Abstract
Introduction
The detailed knowledge of the peritoneal recesses has great significance with respect to internal hernias. The recesses are usually related to rotation and adhesion of abdominal viscera to the posterior abdominal wall and/or the presence of retroperitoneal vessels which raises the serosal fold. The duodenal recesses are usually related to the 3rd and 4th parts of the duodenum. Internal hernias with respect to these recesses are difficult to diagnose clinically and usually noticed at the time of laparotomy. So, the knowledge of these recesses can be valuable to abdominal surgeons.
Material and methods
The present study was conducted in 100 cases including 10 cadavers, 45 post mortem cases and 45 cases undergoing laparotomy.
Results
We found superior and inferior duodenal recesses in 28% and 52% respectively, paraduodenal in 12%, mesentericoparietal in 3%, retroduodenal in 2% and duodenojejunal in 18% of cases. Two abnormal duodenojejunal recesses were found, one on the right (instead of the left) of the abdominal aorta, and in the other the opening was directed upwards instead of downwards. The incidence of internal hernias was 3%.
Conclusions
Thus it was observed that there is low incidence of superior and inferior duodenal recesses, and high incidence of paraduodenal recess. The abnormal recesses might be due to malrotation of the gut. In laparotomy cases, the internal hernia was noticed when the abdomen was opened for intestinal obstruction. The incidence of internal hernia was found to be high.
Keywords: peritoneal recesses, internal hernias, retroperitoneal vessels
Introduction
The present study was carried out to observe the duodenal recesses or fossae and their association with internal hernias, since there is a paucity of data on this subject in the Indian population. The duodenal recesses studied were superior, inferior, paraduodenal, mesentericoparietal, retroduodenal and duodenojejunal. The peritoneal recesses are usually related to rotation of the gut and adhesion of abdominal viscera to the posterior abdominal wall during fetal development, and/or the presence of retroperitoneal vessels which raise serosal folds. These recesses, therefore, are regarded as congenital and have been considered clinically and surgically as sites for internal abdominal hernias [1, 2]. Some of the peritoneal recesses are well known (such as the superior duodenal, the inferior duodenal, and the duodenojejunal) and have been described in the literature. Other recesses such as retroduodenal, mesenterico-parietal, and paraduodenal are less commonly observed. They are clinically relevant as internal abdominal hernias may develop inside them. These hernias are difficult to diagnose clinically as they are usually noticed at the time of laparotomy [3, 4]. Thus, the topography of these recesses is very valuable to abdominal surgeons.
Due to the complex nature of the rotation of the gut and resorption of the mesentery, these recesses may enlarge or recede, and individual variations may lead to the development of different recesses in this area. The normal coalescence of the duodenum to the parietal peritoneum occurs between its 3rd and 4th parts, and at the level of the duodenojejunal flexure, by means of two serous folds, inferior and superior. The majority of internal hernias result from congenital anomalies of intestinal rotation and peritoneal attachment [5, 6].
There has been no descriptive study encompassing all the duodenal recesses. The present study is an attempt to describe these topographically and their association with internal abdominal hernias.
Material and methods
The present study was conducted in 100 cases including 10 cadavers, 45 bodies undergoing post-mortem and 45 patients undergoing laparotomy for different indications in the Department of Anatomy, Department of Forensic Medicine and Toxicology and Department of General and Pediatric Surgery, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi. The recesses were observed for: 1) position and direction of the opening, 2) depth and width, 3) related structures (normal and anomalous) and 4) presence of internal hernia, if any.
This study is a part of a post-graduate thesis which has been undertaken after the approval and permission of the thesis committee (Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi), and there is no ethical issue.
In cadavers, all the observations were made once the abdomen was opened for dissection for academic purposes, and these were taken before the disturbance of the peritoneum by students. The greater omentum and transverse mesocolon were pulled upwards and coils of jejunum along with its mesentery were pulled downwards and to the right side so as to expose the duodenojejunal junction, and the third and fourth part of the duodenum were identified. In post-mortem cases, all the observations were made before removal of abdominal viscera for post mortem examination.
In laparotomy cases, the measurements were made by the operating surgeon in consultation with the investigator. The measurements were made either by Vernier caliper or by measuring tape.
Results
The incidence of duodenal recesses in our study is tabulated in Table I. The other observations are tabulated in Tables II–VII.
Table I.
Incidence of duodenal recesses
| Duodenal recesses | C (N = 10) n (%) | P (N = 45) n (%) | L (N = 45) n (%) | Total incidence (N = 100) n (%) |
|---|---|---|---|---|
| Superior duodenal | 2 (20) | 14 (31.11) | 12 (26.66) | 28 (28) |
| Inferior duodenal | 6 (60) | 25 (55.55) | 21 (46.66) | 52 (52) |
| Paraduodenal | 2 (20) | 8 (17.77) | 2 (4.44) | 12 (12) |
| Mesentericoparietal | 2 (20) | 0 (0) | 1 (2.2) | 3 (3) |
| Duodenojejunal | 2 (20) | 6 (13.33) | 10 (22.22) | 18 (18) |
| Retroduodenal | 1 (10) | 1 (2.22) | 0 (0) | 2 (2) |
C – cadavers, P – postmortem cases, L – laparotomy cases.
