Abstract
INTRODUCTION:
Injury to the inferior epigastric artery (IEA) has been reported following lower abdominal wall surgical incisions, abdominal peritoneocentesis and trocar placements at laparoscopic port sites, resulting in the formation of abdominal wall haematomas that may expand considerably due to lack of tissue resistance. The aim of this study was to localise its course in relation to standard anatomic landmarks and suggest safe areas for performance of invasive procedures.
MATERIALS AND METHODS:
Sixty IEAs of 30 adult cadavers (male = 19; female = 11) were dissected and the course of the IEA noted in relation to the mid-inguinal point, anterior superior iliac spine (ASIS) and umbilicus.
RESULTS:
The mean distance of the IEA from the midline was 4.45 ± 1.42 cm at the level of the mid-inguinal point, 4.10 ± 1.15 cm at the level of ASIS and 4.49 ± 1.15 cm at the level of umbilicus. There was an average of 3.3 branches per IEA with more branches arising from its lateral aspect. The IEA was situated within one-third (32%) of the distance between the midline and the sagittal plane through ASIS at all levels.
CONCLUSION:
To avoid injury to IEA, trocars can be safely inserted 5.5 cm [mean + 1 standard deviation (SD)] away from the midline (or) slightly more than one-third of the distance between the midline and a sagittal plane running through ASIS. These findings may be useful not only for laparoscopic procedures but also for image-guided biopsy, abdominal paracentesis, and placement of abdominal drains.
Key words: Anterior abdominal wall, inferior epigastric artery (IEA), invasive procedure, laparoscopy
INTRODUCTION
The inferior epigastric artery (IEA) is a major blood vessel that supplies the anterior abdominal wall. It arises from the external iliac artery, proximal to the inguinal ligament. Soon thereafter it ascends on the anterior abdominal wall medial to the deep inguinal ring.[1] After piercing the transversalis fascia, the IEA enters the rectus sheath ascending posterior to the rectus abdominis muscle. In the lower abdomen, the IEA raises a fold of parietal peritoneum called the lateral umbilical ligament. Injury to the IEA has been reported following lower abdominal wall surgical incisions, abdominal peritoneocentesis and trocar placements at laparoscopic port sites resulting in the formation of abdominal wall haematomas that may expand considerably due to lack of tissue resistance. Trocar insertion has been reported to rarely cause injury to major blood vessels such as the inferior vena cava, aorta and iliac vessels. Recent studies have shown that the rate of injury to the major blood vessels mentioned above is 0.02-0.04%[2] and 0.01-0.07%[3], respectively. These injuries result in considerable morbidity and mortality, requiring immediate surgical repair. Trauma to the IEA is more common and reported in about 0.2-2% of laparoscopic procedures.[4] The aim of this study was to localise the course of IEA in relation to standard reproducible anatomic landmarks and suggest safe areas for the performance of invasive procedures such as placement of trocars in laparoscopy. Understanding the course of IEA would also help in minimising the likelihood of injury.[5]
MATERIALS AND METHODS
The study was done after obtaining formal permission from the Institutional Review Board. The course and branching pattern of 60 IEAs of 30 adult cadavers (male = 19; female = 11) were studied. The anterior abdominal wall was incised bilaterally along the costal margin, from the xiphoid process up to the anterior axillary line. The incision was further extended inferiorly medial to the anterior superior iliac spine (ASIS). The entire anterior abdominal wall was reflected forwards as a flap. The parietal peritoneum and posterior wall of rectus sheath was reflected to expose the course and branches of IEA. Yellow-coloured pins were inserted through the anterior abdominal wall along the course of the IEA, and pink-coloured pins inserted along the lateral border of rectus abdominis muscle (LRA). The abdominal wall was then reverted to its normal anatomical position [Figure 1]. The following parameters were measured:
Figure 1.

