Abstract
Objective
Insomnia is associated with increased risk for suicide. The Food and Drug Administration (FDA) has warnings regarding suicide in the prescribing information of hypnotics. We conducted a review of the evidence for and against hypnotics increasing the risk of suicide.
Method
This review focused on modern, FDA-approved hypnotics, beginning with the introduction of benzodiazepines, limiting its findings to adults. PubMed and Web of Science were searched, crossing the terms ‘suicide’ and ‘suicidal’ with each of the modern FDA-approved hypnotics. The FDA website was searched for post-marketing safety reviews, and the FDA was contacted to provide detailed case reports for hypnotic-related suicide deaths reported through its Adverse Event Report system.
Results
The epidemiological studies show that hypnotics are associated with increased risk for suicide. However, none of these studies adequately controlled for depression or other psychiatric disorders that may be linked with insomnia. Suicide deaths have been reported from single-agent hypnotic overdoses. A separate concern is that benzodiazepine receptor agonist hypnotics can cause parasomnias, which in rare cases may lead to suicidal ideation or suicidal behavior in persons who were not known to be previously suicidal. On the other hand, ongoing research is testing whether treatment of insomnia might reduce suicidality in depressed adults.
Conclusions
This review indicates hypnotic medications are associated with suicidal ideation. Future studies should be designed to assess both types of possible effects: 1) an increase in suicidality due to central nervous system impairments from a given hypnotic medication; and 2) a decrease in suicidality due to improving insomnia.
Introduction
A growing body of evidence has linked insomnia to suicidal ideation, suicidal behavior, and suicide death, herein referred to collectively as suicide.(1) Insomnia has had an evolving definition over the last 30 years, now defined as a complaint of inadequate duration or poor quality sleep, with adverse daytime consequences, despite adequate opportunity to sleep. (2;3) Insomnia often accompanies psychiatric disorders, but can also be related to chronic pain or other medical conditions.(3)The relationship between insomnia and suicide is maintained after controlling for symptoms of depressive illness.(4) It is not clear whether insomnia is causally related to suicide, or is an indicator for some other factor that drives the risk for suicide, such as Central Nervous System and psychological hyperarousal.(1)
The insomnia/suicide association suggests that treatment of insomnia would reduce the risk of suicide. This hypothesis is presently being tested in a multi-site, randomized clinical trial.(5) In the meantime, the proposition of routinely prescribing hypnotics to suicidal depressed patients is countered by the fact that hypnotics can be part of an intentional overdose, or may induce or aggravate suicide. The latter possibility has public health significance as 3% of non-institutionalized adult Americans reported using a hypnotic in the last month.(6) Up to 10% of adults in the USA use over the counter sleep aids,(7) but over the counter sleep aids have not been linked with suicide, carry no FDA warnings for suicide, and will not be considered further in this paper.
There have been prior reviews on the relationship between hypnotics and suicide. One study found increased rates of suicide death among hypnotic users, hypothesized to be due to impairment of judgment and promotion of violent/risky behaviors.(8) A review of ‘sedative/hypnotics’ similarly concluded that hypnotics could increase the risk of suicide through disinhibition, and that a definitive answer as to whether they increase or reduce risk requires trials specifically naming suicide as the primary outcome.(9) The most recent summary of this topic is a commentary on a single epidemiologic survey reviewed below.(10)
Based on the available reviews and epidemiologic surveys, the link between sedative/hypnotics and suicidality appears to be uncertain. However, no prior review considered the published case reports of suicide death as related to hypnotic medication, or considered the adverse event reports on suicide and hypnotics in the Food and Drug Administration’s (FDA’s) 2006 post-marketing safety review of zolpidem, zaleplon, and eszopiclone (the “Z-drugs”).(11)
Prior to 2006, the FDA had required that hypnotic package labels warn of the risk of prescribing hypnotics to severely depressed patients, “…particularly the recognition that suicidal tendencies may be present and protective measures may be necessary.”(Dalmane label). By 2006, the FDA expressed concern that there was an increased risk of suicide linked to the newer “Z-drugs.”(11) Correspondingly, the package labels for zolpidem, zaleplon and eszopiclone include: “In primarily depressed patients, worsening of depression, including suicidal thoughts and actions (including completed suicides), has been reported in association with the use of sedative/hypnotics.” The labels of hypnotics subsequently approved by the FDA (doxepin 3 mg and 6 mg and suvorexant) also include this same warning. However, the label of suvorexant, the agent most recently FDA-approved for insomnia treatment, also included a stronger statement: “in clinical studies, a dose-dependent increase in suicidal ideation was observed in patients taking Belsomra as assessed by questionnaires.” Ramelteon, doxepin 3 and 6 mg, and suvorexant have mechanisms of action different from benzodiazepine hypnotics and the Z-drugs, all of which are positive allosteric modulators of the gamma amino butyric acid (GABA) type A receptor at the benzodiazepine binding site. Hence an increased risk of suicide with ramelteon, doxepin, or suvorexant would signal a broader problem with hypnotics, beyond the GABA-ergic mechanism of benzodiazepines and Z-drugs.
These warnings have ambiguous implications. They could give the impression that all hypnotic prescriptions are associated with a significant risk of suicide, but don’t address whether suicide risk is elevated more with some hypnotics than others, or in depressed insomniacs versus non-depressed insomniacs. The warning also does not speak to the temporal association between hypnotic use and suicidality. For example, would risk be greater in the interval just after initiation of the prescription, but less so in the long term, or would risk be greater during the period of peak drug effect, and less so hours after significant drug metabolism has occurred?
