Abstract
This study describes specific patterns of elevated inflammatory proteins in clinical subtypes of myasthenia gravis (MG) patients. MG is a chronic, autoimmune neuromuscular disease with antibodies most commonly targeting the acetylcholine receptors (AChRab), which causes fluctuating skeletal muscle fatigue. MG pathophysiology includes a strong component of inflammation, and a large proportion of patients with early onset MG additionally present thymus hyperplasia. Due to the fluctuating nature and heterogeneity of the disease, there is a great need for objective biomarkers as well as novel potential inflammatory targets. We examined the sera of 45 MG patients (40 AChRab seropositive and 5 AChRab seronegative), investigating 92 proteins associated with inflammation. Eleven of the analysed proteins were significantly elevated compared to healthy controls, out of which the three most significant were: matrix metalloproteinase 10 (MMP-10; p = 0.0004), transforming growth factor alpha (TGF-α; p = 0.0017) and extracellular newly identified receptor for advanced glycation end-products binding protein (EN-RAGE) (also known as protein S100-A12; p = 0.0054). Further, levels of MMP-10, C-X-C motif ligand 1 (CXCL1) and brain derived neurotrophic factor (BDNF) differed between early and late onset MG. These novel targets provide valuable additional insight into the systemic inflammatory response in MG.
Myasthenia gravis (MG) is a chronic autoimmune disease, which is caused by antibodies against receptors at the neuromuscular junction. Disruption of neuromuscular transmission results in symptoms of fatigue in proximal skeletal muscles; predominantly facial, bulbar and limb muscles1,2. In approximately 85% of the patients, IgG1 antibodies are directed towards the nicotinic acetylcholine receptors (AChR+)3, while a smaller portion of MG patients possess IgG4 antibodies towards muscle specific tyrosine kinase (MuSK+)4 or low density lipoprotein receptor-related protein 4 (Lrp4)5. Patients who do not have detectable serum antibodies are termed seronegative. The antibody subtype is important to consider, since both symptoms and treatment response substantially differ between the different serological MG subgroups6. MG can be further subdivided into early onset (EOMG) or late onset (LOMG), depending on the age at which the patient first develops myasthenic symptoms. Although there is no absolute consensus at which age to draw the line between EOMG and LOMG7, the most commonly applied cut-off point for LOMG is 50 years of age. The distinction between EOMG and LOMG is important, since patients with LOMG may have a different disease course and typically do not present thymic hyperplasia, which is frequently seen in EOMG8.
As of yet, there are no circulating serum biomarkers that correlate with the disease state between patients or different MG subtypes9. The levels of AChR or MuSK antibodies generally do not correlate well with MG disease severity, neither between patients or inter-individually. Furthermore, clinical muscle fatigue may not be an entirely reliable parameter to follow in clinical trials due to expected fluctuations from one day to another, and even during the course of one day. Recently, microRNA (miRNA) have been described as potential biomarkers regarding miR-150-5p and miR-21-5p for AChR + MG10,11 and the let7 family for MuSK + patients12. Both miR-150-5p and miR-21-5p are involved in the regulation of the autoimmune response, and in particular the development of T- and B-cells. One recent study on inflammatory proteins in MG revealed significantly increased serum levels of a proliferation-inducing ligand (APRIL), and cytokines IL-19, IL-20, IL-28A and IL-35 in MG as compared with controls13. Otherwise, no previous study has focused on defining a broad inflammatory circulating protein profile in MG patients and in different clinical MG subtypes.
Due to the lack of knowledge regarding the inflammatory circulating protein profile in MG, we analysed 92 different proteins associated with inflammation. Further, we analysed protein expressions within the clinical subgroups EOMG vs. LOMG, immunosuppressive medication, gender and thymectomy.
Materials and Methods
Subjects
Sera from 45 MG patients (24 women) were collected at the Neurology Clinics of Jönköping County Hospital and Uppsala University Hospital, Sweden. Sera from healthy controls (HC), matched for age and sex, were collected at Uppsala University Hospital transfusion unit, Sweden. Diagnostic criteria of MG included objective muscle fatigue and neurophysiological evidence of disturbed neuromuscular transmission (decrement on repetitive nerve stimulation and/or increased jitter on single fibre electromyography), further supported by detection of AChR antibodies14. Clinical classification of MG status according to the Myasthenia Gravis Foundation of America (MGFA)15 included only ocular weakness (MGFA class I) and generalized weakness of mild (MGFA class II), moderate (MGFA class III) or severe (MGFA class IV) degree predominantly affecting limb or axial muscles (subtype A) or bulbar muscles (subtype B). Additionally, the degree of clinical MG fatigue was assessed at the time for serum sampling with the MG Composite scale (MGC; range 0–50)16 All subjects gave their written informed consent to participate in the study. Ethical approval was granted by the Ethics Committee of the Ryhov County Hospital, Jönköping (Dnr 2014/459-31) and Uppsala University Hospital, Uppsala (Dnr 2010/446), Sweden and all experiments were performed in accordance with relevant guidelines and regulations.