Table II.
Superior duodenal recess
| S. No. | Position and direction | Depth [cm] | Width [cm] | Related structures (normal) | Related structures (anomalous) |
|---|---|---|---|---|---|
| 1 | Behind D-J fold, Lt of 4th part of duodenum, directed ↓ | 2.0 | 1.2 | – | – |
| 4 | do | 2.4 | 1.4 | – | – |
| 13 | do | 2.3 | 1.8 | – | – |
| 15 | do | 3 | 2 | – | – |
| 18 | do | 3 | 1.7 | – | – |
| 21 | do | 2 | 1.4 | – | – |
| 26 | do | 3 | 1.5 | – | – |
| 29 | do | 3.2 | 1.2 | – | – |
| 32 | do | 2.5 | 1.2 | – | – |
| 36 | do | 2.5 | 1.2 | – | – |
| 38 | do | 3.5 | 2 | – | – |
| 42 | do | 2.5 | 1.2 | – | – |
| 44 | do | 2.5 | 1.2 | – | – |
| 51 | do | 3.5 | 1.2 | – | – |
| 53 | do | 3.5 | 1.2 | – | – |
| 55 | do | 2.5 | 1.2 | ||
| 57 | do | 1.5 | 0.6 | – | – |
| 62 | do | 1.5 | 0.6 | – | – |
| 63 | do | 2.5 | 1.4 | – | – |
| 64 | do | 2.5 | 1.2 | – | – |
| 65 | do | 1.0 | 0.5 | – | – |
| 66 | do | 3.0 | 2.0 | – | – |
| 70 | do | 3.0 | 1.8 | – | – |
| 75 | do | 3.0 | 1.8 | – | |
| 77 | do | 3.5 | 1.8 | – | – |
| 80 | do | 3.0 | 1.4 | ||
| 84 | do | 2.0 | 0.8 | – | – |
| 95 | do | 2.5 | 1.2 |
These are the observations done in individual case. S. No. 1–10: cadavers, S. No. 11–55: post-mortem cases, S. No. 56–100: laparotomy cases (56–90 paediatric cases & 90–100 adult cases), D-J fold – duodenojejunal fold. Lt – left, ↓ – downwards, do – same.
Table VII.
Retroduodenal recess
| S. No. | Position and direction | Depth [cm] | Width [cm] | Related structures (normal) | Related structures (anomalous) |
|---|---|---|---|---|---|
| 10 | Behind the 3rd & 4th part of duodenum, in front of abdominal aorta. opening directed Lt & ↓ | 9.0 | 4.0 | Abdominal aorta deep in the recess | – |
| 48 | Behind the 3rd & 4th part of duodenum, in front of abdominal aorta. opening directed Lt & ↓ | 6.0 | 3.0 | Abdominal aorta deep in the recess | – |
These are the observations done in individual case. S. No. 1–10: cadavers, S. No. 11–55: post-mortem cases, S. No. 56–100: laparotomy cases (56–90 paediatric cases & 90–100 adult cases), Lt – left, ↓ – downwards.
Table III.
Inferior duodenal recess
| S. No. | Position and direction | Depth [cm] | Width [cm] | Related structures (normal) | Related structures (anomalous) |
|---|---|---|---|---|---|
| 3 | Behind DMC fold, Lt of 4th part of duodenum, directed ↑ | 3.6 | 1.0 | – | – |
| 4 | do | 3.0 | 1.0 | – | – |
| 5 | do | 4.0 | 2.0 | – | – |
| 6 | do | 3.6 | 1.5 | – | – |
| 7 | do | 3.5 | 2.0 | – | |
| 10 | do | 4.0 | 3.0 | – | – |
| 11 | do | 4.0 | 1.5 | – | – |
| 13 | do | 4.2 | 1.2 | – | – |
| 14 | do | 3.5 | 1.2 | – | – |
| 17 | do | 4.7 | 2.6 | – | – |
| 19 | do | 5.0 | 2.9 | – | – |
| 22 | do | 4.6 | 2.9 | – | – |
| 23 | do | 4.9 | 2.6 | – | – |
| 26 | do | 4.0 | 2.0 | – | – |
| 27 | do | 3.5 | 2.0 | – | – |
| 29 | do | 4.0 | 1.6 | – | – |
| 30 | do | 2.0 | 1.2 | – | – |
| 31 | do | 3.5 | 2.0 | – | – |
| 32 | do | 3.0 | 1.8 | – | – |
| 34 | do | 3.5 | 1.8 | – | – |
| 35 | do | 2.5 | 1.2 | – | – |
| 36 | do | 4.0 | 2.5 | – | – |
| 37 | do | 3.5 | 1.8 | – | – |
| 38 | do | 4.0 | 2.9 | – | – |
| 40 | do | 4.0 | 2.0 | – | – |
| 42 | do | 4.0 | 2.0 | – | – |
| 44 | do | 4.0 | 2.5 | – | – |
| 45 | do | 2.0 | 1.2 | – | – |
| 50 | do | 4.0 | 1.8 | – | – |
| 51 | do | 4.0 | 2.5 | – | – |
| 54 | do | 4.0 | 1.2 | – | – |
| 57 | do | 2.0 | 1.0 | – | – |
| 60 | do | 3.0 | 1.2 | – | – |
| 62 | do | 3.0 | 1.4 | – | – |
| 63 | do | 3.5 | 1.8 | – | – |
