Abstract
Introduction
This article presents an integrative review of the literature examining the relationship between racial discrimination and adverse birth outcomes.
Methods
Searches for research studies published from 2009 to 2015 were conducted using PubMed, CINAHL, Scopus, PsycINFO, Web of Science, and Embase. Articles were assessed for potential inclusion using the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) 2009 framework.
Results
Fifteen studies met criteria for review. The majority of the studies found a significant relationship between racial discrimination and low birth weight, preterm birth, and small for gestational age. Each of the studies that examined more proximal variables related to birth outcomes such as entry into prenatal care, employment opportunities, neighborhood characteristics, or inflammatory markers found significant associations between the specific variables examined and racial discrimination. Participants in qualitative studies discussed experiences of institutional racism with regard to several components of prenatal care including access and quality of care.
Discussion
Racial discrimination is a significant risk factor for adverse birth outcomes. To best understand the mechanisms by which racial discrimination impacts birth outcomes, and to inform the development of effective interventions that eliminate its harmful effects on health, longitudinal research that incorporates comprehensive measures of racial discrimination is needed. Health care providers must fully acknowledge and address the psychosocial factors that impact health outcomes in minority racial/ethnic women.
Keywords: health care disparities, low birth weight, minority health, pregnancy, premature birth, racial discrimination, racism, review, small for gestational age
INTRODUCTION
Profound disparities in birth outcomes persist in the United States, most significantly in the non-Hispanic black population. The overall infant mortality rate (IMR) in the United States is 5.96 infant deaths per 1000 live births, yet the IMR for non-Hispanic blacks is 11.11 infant deaths per 1000 live births.1 Black infants die before one year of life at more than twice the rate of white infants.1 While the IMR is only one marker of birth outcomes, it’s regarded as one of the most important indicators of the health of a nation as it encompasses several health indicators such as maternal health, access to health care, and public health practices.2 There are also profound disparities in other birth outcomes. The preterm birth rate for non-Hispanic black women is 1.6 times higher than the preterm birth rate for white women,1 and preterm birth–related IMR is 3 times higher in black women compared to white women.1 In 2013, the incidence of low birth weight was 8.02% for all infants in the United States, yet among non-Hispanic black infants the incidence was 13.1%.1 Preterm birth is the primary driver of the difference in IMR between non-Hispanic black and white infants, and it accounts for 54% of disparity.2 Despite significant research in this area, the reason there are racial disparities in birth outcomes remains largely unknown. The purpose of this integrative review is to summarize what is known about the relationship between racial discrimination and adverse birth outcomes in racial and ethnic minority women.
Extant research has largely focused on varied levels of exposure to risk and protective factors in the perinatal period including maternal health behaviors, adequacy of prenatal care, social support, intimate partner violence, and stress.3–6 Other research has focused on select sociodemographic characteristics including socioeconomic status, marital status, and education.7,8 Taken together, these factors do not adequately account for all of the noted disparities in birth outcomes.9
More recently, researchers have noted that racial and ethnic minority women experience higher lifetime exposure to chronic stressors, which may increase their risk for poor pregnancy outcomes.10 The accumulation of stress over a woman’s life course, referred to as allostatic load, is associated with worse health outcomes.11 Racial discrimination is one such chronic stressor that may be a risk factor for adverse birth outcomes. Definitions of racism are varied, yet all include the concept of unequal treatment stemming from skin color or other individual characteristics.12 Racism occurs at multiple levels including institutional, interpersonal, and internalized. Institutionalized racism results in differential access to the resources, services, and opportunities of society by race. With respect to resources, institutionalized racism includes disparities in access to and quality of education, safe housing, employment, health care resources, and environmental conditions. These disparities, combined with disparate opportunities to influence policy (eg, voting rights, media influence, representation in government), limit the power of racial and ethnic minorities to make and enforce decisions. Interpersonal racism refers to prejudice and discrimination with prejudice resulting in differential assumptions about the capabilities and motives of others according to their race. Discrimination includes differential treatment of others based on their race and is most commonly thought of as racism. Finally, internalized racism results in an acceptance of negative attributes, competencies, and worth by members of marginalized groups. Internalized racism limits one’s ability to reach his or her full potential.12
Quick Points.
Significant disparities exist in birth outcomes in the United States, most notably in non-Hispanic black women.
Minority women experience higher lifetime exposure to chronic stressors, thereby increasing their risk for poor pregnancy outcomes.
The overall findings of this review suggest that recent research provides mixed evidence for the association between racial discrimination and adverse birth outcomes.
Health care providers are well positioned to promote favorable birth outcomes well in advance of a woman presenting for prenatal care.
An enhanced examination of the experiences of minority women, using a life course perspective, will provide necessary insight into the pervasive disparities in birth outcomes.
BACKGROUND AND THEORETICAL FRAMEWORK
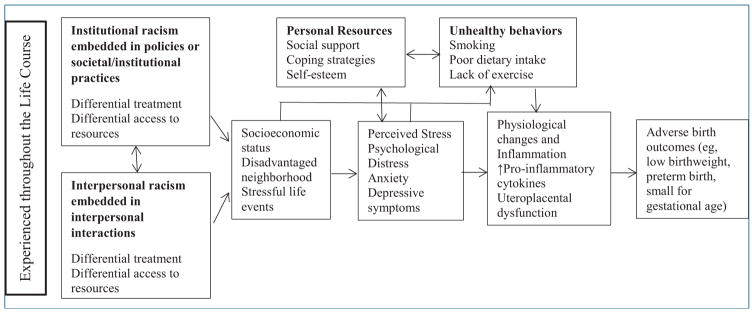
The theoretical frameworks used to guide this review are based on the theories of allostatic load and life course theory, and are presented in Figure 1.13,14 Several pathways by which racial discrimination negatively impacts health have been described. One of the most widely accepted mechanisms is that racial discrimination functions as a psychosocial stressor that increases an individual’s risk for adverse health outcomes.15 In this regard, experiencing racial discrimination, and the exclusion that ensues, elicits a stress response that has detrimental effects on health.15 Briefly, allostatic load represents the chronic physiologic and psychosocial stress experienced over the life course by combining several markers of physical function into a composite score of biologic risk.16 Research has demonstrated that women with a history of small-for-gestational-age birth or preterm birth have higher allostatic load than those women giving birth to normal birth weight infants.16 Thus, allostatic load represents a plausible pathway by which chronic exposure to stressors such as racial discrimination may contribute to poor health outcomes.15
Figure 1.