Protein analysis
The serum samples were analysed using the Olink Proseek Multiplex Inflammation I 96×96 kit (Olink Bioscience, Uppsala, Sweden), which analyses 92 human proteins related to inflammation and various inflammatory diseases (http://www.olink.com/proseek-multiplex/inflammation/). The analysis was performed at the Clinical Biomarkers Facility (Science for Life Laboratory, Uppsala, Sweden). The Proseek Multiplex analysis utilizes the Proximity Extension Assay (PEA) technology, as previously described17,18. In brief, antibodies labelled with oligonucleotide probes, bind in pairs to their specific target protein. These antibody pairs are linked to each other via their unique DNA oligonucleotide sequences, which hybridize when in proximity. The DNA sequences are then extended and amplified by quantitative real-time PCR. Details about data validation, limit of detection (LOD), specificity and reproducibility can be obtained via Olink’s website (http://www.olink.com/data-you-can-trust/validation/). Calibrator curves for correlating the normalized protein expression (NPX) values with actual concentrations are available at Olink’s website (http://www.olink.com/proseek-multiplex/inflammation/biomarkers/). A fold change value of at least 0.5 NPX is considered a biological difference, and not technical variation.
Statistical analysis
The data was log base 2 transformed for the analysis in order to obtain data more similar to a normal distribution. 73 out of the 92 proteins followed a normal distribution, and for these proteins, an unpaired Welch t-test was performed for comparison of the two groups (MG versus HC). For comparison of the proteins that were not normally distributed, a Mann- Whitney U test was performed. The False discovery rate method was applied to manage multiple test errors. To investigate whether gender had any effect on the protein expression, a two-way ANOVA analysis was performed. The MG patients were divided into three sub-groups, depending on (1) early onset (<50 years of age) versus late onset (≥50 years or age) MG; (2) thymectomy versus no thymectomy and; (3) current treatment with immunosuppressant medication versus no immunosuppressive therapy. An unpaired two-tailed Welch t-test was performed to test different subgroup analysis of protein expression. A p-value < 0.05 was considered significant. A non-parametric dynamic principal component analysis (PCA) was performed to identify possible clusters of the proteins that differed the most between MG and HC.
Results
Clinical characteristics of MG patients
Three samples (2 HC and 1 patient) were excluded due to unacceptable technical variations and thus, the final cohort consisted of 87 subjects, 44 MG patients (23 women) and 43 healthy controls (23 women). In the MG patient cohort, mean age was 63 ± 17 years (range 27–87 years) and mean disease duration was 14 ± 12 years (range 1–48 years). The cohort included 22 EOMG and 22 LOMG patients and overall median MGFA disease severity classification was mild MG (MGFA class II; Table 1). 39 patients had verified AChR antibodies whereas the remaining 5 patients were seronegative for AChR and MuSK antibodies. 18 patients had undergone thymectomy and 16 patients had current treatment with immunosuppressive medication. The mean MGC score was 7.0 ± 7.1 (range 0–34) (Table 1).
Table 1. Clinical data on the 45 MG patients included in the study.
| Age/sex | Disease dur | EOMG/LOMG | Tx | IS therapy during disease course | IS now | AChR+ | MGFA/MGC | Hist |
|---|---|---|---|---|---|---|---|---|
| 27/F | 3 | EOMG | No | None | No | Yes | IIIA/8 | NA |
| 29/F | 6 | EOMG | Yes | Pred | Yes | Yes | IIIB/17 | HP |
| 30/F | 2 | EOMG | No | None | No | Yes | IIA/5 | NA |
| 33/F | 17 | EOMG | Yes | None | No | Yes | I/5 | Missing |
| 34/F | 4 | EOMG | Yes | Pred | Yes | Yes | IIB/0 | HP |
| 35/F | 15 | EOMG | Yes | None | No | Yes | IIA/0 | HP |
| 39/F | 32 | EOMG | Yes | None | No | Yes | IIB/0 | HP |
| 46/F | 13 | EOMG | No | None | No | Yes | I/4 | NA |
| 49/F | 28 | EOMG | Yes | Pred, AZA | Yes | Yes | IIB/10 | NA |