| 64 | do | 3.0 | 1.4 | – | – |
| 65 | do | 1.8 | 0.8 | – | – |
| 69 | do | 4.0 | 2.2 | – | – |
| 70 | do | 3.0 | 2.0 | – | – |
| 71 | do | 4.0 | 2.1 | – | – |
| 72 | do | 4.0 | 2.0 | – | – |
| 73 | do | 3.0 | 1.8 | – | – |
| 75 | do | 4.0 | 2.2 | – | – |
| 76 | do | 4.0 | 1.8 | – | – |
| 80 | do | 4.0 | 1.8 | – | – |
| 81 | do | 2.0 | 1.2 | – | – |
| 82 | do | 1.4 | 1.2 | – | – |
| 84 | do | 2.4 | 1.0 | – | – |
| 85 | do | 3.5 | 1.6 | – | – |
| 95 | do | 3.6 | 2.0 | – | Loop of jejunum |
| 97 | do | 3.5 | 1.6 | – | – |
| 100 | do | 3.6 | 1.4 | – | – |
These are the observations done in individual case. S. No. 1–10: cadavers, S. No. 11–55: post-mortem cases, S. No. 56–100: laparotomy cases (56–90 paediatric cases & 90–100 adult cases), DMC – duodenomesocolic fold, Lt – left, ↑ – upwards, do – same.
Table IV.
Paraduodenal recess
| S. No. | Position and direction | Depth [cm] | Width [cm] | Related structures (normal) | Related structures (anomalous) | Internal hernias |
|---|---|---|---|---|---|---|
| 1 | Behind the paraduodenal fold, Lt of 4th part of duodenum, directed Rt ↑ | 2.5 | 3.9 | IMV | Ascending branch of left colic artery | – |
| 9 | Directed RT & ↓ | 2.5 | 3.0 | IMV | – | – |
| 24 | Behind the paraduodenal fold, Lt of 4th part of duodenum, directed Rt ↑ | 4.6 | 2.5 | IMV | Ascending branch of left colic artery | Yes, loop of jejunum |
| 25 | Directed RT & ↓ | 4.0 | 2.5 | IMV | – | – |
| 26 | do | 4.0 | 2.0 | – | – | – |
| 27 | do | 3.5 | 2.0 | – | – | |
| 28 | do | 2.5 | 1.0 | IMV | Ascending branch of Lt of of Lt colic artery | – |
| 33 | do | 4.5 | 2.5 | IMV | – | Yes, loop of jejunum |
| 37 | do | 4.5 | 2.5 | IMV | – | – |
| 46 | do | 2.5 | 1.2 | IMV | – | – |
| 74 | do | 2.0 | 1.2 | IMV | – | – |
| 96 | do | 2.4 | 2.0 | IMV | – |
These are the observations done in individual case. S. No. 1–10: cadavers, S. No. 11–55: post-mortem cases, S. No. 56–100: laparotomy cases (56–90 paediatric cases & 90–100 adult cases), IMV – inferior mesenteric vein, Lt – left, Rt – right, ↓ – downwards, ↑ – upwards, do – same.
Table V.
Duodenojejunal recess
| S. No. | Position and direction | Depth [cm] | Width [cm] | Related structures (normal) | Related structures (anomalous) |
|---|---|---|---|---|---|
| 9 | On the Lt side of abdominal aorta between D-J fold & root of transverse mesocolon, orifice is circular & directed ↓ & Rt | 3.0 | 2.2 | Above pancreas, on Lt by Lt kidney & LRV inferiorly | – |
| 10 | Opening directed ↑ & Lt | 1.5 | 3.0 | do | – |
| 43 | do | 3.5 | 1.5 | do | – |
| 46 | do | 3.0 | 1.2 | do | – |
| 47 | do | 3.5 | 1.2 | do | – |
| 48 | do | 2.5 | 1.0 | do | – |
| 49 | do | 2.5 | 1.2 | do | – |
| 52 | do | 3.0 | 1.2 | do | – |
| 58 | do | 2.0 | 1.0 | do | – |
| 59 | do | 2.0 | 0.8 | do | – |
| 61 | do | 2.0 | 1.2 | do | – |
| 68 | do | 3.0 | 1.2 | do | – |
| 73 | do | 2.0 | 1.0 | do | – |
| 78 | do | 3.0 | 1.2 | IMV in Lt fold | – |
| 79 | do | 3.5 | 2.0 | Above pancreas, on Lt by Lt kidney & LRV inferiorly | – |
| 83 | do | 3.0 | 1.2 | do | – |
| 88 | do | 2.5 | 1.0 | IMV in Lt fold | – |
| 89 | do | 2.2 | 0.4 | do | – |
These are the observations done in individual case. S. No. 1–10: cadavers, S. No. 11–55: post-mortem cases, S. No. 56–100: laparotomy cases (56–90 paediatric cases & 90–100 adult cases), D-J fold – duodenojejunal fold, IMV – inferior mesenteric vein, LRV – left renal vein, Lt – left, Rt – right, ↓ – downwards, ↑ – upwards, do – same.