Conceptual Framework of the Potential Pathways Linking Racial Discrimination to Adverse Birth Outcomes
Note: Adapted from Giurgescu, Engeland, Zenk, & Kavanaugh13; McEwen14; and Lu & Halfon.19
Another pathway by which racial discrimination may impact health is through restricted access to social resources including employment opportunities, housing, and education, which are then related to adverse health outcomes.15 Further, geographic segregation is associated with widespread under-investment in black areas, which facilitates the development of unhealthy physical and social environments. Unhealthy environments and psychosocial stress are inextricably linked and may potentiate adverse effects on physical and mental health.17 Taken together, chronic stress stemming from racial discrimination is recognized to be particularly significant for minority women.
Application of the life course perspective to maternal and child health is grounded in life course theory. Adopting the life course perspective acknowledges the importance of risk and protective factors on an individual’s health throughout the life span and focuses on multiple predictors of health including familial, social, economic, and environmental factors.18,19 Applying a life course perspective to maternal and child health shifts us away from measuring only stressors at the time of pregnancy. It acknowledges the accumulation of events and exposures that have occurred during a woman’s life prior to pregnancy. For the past decade, scholars have pointed to the need for this kind of longitudinal focus in order to understand and eliminate disparities in birth outcomes.18,19 Further, the life course perspective notes that exposures to varied stressors may have differential impacts on health depending on the timing of exposure.18 The application of a life course perspective to better understand the role of social forces, such as racial discrimination, in birth outcomes is critical given the persistence of significant racial disparities.
METHODS
This integrative review builds on an integrative review of racial discrimination and adverse birth outcomes by Giurgescu and colleagues.20 While Giurgescu’s review included studies published up to 2009, this current review includes relevant studies published between 2009 and 2015. Further, Giurgescu and colleagues limited their review to studies conducted among African American women. We included studies that included any ethnic or racial minority group in the United States, although the majority of research examining racial discrimination and birth outcomes has been conducted among African Americans.
We included articles that measured outcomes that have previously been implicated as important predictors of adverse neonatal outcomes. For the purpose of this review, we defined adverse birth outcomes as preterm birth, low birth weight, and small for gestational age.
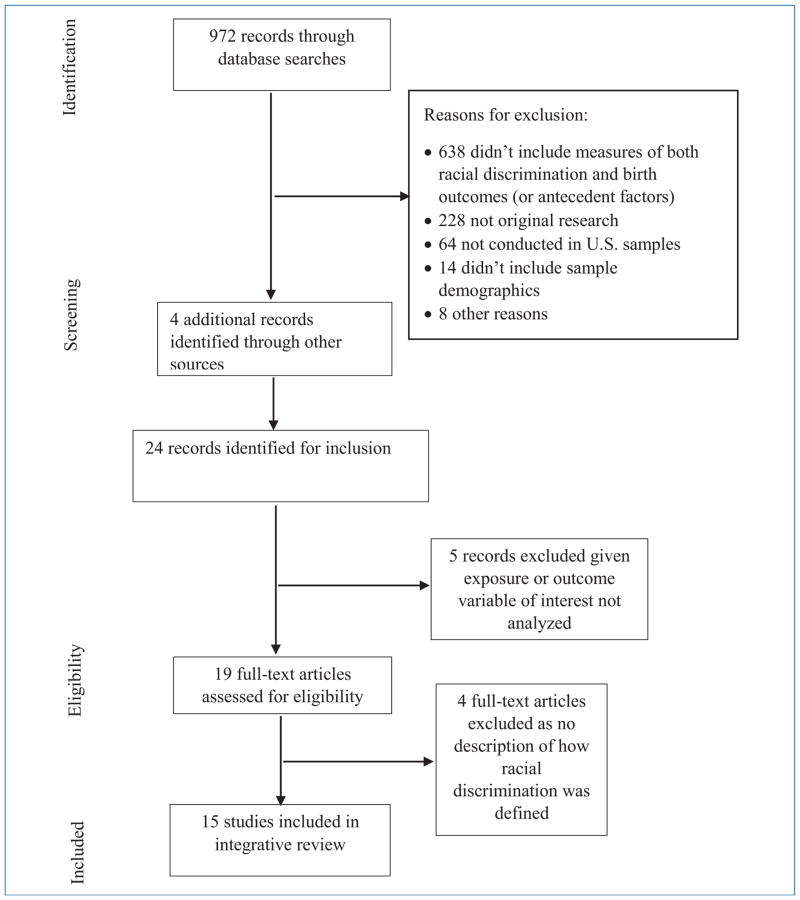
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) approach was used for generating, systematically reviewing, and analyzing original published studies on minority women, birth outcomes, and racial discrimination.21 Further, articles that included measures of widely accepted mediators or moderators of adverse birth outcomes and racism-related measures were included. With the assistance of a university librarian, the following key definitions and Medical Subject Headings (MeSH) terms were used to guide the search for research studies: “prejudice,” “racism,” “discrimination,” “health care disparities,” “pregnancy outcomes,” “obstetric complications,” “spontaneous abortion,” “premature labor,” and “low birth weight.”
The following inclusion criteria were used: 1) original quantitative or qualitative research; 2) studies that clearly delineated the relationship between racial discrimination and adverse birth outcomes, or that included racial discrimination in relation to a factor known to contribute to adverse birth outcomes; 3) studies that included racial and ethnic minority women (and related terms); 4) conducted in the United States; and 5) published in an English language peer-reviewed journal.
After determining study eligibility criteria, MeSH terms were entered into PubMed, CINAHL, Scopus, PsycINFO, Web of Science, and Embase for years 2009 to 2015, yielding 972 records. Articles duplicated between the databases were eliminated. Additional searches within the reference lists and bibliographies of the analyzed studies revealed 976 studies that were included in the final analysis. Two authors completed this process individually and then came together to reach consensus on articles for final inclusion. This process resulted in 15 published studies meeting study eligibility criteria. The large majority of studies excluded were because they did not include measures of both racial discrimination as well as birth outcomes. Figure 2 highlights the research synthesis process.
Figure 2.
PRISMA Diagram Outlining the Research Synthesis Process
Each study was reviewed for its purpose, design, methods, sample size, demographic composition, and results. Each of the identified studies was reviewed by all authors. Table 1 summarizes the studies reviewed.
Table 1.