| 49/F | 40 | EOMG | Yes | AZA | No | No | IIA/4 | Norm |
| 52/F | 11 | EOMG | Yes | CyA | Yes | Yes | IIA/0 | HP |
| 53/F | 19 | EOMG | Yes | AZA | Yes | Yes | IIB/14 | HP |
| 57/F | 34 | EOMG | Yes | None | No | Yes | IIB/9 | Missing |
| 61/F | 27 | EOMG | Yes | None | No | Yes | IIA/14 | HP |
| 66/F | 24 | EOMG | No | None | No | Yes | IIIB/17 | NA |
| 67/F | 19 | EOMG | Yes | Pred | Yes | Yes | IIB/12 | THY |
| 68/F | 48 | EOMG | No | None | No | Yes | IIB/11 | NA |
| 69/F | 41 | EOMG | Yes | Pred, AZA | No | Yes | IIA/0 | Missing |
| 73/F | 33 | EOMG | No | Pred, IvIg | Yes | No | I/5 | NA |
| 84/F | 2 | LOMG | No | AZA | Yes | Yes | IIB/8 | NA |
| 69/F | 11 | LOMG | No | None | No | No | IIA/13 | NA |
| 76/F | 1 | LOMG | No | None | No | Yes | IIIA/13 | NA |
| 86/F | 6 | LOMG | No | None | No | Yes | IIB/2 | NA |
| 42/M | 12 | EOMG | No | None | No | No | I/1 | NA |
| 56/M | 21 | EOMG | Yes | Pred, AZA, CyA | Yes | Yes | IIB/11 | HP |
| 59/M | 23 | EOMG | Yes | Pred, CyA | Yes | Yes | IIB/6 | THY |
| 59/M | 8 | LOMG | No | Pred | Yes | Yes | IIB/0 | NA |
| 66/M | 2 | LOMG | No | Pred, AZA, IvIg | Yes | Yes | IIIB/15 | NA |
| 69/M | 1 | LOMG | No | None | No | Yes | IIIA/13 | NA |
| 69/M | 6 | LOMG | No | Pred, AZA | Yes | Yes | IIB/3 | NA |
| 71/M | 8 | LOMG | Yes | None | No | Yes | IIA/3 | Norm |
| 71/M | 16 | LOMG | Yes | None | No | Yes | IIB/5 | THY |
| 73/M | 1 | LOMG | No | None | No | Yes | IIB/3 | NA |
| 74/M | 15 | LOMG | No | None | No | Yes | 0/0 | NA |
| 75/M | 6 | LOMG | No | Pred, AZA | Yes | Yes | 0/0 | NA |
| 76/M | 1 | LOMG | No | None | No | Yes | IIA/2 | NA |
| 78/M | 2 | LOMG | No | AZA | Yes | Yes | IIIB/18 | NA |
| 78/M | 10 | LOMG | Yes | Pred, AZA | Yes | Yes | 0/0 | Missing |
| 79/M | 13 | LOMG | No | Pred | No | Yes | IIA/2 | NA |
| 79/M | 19 | LOMG | No | None | No | No | 0/0 | NA |
| 80/M | 2 | LOMG | No | None | No | Yes | IIB/15 | NA |
| 86/M | 10 | LOMG | No | AZA | No | Yes | IIA/2 | NA |
| 87/M | 1 | LOMG | No | None | No | Yes | IVB/34 | NA |
| 87/M | 15 | LOMG | No | None | No | Yes | IIA/3 | NA |
Onset, age at onset of MG; Disease dur, duration in years from MG diagnosis; F, female; M, male; Disease dur, years from MG diagnosis; Tx, thymectomy; IS, immunosuppressive medication; pred, prednisone; AZA, azathioprine; IvIg, intravenous immunoglobulin; CyA, cyclosporine; MGFA, Myasthenia Gravis Foundation of America where 0, remission; I, ocular weakness, II, mild weakness, III, moderate weakness and IV severe weakness. MGC, myasthenia gravis composite score; Hist, thymus histology; NA, not applicable; Norm, normal; HP, hyperplasia; THY, thymoma.
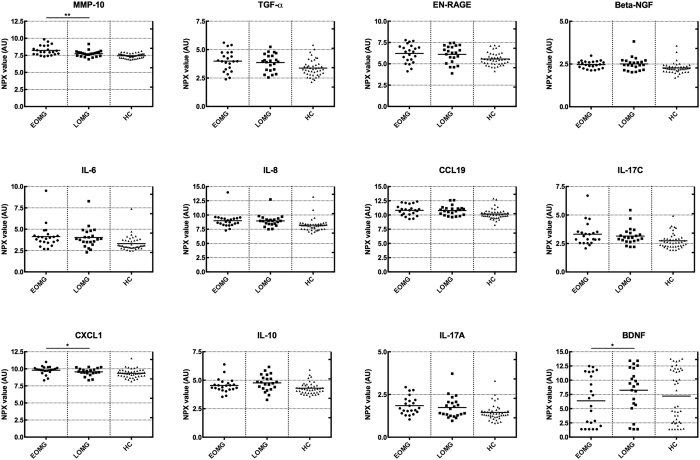
Elevated protein expressions in MG patients
The results from the assay are presented as normalized protein expression units (NPX), which are considered arbitrary units for each individual protein. Out of 92 assayed inflammatory proteins, 11 proteins were significantly elevated in the MG cohort (Table 2). The three proteins that were most significantly separated between MG patients and HC were matrix metalloproteinase 10 (MMP-10), transforming growth factor alpha (TGF-α) and extracellular newly identified receptor for advanced glycation end-products binding protein (EN-RAGE), all p < 0.01. The area under the curve (AUC) for these three inflammatory proteins was 0.76 for MMP-10 (Fig. 1A), 0.63 for TGF-α (Fig. 1B) and 0.66 for EN-RAGE (Fig. 1C). Thus, MMP-10 had the strongest association with MG. The PCA plot indicated tendency towards clustering in the HC group, although no absolute separation was present due to a greater dispersion in the MG patient group (Fig. 2). Other significantly increased levels of inflammatory proteins included nerve growth factor beta (β –NGF), cytokines IL-6, IL-8, IL-10 and IL-17A and C as well as chemokines C-C motif ligand 19 (CCL19) and C-X-C motif ligand 1 (CXCL1; Table 2). None of the investigated proteins had a lower expression in the MG group compared to HC group. Further, no significant correlation was found between any of the elevated proteins and clinical MGC score (Supplementary Table S1).