Table VI.
Mesenterico-parietal recess
| S. No. | Position and direction | Depth [cm] | Width [cm] | Related structures (normal) | Related structures (anomalous) |
|---|---|---|---|---|---|
| 1 | Below the 3rd part of duodenum, behind first part of mesojejunum, directed to Lt | 3.0 | 2.5 | Superior mesenteric vessels | – |
| 8 | do | 3.2 | 2.5 | Superior mesenteric vessels | – |
| 90 | do | 4.0 | 2.5 | Superior mesenteric vessels | – |
These are the observations done in individual case. S. No. 1–10: cadavers, S. No. 11–55: post-mortem cases, S. No. 56–100: laparotomy cases (56–90 paediatric cases & 90–100 adult cases), Lt – left, do – same.
In these the numbers 1 to 100 are: 1–10 were cadavers, 11–55 were post-mortem cases, 56–100 were laparotomy cases (56–90 pediatric cases and 90–100 adult cases).
Two abnormal duodenojejunal recesses were found, one on the right (instead of the left) of the abdominal aorta, and in the other the opening was directed upwards instead of downwards.
Discussion
The peritoneum is the largest and most complexly arranged serous membrane in the body. Its reflections form ligaments, mesenteries, omenta and the route of natural spread of peritoneal fluid. These also serve as boundaries for disease processes and are conduits for disease spread. Computed tomography and to a lesser extent sonography and magnetic resonance (MR) imaging allow the accurate examination of the complex anatomy of the peritoneal cavity, which is the key to understanding the pathological processes affecting it. Hence it is very important to know the peritoneal recesses, their relations and the internal hernias [1, 7].
In certain parts of the abdomen, peritoneal folds may sometimes be found which bind fosse or recesses of the peritoneal cavity. These recesses are of surgical importance since they may become the site of internal herniae, that is, a segment of intestine may enter a recess and may be constricted and get strangulated by the peritoneal fold guarding the entrance to the recess. Since the entrance to the recess may need to be cut to relieve strangulation and allow the gut to be drawn out of the recess, it is necessary to note whether the fold is significantly vascularised [8].
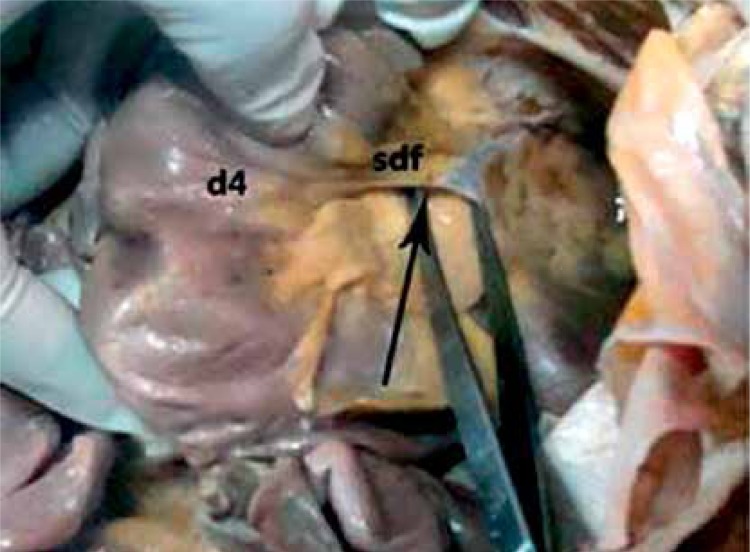
The superior duodenal recess (recessus duodeno-mesocolicus superior) was found in 28% of cases, compared to 40% to 50% found by other researchers [4, 8–11], and was associated with inferior duodenal recess in 75% of cases. It was located on the left side of the 4th part of the duodenum, and the orifice was directed downwards. Its depth and width were 1–3.5 cm and 0.5–2.0 cm respectively (Figure 1).
Figure 1.
Superior duodenal recesses
d4 – ascending part of duodenum, sdf – superior duodenal fold, arrow in the superior duodenal recess.