We have conducted a review of the medical literature and FDA documents to provide greater clarity with respect to these possibilities. This review aims to describe: (1) the toxicology of hypnotics in the setting of suicide; (2) the epidemiologic relationship between hypnotic use and suicide; and (3) illustrative case data on hypnotics and suicide as found in the published literature and FDA databases that have generally not been included in published reviews of the relationship between sedative/hypnotic medications and suicidality.
Methods
This review focused on modern, FDA-approved hypnotics, beginning with the introduction of benzodiazepines, and excluding non-FDA-approved barbiturate hypnotics, ethchlorvynol and chloral hydrate. Therefore, the medications of principal interest are: flurazepam, temazepam, triazolam, estazolam, quazepam, zolpidem, zaleplon, eszopiclone, ramelteon, doxepin 3 and 6 mg, and suvorexant. This review is limited to adults 18 years and older, as there was insufficient information to form opinions regarding children and adolescents. The literature search process began with an inspection of the FDA-approved labeling of all of these agents, then proceeded to a PubMed search that crossed the terms ‘suicide’ and ‘suicidal’ with each of these agents. A similar process was undertaken with the Web of Science search engine, in hopes of locating relevant abstracts that might not be found in Pub Med. Next, the FDA website was searched for post-marketing safety reviews and for commentaries on adverse event reporting for each agent considered. The bibliographies of each document were examined for additional relevant citations. Finally, under the Freedom of Information Act, the FDA was contacted from December 2015 through February 2016 to provide detailed case reports for hypnotic-related suicide deaths reported through the FDA Adverse Event Report system, specifically for those medications that have no accounts published in the medical literature of suicide death by single agent overdose. The reports from the FDA spanned back to the 1970s in order to capture adverse events related to flurazepam and all subsequent FDA-approved hypnotics.
We note that meta-analysis, though preferred, could not be carried out because of the limitations of the available data, including few studies with the same types of design and non-uniformity in the types of outcomes reported.
RESULTS
Hypnotic Toxicology Studies in Suicide Victims
USA Studies
Our review found one hypnotic medication toxicology study from the USA. Toxicology findings of 187 consecutive suicide victims (137 men and 50 women; mean age 44) from the San Diego coroner’s office between 1981 and 1982 indicated that hypnotics were found in 10.7% of cases, and a third of those taking hypnotics also tested positive for alcohol.(12) There were no cases in which a benzodiazepine was the only drug detected and also judged to be the sole cause of death. The authors concluded that in cases of suicide related to benzodiazepines, multi-drug overdoses are of primary concern.
Studies outside of the USA
Our review found two hypnotic medication toxicology studies from outside the USA. A study of 1467 suicide deaths in Switzerland in 1990 reported 22 cases in which a benzodiazepine hypnotic was the single agent leading to a suicide poisoning (1.5% of all suicide deaths), including 16 with flunitrazepam, 2 with triazolam, and 4 with midazolam. (13) However, the authors conceded that the role of alcohol in these ‘single-agent’ cases may have been underestimated.
A second study of 2245 elderly suicides in 2003 through the Swedish Cause of Death Register found that 548 of the suicides were by poisoning, with benzodiazepines playing a role in 216 cases. A single benzodiazepine was the cause of death in 155 cases, and these included the hypnotics flunitrazepam (N=104), nitrazepam (N=36), and triazolam (N=1).(14) Upon reviewing all suicides in Sweden between 1992–1996, the authors found that after correcting for the differences in rates of prescribing for the hypnotics flunitrazepam, nitrazepam, zopiclone, and zolpidem, the associations between these 4 hypnotics and suicide were about the same, with approximately 1 suicide per million daily doses of each drug. Together, these toxicology studies show that modern hypnotics are often involved in suicide deaths, but usually are taken in combination with other sedatives or alcohol.
Retrospective Cohort Studies on the Topic of Hypnotics and Suicide
USA Studies
We found one retrospective cohort study from the USA. A secondary analysis of the National Comorbidity Survey Replication surveyed 5,692 randomly selected, community-dwelling adults between 2001–2003 with 5.8% of respondents answering ‘yes’ to a question inquiring about the use of sleeping pills such as Ambien or Sonata in the last 12 months.(15) Of these, 2.6% endorsed suicidal thinking in the last 12 months, 0.7% endorsed suicide plans, and 0.4% admitted to a suicide attempt. Hierarchical, multivariate logistic regression models, with suicidal thinking, plans, and behaviors as the dependent variables, and with hypnotic use as the independent variable adjusting for gender, age, ethnicity, marital status, education, poverty status, general health conditions, mood disorders, anxiety disorders, substance use disorders, and insomnia indicated odds ratios with 95% confidence intervals of 2.2 (1.5–3.3) for suicidal ideation, 1.9 (1.1–3.3) for suicide plan, and 3.4 (1.6–7.4) for a suicide attempt, as compared with those persons who did not use hypnotics. Strengths of this report include its representative sampling technique, large size, adjustment for insomnia, and inclusion of the Z-drugs. Weaknesses include lack of consideration of high-risk personality disorders, lack of measurement of the severity of depressive illness, the possibility of recollection bias, lack of measurement of completed suicide deaths, and a retrospective design that makes it impossible to understand the temporal association between hypnotic use and suicidal phenomena. Overall, the study adds credence to the idea that in some instances hypnotics might increase risk for suicide, but the study does not shed light on mechanism. The authors correctly point out that clinical trials are required to show causality between hypnotics and suicide. However, the authors calculated the sample size required to show a difference between hypnotics and placebo in rates of suicide attempts in a sample of insomniacs, and this calculation yielded a sample size of 1,068 participants (534 per group). It seems unlikely that such a large trial would ever be attempted; therefore there is justification for trials to detect a proxy risk factor such as suicidal ideation, rather than suicide attempts.