Table 2. Significantly increased levels of inflammatory proteins between MG patients and healthy controls.
| Protein | P-value |
|---|---|
| MMP-10 | 0.0004 |
| TGF-α | 0.0017 |
| EN-RAGE (Protein S100-A12) | 0.0054 |
| β -NGF | 0.0133 |
| IL-6 | 0.0220 |
| IL-8 | 0.0220 |
| CCL19 | 0.0220 |
| IL-17C | 0.0256 |
| CXCL1 | 0.0256 |
| IL-10 | 0.0256 |
| IL-17A | 0.0348 |
MMP-10, metalloproteinase 10; TGF-α, transforming growth factor alpha; EN-RAGE, extracellular newly identified receptor for advanced glycation end-products binding protein; β -NGF, nerve growth factor beta; IL, interleukin; CCL19, C-C motif ligand 19; CXCL1, C-X-C motif ligand 1.
Figure 1.
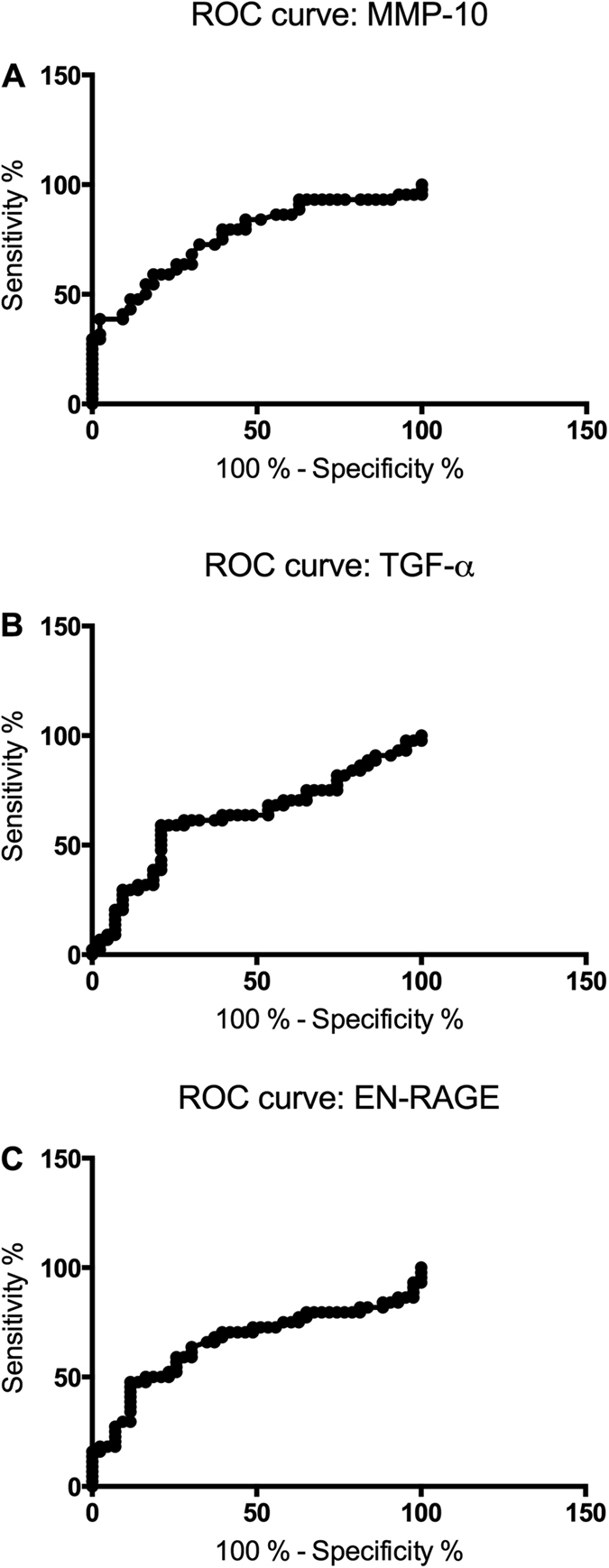
ROC curve of the three most significantly elevated proteins in sera of MG (myasthenia gravis) patients: MMP-10 (A), TGF-α (B) and EN-RAGE (C).
Figure 2. Dynamic three-dimensional principal component analysis (PCA) based on the three proteins with highest levels in MG patients: MMP-10, TGF-α and EN-RAGE.
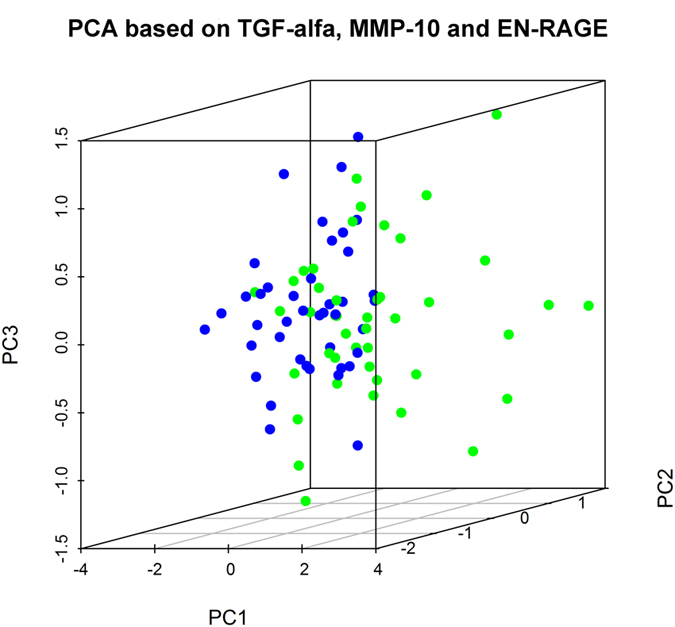
The PCA indicates a tendency for clustering in the MG patients. Blue, healthy controls (HC); green, myasthenia gravis (MG) patients.