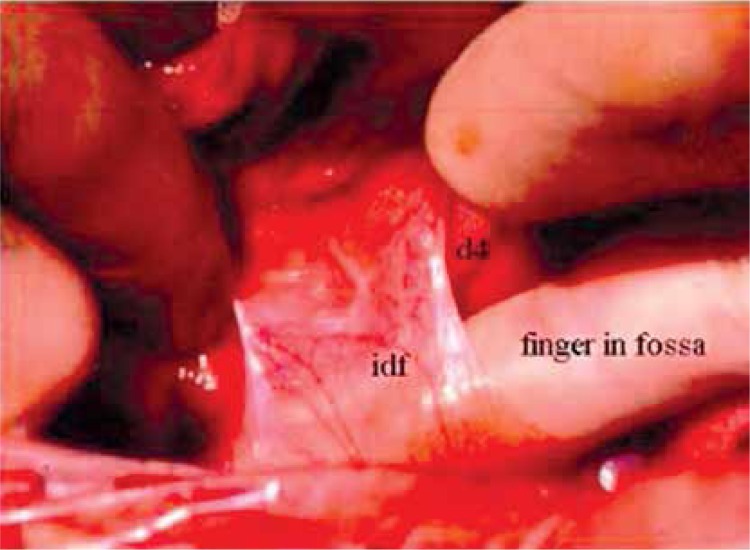
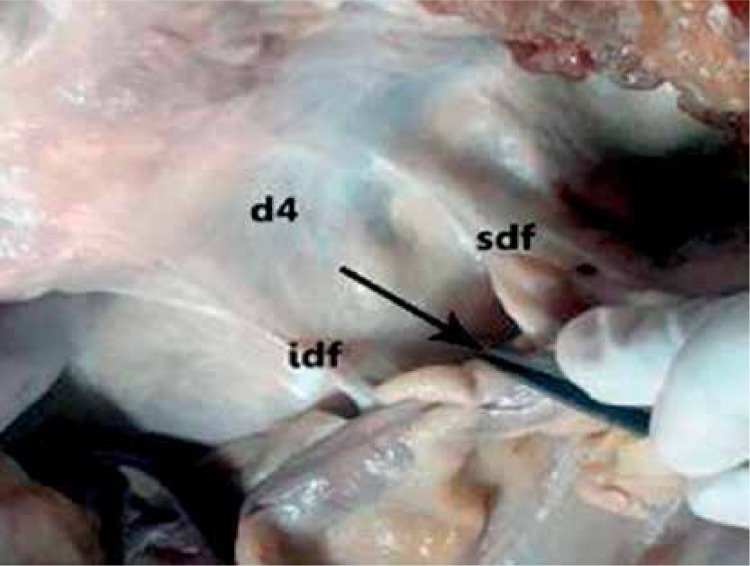
The inferior duodenal recess (fossa duodeno-jejunalis of Treitz; recessus duodeno-mesocolicus inferior of Brosike) was observed in 52% of cases as against 70–75% reported by other workers [4, 8–11]. It was situated on the left of the ascending (4th) part of the duodenum, and the opening was directed upwards. Maximum depth and width were 5.0 cm and 2.9 cm respectively (Figure 2). Also, in one of the cases, we found a common opening for both superior and inferior recesses, a finding not reported earlier (Figure 3).
Figure 2.
Inferior duodenal recesses
d4 – 4th part of the duodenum, idf – inferior duodenal fold, finger in inferior duodenal recess.
Figure 3.
Common opening for both superior and inferior duodenal recesses
d4 – ascending part of duodenum, sdf – superior duodenal fold, idf – inferior duodenal fold, arrow in the common opening for both the recesses.
The genesis of superior and inferior duodenal folds has been described differently by various researchers [4]. According to Treitz, these are traction folds formed during development, due to dragging of the intestine and displacement of the caecum and ascending colon to the right side, whereas Waldeyer describes them as vascular folds due to the inferior mesenteric vein. Treves suggested that the inferior duodenal fold is a remnant of the mesoduodenum, but Told describes these as fusion folds, caused by the process of physiological adhesions between the original left, afterwards anterior surface of the ascending part of the duodenum and the right or anterior surface of the descending mesocolon [4]. Several authors [1, 5, 9, 12] have observed peritoneal fossae, contributing to the discussion about their origin and relationship to congenital or acquired internal abdominal hernias. The process of formation of peritoneal fossae is not easy to explain. According to Ancel and Cavaillon [5], the normal coalescence of the duodenum to the posterior parietal peritoneum would occur between its third and fourth part, and at the level of the duodeno-jejunal flexure, by means of two (inferior and superior) serous folds. These connect the duodenum horizontally to the serosa. In the meantime, the folds would also grow vertically: the inferior upward and the superior downward. In this way the inferior and superior fossae are generated.
These authors [5] noted that the inferior duodenal fold was better developed than the superior one. The incidence of inferior duodenal fossa (52%) is almost double that of superior duodenal fossa (28%) found in the present study, which is a very significant difference. In our study, we found a common opening for the superior and inferior duodenal fossae in one of the cases. This can be explained on the basis of vertical growth of the two folds, and these folds might have grown extensively towards each other and fused laterally, thus forming a common opening.