Summary of Individual Studies Examining Racial Discrimination and Pathways to Adverse Birth Outcomes
| Authors (Year) | Design, Participants | Measure of Health Outcomes | Racism/Discrimination Measure | Results |
|---|---|---|---|---|
| Qualitative Studies | ||||
| Bermudez-Millan (2011)22 | Qualitative descriptive N = 29 Puerto Rican women |
To explore how poverty, the built environment, education, working conditions, health care access, food insecurity, and perceived discrimination are experienced throughout the life course and their perceived impact on health | Open-ended question assessing perceived discrimination/racism | Perceived racial discrimination limited employment opportunities, which in turn was perceived to negatively influence maternal and child health. |
| Giurgescu (2013)13 | Qualitative descriptive N = 22 pregnant AA women |
To explore pregnant AA women’s perceptions of risk and protective factors impacting PTB | Open-ended questions related to perceptions of causes of PTB, influence of neighborhood, and woman’s feelings influencing PTB | Racism was an identified stressor that potentially leads to PTB. |
| Nuru-Jeter (2009)24 | Qualitative descriptive N = 40 AA women with child < 15 years, including pregnant women |
To explore the racism experiences of childbearing women to inform subsequent development of improved measures for birth outcomes research | Semi-structured interview guide intended to engage women in freely discussing their experiences of racism | Women reported experiencing racism 1) over the life course, with childhood experiences being particularly salient; 2) directly and vicariously, particularly with regards to their children; 3) in interpersonal, institutional, and internalized forms. |
| Salm Ward (2013)25 | Qualitative descriptive N = 29 AA women aged ≥ 18 years with a child aged ≤ 1 year |
To examine experiences of racial discrimination during prenatal care | Semi-structured interview guide focused on participants’ thoughts about the effect of race on their experiences | Experiences of perceived discrimination based on insurance or income status, race, and lifetime experiences of racial discrimination. The majority of participants described institutionalized racism, particularly in regards to PNC. |
| Quantitative Studies | ||||
| Carty (2011)27 | Cross-sectional population-based health survey N = 629 participants (n = 407 AA, n = 222 European American) |
To examine how perceived racism is associated with self-rated health and birth | 24 racism questions included in survey | Perceived racism predicted lower self-rated physical health. Emotional responses to racism-related experiences not significantly associated with lower-birth-weight births (P = .06). |
| Christian (2012)28 | Prospective longitudinal N = 56 pregnant women (n = 38 AA, n = 18 white) |
To examine the effects of gestational age, race, and subjective stress on Epstein-Barr virus (EBV) capsid antigen immunoglobulin G (VCA IgG) | Experiences of Discrimination Scale | AA women exhibited higher serum EBV VCA IgG antibody titers than white women (P < .001). This effect was most pronounced among AA women reporting greater racial discrimination. |
| Dailey (2009)29 | Prospective cohort N = 108 pregnant AA women |
To examine the extent to which social stressors, personal resources, and known perinatal risk factors predict newborn birth weight | Everyday Discrimination Scale | Fifty-six percent of participants reported experiences of discrimination attributed to race. In final model, tobacco use, number of prenatal care visits, and discrimination due to age and physical disability were significant predictors of birth weight (R2 = .25; P < .001). |
| Earnshaw (2013)30 | Secondary data analysis of control group from longitudinal RCT N = 420 pregnant women who identified as black (n = 158) or Latina (n = 262) |
To examine the association between maternal everyday discrimination and newborn birth weight | Modified version of the Everyday Discrimination Scale | Path analysis demonstrated that everyday discrimination was associated with lower birth weight. Depressive symptoms mediated this relationship. |
| Giurgescu (2012)26 | Descriptive correlational comparative N = 72 AA with full term birth (n = 39) or PTB (n = 33) |
To determine if neighborhood environment, racial discrimination, and psychological distress predicted PTB | Experiences of Discrimination Scale | Women who reported more experiences of racial discrimination reported higher levels of psychological distress (r = .44, P < .001). Discrimination not significantly associated with PTB (P = .39) |
| Mendez (2014)31 | Secondary data analysis from clinic-based sample of pregnant women (N = 3462) with linked data from the 2000 US Census and Home Mortgage Disclosure Act data | To examine if reported stress, discrimination, and neighborhood quality were associated with PTB | Investigator-developed measure of experiences of discrimination | After adjustment for covariates, discrimination not significantly associated with PTB (OR, 1.0; 95% CI, 0.8–1.3) |
| Misra (2010)32 | Hybrid retrospective and prospective cohort N = 832 AA women |
To examine how social and psychosocial factors, including racism, relate to risk of PTB | Racism and Lifetime Experiences Scale (RALES) and 3 items from RALES Daily Life Experiences Scale | In adjusted and unadjusted models, exposure to racism over a women’s lifetime had no effect on PTB. However, racism scores above the median were significantly associated with an increased risk of PTB in 3 subgroups with the effect moderated by depressive symptoms and stress |
| Rankin (2011)33 | Case-control N = 277 AA mothers of PTB LBW (n = 160 cases) and term newborns (n = 117 controls) |
To determine if AA women’s coping behaviors modify the relationship between racial discrimination and PTB | Modified version of the Perceived Racism Scale | A greater percentage of AA mothers of preterm newborns had higher past-year exposure to racism than their counterparts who gave birth to term newborns (OR, 2.5; 95% CI, 1.2–5.2) |
| Ruiz (2014)34 | Secondary analysis of Louisiana Pregnancy Risk Assessment Monitoring System Unweighted n = 1561 white mothers and n = 899 black mothers |
To examine impact of perceived access to health care services and information received on birth outcomes | Investigator-developed variables used as potential proxy for perceived discrimination | In adjusted models, self-perceived access to health care was associated with PTB for black women (OR, 2.94; 95% CI, 1.1–8.3) and infant mortality for white women (OR, 340.5; 95% CI, 35.7 > 999.9) |
| Slaughter-Acey (2013)35 | Prospective/retrospective cohort design N = 872 AA women |
To examine the relationship between racism and prenatal care initiation | Investigator-developed index | Entry into PNC not significantly associated with experiences of racism (P = .33) though significantly associated with group (eg, family, friends, neighbors, other AA individuals) experiences of racism (P < .01). |
| Wallace (2015)36 | Retrospective; electronic medical records from singleton births to white and black women (N = 121,758) linked to state-level indicators of structural racism | To examine the synergistic effects of racial and socioeconomic inequality associated with SGA birth | Investigator-developed index using indicators of structural racism including employment, incarceration, and education ratios of blacks and whites. | High levels of racial inequality and socioeconomic inequality significantly associated with SGA birth. In areas with high inequality levels, AORs ranged from 1.81 to 2.11 for the 3 structural racism indicators. |
Abbreviations: AA, African American; AOR, adjusted odds ratio; CI, confidence interval; LBW, low birth weight; OR, odds ratio; PNC, prenatal care; PTB, preterm birth; RCT, randomized control trial; SGA, small for gestational age.