Proteins associated with clinical MG subgroups
In the subgroup two-way ANOVA analysis, none of the proteins were expressed differently in female compared to male MG patients. Patients in the EOMG subgroup had significantly higher levels of MMP-10 (p = 0.0092; Fig. 3) as well as CXCL1 (p = 0.033; Fig. 3) compared to the LOMG group. Brain-derived neurotrophic factor (BDNF), although not significantly separated in the MG group as a whole, was markedly elevated in LOMG compared to EOMG patients (p = 0.0318; Fig. 3). No proteins were clearly separated in the subgroups of immunosuppressive medication or previous thymectomy. Although not significant, some other proteins were separated with at least 0.5 NPX difference between group means (Table 3).
Figure 3. NPX levels in the different subgroups: EOMG, early onset myasthenia gravis; LOMG, late onset myasthenia gravis; HC, healthy controls; AU, arbitrary units.
Lines indicate mean NPX value in each group. *p < 0.05, **p < 0.01. MMP-10, metalloproteinase 10; TGF-α, transforming growth factor alpha; EN-RAGE, extracellular newly identified receptor for advanced glycation end-products binding protein; beta-NGF, nerve growth factor beta; IL, interleukin; CCL19, C-C motif ligand 19; CXCL1, C-X-C motif ligand 1; BDNF, brain-derived neurotrophic factor.
Table 3. Separated proteins (> 0.5 NPX fold change of log2 data) between the different subgroups.
| Increased NPX for patients w/o Tx | Tx | No Tx | Fold change |
|---|---|---|---|
| BDNF | 6.3 | 8.0 | 1.7 |
| CXCL9 | 8.1 | 8.9 | 0.8 |
| Increased NPX for patients w/o IS | Current | None | Fold change |
| CXCL11 | 8.3 | 9.1 | 0.7 |
| FGF-19 | 9.0 | 9.6 | 0.7 |
| 4E-BP1 | 5.9 | 6.6 | 0.6 |
| TNFSF14 | 4.4 | 5.0 | 0.6 |
| SIRT2 | 4.4 | 4.9 | 0.6 |
| CCL4 | 7.2 | 7.8 | 0.6 |
BDNF, brain-derived neurotrophic factor; CXCL9, C-X-C motif chemokine 9; CXCL11, C-X-C motif chemokine 11; FGF-19, Fibroblast growth factor 19; 4E-BP1, Eukaryotic translation initiation factor; TNFSF14, 4E-binding protein 1; SIRT2, SIR2-like protein 2; CCL4, C-C motif chemokine 4. Tx, thymectomy; IS, immunosuppressive medication.
Discussion
In this study, we found that 11 of the 92 different inflammatory proteins were elevated in the sera of MG patients. The fact that the dispersion of inflammatory proteins was greater in the MG group than the control group was largely expected, due to the heterogeneous nature of MG, with several subgroups and different clinical presentations. The protein that was most strongly associated with MG was MMP-10, also known as Stromelysin-2, which is a member of the metalloproteinase family. Metalloproteinases enzymatically break down the extracellular matrix, resulting in degradation of collagens, fibronectin and gelatines, both in physiological and disease processes. One previous study linked elevated serum levels of MMP-10 to sepsis in human patients19. Another study found that levels of MMP-10, secreted by microglia and macrophages, were considerably elevated in experimental autoimmune encephalomyelitis (EAE), which is an animal model for multiple sclerosis, and that these levels correlated with the severity of symptoms20. The model of EAE has many similarities to the animal model of experimental autoimmune MG (EAMG), for example in its response to immunomodulators21.
TGF-α is a growth factor that has important roles for epithelial proliferation and differentiation, mediated through its receptor the epidermal growth factor receptor (EGFR). TGF-α is mainly produced in macrophages, neurons, astrocytes and keratinocytes. Stimulation of proliferation via the EGFR signalling pathway results in inhibition of apoptosis and angiogenesis. Further, TGF-α has neurotrophic characteristics, such as stimulating proliferation and differentiation of neural precursor cells in the developing brain, and is able to stimulate proliferation in rat brain after stroke22. TGF-α also reduces the infarct size following stroke in mice, and stimulates angiogenesis and neurogenesis23. Although this neurotrophic role of TGF-α is known in the brain, nothing is so far known of its role in the peripheral nervous system.
EN-RAGE, also known as protein S100-A12, is a protein that binds to calcium, zinc and copper. Just like MMP-10 and TGF-α, EN-RAGE is involved in the cell cycle progression and differentiation and intriguingly this protein actually inhibits metalloproteinases. Additionally, EN-RAGE possesses pro-inflammatory properties, and is involved in inflammation by activating mast cells and monocytes. Further, EN-RAGE is induced by TNF-α in neutrophils and is upregulated by IL-6 in macrophages24. Previous studies proved that IL-6 is upregulated in thymic epithelial cells in MG patients25 and impaired expression of IL-6 among other cytokines is believed to play a role in the inflammatory response in MG26. EN-RAGE is a ligand for the receptor for advanced glycation end products (RAGE), a well-known pro-inflammatory receptor that is involved in diabetic neuropathy, cardiovascular disorders and neuroinflammatory and neurodegenerative disorders27,28. Binding of EN-RAGE to RAGE activates the transcription factor NF-κB, induces secretion of cytokines and has pro-inflammatory effects on lymphocytes, neutrophils and endothelial cells29.