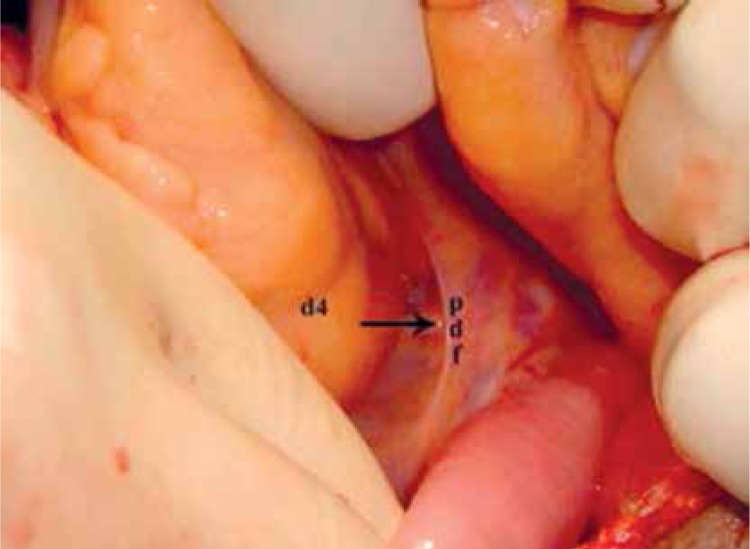
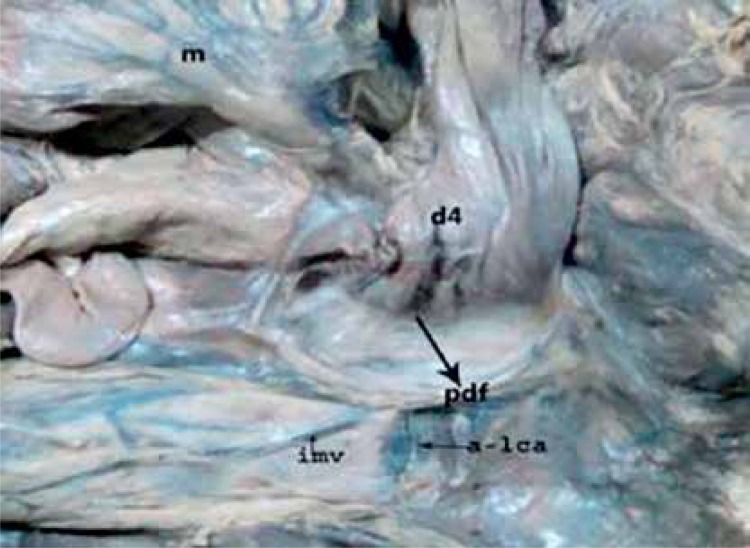
Paraduodenal fossa (recess venosus, fossa of Landzert) originates as congenital peritoneal anomaly owing to failure of mesenteric fusion with the parietal peritoneum. There is also an associated abnormal rotation during imprisonment of the small intestine beneath the developing colon [6]. In the present study a paraduodenal recess was found in 12% of cases, which is contrary to many studies [2, 4, 8, 11] where it was 2%. Each was situated on the left side of the 4th part of the duodenum, and the opening was directed downwards and to the right – a finding similar to that of other authors [2, 4, 8, 12–14]. Its depth was 2 to 4.5 cm and width 1 to 4 cm (Figure 4). We found its association with the mesentericoparietal recess in one instance and the inferior duodenal recess in three cases.
Figure 4.
Paraduodenal recesses
d4 – ascending part of duodenum, pdf – paraduodenal fold, arrow in the paraduodenal recess.
The genesis of the paraduodenal fossa might be due to raising of the serosal fold(s) by the underlying inferior mesenteric vein and/or the ascending branch of the left colic artery [3, 4]. In the present study, we found two separate paraduodenal recesses, one due to the ascending branch of the left colic artery (arterial recess) and the other due to the inferior mesenteric vein (venous recess) (Figure 5). This hypothesis has been described by other authors [1, 5, 9]. Paraduodenal hernia was observed in 2 (16.66%) cases of the total number of paraduodenal fossae found in our study. Also, both of these hernias were seen only on the left side.
Figure 5.
Vessels in paraduodenal fold
d4 – ascending part of duodenum, pdf – paraduodenal fold, imv – inferior mesenteric vein, a-lca – ascending branch of left colic artery, m – the mesentery.
Mesentericoparietal recess (of Waldeyer) was observed in the first part of the mesojejunum in our study. It was immediately behind the superior mesenteric artery, and just below the 3rd part of the duodenum. It was present in 3% of cases and mostly found in adults, in contrast to others [4, 8, 9] who found the prevalence higher in the pediatric age group. This recess was not associated with other duodenal fossae. Its depth and width were 3–4 cm and 2.5 cm respectively.