RESULTS
Design
Four of the studies reviewed were qualitative designs,22–25 and 11 studies included quantitative designs.26–36 All of the qualitative studies were descriptive in nature. Of the quantitative studies, 8 used convenience sampling,26,28–33 while 3 of the population-based studies used quota sampling27,36 and stratified sampling.34 The qualitative studies used convenience sampling,23 purposeful sampling,25 purposeful and snowball sampling,24 and convenience sampling with purposeful assignment to a focus group based on participant age and parity.22
Defining Race
Of the 15 studies reviewed, 12 provided information on how participant race was defined.22–32 In these studies, all asked participants to self-identify their race. In several of the studies, it was not clear what categories were provided to participants for self-identification of race, and 3 of these studies included all African American participants.26,29,33 A study using Pregnancy Risk Assessment Monitoring System (PRAMS) data compared white women to black women without consideration of other racial groups given that white and black women comprise 95% of the population in the region examined.34 In one study, participants who identified as both African American and white were counted as African Americans in the analyses as the authors posited that participant experiences of racism were thought to better approximate those of African Americans versus whites.28 One study did not differentiate outcomes among the study sample that was composed of blacks and Latinas.30 A qualitative study purposefully included only women who identified as Puerto Rican given that Puerto Rican women have the highest incidence of preterm birth among Latinas.22 Overall, the majority of studies were conducted to assess the relationship between racial discrimination and adverse birth outcomes in African Americans.
Measure of Racism
In recent years, there has been a significant increase in research focused on developing instruments to measure experiences and perceptions of racism.37 This area of research has increased our understanding of the relevance between racial discrimination and the health and well-being of minority populations.37 Several measures were used to measure racial discrimination in these studies. In the qualitative studies, either an open-ended question or several open-ended questions were used to elicit participants’ experiences with racism. Two of the quantitative studies26,28 measured racial discrimination through the Experiences of Discrimination Scale.38 The Everyday Discrimination Scale39 or a modified version thereof was used in 2 of the studies.29,30 Two studies used the Racism and Lifetime Experience Scale40 or a modified version thereof,32,35 and a modified version of the Perceived Racism Scale41 was used in one study.33 Finally, 4 studies used either investigator-developed questionnaires31,34,36 or a combination of items from several scales.27 Table 2 summarizes the measures used in the quantitative studies, although it does not include investigator-developed questionnaires.
Table 2.
Instruments Used to Measure Racial Discrimination in Reviewed Studies
| Instrument, Studies Using | Domain or Construct Measured | Instrument Specifics | Psychometrics in Reviewed Studies |
|---|---|---|---|
| Experiences of Discrimination Scale (EOD)38/ Christian (2012)28, Giurgescu (2012)26 |
Measures experiences of discrimination due to race/ethnicity in varied settings (eg, school, employment, or judicial setting; seeking employment, housing, health care) | Nine-item scale assessing the occurrence and frequency of experiences of discrimination in 9 settings, with score ranging from 0 to 9. Frequency calculated as 0 (never), 1 (once), 2.5 (2–3 times), and 5 (≥ 4 times), with scores ranging from 0 to 45. | Cronbach’s alpha = 0.7831 |
| Everyday Discrimination Scale (EDS)39/ Dailey (2009)29, Earnshaw (2013)30 |
Measures experiences of being treated with less courtesy or respect than others; receiving poorer service than others at restaurants or stores; people acting as if you are not smart, as if they are afraid of you, as if you are dishonest, as if they are better than you; being called names or insulted; and being threatened or harassed | Nine-item scale assessing the presence, frequency, and source of chronic and routine experiences of discrimination; responses range from 1 (never) to 6 (almost every day) with scores ranging from 0 to 54. | Cronbach’s alpha = 0.8435–0.8634 |
| Racism and Lifetime Experiences Scale (RALES)40 Misra (2010)32, Slaughter-Acey (2013)35 |
A series of scales that measures racism-related stress, coping, socialization, and attitudes | Full measure includes 10 subscales assessing various experiences and responses to racism; subscales are of varied length and measured on Likert-type scale. | Cronbach’s alpha = 0.61–0.8240 |
| Perceived Racism Scale (PRS)41 Rankin (2011)33 |
Measures exposure to perceived racism in several domains, including individual, institutional, cultural, behavioral, and attitudinal domains | 51-item scale assessing experiences with racism in 3 categories (frequency of exposure, emotional responses, and coping responses) across 4 areas (job, academic setting, public setting, exposure to racial statements). Responses range from 0 (not applicable), 1 (almost never), to 7 (several times a day). Participants also rate their emotional responses (eg, angry, frustrated, sad, hopeless) to experiences of racism across 4 areas on a 5-point Likert scale from 1 (not at all) to 5 (extremely) as well as coping responses (eg, speak up, pray, ignore, accept). | Not provided |
Factors That May Explain the Relationship Between Racial Discrimination and Birth Outcomes
As highlighted in Figure 2, and consistent with recent theoretical work,15,18,42 there are several mechanisms through which racial discrimination is a risk factor for adverse birth outcomes. Five studies reviewed included antecedent factors that may help explain the relationship between racial discrimination and adverse birth outcomes. These factors included limited employment opportunities,22 experiences of institutional racism in both accessing and receiving prenatal care,24,25,35 and inflammatory markers of stress.28 Two studies examined racial discrimination during prenatal care25 and racial discrimination as a barrier to accessing prenatal care.35
In a qualitative study, African American women described experiencing both racism directed at them personally as well as institutionalized racism during prenatal care.25 Participants discussed individual experiences of racism during prenatal care including blatant behaviors (eg, racial slurs directed at them) as well as more subtle forms of racism. One participant described telling her midwife that she didn’t like going to her prenatal care appointments, and the midwife asked the participant, “Do you do crack?” The participant felt that the midwife asked her about crack use because she was black, and other focus group participants were in agreement. Participants also described experiences of institutionalized racism including experiencing differential treatment based on receipt of public assistance. One participant noted that, “White people don’t have blue cards” (ie, the color of the state’s medical assistance ID cards) and described differential treatment based on race and financial status. Similarly, another participant stated, “You learn to go last. No matter how much people talk about it … it’s been like that forever.” Importantly, participants were initially reluctant to discuss racial discrimination in several of the focus groups without probing questions from trained facilitators or validation of their feelings from other focus group participants.25
