likely to use treatment than those highly acculturated.
Utilizing data from the AI-SUPERPFP, Beals et al. (2005) reported rates of lifetime help-seeking for American Indians with a diagnosis of lifetime SUD from two geographical populations: the Southwest and Northern Plains. The rate for help-seeking was 55.8% for those in the Southwest and 40.1% for those in the Northern Plains. A considerable proportion of help (37.7% Southwest Tribe; 16.9% Northern Plains Tribes) was sought from traditional healers; demonstrating that many American Indians seek both Western and traditional healing modalities. Comparing lifetime help-seeking in these two American Indian groups with national data, Beals et al. (2003) reported higher rates for help-seeking from specialty providers for American Indians (16.4% and 18.9%) than for the U.S. national sample (7.8%).
These data indicate that admission to alcohol treatment is complex and is dependent on the presence and severity of alcohol problems but also on a variety of other factors. These include individuals’ sociodemographic characteristics, the availability of appropriate services, factors that may trigger coercion into treatment by family, friends, employers and the legal system, and the overall organization of the treatment system.
A full understanding of access to and utilization of treatment among different racial/ethnic groups requires consideration of the characteristics of the SUD being treated, the individual to be treated, and the characteristics of the treatment system. Results on need and utilization of treatment by racial/ethnic minorities depend on the settings and modalities of treatment and the time frame under consideration for the receipt of treatment. For immigrant groups, the availability of culturally and linguistically appropriate services is crucial in determining utilization. Making generalizations about which racial/ethnic group is over- or underrepresented in treatment generally, and by modality or setting, is difficult. This is true for those racial/ethnic groups for which data on need and utilization are available, Whites, Blacks, Hispanics, and to a lesser extent, American Indians/Alaskan Natives, as well as for groups that have not been the focus of much research: Asian Americans and Pacific Islanders. Consequently, more research is needed to understand facilitators and barriers to treatment to improve access to services and support.
Directions for Future Research
The path ahead for research with racial/ethnic minority groups presents both challenges and opportunities. Given that many racial/ethnic groups are also immigrants, future research opportunities include both a better understanding of the characteristics of immigration and life upon arrival to the U.S. for immigrants. There are also research opportunities that focus on non-immigrant groups such as Blacks and American Indians/Alaskan Natives. This research should be guided by multiple theoretical frameworks based on specific disciplinary perspectives. Several areas of inquiry are important to all racial/ethnic groups, such as those focusing on psychological risk factors and socioeconomic status. Others, given the cultural and historical diversity of these groups are specific, for example, developing a better understanding of the influence of historical trauma and racism among American Indians/Alaska Natives and Blacks.
Future research requires many foci in order to identify risk and protective factors at both personal and environmental levels. For instance, there have been considerable advances in understanding how the neighborhood environment exacerbates risk behavior (e.g., residential segregation and disadvantage; Mason et al., 2011; Cooper et al., 2007; Williams and Collins, 2001; Acevedo-Garcia et al., 2003; Karriker-Jaffe et al., 2012; Mulia and Karriker-Jaffe, 2012; Cerdá et al., 2010; Karriker-Jaffe, 2013; Jason et al., 2001). There is also an increased understanding of the potentially protective effects of neighborhoods such as social cohesion, social support, and collective efficacy (Hong et al., 2014; Shell et al., 2013; Frank et al., 2007; Vega et al., 2011). But further knowledge is needed to fully understand how these neighborhood factors interact with personal characteristics across racial/ethnic groups to increase or decrease risk for drinking and problems. Personal ecologies (i.e., interactions with different actors in different drinking related settings, such as at home, bars, or parties, can also bring risk or protection; Gruenewald 2007). Personal behaviors, alcohol availability, and the defining characteristics of these settings can influence drinking and an increased understanding of these factors is needed. It is likely that moderating effects of race/ethnicity on these associations will exist.
Research directions such as those outlined above often demand testing of hypotheses about complex systems of associations, which may require large samples as well as longitudinal studies with multiple points of measurement. Such research endeavors, however, are costly. At a time of reducing National Institutes of Health budgets, the tension between the costs of studying larger and more representative samples of diverse racial/ethnic groups, and more economically efficient and smaller but non-representative samples is quite real. The path ahead calls for a variety of methodological strategies to further advance research. Mobile device-based data collection offers a strategy that is both effective and economic. Online data collection with a first stage of randomly selected panels of respondents also offer economic advantages over face-to-face and telephone interviewing. Some U.S. racial/ethnic groups are relatively large (e.g., Blacks, Hispanics and Whites). But even such groups are not randomly distributed across the U.S. For instance, in spite of growing numbers and dispersion, Mexican Americans are still largely concentrated in the Southwest (Pew Research Center, 2014). Focusing data collection with this group in large Southwestern cities and some carefully selected rural areas can answer research questions with generalizability and can provide important results for local public health officials. Such a strategy can be similarly applied to research on other Hispanic and Asian national groups, Pacific Islanders, Native Americans, and Alaskan Natives.