Studies outside of the USA
We discovered two retrospective case-control studies from outside the USA on the topic of suicide and hypnotics. A retrospective case-control study examined medications prescribed to 25 Finnish psychiatric inpatients who died by suicide during their hospitalization compared with 25 inpatient controls matched on age, gender, and psychiatric diagnosis (schizophrenia [n=14]; major depression [n=7]; personality disorder [n=3]; ‘neurosis’ [n=1]).(16) The suicide victims were more likely to be receiving a benzodiazepine (72%) as compared with the controls (44%), p<0.05. Limitations included lack of detail on whether the benzodiazepines were prescribed for anxiety or insomnia, lack of matching the groups on severity of symptoms, and small sample size.
The second study reported on the association between zolpidem and suicide (defined here as suicide death plus hospitalizations for suicide attempt) from a Taiwanese nationwide register covering 2002–2011. Each suicide case was matched on age, gender, occupation, and urban vs rural setting with 10 controls without history of suicide attempts.(17) The adjusted odds ratio for exposure to zolpidem was 2.08 (1.83–2.36) and remained significant regardless of whether depression, insomnia, anxiety, bipolar disorder or other comorbidities were present. However, the study was limited by imprecision in establishing the diagnoses of depression, insomnia and other mental disorders, and the lack of measurement of severity of symptoms between the cases and controls. The investigators speculated that zolpidem use could lead to a “dreamlike confusion state [that may] cause bizarre behavior [and] lead to potentially dangerous self-harm and even fatality.”
Prospective Cohort Studies Regarding Hypnotics and Suicide
USA Studies
Our review produced one prospective cohort study regarding hypnotics and suicide. The American Cancer Society evaluated frequency of “prescription sleeping pills” use in a convenience sample of 1,099,830 participants in 1982.(18) Respondents self-determined whether they were taking a “prescription sleeping pill” and hence the data likely mixed benzodiazepines with barbiturates and antidepressants. The sample was followed prospectively until 1986. Over this interval, adjusted hazard ratios for suicide were elevated in men (1.32) and women (1.22) who had nightly use of “prescription sleeping pills,” as compared with those who did not have nightly use of “sleeping pills” after controlling for body mass index, cigarette smoking, diet, and other mortality predictors. Apart from the non-representative nature of the sample and poor characterization of “prescription sleeping pills”, another weakness of the study included failure to take into account psychiatric diagnoses. The authors called for the measurement of suicidal ideation and behavior in clinical trials.
Studies outside of the USA
The review produced three prospective cohort studies from outside the USA that examined hypnotics and suicide. The first of these studies examined 26,952 adult Swedes between 1975 and 1981, 500 of whom (2%) were frequent hypnotic users (345 women, and 155 men), and tracked suicides until 1985 in the national Cause of Death Registry.(19) Subsequent suicides were found in 1.1% of hypnotic-treated women versus 0.1% of the women not taking hypnotics (OR=2.6, p<0.05). No men died by suicide. Study strengths include prospective measurement, which reduces ascertainment bias risk. Weaknesses include 1) inability to adequately control for depression diagnoses, other psychiatric disorders and insomnia, which are known risk factors for suicide, and 2) failure to define “hypnotics.”
In the second prospective cohort study, the rate of suicide attempts among benzodiazepine users was evaluated in persons enrolled in the Saskatchewan Health Data Bases.(20) The study compared 225,796 adults taking benzodiazepines (all new prescriptions from 1979–1986) and 97,862 age and gender-matched controls. The benzodiazepines included triazolam, flurazepam, lorazepam, diazepam and oxazepam. Those cases receiving an antidepressant concurrent with their benzodiazepine did not have increased suicide attempts or suicide death over the 60 days following filling a new benzodiazepine prescription vs controls. In contrast, cases not taking an antidepressant when filling their benzodiazepine prescription had six times the odds (OR=6.2; p<0.05) for suicide attempts or suicide death during the 60 days after filling their prescription versus controls. The authors speculated that “benzodiazepines may cause disinhibition, consisting of poor impulse control, and paradoxical reactions that may induce suicidal impulse.” Weaknesses of the study include the confounding of treatment (benzodiazepines and antidepressants) with diagnoses, as mood disorder diagnoses were not considered in the analyses.
In the third prospective cohort study, cause specific mortality was tracked for 20 years in a randomly selected sample of 1750 men and 1773 women who responded to a mail survey in Sweden in 1983 asking “how often do you use sleep medication?”. Data were collected regarding sleeping problems, medical diagnoses, depression, and body mass index.(21) There were 19 suicide deaths (10 men, 9 women). The adjusted hazard ratio for suicide among male regular hypnotic users was 21.2 (2.6–173.7), and the hazard ratio in women was 24.3 (4.4–132.2). Limitations include the small number of observed events, the lack of measurement of alcohol and substance abuse, and uncertainty as to what medications were being included among “sleep medications.” The authors concluded that regular hypnotic use is an indicator of increased risk of mortality, including suicide, but that the study design did not show causality. They called for clinical trials to clarify the directionality of these relationships.
Collectively, these prospective cohort studies show an association between hypnotic use and suicide, but all of these studies suffer from confounding of hypnotic use with psychiatric and substance abuse diagnoses.
Illustrative Cases on the Topic of Hypnotics and Suicide
Flurazepam (Original approval April 7, 1970)
The results of toxicology from a suicide were reported in which the only drug isolated was flurazepam, and post-mortem flurazepam blood concentration indicated ingestion of 80 30-mg tablets.(22) Alcohol was not involved.