In a large sample of African American women by Slaughter-Acey et al (N = 872), timing of prenatal care initiation was not significantly associated with personal experiences of racism (P = .33) but was associated with group experiences (P < .01). Participants who denied group experiences of racism (eg, experiences of racism that affected persons close to the participant or experiences of racism directed at other African Americans) were significantly more likely to enter prenatal care during the third trimester or to not receive any prenatal care. The authors suggested that these women may suppress experiences of racism as a protective mechanism to avoid feeling powerless or vulnerable.35
Two qualitative studies described the influence of racial discrimination over the life course on health and well-being. Among a sample of Puerto Rican women, participants described perceived racial discrimination related to employment opportunities. Further, participants discussed the significant stressors they experienced related to living in poverty, in high-crime neighborhoods with significant exposure to violence, and fear of speaking to authorities without having the necessary resources to move to safer environments. The majority of participants described the influence of stress on their physical and mental health including experiencing changes in their physical appearance as well as episodes of chest pain, alopecia, depression, and suicidal thoughts.22 In another qualitative study by Nuru-Jeter et al,24 African American women described experiencing racism throughout the life course with childhood experiences perceived as particularly salient. This study was conducted to explore the racism experiences of childbearing women in an effort to inform the development of improved measures of experiences of racism for birth outcomes research. Participants described childhood events often being the first experience of “being different” and that these experiences had enduring effects on the participants. Further, many participants described somatic responses to racist encounters including feeling sick, having headaches, stomachaches, and shaking all over.24 While participants didn’t specifically ascribe racial discrimination to adverse birth outcomes, they did provide valuable insights into the enduring impact of childhood experiences of racism, vicarious responses related to their own children, and the pervasiveness and chronicity of racial discrimination.24 Taken together, these results highlight the need for more comprehensive measures of racial discrimination.
Finally, one of the studies reviewed used a biologic marker to examine the effects of race and racial discrimination.28 Specifically, the relationship between Epstein-Barr virus (EBV) capsid antigen immunoglobulin G (VCA IgG) and race and racial discrimination was examined in women during pregnancy and the postpartum period. Briefly, EBV VCA IgG antibody titers can serve as an indicator of stress-induced immune dysregulation.43 Results revealed that at every time point, African American women exhibited higher EBV VCA IgG antibody titers than white women (P < .001). The effect was most pronounced among African American women reporting experiencing higher levels of racial discrimination in the first and second trimesters (P = .03 and P = .04, respectively), supporting a role that chronic stress is related to this association.43
Birth Outcomes
Six of the studies reviewed examined preterm birth as the outcome of interest, and one of these studies was qualitative in design. In a small sample of African American women (N = 72), racial discrimination was significantly associated with higher levels of psychological distress (r = .44, P < .001), yet there was not a significant association between racial discrimination and preterm birth. Importantly, women reported relatively low levels of racial discrimination.26 In a larger sample of women (N = 3462), after adjusting for several covariates, racial discrimination was not significantly associated with preterm birth (odds ratio [OR], 1.0; 95% confidence interval [CI], 0.8–1.3).22 Similarly, in an urban sample, racial discrimination over a woman’s lifetime was not significantly associated with preterm birth. However, women with racism scores above the median were at significantly increased risk of preterm birth with the effect moderated by depressive symptomatology.32 Two of the quantitative studies reviewed found significant associations between racial discrimination and preterm birth.33,34 A case-control study conducted in Chicago, Illinois, demonstrated that African American women with preterm birth reported higher past-year exposure to racism than their counterparts who gave birth to full-term newborns (OR, 2.5; 95% CI, 1.2–5.2).33 Using Louisiana PRAMS data, Ruiz and colleagues demonstrated that racial discrimination was significantly associated with preterm birth for black women (OR, 2.94; 95% CI, 1.1– 8.3).34 Finally, in a qualitative study, pregnant African American women identified racial discrimination as a plausible stressor leading to higher rates of preterm birth.23 Taken together, research findings are mixed with regard to the association between racial discrimination and preterm birth.
Three of the studies reviewed examined the association between racial discrimination and low birth weight.27,29,30 Dailey found that in a sample of African American women (N = 108), perceived discrimination due to race was reported by 56% of the sample. In the hierarchal multiple regression model, tobacco use, number of prenatal care visits, and perceived discrimination due to age and physical disability were significant predictors of birth weight (R2 = .25; P 3.001).29 In a sample of black and Latina women (N = 420), Earnshaw et al found that perceived racial discrimination was associated with an increased odds of low birth weight; however, depressive symptoms mediated this relationship.30 Experiences of everyday discrimination were associated with increased depressive symptoms. In turn, depressive symptoms were associated with giving birth to a low-birth-weight neonate, after controlling for education, parity, and gestational age. The final path model revealed that for every point increase in the measure of everyday discrimination, birth weight decreased by approximately 49 grams. The third study, by Carty et al, included a large sample of women (N = 629). In this study, perceived racism was significantly associated with lower self-rated physical health and a higher likelihood of smoking, yet women’s responses to racism-related experiences were not significantly associated with low birth weight (P = .06).27 Importantly, birth outcomes were collected via self-report, and the interval between pregnancies and data collection were not clear.