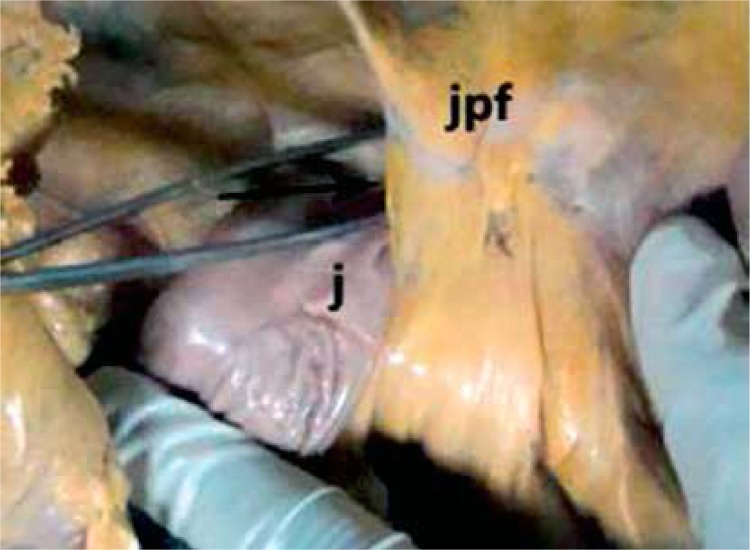
The duodenojejunal fossa (recessus duodeno-jejunalis superior) was seen by pulling the jejunum downwards and to the right, after the transverse colon was pulled upwards. These were found in 18% of cases in the present study, quite similar to those reported by other researchers [4, 8]. Their depth and width measured 1.5–3.5 cm and 0.4–3.0 cm respectively.
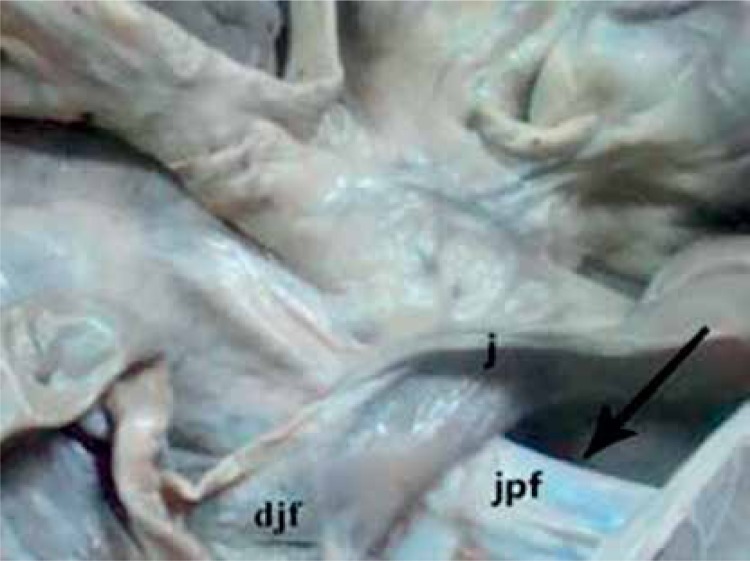
Two abnormal duodenojejunal fossae were found, one on the right side of the abdominal aorta and opening was directed to the right and downwards (Figure 6), and in the other the opening was directed upwards instead of downwards (Figure 7). This might be due to the malrotation of the gut.
Figure 6.
Duodenojejunal recesses
j – jejunum, jpf – jejunoparietal fold, arrow in the duodenojejunal recess.
Figure 7.
Duodenojejunal recesses
j – jejunum, jpf – jejunoparietal fold, djf – duodenojejunal flexure, arrow in the duodenojejunal recess.
Retroduodenal recess was found to be the largest of the duodenal recesses in the present study and was behind the horizontal and the ascending part of the duodenum, in front of the abdominal aorta. It was observed in 2% of cases. In one of the cases, it was extending upwards as far as the duodenojejunal junction. It was 6 cm and 10 cm deep and 3 cm and 4 cm in width and was bounded on both sides by duodenoparietal folds. Its orifice was facing downwards and to the left.
An internal abdominal hernia is defined as the protrusion of a viscous through a normal or abnormal aperture within the confines of the peritoneal cavity. The hernial orifice may be a preexisting anatomic structure, such as the foramen of Winslow, or a pathologic defect of congenital or acquired origin. The incidence of these hernias is estimated between 0.2% and 2% of abdominal hernias, and 0.2% to 0.9% of autopsies. These hernias mostly presented as an intestinal obstruction, and diagnosis is usually made at the time of surgery [3, 5, 6, 15–18].
The role of preoperative radiologic diagnosis of internal hernias has generally not been appreciated. Indeed, in the differential diagnosis of radiographic findings of intestinal obstruction or unusual appearing grouping of bowel loops, “some type of internal hernia” is often loosely entertained without a precise appreciation of types and distinctive findings. Hence, with awareness of the underlying anatomic features of recesses and of the dynamics of intestinal entrapment, the correct diagnosis of an internal hernia can be made [15–22].
We found the incidence of internal hernias quite high in the Indian population, at was around 3%. These were, two left paraduodenal hernias, found in postmortem cases, and one in the inferior duodenal recesses, seen in a laparotomy case. In the case of inferior duodenal hernia, the patient was explored for intestinal obstruction, and it was seen that the jejunal loop was herniated into this fossa and was strangulated.
In conclusion, based on the anatomic findings, these fossae or recesses, because of their size and topography, might play a role in the etiopathogenesis of internal abdominal hernias. Henceforth, the findings of the present study may help the abdominal surgeon to appreciate these recesses, which might prove to be quiet significant in differential diagnosis with cases of intestinal obstruction.