β-NGF is another well-known protein, which belongs to the neurotrophin family. It is important for the survival and development of neurons in both the central nervous system (CNS) and the peripheral nervous system (PNS). However, it also has a role in the inflammatory response due to its release by T- and B-cells, mast cells, eosinophils and macrophages. β-NGF participates in a complex network of inflammation, being upregulated by inflammatory cytokines, activating inflammatory cells and stimulating further cytokine release as well as chemotaxis30.
Interleukins are well-known regulators of the inflammatory response in autoimmune diseases. Both IL-6 and IL-10 are produced by activated B cells (as well as T-cells), and affects macrophages as well as immunoregulatory T-cells31,32 and B-cells. IL-6 is particularly important for the development of the autoimmune response in EAMG33, by stimulating the development of Th17 cells. Th17 cells in turn secrete the cytokine IL-17A32, and a recent study found that plasma levels of IL-17A were increased in MG patients and that higher levels of IL-17A correlated with greater severity of the disease34. Furthermore, another study presented evidence that serum levels of IL-17 correlates with the AChR antibody titre35. IL-17C, another member of the IL-17 family, has not previously been linked to MG. Nevertheless, IL-17C is important in the development of EAE, and in regulating the autoimmune response through its receptor, IL-17E, which is highly expressed in Th17 cells36. Our data support the previous report on upregulation of the pro-inflammatory cytokine IL-8 in the sera of MG patients37. IL-8 is known to attract neutrophils and T-cells and has been linked to the occurrence of thymoma in MG patients38. In line with previous studies, our findings further validate the importance of these inflammatory cytokines in MG and emphasize the possibility that they could serve as targets for more specific novel MG treatments.
CCL19 is a cytokine that is secreted by medullary thymic epithelial cells and promotes migration of T-cells towards the medullary zone, as well as exporting mature thymocytes towards the periphery. CCL19, along with chemokine CCL21, is known to be upregulated in the thymus of MG patients with thymic hyperplasia39. Even though CCL21 was not included in our assay, our data support previous findings of the important role of CCL19 also in the circulation of MG patients. Another chemokine that was upregulated in the sera of MG patients is CXCL1, which stimulates chemotaxis of neutrophils and is produced by several cells in the immune system, such as macrophages and neutrophils40,41. Intriguingly, CXCL1 and IL-8 share the same receptor, CXCR2, which is present on mast cells, neutrophils, basophils and T-cells42. CXCR2 knockout mice present with defect neutrophil recruitment in wounds and delayed healing of wounds43. The fact that two ligands for CXCR2 are both elevated in the sera of MG patients reinforces the possibility that CXCR2 plays a crucial part in the autoimmune response in MG patients.
In the sub-group comparing onset of MG, patients with LOMG had almost four times higher levels of BDNF than the patients with EOMG. The ratio was almost the same when comparing patients who underwent thymectomy with those who did not. This was expected, since patients with LOMG are rarely treated with thymectomy unless they have a thymoma. Hence, the reason for the different BDNF levels is most likely due to the thymus differences between EOMG and LOMG, rather than effects from the thymectomy. Since BDNF is a neurotrophic protein, it is essential for differentiation and growth of neurons both in the CNS and the PNS. Notably, pro-inflammatory cytokines actually cause a reduction of BDNF gene expression44. One possible explanation for the higher levels of BDNF in patients with LOMG could be that their disease is less driven by inflammation compared to EOMG. The fact that EOMG patients more often have thymus hyperplasia and more effect of thymectomy is in conjunction with this finding. However, apart from neurons, inflammatory cells also produce BDNF, which may serve a neuroprotective role during inflammation45. Furthermore, BDNF also plays an important role in late-phase long-term potentiation and long-term memory storage46,47. Previous studies indicate that a fraction of MG patients do suffer spatial, logical and visual memory deficits, probably due to impaired cholinergic signaling in the CNS, since AChR antibodies are also found in the cerebrospinal fluid48. Impaired expression of BDNF could also be a possible reason for the cognitive deficits in some MG patients49.
Since the results from this protein panel are expressed in arbitrary units, the protein levels cannot be compared to other proteins, or even to the same protein in another assay due to usage of different batches of antibodies. This may be considered a drawback of the method, and thus limits the potential of this particular protein assay in its role to identify possible biomarkers for treatment response or inflammatory activity. The fact that many patients had current treatment with immunosuppressive treatment could also lower the levels of certain circulatory inflammatory proteins. Nevertheless, these findings provide valuable insight into the role of inflammatory mechanisms in MG pathophysiology.
In summary, we found eleven elevated inflammatory proteins in the sera of MG patients. These proteins, out of which MMP-10, TGF-α and EN-RAGE were the most significant, all have possible functions as new biomarkers of inflammatory activity, and possibly treatment response in MG.