Finally, Wallace et al examined the synergistic effects of racial and socioeconomic inequality with giving birth to a small-for-gestational-age newborn.36 Socioeconomic inequality was measured via use of the Gini coefficient and racial inequality was measured via use of 3 well-established indicators of structural racism including inequality in educational attainment, an employment disparity indicator, and a disparity in incarceration indicator. Using an electronic medical record–based cohort (N = 121,758) from hospitals in multiple states to assure geographical diversity, these investigators found the joint effects of racial and income inequality were significantly associated with giving birth to a small-for-gestational-age newborn only when levels of both racial and income inequality were high. Specifically, women were significantly more likely to give birth to a small-for-gestational-age newborn in areas with high income inequality and high educational attainment inequality (adjusted odds ratio [AOR], 2.11; 95% CI, 1.59–2.80), high incarceration inequality (AOR, 1.81; 95% CI, 1.28–2.56), and high employment inequality (AOR, 1.85; 95% CI, 1.23–2.79) than those women residing in areas with low levels of racial and income inequality. When data were further stratified by race (black vs white), black women had significantly higher odds of giving birth to a small-for-gestational-age newborn when exposed to all indicators of structural racism including educational inequality (AOR, 1.53; 95% CI, 1.22–1.92), incarceration inequality (AOR, 1.57; 95% CI, 1.27–1.95), employment inequality (AOR, 1.57; 95% CI, 1.25–1.96), and an income inequality measure (AOR, 1.61; 95% CI, 1.36–1.91).36
DISCUSSION
Reducing disparities in birth outcomes has been a national priority in the United States for several decades.2 An increasing body of research demonstrates that racial discrimination is significantly associated with negative physical and mental health in racial and ethnic minority individuals, and consequently racial discrimination may perpetuate significant disparities in a multitude of health outcomes, including birth outcomes.44 The overall findings of this review provide mixed support for the association between racial discrimination and adverse birth outcomes. Notably, across studies there were significant differences in sample sizes, instruments used to measure racial discrimination, variables included in final analytic models, and time period assessed with regard to racial discrimination, which may help explain differences in study findings.
In each of the qualitative studies, participants provided support for racial discrimination as a risk factor for adverse birth outcomes. Participants described experiencing institutional racism in receiving prenatal care24,25 and seeking employment,22 racial discrimination during childhood having lasting health effects,24 and how the stress associated with racial discrimination could be a risk factor for preterm birth.23
Each of the studies that examined the association between racial discrimination and more proximal measures known to be associated with adverse birth outcomes found significant associations. Access to and quality of prenatal care, employment opportunities, neighborhood characteristics, and inflammatory markers were significantly associated with racial discrimination suggesting the effects of racial discrimination play an important role in the pathway linking racial discrimination to adverse birth outcomes.22,24,25,28,35
The majority of the studies that examined preterm birth, low birth weight, or small for gestational age as outcomes of interest found a significant association between racial discrimination and adverse birth outcomes with few exceptions.26,27,31 One of the studies that did not find a significant association between racial discrimination and birth outcomes examined institutional racism, specifically, residential redlining (ie, mortgage loan denial), as the exposure of interest. Notably, these authors posited that black women living in redlined neighborhoods were less likely to be exposed to white people, and this segregation may have acted as a stress buffer from racial discrimination.31 The other study that did not find an association between racial discrimination and adverse birth outcomes was limited by a small sample size and relatively low levels of reported racial discrimination.26 Because other studies have found significant associations between segregation and birth outcomes,45,46 future studies should consider other forms of institutional racism in diverse geographic areas.
Racial discrimination is likely to date back to a woman’s childhood and likely to previous generations. Consistent with Geronimus’s concept of “weathering,” repeated exposure to stressors such as racial discrimination accumulates and increases an individual’s disease vulnerability.42 Thus, it may be that lifelong exposures influence the reproductive health of young women, increasing their risk of poor outcomes well before conception.7,19 Indeed, in one of the qualitative studies reviewed here,24 participants discussed racial discrimination endured in childhood as being particularly salient. The study by Misra et al32 that included a measure of lifetime experiences of racism also found that elevated racism scores were associated with an increased risk of preterm birth, although the effect was mediated by depressive symptoms and stress. While limited, results of these 2 studies suggest future research should include understanding how lifetime exposure to racial discrimination as well as experiences occurring in the perinatal period contribute to birth outcomes.
Few studies in this review included Hispanic women and only one qualitative study analyzed racial discrimination among Hispanic women as a distinct minority group.22 The Hispanic population in the United States is expected to double by 2050, when it will constitute nearly one-third of the total population in the United States.47 Interestingly, Hispanic women in the United States give birth to low-birth-weight newborns at rates that are comparable to that of non-Hispanic white women despite the pervasive socioeconomic disadvantage among Hispanic women.9 This favorable health outcome is commonly referred to as the Hispanic Paradox and several explanations for these protective effects have been offered including the notion that Hispanic neighborhoods may buffer Hispanics from stigma and racism.48 Importantly, advantageous health outcomes decline with longer residence in the United States suggesting acculturation plays an important role in health outcomes.9 Given the growth and increasing diversity of the Hispanic population in the United States, further research is needed to understand the relationships between ethnic density, racial discrimination, and birth outcomes.
Small for gestational age is increasingly recognized as an adverse pregnancy outcome that has significant negative consequences which may extend into adulthood including increased rates of coronary heart disease, stroke, diabetes, and metabolic syndrome.49 The finding of Wallace et al that demonstrated high levels of racial and income inequality were significantly associated with an increased odds of small-for-gestational-age birth provides important insights about the complex synergistic effects of class and race on perinatal health.36 State-level funding policies in areas of health care, education, and employment, combined with systemic racism, may be one pathway by which structural racism at the state level and income inequality contribute to disparities in birth outcomes. An examination of additional state-level practices and policies that systematically disadvantage minority women is critical to better understand the influence of structural racism on health outcomes.
There are several important limitations to this integrative review. First, the method of defining race was varied across studies with the majority of studies using self-identified race. None of the studies reviewed sought to further delineate black or African American women into different subgroups, such as black Caribbean. These broad classifications of race limit our ability to examine intragroup differences between those women who identified as black or African American. Research has demonstrated significant differences in both experiences of racism and birth outcomes in US-born and foreign-born black women50; thus, future studies should incorporate additional racial categories to better disentangle disparities among groups identified as black or African American.
Consistent with extant literature, results of this review demonstrate that the terms racism and discrimination are often used interchangeably. Both terms are used to describe an unequal distribution of power that provides opportunities and assigns values to individuals based on their perceived race. Despite the absence of a foundation for a biologic construct of race, race continues to function as a social construct in our society with evident social stratifications.51 The majority of research reviewed here examined interpersonal racism, largely focused on an individual’s perception of experiencing racism. However, racism is pervasive in interpersonal, institutional, and societal contexts of social life. Because it is so pervasive, it often goes unnoticed or unchallenged thereby resulting in underreporting.52 Only one study reviewed included a biologic marker of stress examined in relationship to racial discrimination.28 Relying on self-reported experiences of discrimination (or racism) might not fully capture the actual effect of racial discrimination on health outcomes. Researchers have urged the development of measures for racism that aren’t limited to self-report.53
Another limitation of this review is that the studies included were quite varied with regard to sample size and sampling methods. Many of the studies used convenience sampling, which limits generalizability of findings. However, this review included studies of all sizes in order to provide a comprehensive overview of recent research.