While the primary thinking behind these suggestions has been guided by the epidemiological research reviewed herein, many concerns and solutions apply to clinical studies of treatment access and utilization, or lack thereof, and treatment efficacy and effectiveness. Here too, there are general themes that cut across racial/ethnic groups (e.g., certain treatment barriers) and that co-exist with group specific questions. While the study of national samples is informative for the country as a whole, data at the local level are also less costly to collect and, and will provide information about local populations This, of course, is of great value for treatment providers and public health authorities.
Acknowledgments
Funding:
Work on this paper was supported by grant (RO1-AA020542) from the National Institute on Alcohol Abuse and Alcoholism to the Pacific Institute for Research and Evaluation.
Contributor Information
Patrice A.C. Vaeth, Prevention Research Center, Pacific Institute for Research and Evaluation, Oakland, CA, USA
Meme Wang-Schweig, Prevention Research Center, Pacific Institute for Research and Evaluation, Oakland, CA, USA
Raul Caetano, Prevention Research Center, Pacific Institute for Research and Evaluation, Oakland, CA, USA and The University of Texas School of Public Health, Dallas Regional Campus, Dallas, TX, USA
References
- Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: A multilevel approach. Am J Public Health. 2003;93:215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alba R, Deane G, Denton N, Disha I, Mckenzie B, Napierala J. The role of immigrant enclaves for Latino residential inequalities. J Ethn Migr Stud. 2014;40:1–20. doi: 10.1080/1369183X.2013.831549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen CN, Meng XL. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvanzo AA, Storr CL, La Flair L, Green KM, Wagner FA, Crum RM. Race/ethnicity and sex differences in progression from drinking initiation to the development of alcohol dependence. Drug Alcohol Depend. 2011;118:375–382. doi: 10.1016/j.drugalcdep.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez KJ, Levy BR. Health advantages of ethnic density for African American and Mexican American and Mexican American elderly individuals. Am J Public Health. 2012;102:2240–2242. doi: 10.2105/AJPH.2012.300787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, Grube JW, Hill L, Holder H, Homel R. Research and Public Policy. Oxford University Press; Oxford: 2010. Alcohol: No Ordinary Commodity. [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Arch Gen Psychiatr. 2005;62:99–108. doi: 10.1001/archpsyc.62.1.99. [DOI] [PubMed] [Google Scholar]
- Beals J, Spicer P, Mitchell CM, Novins DK, Manson SM, Big Crow CK, Buchwald D, Chambers B, Christensen ML, Dillard DA, Dubray K, Espinoza PA, Fleming CM, Frederick AW, Gurley D, Jervis LL, Jim SM, Kaufman CE, Keane EM, Klein SA, Lee D, McNulty MC, Middlebrook DL, Moore LA, Nez TD, Norton IM, Orton HD, Randall CJ, Sam A, Shore JH, Simpson SG, Yazzie LL. Racial disparities in alcohol use: Comparison of 2 American Indian reservation populations with national data. Am J Public Health. 2003;93:1683–1685. doi: 10.2105/ajph.93.10.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place. 2009;15:700–708. doi: 10.1016/j.healthplace.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Bécares L, Shaw R, Nazroo J, Stafford M, Albor C, Atkin K, Kiernan K, Wilkinson R, Pickett K. Ethnic density effects on physical morbidity, mortality, and health behaviors: a systematic review of the literature. Am J Public Health. 2012;102:e33–e66. doi: 10.2105/AJPH.2012.300832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berke EM, Tanski SE, Demidenko E, Alford-Teaster J, Shi X, Sargent JD. Alcohol retail density and demographic predictors of health disparities: A geographic analysis. Am J Public Health. 2010;100:1967–1971. doi: 10.2105/AJPH.2009.170464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein KT, Galea S, Ahern J, Tracy M, Vlahov D. The built environment and alcohol consumption in urban neighborhoods. Drug Alcohol Depend. 2007;91:244–252. doi: 10.1016/j.drugalcdep.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Berry JW. Acculturation: Living successfully in two cultures. Int J Intercult Relat. 2005;29:697–712. [Google Scholar]
- Borges G, Medina-Mora ME, Lown A, Ye Y, Robertson MJ, Cherpitel C, Greenfield T. Alcohol use disorders in national samples of Mexicans and Mexican-Americans: The Mexican National Addiction Survey and the U.S. National Alcohol Survey. Hisp J Behav Sci. 2006;28:425–449. [Google Scholar]
- Borrell LN, Diez-Roux AV, Jacobs DR, Shea S, Jackson SA, Shrager S, Blumenthal RS. Perceived racial/ethnic discrimination, smoking and alcohol consumption in the Multi-Ethnic Study of Atherosclerosis (MESA) Prev Med. 2010;51:307–312. doi: 10.1016/j.ypmed.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell LN, Kiefe CI, Diez-Roux AV, Williams DR, Gordon-Larsen P. Racial discrimination, racial/ethnic segregation and health behaviors in the CARDIA Study. Ethn Health. 2013;18:227–243. doi: 10.1080/13557858.2012.713092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Chang DF. Psychiatric disorders among foreign-born and US-born Asian-Americans in a U.S. national survey. Soc Psychiatry Psychiatr Epidemiol. 2006;41:943–50. doi: 10.1007/s00127-006-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E, Gallo LC, Myers HF. Race, racism and health: disparities, mechanisms, and interventions. J Behav Med. 2009;32:1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- Brenner AB, Diez Roux AV, Barrientos-Gutierrez T, Borrell LN. Associations of alcohol availability and neighborhood socioeconomic characteristics with drinking: Cross-sectional results from the Multi-ethnic Study of Atherosslerosis (MESA) Subst Use Misuse. 2015;50:1606–1617. doi: 10.3109/10826084.2015.1027927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Indian Affairs. [Accessed 09/12/2016];Federal and State Recognized Tribes. 2016 Available at: http://www.ncsl.org/research/state-tribal-institute/list-of-federal-and-state-recognized-tribes.aspx.