A 52 year old woman with a history of depression and prior suicide attempts was found dead in her bed.(23) Toxicology on blood, urine, and bile indicated only the presence of flurazepam and no other drugs, poisons, or alcohol, and the equivalent of 20 30-mg flurazepam tablets in her stomach. A total of 70 flurazepam tablets were missing from a prescription filled 2 days prior.
A 68 year old woman was found dead at home with no evidence of trauma.(24) Her body was surrounded by empty medication boxes. Autopsy revealed no evidence of significant natural disease. Toxicology revealed a blood flurazepam level of 2.8 ug/mL. Other than a trace of alcohol in her blood (0.1 mg/mL), no other drugs were detected. The authors postulate the cause of death was respiratory depression due to a single-drug overdose from flurazepam.
Temazepam (Original approval February 27, 1981)
There are two published cases of suicide from temazepam as a single agent in the medical literature,(25;26) four cases reported by the Poison Control Center,(27–30) and two more adverse event reports from the FDA, altogether accounting for 8 cases of suicide death from overdose of temazepam as a single agent. These cases included six men with ages of 49, 66, 73, 74, 77, and 92 years and two women, ages 83 and 85 years old. The suicide of the 73 year old man occurred after taking temazepam for only 2–3 nights who gave no prior indication that he was suicidal.
Triazolam (Original approval November 15, 1982)
A 77 year old woman was found dead at home. Empty triazolam bottles were at the scene.(31) A complete autopsy was unremarkable. Toxicological analysis of blood and urine indicated no alcohol or other drugs besides triazolam.
A 57 year old man was found dead outdoors in winter in Japan.(32) Full autopsy failed to reveal a cause of death from natural causes. Stomach contents included 8.4 mg of triazolam (equivalent of 33 0.25-mg tablets). Toxicological analysis of blood and urine revealed high levels of triazolam but no other drugs.
Two additional cases of suicide death were reported due to triazolam alone, as confirmed by gas chromatography/mass spectrometry.(33)
Quazepam (Original approval December 27, 1985)
There are no published cases of suicide with quazepam. A search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to quazepam.
Estazolam (Original approval December 26, 1990)
There are no published cases of suicide with estazolam. A search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to estazolam.
Zolpidem (Original approval December 16, 1992)
A 68 year old woman had been found dead in her bed with an empty bottle of zolpidem 10 mg which had been dispensed with 30 pills the day before. (34)
A suicide death of an 86 year old woman who drowned in her bathtub after ingestion of zolpidem as a single agent overdose was reported and confirmed by gas chromatography/ mass spectrometry.(35)
Two cases of suicide death from zolpidem poisoning were reported including a 58 year old woman in which zolpidem was a single agent, as confirmed by gas chromatography.(36)
Apart from suicide deaths, there are numerous publications of suicide attempts that occurred during intoxication with zolpidem. A compilation of spontaneous adverse event reports from Australia between 2001 and 2008 indicated that zolpidem had higher odds for “parasomnia, amnesia, hallucinations, and perhaps suicidality compared to either all other drugs or hypnotics…”(37) They calculated an odds ratio of 8.3 (5.4–12.8) for suicidality related to zolpidem as compared to other psychotropic drugs in the survey. The authors acknowledged that a role for alcohol in the findings could not be ruled out and implicitly raise the concern that some of the unexpectedly high risk for suicide attempts with zolpidem could be related to a higher rate of parasomnia behavior during the period of peak drug effect. This possibility is supported by several detailed case reports.
A report of 91 coroner’s cases from New South Wales, Australia between 2001 and 2010 noted two cases of ‘bizarre, dissociative ‘ behavior leading to suicide death in decedents with toxicology-proven zolpidem use.(38) In one case, a person was dancing on a high ledge before falling, while in another case the person impulsively jumped out of a window during an argument. A 27 year old man with no known prior history of psychiatric illness, suicidal ideation, or sleep disorder took 20 mg zolpidem, in the absence of alcohol, and then took an additional 40 mg sometime in the middle of the night. The patient’s only explanation was that he remembered feeling suicidal later in the night.(39)
The FDA’s post-marketing safety review of the Z-drugs in 2006 included additional adverse event reports for zolpidem that were not found in the medical literature.(11) The FDA report describes 49 total suicidal-related adverse events in which zolpidem was judged to be a factor, including suicidal ideation (n=12), suicide attempt/self-harm (n=16), and suicide deaths (n=21). In 9/49 cases there was no prior history of psychiatric illness and no other use of psychotropic medication in 8 cases. In one instance, a 33 year old man with no history of mental illness took zolpidem for 4 or 5 nights, then on the last night took zolpidem 10 mg at 2:30 AM, awoke at 6 AM (3.5 hours later), went to work and the next thing he remembered was “standing on a pile of boxes with a noose around his neck.” In another case, a 38 year old man with no history of mental disorder began using zolpidem 10 mg and died by suicide on the 4th day (method not described). Finally, a 39 year old man with no history of mental illness took zolpidem 10 mg for 3 nights. On the third night, his wife “found him sleep walking in the closet with no memory of how he got there.” The next morning he “could not focus” and walked into the woods and shot himself. The FDA report summarized the zolpidem cases by noting that the suicidal events often occurred within a week of initiation, and many were accompanied by bizarre behavior, hallucinations, or paranoia.