Finally, the majority of the reviewed studies did not test for moderation or mediation by other variables that have been independently linked to both the exposure and outcome variables of interest. For example, in the study by Dailey,29 tobacco use was a significant predictor of birth weight, while racial discrimination wasn’t a significant predictor in the final model. It could be hypothesized that tobacco use is a coping mechanism used to deal with the stress of racial discrimination and may well function as a mediator in the racial discrimination-adverse birth outcome association.
Recommendations for Future Research
Additional research is needed to enhance our understanding of the complexity of the relationship between racism and birth outcomes. For instance, social support, self-esteem, social capital, or optimism could be measured to determine if they are protective against the prenatal impacts of racial discrimination. The existing research also fails to clearly determine the differential impact of current versus lifetime racism. Additional research to understand the individual influence of each would help inform the development of interventions. And, studies that examine racial discrimination during pregnancy should also explore potential for varying levels of impact depending on the trimester of exposure.
Research with nonpregnant women as participants has found racial discrimination to be associated with a range of biological indices of stress including markers of inflammation.54 Further, elevated inflammatory markers have been associated with chronic stress and preterm birth in several studies.55 An enhanced understanding of associations between racism-related stress and biological measures of chronic stress that are subsequently associated with adverse birth outcomes is needed. This will facilitate a better understanding of the biologic pathways involved in the racial and ethnic disparities that have been documented in birth outcomes.
Finally, more population-based studies are needed to explore the relationship between racial discrimination and birth outcomes. The 2009 to 2011 PRAMS survey added questions about racial discrimination, but only New York City included a question specific to differential treatment based on race during pregnancy, and Washington state included a similar question to encompass the perinatal period. In the future, all participating states should include these questions, as well as questions specific to lifetime experiences, so that larger samples with sufficient power can be studied.
Clinical Implications
Health care providers are well positioned to promote favorable birth outcomes well in advance of a woman presenting for prenatal care. A women’s health at conception, and the consequent health of her newborn, is largely shaped by her biopsychosocial experiences up until that point. Thus, the reproductive health of ethnic and minority women may be compromised long before they present for prenatal care. By adopting a life course perspective, health care providers can place a greater emphasis on preventive and preconception care, both integral to optimizing reproductive health outcomes.19 Further, applying a life course perspective acknowledges that certain exposures throughout life, particularly during biologically vulnerable periods of time, as well as cumulative risk influence health outcomes at later ages. This is particularly salient for understanding disparities among immigrant populations. Extant social epidemiology research often combines race/ethnicity with nativity, which limits our understanding of how these distinct dimensions of inequity influence an individual’s health.56
Results from the current review demonstrate that ethnic and minority women continue to encounter negative experiences in the health care setting as a result of their race. Eliminating system-level barriers to quality health care is an important step, though key to improving health outcomes is the establishment of a trusting patient-provider relationship. Research demonstrates that negative racial stereotypes are significantly associated with health care providers’ provision of care as well as the patient-provider relationship.57 While health care provider bias is often unintentional and unrecognized, it does lead to mistrust in the health care system as well as poor satisfaction with patient care.
There is a significant need for the development and testing of interventions addressing racial discrimination. These interventions should target multiple levels including primary prevention for health care professional students, interventions for health care professionals engaged in patient care, and interventions that address biases inherent in varied health care institutions. Interventions addressing racial discrimination ought to adapt a community-based participatory research framework, an approach that emphasizes co-learning with community partners as fully engaged partners in the entire research process.58 Establishing mutually respectful relationships, shared responsibilities, and capacity building within our communities may remove barriers that impede progress in reducing disparities.58
For women at highest risk of adverse birth outcomes, health care providers should work with local community agencies to make appropriate referrals for additional services such as home visiting. Research has demonstrated improved perinatal health and pregnancy outcomes through home visiting.59 If delayed access to prenatal care is due to previous racialized experiences, the home visitor may be an important advocate and confidant for the pregnant woman. Indeed, the relationship between the home visitor and woman is key to retention in home visiting programs.60
CONCLUSION
Results of this integrative review provide support for the association between racial discrimination and adverse birth outcomes among minority women. An enhanced examination of the personal experiences of minority women, using a life course perspective, will provide necessary insight into important factors that contribute to the pervasive racial disparities in birth outcomes. As the United States becomes more culturally diverse, health care professionals are well positioned to educate themselves, their colleagues, and their students about the tenets of culturally sensitive health care. Eliminating racial disparities in birth outcomes necessitates a thoughtful commitment from health care professionals, policy makers, and social and economic institutions to eradicate racism and the ensuing social inequities.
Acknowledgments
This study was supported by funding from the National Institutes of Health (NIH), National Institute of Nursing Research grant K23NR015810.
Biographies
Jeanne L. Alhusen, PhD, CRNP, RN, is an Associate Professor at the University of Virginia School of Nursing and a family nurse practitioner. Her research is focused on disparities in birth outcomes.
Kelly Bower, PhD, RN, is an Assistant Professor in the Department of Community-Public Health at Johns Hopkins School of Nursing, and her practice is with the Fetal and Infant Mortality Review within the Baltimore City Health Department, Baltimore, MD.
Elizabeth Epstein, PhD, RN, is an Associate Professor at the University of Virginia School of Nursing. Dr. Epstein’s research is focused on moral distress and end-of-life issues in neonatal nursing.