- Caetano R, Baruah J, Ramisetty-Mikler S, Ebama MS. Sociodemographic predictors of pattern and volume of alcohol consumption across Hispanics, Blacks, and Whites: 10-year trend (1992–2002) Alcoh Clin Exp Res. 2010;34:1782–1792. doi: 10.1111/j.1530-0277.2010.01265.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): The association between birthplace, acculturation and alcohol abuse and dependence across Hispanic national groups. Drug Alcohol Depend. 2009;99:215–221. doi: 10.1016/j.drugalcdep.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Vaeth PAC, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): Acculturation. birthplace and alcohol-related social problems across Hispanic national groups. Hisp J Behav Sci. 2012;31:95–117. doi: 10.1177/0739986311424040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Clark CL. Accculturation, alcohol consumption, smoking, and drug use among Hispanics. In: Chun KM, editor. Acculturation: Advances in Theory, Measurement, and Applied Research. American Psychological Association; Washington, D.C: 2003. pp. 223–239. [Google Scholar]
- Canino G, Vega WA, Sribney WM, Warner LA, Alegría M. Social relationships, social assimilation, and substance use disorders among adult Latinos in the U.S. J Drug Issues. 2008;38:69–101. doi: 10.1177/002204260803800104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed 07/25/2016];Alcohol Related Disease Impact (ARDI) Application. 2013 Available at: www.cdc.gov/ARDI.
- Cerdá M, Diez-Roux AV, Tchetgen Tchetgen E, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: Estimation by marginal structural models. Epidemiology. 2010;21:482–489. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey JC, Stoddard AM, Krieger N. Alcohol disorders among Asian Americans: associations with unfair treatment, racial/ethnic discrimination, and ethnic identification (the National Latino and Asian Americans Study, 2002–2003) J Epidemiol Community Health. 2008;62:973–979. doi: 10.1136/jech.2007.066811. [DOI] [PubMed] [Google Scholar]
- Chartier KG, Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Res Health. 2010;33:152–160. [PMC free article] [PubMed] [Google Scholar]
- Collins SE. Associations between socioeconomic factors and alcohol outcomes. Alcohol Res. 2016;38:83–94. doi: 10.35946/arcr.v38.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coohey C. The relationship between familism and child maltreatment in Latino and Anglo families. Child Maltreat. 2001;6:130–142. doi: 10.1177/1077559501006002005. [DOI] [PubMed] [Google Scholar]
- Cook WK, Bond J, Karriker-Jaffe KJ, Zemore S. Who’s at risk? Ethnic drinking cultures, foreign nativity, and problem drinking among Asian American young adults. J Stud Alcohol Drugs. 2013;74:532–541. doi: 10.15288/jsad.2013.74.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook WK, Caetano R. Ethnic drinking cultures, gender, and socioeconomic status in Asian American and Latino drinking. Alcohol Clin Exp Res. 2014;38:3043–3051. doi: 10.1111/acer.12573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook WK, Karriker-Jaffe KJ, Bond J, Lui C. Asian American problem drinking trajectories during the transition to adulthood: Ethnic drinking cultures and neighborhood contexts. Am J Public Health. 2015;105:1020–1027. doi: 10.2105/AJPH.2014.302196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook WK, Mulia N, Karriker-Jaffe K. Ethnic drinking cultures and alcohol use among Asian American adults: findings from a national survey. Alcohol Alcohol. 2012;47:340–348. doi: 10.1093/alcalc/ags017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Friedman SR, Tempalski B, Friedman R. Residential segregation and injection drug use prevalence among Black adults in US metropolitan areas. Am J Public Health. 2007;97:344–352. doi: 10.2105/AJPH.2005.074542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JK, Solomin TA, Muramoto ML. Alcohol use among Native Americans compared to whites: Examining the veracity of the “Native American elevated alcohol consumption” belief. Drug Alcohol Depend. 2016;160:65–75. doi: 10.1016/j.drugalcdep.2015.12.015. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Saha TD, Grant BF. Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug Alcohol Depend. 2015;148:56–61. doi: 10.1016/j.drugalcdep.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denny CH, Holtzman D, Cobb N. Surveillance for health behaviors of American Indians and Alaska Natives. Findings from the Behavioral Risk Factor Surveillance System, 1997–2000. MMWR. 2003;52:1–13. [PubMed] [Google Scholar]