Zaleplon (Original approval August 13, 1999)
While there are no published cases of suicide with zaleplon, the FDA Post-marketing Safety Review described one case of suicidal ideation, 3 cases of self-harm/suicide attempt, and 3 cases of suicide death related to zaleplon; however, only one of these cases had no prior psychiatric history. All of the zaleplon adverse events occurred within 14 days of drug initiation.(11)
Eszopiclone (Original approval December 15, 2004)
Sixty instances of poisoning with eszopiclone as a single agent were reported in Texas between 2005 and 2006.(40) There were no instances of death when eszopiclone was taken as a single agent in an overdose. However, the FDA Post-marketing Safety Review described 16 suicide-related adverse events, including seven cases of suicidal ideation, 5 cases of self-injury/suicidal attempt, and 4 suicide deaths. A psychiatric history was reported in all but one case, and in 13 cases the adverse event occurred within 1 month of initiation. Several cases were accompanied by “irritability, agitation, confusion, or worsening depression” before the event.(11)
Ramelteon (Original approval July 22, 2005)
There are no published cases of suicide with ramelteon. A search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to ramelteon.
Doxepin 3 and 6 mg (Original approval March 17, 2010)
There are no published cases of suicide with doxepin prescribed in low dose for insomnia.
Suvorexant (Original approval August 13, 2014)
In 2012, the FDA recommended prospective, systematic assessment of suicide in all clinical trials used in the registration of any new psychoactive medication. The Columbia-Suicide Severity Rating Scale was specifically named as a suitable instrument for this purpose.(41) Consequently, the research and development of suvorexant followed the FDA recommendations, and the findings of this analysis were reported in the FDA Suvorexant Advisory Committee Meeting in 2013.(42) As per the 2012 FDA recommendations, data were pooled across all Phase 3 trials. In the case of the NDA 204569 for suvorexant, this meant the collation of one combined-age, blinded, randomized high dose trial and one blinded, randomized combined-age low dose trial. High dose and low dose were defined as follows: Young adults: low dose 20 mg; high dose 40 mg; Elderly > 65: low dose 15 mg; high dose 30 mg. There were a total of 10 persons expressing suicidal ideation across both studies, as defined by the Columbia-Suicide Severity Rating Scale. (Table 1).
Table 1.
Allocation of. Columbia-Suicide Severity Rating Scale-defined suicidal ideation across suvorexant trials
| Frequency with suicidal ideation per CSSRS | % with suicidal ideation | |
|---|---|---|
| Placebo (n=1025) | 1 | 0.1% |
| Low dose (n=493) | 1 | 0.2% |
| High dose (n=1291) | 8 | 0.7% |
While there were no suicidal behaviors reported, and while the majority of suicidal ideation events lasted ‘minutes to hours and were mild to moderate in intensity,’ the FDA interpreted the results as supporting a dose-response relationship between suvorexant exposure and suicidal ideation.(42) As a result, the package label for suvorexant carries the unique warning that “in clinical studies, a dose-dependent increase in suicidal ideation was observed in patients taking Belsomra as assessed by questionnaires.” Examination of the specific cases of suicidal ideation as described in the Advisory Committee Meeting show that the data collection method failed to record whether the suicidal ideation occurred in temporal proximity to drug ingestion (i.e. at night, within a few hours of ingestion), or occurred later in the day after the drug effect would have dissipated. Finally, a search of the FDA’s adverse event files failed to reveal any possible single-agent suicide deaths related to suvorexant.
Discussion
Toxicology studies show that modern hypnotics have frequently been taken prior to suicide deaths, although the hypnotics are often taken in combination with other sedatives or alcohol. Still, death is possible when hypnotics are used as a single agent for self-poisoning, and we found examples of this for flurazepam, temazepam, triazolam, and zolpidem. While the available data might give the impression that some hypnotics are more likely to be associated with suicide than others, this conclusion should be tempered by the large variation in the time that different agents have been available and the different rates of prescribing.(43)
The retrospective case series have consistently shown that hypnotic users are over-represented among suicide victims, with odds ratios in the range of 2–3, but these studies have been unable to disentangle the confounding effect of treatment and diagnosis. Similarly, the prospective cohort studies show elevated Odds/Hazard Ratios from 1.2 up to 24.3. The prospective design solves the problem of demonstrating exposure to hypnotics before the suicide event, but three of the available prospective cohort studies did not collect information about diagnosis, so treatment and diagnosis are again confounded. The fourth of these studies considered psychiatric diagnosis, but not alcohol or substance abuse. Understandably, the retrospective and prospective cohort studies call for clinical trials to disentangle diagnoses and treatment effects. The implications of cohort studies are weakened by the frequent omission of a definition of what was considered a “hypnotic,” and by the inclusion of medications not usually considered as hypnotics, i.e., phenothiazines. The clinical trials of suvorexant are the only hypnotic trials that have prospectively and systematically measured suicidal ideation, and the pooled data may suggest a dose-response relationship between suvorexant exposure and increasing risk of suicidal ideation in individuals with primary insomnia.
The possibility of a causal relationship between suvorexant exposure and suicidal ideation raises the question of whether risk of suicide is limited to the benzodiazepine receptor mechanism, or instead may be a more general risk of exposures to various types of hypnotics. A common feature of risk could be disinhibition or increased impulsivity during the time of peak drug effect for some hypnotics.