Anterior abdominal wall with yellow pins inserted along the course of the IEA and pink pins along the LRA
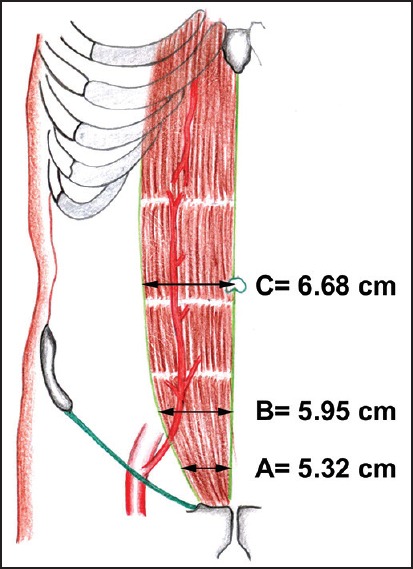
Distance from midline to LRA at the level of mid-inguinal point (A), ASIS (B) and umbilicus (C) [Figure 2].
Distance from midline to IEA at the level of mid-inguinal point (D), ASIS (E) and umbilicus (F) [Figure 3].
Distance from midline to a sagittal plane through ASIS (G).
The distance from midline to IEA and that from midline to LRA at the three levels, were divided by the distance from midline to ASIS and expressed as a ratio, to correct for variable body build.
The larger branches of the IEA (approx. size >1 mm) were noted and their course traced.
Figure 2.
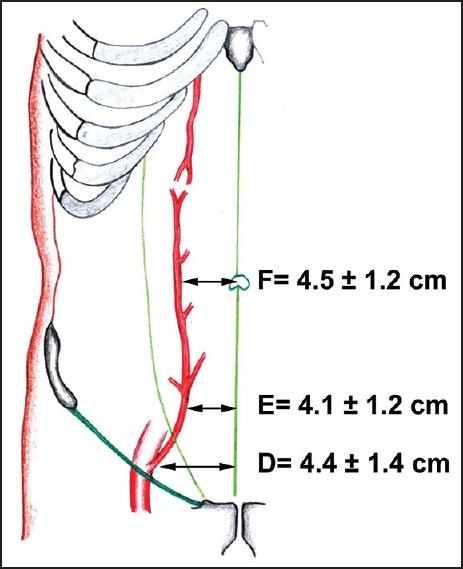
Course of the IEA, and the mean distance from midline to IEA at the three levels
Figure 3.
Rectus abdominis muscle, and the mean distance from midline to LRA at the three levels
All data were entered into Excel workbook sheets (Microsoft Office Excel; version 2007, Microsoft® Corporation, Washington, USA) and analysed using SPSS (version 16.0, SPSS Inc., Chicago, IL, USA). The measured parameters and ratios were summarised as mean and standard deviation (SD). The Mann–Whitney test was used to compare mean values between the sexes. The independent sample t test was used to compare mean values between the left and right sides. Bivariate correlation was done between various sets of variables and Pearson's correlation coefficient obtained to identify any correlation, if present.
RESULTS
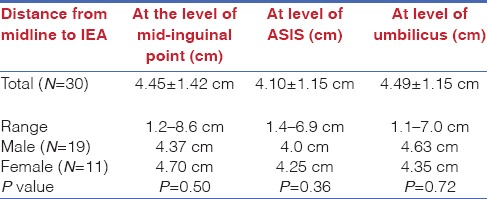
In 28% of cases, the IEA ended below the level of umbilicus. Of the remaining 72%, the IEA coursed upwards and medially in 44%, and upwards and slightly laterally in 56%. The mean distances from midline to IEA at the three levels are shown in Table 1 and Figure 3. The mean distance from midline to IEA at the level of mid-inguinal point (D) was 4.45 ± 1.42 cm (range = 1.2-8.6 cm; female = 4.70 cm, male = 4.37 cm; P = 0.50). The mean distance from midline to IEA at the level of ASIS (E) was 4.10 ± 1.15 cm (range = 1.4-6.9 cm; female = 4.25 cm, male = 4.0 cm; P = 0.36). The mean distance from midline to IEA at the level of umbilicus (F) was 4.49 ± 1.15 cm (range = 1.1-7.0 cm; female = 4.35 cm, male = 4.63; P = 0.72). There is no significant difference between the positions of IEA between the sides or the sexes [Table 1].