Additional Information
How to cite this article: Molin, C. J. et al. Profile of upregulated inflammatory proteins in sera of Myasthenia Gravis patients. Sci. Rep. 7, 39716; doi: 10.1038/srep39716 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
The authors are grateful to Dr. Marta Lewandowska for proofreading the manuscript and to Emil Nilsson, Olink, for statistical discussion. This study was supported by funds from Futurum (FUTURUM-520281), Swedish Society of Medicine (SLS-330141), Neuroförbundet (NEURO Sweden), Selanders memorial foundation and by the Swedish Research Council (VR-523-2014-2048).
Footnotes
Author Contributions Study concept and design: A.R.P. and E.W. Data acquisition: E.W. and A.R.P. Analysis and data interpretation: C.J.M. and A.R.P. Drafting of the manuscript: C.J.M. and E.W. Critical revision of the manuscript: A.R.P. All authors reviewed and approved the final version of the manuscript.
References
- Gradolatto A. et al. Defects of immunoregulatory mechanisms in myasthenia gravis: role of IL-17. Ann N Y Acad Sci 1274, 40–7 (2012). [DOI] [PubMed] [Google Scholar]
- Meriggioli M. N. & Sanders D. B. Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity. Lancet Neurol 8, 475–90 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent A. & Newsom-Davis J. Acetylcholine receptor antibody as a diagnostic test for myasthenia gravis: results in 153 validated cases and 2967 diagnostic assays. J Neurol Neurosurg Psychiatry 48, 1246–52 (1985). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoch W. et al. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nat Med 7, 365–8 (2001). [DOI] [PubMed] [Google Scholar]
- Higuchi O., Hamuro J., Motomura M. & Yamanashi Y. Autoantibodies to low-density lipoprotein receptor-related protein 4 in myasthenia gravis. Ann Neurol 69, 418–22 (2011). [DOI] [PubMed] [Google Scholar]
- Gilhus N. E. & Verschuuren J. J. Myasthenia gravis: subgroup classification and therapeutic strategies. Lancet Neurol 14, 1023–36 (2015). [DOI] [PubMed] [Google Scholar]
- Binks S., Vincent A. & Palace J. Myasthenia gravis: a clinical-immunological update. J Neurol 263, 826–34 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx A. et al. The different roles of the thymus in the pathogenesis of the various myasthenia gravis subtypes. Autoimm Rev 12, 875–84 (2013). [DOI] [PubMed] [Google Scholar]
- Benatar M., Sanders D. B., Wolfe G. I., McDermott M. P. & Tawil R. Design of the efficacy of prednisone in the treatment of ocular myasthenia (EPITOME) trial. Ann N Y Acad Sci 1275, 17–22, (2012). [DOI] [PubMed] [Google Scholar]
- Punga A. R., Andersson M., Alimohammadi M. & Punga T. Disease specific signature of circulating miR-150-5p and miR-21-5p in myasthenia gravis patients. J Neurol Sci 356, 90–6 (2015). [DOI] [PubMed] [Google Scholar]
- Punga T. et al. Circulating miRNAs in myasthenia gravis: miR-150-5p as a new potential biomarker. Ann Clin Transl Neurol 1, 49–58 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punga T. et al. Disease specific enrichment of circulating let-7 family microRNA in MuSK+ myasthenia gravis. J Neuroimmunol 292, 21–6 (2016). [DOI] [PubMed] [Google Scholar]
- Uzawa A. et al. Changes in inflammatory cytokine networks in myasthenia gravis. Sci Rep 6, 25886, doi: 10.1038/srep25886 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillane J., Beeson D. J. & Kullmann D. M. Myasthenia and related disorders of the neuromuscular junction. J Neurol Neurosurg Psychiatry 81, 850–7 (2010). [DOI] [PubMed] [Google Scholar]
- Jaretzki A. 3rd et al. Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Neurology 55, 16–23 (2000). [DOI] [PubMed] [Google Scholar]
- Burns T. M., Conaway M. & Sanders D. B. The MG Composite: A valid and reliable outcome measure for myasthenia gravis. Neurology 74, 1434–40 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assarsson E. et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PloS One 9, e95192, doi: 10.1371/journal.pone.0095192 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundberg M., Eriksson A., Tran B., Assarsson E. & Fredriksson S. Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood. Nucleic Acids Res 39, e102, doi: 10.1093/nar/gkr424 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorente L. et al. Matrix metalloproteinase-9, -10, and tissue inhibitor of matrix metalloproteinases-1 blood levels as biomarkers of severity and mortality in sepsis. Crit Care 13, R158, doi: 10.1186/cc8115 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toft-Hansen H., Nuttall R. K., Edwards D. R. & Owens T. Key metalloproteinases are expressed by specific cell types in experimental autoimmune encephalomyelitis. J Immunol 173, 5209–18 (2004). [DOI] [PubMed] [Google Scholar]
- Karussis D. M. et al. Immunomodulation of experimental autoimmune myasthenia gravis with linomide. J Neuroimmunol 55, 187–93 (1994). [DOI] [PubMed] [Google Scholar]
- Guerra-Crespo M. et al. Transforming growth factor-alpha induces neurogenesis and behavioral improvement in a chronic stroke model. Neuroscience 160, 470–83 (2009). [DOI] [PubMed] [Google Scholar]