This scenario is reinforced by the published case reports and the FDA adverse event reports that show that some suicidal behaviors and suicide deaths occur during a period of confusion, amnesia, hallucination, or paranoia in the first few hours after ingestion of a hypnotic, i.e., that suicide is linked to hypnotic induced parasomnia during the time of peak drug effect. Cognitive impairment, specifically problems with decision making and executive function, are common to both insomnia and suicide;(44;45) hence further cognitive impairment at the time of peak drug effect may further tilt the balance towards suicide. The risk of this scenario appears to be higher if the drug is consumed with alcohol, taken in a dose higher than recommended, if the patient does not go to bed or fall asleep soon after ingestion, or awakens a few hours after ingestion. This proposition does not address whether suicide risk is higher in hypnotic users during those hours long after the drug should have been metabolized. For example, is the risk of suicide elevated in a person who consumes zolpidem at 9:50 PM, is in bed by 10:00 PM, sleeps uninterrupted for 8 hours, and rises at 6 AM (assuming that the drug is nearly completely eliminated by that time)?
To the contrary, the possibility remains open that judicious prescription of hypnotics, when taken appropriately, might reduce (not increase) the risk of suicide. While this premise has not been directly tested, it has been shown that the addition of an FDA-approved hypnotic to an antidepressant will improve the overall rates of response to the antidepressant,(46;47) and it is reasonable to posit that superior antidepressant response would lead to superior reduction in suicide risk. Although alprazolam is approved as a benzodiazepine anxiolytic and not as a hypnotic, nevertheless, a meta-analysis of alprazolam clinical trials showed that (1) alprazolam was no more likely than placebo to be associated with emergence of worsening of suicidal ideation, but (2) alprazolam was more likely than placebo to be associated with an improvement in pre-existing suicidal ideation.(48)
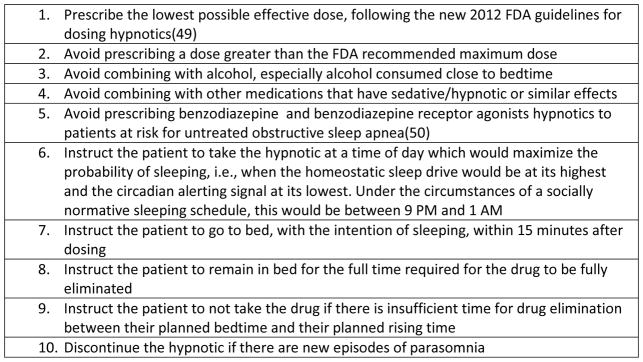
The principal new contribution of this review is the clarification regarding the timing of suicide risk related to ingestion of hypnotics. Under specific conditions, hypnotics might induce or exacerbate suicidality by altering consciousness or disinhibition at the time of peak drug effect, while at the same time hypnotics might reduce or prevent suicidal ideation in persons with insomnia and mental illness after appropriate drug metabolism. While the latter possibility is being evaluated, the risk of the former possibility might be reduced through the steps outlined in Figure 1 when prescribing hypnotics.
Figure 1.
Steps for Decreasing the Risks of Suicide When Prescribing Hypnotics
Acknowledgments
Supported by NIMH MH095776 and American Foundation for Suicide Prevention DIG-0-087-13 (MCG), MH095780 (Duke), and MH95778 (WI)
Footnotes
Disclosures: Dr. McCall receives honoraria from Wolters Kluwer Publishing, Global CME, Inc., CME Outfitters, and Anthem Inc. Dr. Benca is a consultant for Merck & Co, Janssen and Jazz Pharmaceuticals, and receives grant support from Merck. Dr. Rumble receives research support from Merck & Co Pharmaceuticals. Dr. Krystal receives grant support from NIH, Teva, Sunovion, Astellas, Abbott, Neosync, Brainsway, Janssen, ANS St Jude, Novartis and is a consultant to Abbott, Astellas, Astrazeneca, Attentiv, BMS, Teva, Eisai, Eli Lilly, GlaxoSmithKline, Jazz, Janssen, Merck, Neurocrine, Otsuka, Lundbeck, Roche, Sanofi-Aventis, Somnus, Sunovion, Takeda, Transcept and Vantia.
Reference List
- 1.McCall W, Black C. The link between suicide and insomnia: theoretical mechanisms. Current Psychiatry Reports. 2013;15:389. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edinger JD, Bonnet MH, Bootzin RR, Doghramji K, Dorsey CM, Epsie C, Jamieson A, McCall V, Morin CM, Stepanski E. Derivation of research diagnostic criteria for insomnia: Report of an American Academy of Sleep Medicine work group. Sleep. 2004;27:1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, Virginia: APA; 2013. [Google Scholar]
- 4.McCall WV, Blocker JN, D’Agostino R, Jr, Kimball J, Boggs N, Lasater B, Rosenquist PB. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Medicine. 2010;11:822–827. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCall W, Benca R, Rosenquist P, Riley M, Hodges C, Gubosh B, McCloud L, Newman J, Case D, Rumble M, Mayo M, White K, Phillips M, Krystal A. A multi-site randomized clinical trial to reduce suicidal ideation in suicidal adult outpatients with major depressive disorder: development of a methodology to enhance safety. Clinical Trials. 2015;12:189–198. doi: 10.1177/1740774515573958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bertisch SM, Herzig SJ, Winkelman JM, Buettner C. National use of prescription medications for insomnia: NHANES 1999–2010. Sleep. 2014;37:343–349. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999 May 1;22(Suppl 2):S347–S353. [PubMed] [Google Scholar]