- Factor R, Williams DR, Kawachi I. Social resistance framework for understanding high-risk behavior among nondominant minorities: Preliminary evidence. Am J Public Health. 2013;103:2245–2251. doi: 10.2105/AJPH.2013.301212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Factor R, Kawachi I, Williams DR. Understanding high-risk behavior among non-dominant minorities: A social resistance framework. Soc Sci Med. 2011;73:1292–1301. doi: 10.1016/j.socscimed.2011.07.027. [DOI] [PubMed] [Google Scholar]
- Foster WM, Sharp RR. Beyond race: toward a whole-genome perspective on human populations and genetic variation. Nature Reviews Genetics. 2004;5(10):790–796. doi: 10.1038/nrg1452. [DOI] [PubMed] [Google Scholar]
- Frank R, Cerdá M, Rendon M. Barrios and burbs: residential context and health-risk behaviors among Angeleno adolescents. J Health Soc Behav. 2007;48:283–300. doi: 10.1177/002214650704800306. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban Neighborhood Poverty and the Incidence of Depression in a Population-Based Cohort Study. Ann Epidemiol. 2007;17:171–179. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Delva J, Takeuchi DT. Relationships between self-reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. Am J Public Health. 2007;97:933–940. doi: 10.2105/AJPH.2005.075739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert PA, Zemore SE. Discrimination and drinking: A systematic review of the evidence. Soc Sci Med. 2016;161:178–194. doi: 10.1016/j.socscimed.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ. The spatial ecology of alcohol problems: Niche theory and assortative drinking. Addiction. 2007;102:870–878. doi: 10.1111/j.1360-0443.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- Hackbarth DP, Schnopp-Wyatt D, Katz D, Williams J, Silvestri B, Pfleger M. Collaborative research and action to control the geographic placement of outdoor advertising of alcohol and tobacco products in Chicago. Public Health Rep. 2001;116:558–567. doi: 10.1016/S0033-3549(04)50088-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong S, Zhang W, Walton E. Neighborhoods and mental health: Exploring ethnic density, poverty, and social cohesion among Asian Americans and Latinos. Soc Sci Med. 2014;111:117–124. doi: 10.1016/j.socscimed.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, Frank RG. The Affordable Care Act will revolutionize care for substance use disorders in the United States. Addiction. 2014;109:1957–1958. doi: 10.1111/add.12606. [DOI] [PubMed] [Google Scholar]
- Iceland J, Nelson KA. Hispanic segregation in metropolitan America: Exploring the multiple forms of spatial assimilation. Am Sociol Rev. 2008;73:741–765. [Google Scholar]
- Iwamoto DK, Kaya A, Grivel M, Clinton L. Under-researched demographics: Heavy episodic drinking and alcohol-related problems among Asian Americans. Alcohol Res. 2016;38:17–25. doi: 10.35946/arcr.v38.1.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jargowsky PA. Immigrants and neighbourhoods of concentrated poverty: Assimilation or stagnation? J Ethn Migr Stud. 2009;35:1129–1151. [Google Scholar]
- Jason DB, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42:151–165. [PubMed] [Google Scholar]
- Jetelina KK, Reingle Gonzalez JM, Vaeth PAC, Mills BA, Caetano R. An investigation of the relationship between alcohol use and major depressive disorder across Hispanic national groups. Alcohol Clin Exp Res. 2016;40:536–542. doi: 10.1111/acer.12979. [DOI] [PubMed] [Google Scholar]
- Karriker-Jaffee KJ, Liu H, Kaplan LM. Understanding associations between neighborhood socioeconomic status and negative consequences of drinking: A moderated mediation analysis. Prev Sci. 2016;17:513–524. doi: 10.1007/s11121-016-0641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffee KJ, Zemore SE, Mulia N, Jones-Webb R, Bond J, Greenfield TK. Neighborhood disadvantage and adult alcohol outcomes: Differential risk by race and gender. J Stud Alcohol Drugs. 2012;73:865–873. doi: 10.15288/jsad.2012.73.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffee KJ. Neighborhood socioeconomic status and substance use by U.S. adults. Drug Alcohol Depend. 2013;133:212–221. doi: 10.1016/j.drugalcdep.2013.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ. Areas of disadvantage: A systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug Alcohol Rev. 2011;30:84–95. doi: 10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Alberti P, Narrow WE, Grant BF, Hasin DS. Service utilization differences for Axis 1 psychiatric and substance use disorders between White and Black adults. Psychiatr Serv. 2008;59:893–901. doi: 10.1176/appi.ps.59.8.