Table 1.
Mean distance from midline to IEA at the three levels in the total group and in the sexes
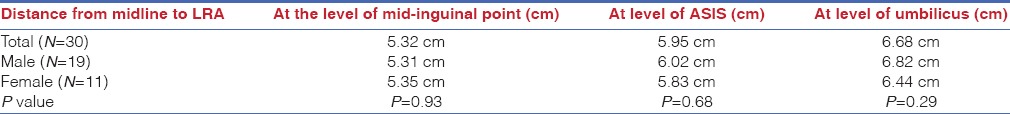
The mean distance from midline to LRA at the three levels is shown in Table 2 and Figure 2. The mean distance from midline to LRA at the level of mid-inguinal point (A) was 5.32 cm (female = 5.35 cm, male = 5.31 cm; P = 0.93). The mean distance from midline to LRA at the level of ASIS (B) was 5.95 cm (female = 5.83 cm, male = 6.02 cm; P = 0.68). The mean distance from midline to LRA at the level of umbilicus (C) was 6.68 cm (female = 6.44 cm, male = 6.82 cm; P = 0.29).
Table 2.
Mean distance from midline to LRA at three levels in the total group and in the sexes
Larger branches of the IEA (size >1 mm) were studied. There was an average of 3.3 branches per IEA. More branches arose from its lateral aspect (1.9 branches per IEA) than its medial side (1.4 branches/per IEA). The supra-umbilical portion of IEA gave very few branches from its lateral aspect and almost no branch from its medial aspect. All lateral branches were contained within the rectus sheath. In 20% of cases, a large medial branch ran parallel to the IEA. In 10% of cases, these medial branches crossed the midline. The main trunk of IEA entered the rectus sheath below the level of ASIS [Figure 3].
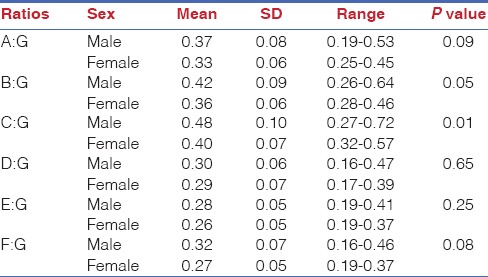
To correct for variable body build, ratios were calculated by dividing the measured parameters D, E, F by the distance from midline to ASIS (G) [Table 3]. Correlation analysis was done between the ratios D/G, E/G, F/G and the distance of IEA from the midline at the three levels. There was significant positive correlation between them. As the ratios D/G, E/G and F/G increased, there was a linear increase in the distance from midline to IEA at the three levels. The IEA was situated within one-third (32%) of the distance between midline and the sagittal plane through ASIS at all three levels [Table 3]. The LRA, however, moved from one-third of the distance between midline and the sagittal plane at ASIS at the level of mid-inguinal point, to about half (48%) of it at the level of umbilicus [Table 3].
Table 3.