- 8.Kripke Daniel F. Chronic hypnotic use: deadly risks, doubtful benefit. Sleep Medicine Reviews. 2000;4(1):5–20. doi: 10.1053/smrv.1999.0076. [DOI] [PubMed] [Google Scholar]
- 9.Youssef NA, Rich CL. Does acute treatment with sedative/hypnotics for anxiety in depressed patients affect suicide risk? A literature review. Annals of Clinical Psychiatry. 2008;20(3):157–169. doi: 10.1080/10401230802177698. [DOI] [PubMed] [Google Scholar]
- 10.Pae C-U, Koh JS, Lee S-J, Han C, Patkar AA, Masand PS. Association of sedative-hypnotic medications with suicidality. Expert Review Neurother. 2011;11(3):345–349. doi: 10.1586/ern.11.9. [DOI] [PubMed] [Google Scholar]
- 11.Mary Ross Southwork - Division of Drug Risk Evaluation. ODS Postmarketing safety review drug(s) zaleplon (20-859) - eszopiclone (21-476) - zolpidem (19-908) Event - suicidal ideation and attempts - completed suicides. Center for Drug Evaluation and Research of the Food and Drug Administration; D050402 D050403 D050404. 8-31-2006. [Google Scholar]
- 12.Mendelson WB, Rich C. Sedatives and suicide: the San Diego study. Acta Psychiatr Scand. 1993;88:337–341. doi: 10.1111/j.1600-0447.1993.tb03469.x. [DOI] [PubMed] [Google Scholar]
- 13.Michel K, Arestegui G, Spuhler T. Suicide with psychotropic drugs in Switzerland. Pharmacopsychiatry. 1994;27:114–118. doi: 10.1055/s-2007-1014289. [DOI] [PubMed] [Google Scholar]
- 14.Carlsten A, Waern M, Holmgren P, Allebeck P. The role of benzodiazepines in elderly suicides. Scand J Public Health. 2003;31:224–228. doi: 10.1080/14034940210167966. [DOI] [PubMed] [Google Scholar]
- 15.Brower KJ, McCammon RJ, Wojnar M, Ilgen MA, Wojnar J, Valenstein M. Prescription sleeping pills, insomnia, and suicidality in the National Comorbidity Survey Replication. J Clin Psychiatry. 2011;72(4):515–521. doi: 10.4088/JCP.09m05484gry. [DOI] [PubMed] [Google Scholar]
- 16.Taiminen T. Effect of psychopharmacotherapy on suicide risk in psychiatric inpatients. Acta Psychiatr Scand. 1993;87:45–47. doi: 10.1111/j.1600-0447.1993.tb03328.x. [DOI] [PubMed] [Google Scholar]
- 17.Sun Y, Lin C-C, Lu C-L, Hsu C-Y, Kao C-H. Association between zolpidem and suicide: a nationwide population-based case-control study. Mayo Clin Proc. 2016 doi: 10.1016/j.mayocp.2015.10.022. in press. [DOI] [PubMed] [Google Scholar]
- 18.Kripke D, Klauber MR, Wingard DL, Fell RL, Assmus JD, Garfinkel L. Mortality hazard associated with prescription hypnotics. Biological Psychiarty. 1998;43:687–693. doi: 10.1016/s0006-3223(97)00292-8. [DOI] [PubMed] [Google Scholar]
- 19.Allgulander C, Nasman P. Regular hypnotic drug treatment in a sample of 32,679 Swedes: associations with somatic and mental health, inpatient psychiatric diagnoses and suicide, derived with automated record-linkage. Psychosomatic Medicine. 1991;53:101–108. doi: 10.1097/00006842-199101000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Neutel CI, Patten SB. Risk of suicide attempt after benzodiazepine and/or hypnotic use. Ann Epidemiol. 1997;7:568–574. doi: 10.1016/s1047-2797(97)00126-9. [DOI] [PubMed] [Google Scholar]
- 21.Mallon L, Broman J-E, Hetta J. Is usage of hypnotics associated with mortality? Sleep Medicine. 2009;10:279–286. doi: 10.1016/j.sleep.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Aderjan R, Mattern R. Eine todlich verlaufene Monointoxikation mit Flurazepam (Dalmadorm) Arch Toxicol. 1979;43:69–75. doi: 10.1007/BF00695876. [DOI] [PubMed] [Google Scholar]
- 23.McIntyre IM, Syrjanen ML, Lawrence KL, Dow C, Drummer OH. A fatality due to flurazepam. Journal of Forensic Sciences. 1994;39:1571–1574. [PubMed] [Google Scholar]
- 24.Martello S, Oliva A, de Giorgio F, Chiarotti M. Acute flurazepam intoxication. Am J Forensic Med Pathol. 2006;27:55–57. doi: 10.1097/01.paf.0000201106.59902.fb. [DOI] [PubMed] [Google Scholar]
- 25.Jung M, Rana S, Paik I, Bedward Y. Palliative care after an attempted suicide: an ethical dilemma in the absence of terminal disease. AGS. 2014:S168. [Google Scholar]
- 26.Watson W, Litovitz T, Rogers G, Klein-Schwartz W, Reid N, Youniss J. 2004 Annual Report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. American Journal of Emergency Medicine. 2005;23:589–666. doi: 10.1016/j.ajem.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 27.Bronstein A, Spyker D, Cantilena L, Green J, Rumack B, Giffin S. 2008 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 26th annual report. Clinical Toxicology. 2009;47:911–1084. doi: 10.3109/15563650903438566. [DOI] [PubMed] [Google Scholar]
- 28.Bronstein A, Spyker D, Cantilena L, Green J, Rumack B, Giffin S. 2009 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 27th annual report. Clinical Toxicology. 2010;(48):979–1178. doi: 10.3109/15563650.2010.543906. [DOI] [PubMed] [Google Scholar]
- 29.Bronstein A, Spyker D, Cantilena L, Rumack B, Dart R. 2011 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th annual report. Clinical Toxicology. 2012;50:911–1164. doi: 10.3109/15563650.2012.746424. [DOI] [PubMed] [Google Scholar]