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Grant BF, Hasin DS. Stress and alcohol: Epidemiologic evidence. Alcohol Res. 2012;34:391–400. doi: 10.35946/arcr.v34.4.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. 2011;218:1–17. doi: 10.1007/s00213-011-2236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss MP, Yuan NP, Dightman D, Prince RJ, Polacca M, Sanderson B, Goldman D. Adverse childhood exposures and alcohol dependence among seven Native American tribes. Am J Prev Med. 2003;25:238–244. doi: 10.1016/s0749-3797(03)00195-8. [DOI] [PubMed] [Google Scholar]
- Kwate NO. Take one down, pass it around, 98 alcohol ads on the wall: Outdoor advertising in New York City’s Black neighbourhoods. Int J Epidemiol. 2007;36:988–990. doi: 10.1093/ije/dym117. [DOI] [PubMed] [Google Scholar]
- Kwate NO, Lee TH. Ghettoizing outdoor advertising: Disadvantage and ad panel density in Black neighborhoods. J Urban Health. 2007;84:21–31. doi: 10.1007/s11524-006-9127-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Wallace JM. Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51:613–617. doi: 10.1016/s0277-9536(00)00004-6. [DOI] [PubMed] [Google Scholar]
- Lee HK, Han B, Gfroerer JC. Differences in the prevalence rates and correlates of alcohol use and binge alcohol use among five Asian American subpopulations. Addict Behav. 2013;38:1816–1823. doi: 10.1016/j.addbeh.2012.11.001. [DOI] [PubMed] [Google Scholar]
- Lee CA, Colby SM, Rohsenow DJ, Lopez SR, Hernandez L, Caetano R. Acculturstion stress and drinking problems among urban heavy drinking Lationo in the Northeast. J Ethn Subst Abuse. 2013;12:308–320. doi: 10.1080/15332640.2013.830942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MA, Ferraro KF. Neighborhood residential segregation and physical health among Hispanic Americans: Good, bad, or benign? J Health Soc Behav. 2007;48:131–148. doi: 10.1177/002214650704800203. [DOI] [PubMed] [Google Scholar]
- Lo CC, Cheng TC, Howell RJ. The role of immigration status in heavy drinking among Asian Americans. Subst Use Misuse. 2014;49:932–940. doi: 10.3109/10826084.2013.852578. [DOI] [PubMed] [Google Scholar]
- Markides KS, Snih SA, Walsh T, Cutchin M, Ju H, Goodwin JS. Problem drinking among Mexican Americans: The influence of nativity and neighborhood context? Am J Health Promot. 2012;26:225–229. doi: 10.4278/ajhp.100510-QUAN-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsiglia FF, Parsai M, Kulis S. Effects of familismo and family cohesion on problem behaviors among adolescents in Mexican immigrant families in the southwest United States. J Ethn Cult Divers Soc Work. 2009a;18:203–220. doi: 10.1080/15313200903070965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsiglia FF, Kulis S, Parsai M, Villar P, Garcia C. Cohesion and conflict: Family influences on adolescent alcohol use in immigrant Latino families. J Ethn Subst Abuse. 2009b;8:400–412. doi: 10.1080/15332640903327526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JK, Tuch SA, Roman PM. Problem drinking patterns among African Americans: the impacts of reports of discrimination, perceptions of prejudice, and “risky” coping strategies. J Health Soc Behav. 2003;44:408–425. [PubMed] [Google Scholar]
- Mason SM, Kaufhan JS, Daniels JL, Emch ME, Hogan VK, Savitz DA. Neighborhood ethnic density and preterm birth across seven ethnic groups in New York City. Health Place. 2011;17:280–288. doi: 10.1016/j.healthplace.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey DS. Residential segregation and neighborhood conditions in U.S. metropolitan areas. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America Becoming: Racial Trends and Their Consequences. Vol. 1. National Academies Press; Washington, D.C: 2001a. pp. 391–434. [Google Scholar]
- Massey DS. In: Segregation and violent crime in urban America. Problem of the Century: Racial Stratification in the United States. Anderson E, Massey DS, editors. Russell Sage Foundation; New York: 2001b. pp. 317–346. [Google Scholar]