Acknowledgments
We express our sincerest thanks to the residents of the Anatomy, Forensic Medicine and Toxicology, General and Pediatric Surgery. We are grateful to Dr. A.K. Agarwal, Dean and Dr. J.M. Kaul, Director Professor and Head, Department of Anatomy, Maulana Azad Medical College, New Delhi for their guidance and permission to publish this work. Special thanks to Mrs. Swati Tambe for her unfailing support, guidance and encouragement.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Barberini F, Carone VS, Caggiati A, Macchiarelli G, Corner S. An unusual peritoneal fossa: anatomic report and clinical implications. Surg Radiol Anat. 1999;21:287–91. doi: 10.1007/BF01631402. [DOI] [PubMed] [Google Scholar]
- 2.Peltier J, Gars DL, Page C, Yzet T, Launde M. The duodenal fossae: anatomic study and clinical correlations. Surg Radiol Anat. 2005;27:303–7. doi: 10.1007/s00276-005-0332-9. [DOI] [PubMed] [Google Scholar]
- 3.Blachar A, Federle MP, Dodson SF. Internal hernia: clinical and imaging findings in 17 patients with emphasis on CT criteria. Radiology. 2001;218:68–74. doi: 10.1148/radiology.218.1.r01ja5368. [DOI] [PubMed] [Google Scholar]
- 4.Moynihan BGA. The Arris and Gale lectures on the anatomy and surgery of the peritoneal fossae. BMJ. 1899;1:522–5. doi: 10.1136/bmj.1.1992.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barberini F, Zani A, Ripani M, Di Nitto V, Brunone F. The complex arrangement of an “aorto-jejunal paraduodenal” fossa, as revealed by dissection of human posterior parietal peritoneum. Ann Anat. 2007;189:299–303. doi: 10.1016/j.aanat.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Takeyama N, Gokan T, Ohgiya Y, et al. CT of internal hernias. RadioGraphics. 2005;25:997–1015. doi: 10.1148/rg.254045035. [DOI] [PubMed] [Google Scholar]
- 7.Healy JC, Reznek RH. The peritoneum, mesenteries and omenta: normal anatomy and pathological processes. Eur Radiol. 1998;8:886–900. doi: 10.1007/s003300050485. [DOI] [PubMed] [Google Scholar]
- 8.Williams PL, Warwick R. Gray’s Anatomy. 36th ed. Edinburgh: Churchill Livingstone; 1980. pp. 1330–1. [Google Scholar]
- 9.Hirasaki S, Koide N, Shima Y, et al. Unusual variant of left paraduodenal hernia herniated into the mesocolic fossa leading to the jejunal strangulation. J Gastroenterol. 1998;33:734–8. doi: 10.1007/s005350050164. [DOI] [PubMed] [Google Scholar]
- 10.Decker G, du Plessis DJ. Lee McGregor’s Synopsis of Surgical Anatomy. 12th ed. Bombay: Varghese Publishing House; 1986. pp. 33–5. [Google Scholar]
- 11.Snell RS. Clinical anatomy by regions. 8th ed. New Delhi: Lippincott Williams and Wilkins; 2009. pp. 208–9. [Google Scholar]
- 12.Romanes GJ. Cunningham’s Mannual of Practical Anatomy. 5th ed. New York: Oxford University Press; 1986. p. 121. [Google Scholar]
- 13.Lee TKY, Voon FCT, Chow KW, Teo NH. Unusual variant of right paraduodenal hernia. Aust NZ J Surg. 1990;60:483–5. doi: 10.1111/j.1445-2197.1990.tb07408.x. [DOI] [PubMed] [Google Scholar]
- 14.Forgacs B, Istvan G, Sugar I, Ondrejka P. Uncommon case of incomplete left paraduodenal hernia. Magy Seb. 2003;56:243–6. [PubMed] [Google Scholar]
- 15.Patterson JA, Tadros EG, Wilkinson AJ. An unusual case of left paraduodenal hernia. Int J Clin Pract. 2001;55:649. [PubMed] [Google Scholar]
- 16.Ghahremani GG. Internal abdominal hernias. Surg Clin North Am. 1984;64:393–406. doi: 10.1016/s0039-6109(16)43293-7. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong O, Letessier E, Genier F, Lasserre P, Le Neel JC. Internal hernia: report of nine cases. Hernia. 1997;1:143–5. [Google Scholar]
- 18.Selcuk D, Kantarci F, Ogut G, Korman U. Radiological evaluation of internal abdominal hernias. Turk J Gastroenterol. 2005;16:57–64. [PubMed] [Google Scholar]
- 19.Kohli A, Choudhury HS, Rajput D. Internal hernia: a case report. Indian J Radiol Imaging. 2006;16:563–6. [Google Scholar]
- 20.Hansmann GH, Morton SA. Intra-abdominal hernia: report of case and review of the literature. Arch Surg. 1993;39:973–86. [Google Scholar]
- 21.Mall FP. Development of the human intestine and its position in the adult. Bull Johns Hopkins Hosp. 1898;9:197–208. [Google Scholar]
- 22.Frazer TE, Robbins RF. On the factors concerned in causing rotation of the intestine in man. J Anat Physiol. 1915;50:74–100. [PMC free article] [PubMed] [Google Scholar]