- 30.Mowry J, Spyker D, Cantilena L, McMillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers: A National Poison Data System (NPDS): 31st annual report. Clinical Toxicology. 2014;52:1032–1283. doi: 10.3109/15563650.2014.987397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levine B, Grieshaber A, Pestaner KA, Smialek JE. Distribution of triazolam and alpha hydroxytriazolam in a fatal intoxication case. Journal of Analytical Toxicology. 2002;26:52–54. doi: 10.1093/jat/26.1.52. [DOI] [PubMed] [Google Scholar]
- 32.Moriya F, Hashimoto Y. A case of fatal triazolam overdose. Legal Medicine. 2003;5:S91–S95. doi: 10.1016/s1344-6223(02)00074-3. [DOI] [PubMed] [Google Scholar]
- 33.Joynt BP. Triazolam blood concentrations in forensic cases in Canada. Journal of Analytical Toxicology. 1993;17:171–177. doi: 10.1093/jat/17.3.171. [DOI] [PubMed] [Google Scholar]
- 34.Winek CL, Wahba WW, Janssen JK, Rozin L, Rafizadeh V. Acute overdose of zolpidem. Forensic Science International. 1996;78:165–168. doi: 10.1016/0379-0738(95)01875-1. [DOI] [PubMed] [Google Scholar]
- 35.Lichtenwalner M, Tulley R. A fatality involving zolpidem. Journal of Analytic Toxicology. 1997;21:567–569. doi: 10.1093/jat/21.7.567. [DOI] [PubMed] [Google Scholar]
- 36.Gock SB, Wong SH, Nuwayhid N, Venuti SE, Kelley PD. Acute zolpidem overdose - report of two cases. Journal of Analytical Toxicology. 1999;23:559–562. doi: 10.1093/jat/23.6.559. [DOI] [PubMed] [Google Scholar]
- 37.Ben-Hamou M, Marshall NS, Grunstein RR, Saini B, Fois RA. Spontaneous adverse event reports associated with zolpidem in Australia 2001–2008. Journal of Sleep Research. 2011;20:559–568. doi: 10.1111/j.1365-2869.2011.00919.x. [DOI] [PubMed] [Google Scholar]
- 38.Darke S, Deady M, Duflou J. Toxicology and characteristics of deaths involving zolpidem in New South Wales Australia 2001–2010. J Forensic Sci. 2012;57(5):1259–1262. doi: 10.1111/j.1556-4029.2012.02117.x. [DOI] [PubMed] [Google Scholar]
- 39.Hejri SM, Faizi M, Babaeian Zolpidem-induced suicide attempt: a case report. DARU Journal of Pharmaceutical Sciences. 2013;21(77) doi: 10.1186/2008-2231-21-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Forrester MB. Eszopiclone ingestions reported to Texas poison control centers, 2005–2006. Human &Experimental Toxicology. 2007;26:795–800. doi: 10.1177/0960327107084045. [DOI] [PubMed] [Google Scholar]
- 41.Center for Drug Evaluation and Research of the Food and Drug Administration. Guidance for Industry - Suicidal ideation and behavior - prospective assessment of occurrence in clinical trials (revision 1) Food and Drug Administration; Aug 6, 2012. [Google Scholar]
- 42.Peripheral &Central Nervous System Drugs Advisory Committee. Suvorexant Advisory Committee Meeting Briefing Document - Suvorexant Tablets Insomnia Indication - NDA 204569. Food and Drug Administration; May 22, 2013. [Google Scholar]
- 43.Kaufmann CN, Spira AP, Alexander GC, Rutkow L, Mojtabai R. Trends in prescribing of sedative hypnotic medications in the USA: 1993–2010. Pharmacoepidemiology and Drug Safety. doi: 10.1002/pds.3951.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin C. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Rev Med. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 45.Pollock L, Williams J. Problem-solving in suicide attempters. Psychol Med. 2004;34:163–167. doi: 10.1017/s0033291703008092. [DOI] [PubMed] [Google Scholar]
- 46.Fava M, McCall V, Krystal A, Wessel TC, Rubens R, Caron J, Amato D, Roth T. Eszopiclone Co-Administered With Fluoxetine in Patients With Insomnia Coexisting With Major Depressive Disorder. Biol Psychiatry. 2006;59:1052–1060. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 47.McCall WV, Blocker JN, D’Agostino RB, Jr, Kimball J, Boggs N, Lasater B, Haskett R, Krystal A, McDonald WM, Rosenquist PB. Treatment of insomnia in depressed insomniacs: effects on health-related quality of life, objective and self-reported sleep, and depression. Journal of Clinical Sleep Medicine. 2010;6:322–329. [PMC free article] [PubMed] [Google Scholar]
- 48.Jonas J, Hearron A. Alprazolam and suicidal ideation: a meta-analysis of controlled trials in the treatment of depression. Journal of Clinical Psychopharmacology. 1996;16:208–211. doi: 10.1097/00004714-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 49.FDA. US Department of Health and Human Services; Jan 10, 2013. http:,www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm334798.htm. FDA requiring lower recommended dose for certain sleep drugs containing zolpidem. [Google Scholar]
- 50.McEntire DM, Kirkpatrick DR, Kerfeld MJ, Hambsch ZJ, Reisbig MD, Agrawal DK, Youngblood CF. Effect of sedative-hypnotics, anesthetics and analgesics on sleep architecture in obstructive sleep apnea. Expert Review of Clinical Pharmacology. 2014;7:787–806. doi: 10.1586/17512433.2014.966815. [DOI] [PubMed] [Google Scholar]