- Masson CL, Shopshire MS, Sen S, Hoffman KA, Hengl NS, Bartolome J, McCarty D, Sorensen JL, Iguchi MY. Possible barriers to enrollment in substance abuse treatment among a diverse sample of Asian Americans and Pacific Islanders: Opinions of treatment clients. J Subst Abuse Treat. 2013;44:309–315. doi: 10.1016/j.jsat.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson FI, Moineddin R, Dunn JR, Creatore MI, Gozdyra P, Glazier RH. Urban neighborhoods, chronic stress, gender and depression. Soc Sci Med. 2006;63:2604–2616. doi: 10.1016/j.socscimed.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Mills BA, Caetano R. Decomposing associations between acculturation and drinking in Mexican Americans. Alcohol Clin Exp Res. 2012;36:1205–1211. doi: 10.1111/j.1530-0277.2011.01712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina KM, Alegria M, Chen CN. Neighborhood context and substance use disorders: A comparative analysis of racial and ethnic groups in the United States. Drug Alcohol Depend. 2012;125S:S35–S43. doi: 10.1016/j.drugalcdep.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Karriker-Jaffe KJ. Interactive influences of neighborhood and individual socioeconomic status on alcohol consumption and problems. Alcohol Alcohol. 2012;47:178–186. doi: 10.1093/alcalc/agr168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among Black, Hispanic, and White Americans: Findings from the 2005 U.S. National Alcohol Survey. J Stud Alcohol Drugs. 2008;69:824–833. doi: 10.15288/jsad.2008.69.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Greenfield TK, Zemore SE. Disparities in alcohol-related problems among White, Black, and Hispanic Americans. Alcohol Clin Exp Res. 2009;33:654–662. doi: 10.1111/j.1530-0277.2008.00880.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Zemore SE. Social adversity, stress, and alcohol problems: Are racial/ethnic minorities and the poor more vulnerable? J Stud Alcohol Drugs. 2012;73:570–580. doi: 10.15288/jsad.2012.73.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- Novins DK, Aarons GA, Conti SG, Dahlke D, Daw R, Fickenscher A, Fleming C, Love C, Masis K, Spicer P for the Centers for American Indian and Alaska Native Health’s Substance Abuse Treatment Advisory Board. Use of evidence base in substance abuse treatment programs for American Indians and Alaska Natives: Pursuing quality in the crucible of practice and policy. Implement Sci. 2011;6:63. doi: 10.1186/1748-5908-6-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell JM, Novins DK, Beals J, Spicer P. Disparities in Patterns of Alcohol Use Among Reservation-based and Geographically Dispersed American Indian Populations. Alcohol Clin Exp Res. 2005;29:107–116. doi: 10.1097/01.alc.0000153789.59228.fc. [DOI] [PubMed] [Google Scholar]
- Oleski J, Mota N, Cox BJ, Sareen J. Percecived need for care, help seeking, and perceived barrieers to care for alcohol use disorders in a national sample. Psychiatr Serv. 2010;61:1223–1231. doi: 10.1176/ps.2010.61.12.1223. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Eschbach K, Markides KS, Goodwin JS. Neighbourhood composition and depressive symptoms among older Mexican Americans. J Epidemiol Community Health. 2003;57:987–992. doi: 10.1136/jech.57.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otiniano Verissimo AD, Gee GC, Ford CL, Iguchi MY. Racial discrimination, gender discrimination, and substance abuse among Latina/os nationwide. Cultur Divers Ethnic Minor Psychol. 2014;20:43–51. doi: 10.1037/a0034674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SY, Anastas J, Shibusawa T, Nguyen D. The impact of acculturation and acculturative stress on alcohol use across Asian immigrant subgroups. Subst Use Misuse. 2014;49:922–31. doi: 10.3109/10826084.2013.855232. [DOI] [PubMed] [Google Scholar]
- Patel KV, Eschbach K, Rudkin LL, Peek MK, Markides KS. Neighborhood context and self-rated health in older Mexican Americans. Ann Epidemiol. 2003;13:620–628. doi: 10.1016/S1047-2797(03)00060-7. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. [Accessed 09/16/2016];Mapping the nation’s Latino population: By state, county and city. 2014 Available at: http://www.pewhispanic.org/packages/latinos-by-geography/
- Pickett KE, Wilkinson RG. People like us: Ethnic group density effects on health. Ethn Health. 2008;13:321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighborhood socioeconomic context and health outcomes: A critical review. J Epidemiol Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramisetty-Mikler S, Caetano R, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): Alcohol consumption and sociodemographic predictors across Hispanic national groups. J Subst Use. 2010;15:402–416. doi: 10.3109/14659891003706357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Rios-Bedoya CF, Freile-Salinas D. Incidence of alcohol use disorders among Hispanic subgroups in the USA. Alcohol Alcoholism. 2014;49:549–556. doi: 10.1093/alcalc/agu032. [DOI] [PubMed] [Google Scholar]