- Leker R. R. et al. Transforming growth factor alpha induces angiogenesis and neurogenesis following stroke. Neuroscience 163, 233–43 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyette J. & Geczy C. L. Inflammation-associated S100 proteins: new mechanisms that regulate function. Amino Acids 41, 821–42 (2011). [DOI] [PubMed] [Google Scholar]
- Cohen-Kaminsky S. et al. High IL-6 gene expression and production by cultured human thymic epithelial cells from patients with myasthenia gravis. Ann N Y Acad Sci 681, 97–9 (1993). [DOI] [PubMed] [Google Scholar]
- Yilmaz V. et al. Differential Cytokine Changes in Patients with Myasthenia Gravis with Antibodies against AChR and MuSK. PloS One 10, e0123546, doi: 10.1371/journal.pone.0123546 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuah Y. K., Basir R., Talib H., Tie T. H. & Nordin N. Receptor for advanced glycation end products and its involvement in inflammatory diseases. Int J Inflam 2013, 403460, doi: 10.1155/2013/403460 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R., Juranek J. K. & Rai V. RAGE axis in neuroinflammation, neurodegeneration and its emerging role in the pathogenesis of amyotrophic lateral sclerosis. Neurosci Biobehav Rev 62, 48–55 (2016). [DOI] [PubMed] [Google Scholar]
- Pietzsch J. & Hoppmann S. Human S100A12: a novel key player in inflammation? Amino Acids 36, 381–9 (2009). [DOI] [PubMed] [Google Scholar]
- Freund V. & Frossard N. Expression of nerve growth factor in the airways and its possible role in asthma. Prog Brain Res 146, 335–46 (2004). [DOI] [PubMed] [Google Scholar]
- Dalakas M. C. Invited article: inhibition of B cell functions: implications for neurology. Neurology 70, 2252–60 (2008). [DOI] [PubMed] [Google Scholar]
- Dalakas M. C. Future perspectives in target-specific immunotherapies of myasthenia gravis. Ther Adv Neurol Disord 8, 316–27 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aricha R., Mizrachi K., Fuchs S. & Souroujon M. C. Blocking of IL-6 suppresses experimental autoimmune myasthenia gravis. J Autoimmun 36, 135–41 (2011). [DOI] [PubMed] [Google Scholar]
- Xie Y. et al. Elevated plasma interleukin-17A in a subgroup of Myasthenia Gravis patients. Cytokine 78, 44–6 (2016). [DOI] [PubMed] [Google Scholar]
- Roche J. C. et al. Increased serum interleukin-17 levels in patients with myasthenia gravis. Muscle Nerve 44, 278–80,(2011). [DOI] [PubMed] [Google Scholar]
- Chang S. H. et al. Interleukin-17C promotes Th17 cell responses and autoimmune disease via interleukin-17 receptor E. Immunity 35, 611–21 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chunjie N., Huijuan N., Zhao Y., Jianzhao W. & Xiaojian Z. Disease-specific signature of serum miR-20b and its targets IL-8 and IL-25, in myasthenia gravis patients. Eur Cytokine Netw 26, 61–6 (2015). [DOI] [PubMed] [Google Scholar]
- Uzawa A., Kawaguchi N., Himuro K., Kanai T. & Kuwabara S. Serum cytokine and chemokine profiles in patients with myasthenia gravis. Clin Exp Immunol 176, 232–7 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrih-Aknin S. et al. CCL21 overexpressed on lymphatic vessels drives thymic hyperplasia in myasthenia. Ann Neurol 66, 521–31 (2009). [DOI] [PubMed] [Google Scholar]
- Moser B., Clark-Lewis I., Zwahlen R. & Baggiolini M. Neutrophil-activating properties of the melanoma growth-stimulatory activity. J Exp Med 171, 1797–1802 (1990). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iida N. & Grotendorst G. R. Cloning and sequencing of a new gro transcript from activated human monocytes: expression in leukocytes and wound tissue. Mol Cell Biol 10, 5596–9 (1990). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippert U. et al. Expression and functional activity of the IL-8 receptor type CXCR1 and CXCR2 on human mast cells. J Immunol 161, 2600–8 (1998). [PubMed] [Google Scholar]
- Devalaraja R. M. et al. Delayed wound healing in CXCR2 knockout mice. J Invest Dermatol 115, 234–44 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese F. et al. Brain-derived neurotrophic factor: a bridge between inflammation and neuroplasticity. Front Cell Neurosci 8, 430, doi: 10.3389/fncel.2014.00430 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerschensteiner M. et al. Activated human T cells, B cells, and monocytes produce brain-derived neurotrophic factor in vitro and in inflammatory brain lesions: a neuroprotective role of inflammation? J Exp Med 189, 865–70 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekinschtein P. et al. BDNF is essential to promote persistence of long-term memory storage. Proc Natl Acad Sci USA 105, 2711–6 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y., Christian K. & Lu B. BDNF: a key regulator for protein synthesis-dependent LTP and long-term memory? Neurobiol Learn Mem 89, 312–23 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohbot V. D., Jech R., Bures J., Nadel L. & Ruzicka E. Spatial and nonspatial memory involvement in myasthenia gravis. J Neurol 244, 529–32 (1997). [DOI] [PubMed] [Google Scholar]
- Paul R. H., Cohen R. A., Gilchrist J. M., Aloia M. S. & Goldstein J. M. Cognitive dysfunction in individuals with myasthenia gravis. J Neurol Sci 179, 59–64 (2000). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.