Comparison of ratios between male and female cadavers
DISCUSSION
Very few studies have shown the course and position of IEA with relevance to invasive procedures of the anterior abdominal wall. No studies have been done in the Indian context. We had done a similar study on the course of IEA in 50 computed tomography (CT) angiograms and found that the mean distance of the IEA from the midline was 5.17 ± 0.93 cm at the level of mid-inguinal point, 4.57 ± 1.05 cm at the level of ASIS and 5.27 ± 1.17 cm at the level of umbilicus. There was a definitive predictive pattern in the course of the artery as seen in correlation and regression analysis.[6] Epstein et al. in their study of 30 cadavers (18 female and 12 male) found that the IEA ran vertically throughout its course in the anterior abdominal wall.[7] In our study, the IEA terminated below the level of umbilicus in 28% of cases. In the remaining 72%, the IEA coursed upwards and slightly medially in 44%, and upwards and slightly laterally in 56%. Rahn et al. in their study of 11 cadavers found the IEA was 3.7 cm (range = 2.6-5.5 cm) from the midline at the level of ASIS,[8] whereas in our study, the IEA was found 4.10 cm (range = 1.4-6.9 cm) from the midline. The difference could be attributed to racial variation in body build. We found an average of 3.3 branches per IEA. Heitmann et al. similarly described 1-2 branches per IEA, which were over 1 mm in diameter.[9] Hoeing et al. described 3-6 branches per IEA, but the author studied branches even less than 1 mm in diameter.[10] We found a large medial branch that ran parallel to the main trunk of IEA in 20% of cases. Studies done by Epstein et al. and Milloy et al. also showed a similar large medial branch in 29% and 14% of cases, respectively.[7,11]
CONCLUSION
In conclusion, we suggest safe areas for performance of invasive abdominal procedures based on our study. To avoid injury to the IEA, trocars can be safely inserted at 5.5 cm (mean + 1 SD) away from the midline (or) more than one-third of the distance between the midline and a sagittal plane through ASIS [Figure 2]. These findings may be useful not only for laparoscopic procedures but also for image-guided biopsy, abdominal paracentesis, and placement of abdominal drains.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Standring S. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 40th ed. China: Churchill Livingstone Elsevier; 2008. p. 1056. [Google Scholar]
- 2.Philips PA, Amaral JF. Abdominal access complications in laparoscopic surgery. J Am Coll Surg. 2001;192:525–36. doi: 10.1016/s1072-7515(01)00768-2. [DOI] [PubMed] [Google Scholar]
- 3.Hanney RM, Alle KM, Cregan PC. Major vascular injury and laparoscopy. Aust N Z J Surg. 1995;65:533–5. doi: 10.1111/j.1445-2197.1995.tb01800.x. [DOI] [PubMed] [Google Scholar]
- 4.Aharoni A, Condrea A, Leibovitz Z, Paz B, Levitan Z. A comparative study of Foley catheter and suturing to control trocar-induced abdominal wall haemorrhage. Gynaecol Endosc. 1997;6:31–2. [Google Scholar]
- 5.Balzer KM, Witte H, Recknagel S, Kozianka J, Waleczek H. Anatomic guidelines for the prevention of abdominal wall hematoma induced by trocar placement. Surg Radiol Anat. 1999;21:87–9. doi: 10.1007/s00276-999-0087-9. [DOI] [PubMed] [Google Scholar]
- 6.Joy P, Simon B, Prithishkumar IJ, Isaac B. Topography of inferior epigastric artery relevant to laparoscopic surgery: A CT angiographic study. Surg Radiol Anat. 2015 doi: 10.1007/s00276-015-1513-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Epstein J, Arora A, Ellis H. Surface anatomy of the inferior epigastric artery in relation to laparoscopic injury. Clin Anat. 2004;17:400–8. doi: 10.1002/ca.10192. [DOI] [PubMed] [Google Scholar]
- 8.Rahn DD, Phelan JN, Roshanravan SM, White AB, Corton MM. Anterior abdominal wall nerve and vessel anatomy: Clinical implications for gynecologic surgery. Am J Obstet Gynecol. 2010;202:234.e1–5. doi: 10.1016/j.ajog.2009.10.878. [DOI] [PubMed] [Google Scholar]
- 9.Heitmann C, Felmerer G, Durmus C, Matejic B, Ingianni G. Anatomical features of perforator blood vessels in the deep inferior epigastric perforator flap. Br J Plast Surg. 2000;53:205–8. doi: 10.1054/bjps.1999.3257. [DOI] [PubMed] [Google Scholar]
- 10.Hoenig SJ, Hodin RA, Novak G, Cohn WE. Videoscopic harvest of the inferior epigastric artery. Ann Thorac Surg. 1999;67:565–6. doi: 10.1016/s0003-4975(98)01294-6. [DOI] [PubMed] [Google Scholar]
- 11.Milloy FJ, Anson BJ, Mcafee DK. The rectus abdominis muscle and the epigastric arteries. Surg Gynecol Obstet. 1960;110:293–302. [PubMed] [Google Scholar]