- Rivera FI, Guarnaccia PJ, Mulvaney-Day N, Lin JY, Torres M, Alegria M. Family cohesion and its relationship to psychological distress among Latino groups. Hisp J Behav Sci. 2008;30:357–378. doi: 10.1177/0739986308318713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romley JA, Cohen D, Ringel J, Sturm R. Alcohol and environmental justice: the density of liquor stores and bars in urban neighborhoods in the United States. J Stud Alcohol Drugs. 2007;68:48–55. doi: 10.15288/jsad.2007.68.48. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Kagotho N, Vaughn MG. Mood, anxiety, and personality disorders among first and second-generation immigrants to the United States. Psychiatry Res. 2014a;220:1028–1036. doi: 10.1016/j.psychres.2014.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Clark TT, Terzis LD, Córdova D. Substance use disorders among first- and second-generation immigrant adults in the United States: Evidence for an immigrant paradox. J Stud Alcohol Drugs. 2014b;75:958–967. doi: 10.15288/jsad.2014.75.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. Results from the 2011 National Survey on Drug Use and Health: Detailed Tables, Figure 3.1. Rockville, MD: U. S. Department of Health and Human Services; 2012a. [Google Scholar]
- SAMHSA. Series The NSDUH Report: Need for and receipt of substance use treatment among Hispanics. Rockville, MD: 2012b. The NSDUH Report: Need for and receipt of substance use treatment among Hispanics. [Google Scholar]
- SAMHSA. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: U.S. Department of Health and Human Services; 2014a. [Google Scholar]
- SAMHSA. Treatment Episode Data set (TEDS): 2002–2012. National Admission to Substance Abuse Treatment Services; Rockville, MD: 2014b. BHSIS Series S-71. [Google Scholar]
- SAMSHA. [Accessed 03/09/2016];Results from the 2014 National Survey on Drug Use and Health: Detailed tables. 2015a Available at: http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2014/NSDUH-DetTabs2014.pdf.
- SAMHSA. Behavioral Health Equity Barometer: United States, 2014. Rockville, MD: 2015b. [Accessed 03/08/2016]. Available at: http://www.samhsa.gov/data/sites/default/files/Health_Equity_National_BHB_1-27-16_508.pdf. [Google Scholar]
- Santiago AM. Patterns of Puerto Rican segregation and mobility. Hisp J Behav Sci. 1992;14:107–133. [Google Scholar]
- Schmidt L, Ye Y, Greenfield TK, Bond J. Ethnic disparities in clinical severity and services for alcohol problems: results from the National Alcohol Survey. Alcohol Clin Exp Res. 2007;31:48–56. doi: 10.1111/j.1530-0277.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- Shell AM, Peek MK, Eschbach K. Neighborhood Hispanic composition and depressive symptoms among Mexican-descent residents of Texas City, Texas. Soc Sci Med. 2013;99:56–63. doi: 10.1016/j.socscimed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- Spicer P, Beals J, Croy CD, Mitchell CM, Novins DK, Moore L, Manson SM The American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project Team. The prevalence of DSM-III-R alcohol dependence in two American Indian populations. Alcohol Clin Exp Res. 2003;27:1785–1797. doi: 10.1097/01.ALC.0000095864.45755.53. [DOI] [PubMed] [Google Scholar]
- Spicer P, Bezdek M, Manses SM, Beals J. A program of research on spirituality and American Indian alcohol use. South Med. 2007;100:430–432. doi: 10.1097/SMJ.0b013e318031715c. [DOI] [PubMed] [Google Scholar]
- Stafford M, Bécares L, Nazroo J. Ethnicity and Integration. Springer; 2010. Racial discrimination and health: Exploring the possible protective effects of ethnic density. [Google Scholar]
- Steele CB, Cardinez CJ, Richardson LC, Tom-Orme L, Shaw KM. Surveillance for health behaviors of American Indians and Alaska Natives - Findings from the Behavioral Risk Factor Surveillance System, 2000–2006. Cancer. 2008;113:1131–1141. doi: 10.1002/cncr.23727. [DOI] [PubMed] [Google Scholar]
- Stroope S, Martinez BC, Eschbach K, Peek MK, Markides KS. Neighborhood ethnic composition and problem drinking among older Mexican American men: Results from the Hispanic Established Populations For The Epidemiologic Study Of The Elderly. J Immigr Minor Health. 2015;17:1055–1060. doi: 10.1007/s10903-014-0033-8. [DOI] [PubMed] [Google Scholar]
- Szaflarski M, Cubbins LA, Ying J. Epidemiology of alcohol abuse among US immigrant populations. J Immigr Minor Health. 2011;13:647–658. doi: 10.1007/s10903-010-9394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran AG, Lee RM, Burgess DJ. Perceived discrimination and substance use in Hispanic/Latino, African-born Black, and Southeast Asian immigrants. Cultur Divers Ethnic Minor Psychol. 2010;16:226–236. doi: 10.1037/a0016344. [DOI] [PubMed] [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. J Ment Health Policy Econ. 2006;9:137–154. [PubMed] [Google Scholar]
- Vaeth PA, Caetano R, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): The association between acculturation, birthplace and alcohol consumption across Hispanic national groups. Addict Behav. 2012;37:1029–1037. doi: 10.1016/j.addbeh.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Ang A, Rodriguez MA, Finch BK. Neighborhood protective effects on depression in Latinos. Am J Commun Psychol. 2011;47:114–126. doi: 10.1007/s10464-010-9370-5. [DOI] [PubMed] [Google Scholar]
- Vega WA, Sribney WM, Achara-Abrahams I. Co-Occurring Alcohol, Drug, and Other Psychiatric Disorders Among Mexican-Origin People in the United States. Am J Public Health. 2003;93:1057–1064. doi: 10.2105/ajph.93.7.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31:99–112. doi: 10.1093/epirev/mxp008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venner KL, Greenfield BL, Hagler KJ, Simmons L, Lupee D, Homer E, Yamutewa Y, Smith JE. Pilot outcome results of culturally adapted evidence-based substance use disorder treatment with a Southwest tribe. Addict Behav Rep. 2016;3:21–27. doi: 10.1016/j.abrep.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl AMG, Breckenridge RS, Gunkel SE. Latinos, residential segregation and spatial assimilation in micropolitan areas: Exploring the American dilemma on a new frontier. Soc Sci Res. 2007;36:995–1020. [Google Scholar]
- Weisner C, Matzger H, Tam T, Schmidt L. Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. J Stud Alcohol. 2002;63:673–682. doi: 10.15288/jsa.2002.63.673. [DOI] [PubMed] [Google Scholar]
- Weisner C, Schmidt LA. Rethinking access to alcohol treatment. Recent Dev Alcohol. 2001;15:107–136. doi: 10.1007/978-0-306-47193-3_7. [DOI] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Big Crow C, Mitchell CM, Novins DK. Am J Drug Alcohol Abuse. 2012;38:376–383. doi: 10.3109/00952990.2012.694527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt J, Mulia N, Zemore SE, Kerr WC. Racial/ethnic disparities in alcohol-related problems: Differences by gender and level of heavy drinking. Alcohol Clin Exp Res. 2014;38:1662–1670. doi: 10.1111/acer.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yudell M, Roberts D, DeSalle R, Tishkoff S. Taking race out of human genetics. Science. 2016;351:564–565. doi: 10.1126/science.aac4951. [DOI] [PubMed] [Google Scholar]
- Zemore SE. Re-examining whether and why acculturation relates to drinking outcomes in a rigorous, national survey of Latinos. Alcohol Clin Exp Res. 2005;29:2144–2153. doi: 10.1097/01.alc.0000191775.01148.c0. [DOI] [PubMed] [Google Scholar]
- Zemore SE. Acculturation and alcohol among Latino adults in the United States: A comprehensive review. Alcohol Clin Exp Res. 2007;31:1968–1990. doi: 10.1111/j.1530-0277.2007.00532.x. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Mulia N, Yu Y, Borges G, Greenfield TK. Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three National Alcohol Surveys. J Subst Abuse Treat. 2009;36:446–456. doi: 10.1016/j.jsat.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Karriker-Jaffe KJ, Keithly S, Mulia N. Racial prejudice and unfair treatment: Interactive effects with poverty and foreign nativity on problem drinking. J Stud Alcohol Drugs. 2011;72:361–370. doi: 10.15288/jsad.2011.72.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Karriker-Jaffe KJ, Mulia N. Temporal trends and challenging racial/ethnic disparities in alcohol problems: Results from the 2000 to 2010 National Alcohol Surveys. J Addict Res Ther. 2013;4 doi: 10.4172/2155-6105.1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Murphy R, Mulia N, Gilbert PA, Martinez P, Bond J, Polcin DL. A moderating role for gender in racil/ethnic disparities in alcohol services utilization: Results from the 2000–2010 National Alcohol Surveys. Alcohol Clin Exp Res. 2014;38:2286–2296. doi: 10.1111/acer.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Ye Y, Mulia N, Martinez P, Jones-Webb R, Karriker-Jaffe K. Poor, persecuted, young, and alone: Toward explaining the elevated risk of alcohol problems among Black and Latino men who drink. Drug Alcohol Depend. 2016;163:31–39. doi: 10.1016/j.drugalcdep.2016.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]