Phyllis Sharps, PhD, RN, FAAN, is an Professor and Associate Dean for Community and Global Programs at Johns Hopkins School of Nursing. Dr. Sharps’ research is focused on the effects of intimate partner violence on the health of pregnant women, infants, and young children.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
References
- 1.Matthews TJ, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital Stat Rep. 2015;64:1–30. [PubMed] [Google Scholar]
- 2.MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Semin Perinatol. 2011;35:200–208. doi: 10.1053/j.semperi.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 3.Shapiro GD, Fraser WD, Frasch MG, Seguin JR. Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. J Perinat Med. 2013;41:631–645. doi: 10.1515/jpm-2012-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denny CH, Floyd RL, Green PP, Hayes DK. Racial and ethnic disparities in preconception risk factors and preconception care. J Womens Health (Larchmt) 2012;21:720–729. doi: 10.1089/jwh.2011.3259. [DOI] [PubMed] [Google Scholar]
- 5.Alhusen JL, Bullock L, Sharps P, Schminkey D, Comstock E, Campbell J. Intimate partner violence during pregnancy and adverse neonatal outcomes in low-income women. J Womens Health. 2014;23:920–926. doi: 10.1089/jwh.2014.4862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gavin AR, Nurius P, Logan-Greene P. Mediators of adverse birth outcomes among socially disadvantaged women. J Womens Health (Larchmt) 2012;21:634–642. doi: 10.1089/jwh.2011.2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braveman PA, Heck K, Egerter S, et al. The role of socioeconomic factors in black-white disparities in preterm birth. Am J Public Health. 2015;105:694–702. doi: 10.2105/AJPH.2014.302008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorch SA, Kroelinger CD, Ahlberg C, Barfield WD. Factors that mediate racial/ethnic disparities in US fetal death rates. Am J Public Health. 2012;102:1902–1910. doi: 10.2105/AJPH.2012.300852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin LP. Maternal and pediatric health and disease: integrating biopsychosocial models and epigenetics. Pediatr Res. 2016;79:127–135. doi: 10.1038/pr.2015.203. [DOI] [PubMed] [Google Scholar]
- 10.Latendresse G. The interaction between chronic stress and pregnancy: preterm birth from a biobehavioral perspective. J Midwifery Womens Health. 2009;54:8–17. doi: 10.1016/j.jmwh.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McEwen BS. Stress, adaptation, and disease: allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 12.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90:1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giurgescu C, Engeland CG, Zenk SN, Kavanaugh K. Stress, inflammation and preterm birth in African American women. Newborn Infant Nurs Rev. 2013;13:171–177. [Google Scholar]
- 14.McEwen BS. Stressed or stressed out: what is the difference? J Psychiatry Neurosci. 2005;30:315–318. [PMC free article] [PubMed] [Google Scholar]
- 15.Berger M, Sarnyai Z. “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress. 2015;18:1–10. doi: 10.3109/10253890.2014.989204. [DOI] [PubMed] [Google Scholar]
- 16.Hux VJ, Catov JM, Roberts JM. Allostatic load in women with a history of low birth weight infants: the national health and nutrition examination survey. J Womens Health (Larchmt) 2014;23:1039–1045. doi: 10.1089/jwh.2013.4572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christian LM. Psychoneuroimmunology in pregnancy: immune pathways linking stress with maternal health, adverse birth outcomes, and fetal development. Neurosci Biobehav Rev. 2012;36:350–361. doi: 10.1016/j.neubiorev.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braveman P. What is health equity: and how does a life-course approach take us further toward it? Matern Child Health J. 2014;18:366–372. doi: 10.1007/s10995-013-1226-9. [DOI] [PubMed] [Google Scholar]
- 19.Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7:13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- 20.Giurgescu C, McFarlin BL, Lomax J, Craddock C, Albrecht A. Racial discrimination and the black-white gap in adverse birth outcomes: a review. J Midwifery Womens Health. 2011;56:362–370. doi: 10.1111/j.1542-2011.2011.00034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 22.Bermudez-Millan A, Damio G, Cruz J, et al. Stress and the social determinants of maternal health among Puerto Rican women: a CBPR approach. J Health Care Poor Underserved. 2011;22:1315–1330. doi: 10.1353/hpu.2011.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giurgescu C, Banks A, Dancy BL, Norr K. African American women’s views of factors impacting preterm birth. MCN Am J Matern Child Nurs. 2013;38:229–234. doi: 10.1097/NMC.0b013e318293bbbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nuru-Jeter A, Dominguez TP, Hammond WP, et al. “It’s the skin you’re in”: African-American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J. 2009;13:29–39. doi: 10.1007/s10995-008-0357-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salm Ward TC, Mazul M, Ngui EM, Bridgewater FD, Harley AE. “You learn to go last”: perceptions of prenatal care experiences among African-American women with limited incomes. Matern Child Health J. 2013;17:1753–1759. doi: 10.1007/s10995-012-1194-5. [DOI] [PubMed] [Google Scholar]
- 26.Giurgescu C, Zenk SN, Dancy BL, Park CG, Dieber W, Block R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in African American women. J Obstet Gynecol Neonatal Nurs. 2012;41:E51–61. doi: 10.1111/j.1552-6909.2012.01409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carty DC, Kruger DJ, Turner TM, Campbell B, DeLoney EH, Lewis EY. Racism, health status, and birth outcomes: results of a participatory community-based intervention and health survey. J Urban Health. 2011;88:84–97. doi: 10.1007/s11524-010-9530-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Christian LM, Iams JD, Porter K, Glaser R. Epstein-Barr virus reactivation during pregnancy and postpartum: effects of race and racial discrimination. Brain Behav Immun. 2012;26:1280–1287. doi: 10.1016/j.bbi.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dailey DE. Social stressors and strengths as predictors of infant birth weight in low-income African American women. Nurs Res. 2009;58:340–347. doi: 10.1097/NNR.0b013e3181ac1599. [DOI] [PubMed] [Google Scholar]
- 30.Earnshaw VA, Rosenthal L, Lewis JB, et al. Maternal experiences with everyday discrimination and infant birth weight: a test of mediators and moderators among young, urban women of color. Ann Behav Med. 2013;45:13–23. doi: 10.1007/s12160-012-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Health. 2014;19:479–499. doi: 10.1080/13557858.2013.846300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Misra D, Strobino D, Trabert B. Effects of social and psychosocial factors on risk of preterm birth in black women. Paediatr Perinat Epidemiol. 2010;24:546–554. doi: 10.1111/j.1365-3016.2010.01148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rankin KM, David RJ, Collins JWJ. African American women’s exposure to interpersonal racial discrimination in public settings and preterm birth: the effect of coping behaviors. Ethn Dis. 2011;21:370–376. [PubMed] [Google Scholar]
- 34.Ruiz RL, Shah MK, Lewis ML, Theall KP. Perceived access to health services and provider information and adverse birth outcomes: findings from LaPRAMS, 2007–2008. South Med J. 2014;107:137–143. doi: 10.1097/SMJ.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 35.Slaughter-Acey J, Caldwell CH, Misra DP. The influence of personal and group racism on entry into prenatal care among African American women. Womens Health Issues. 2013;23:e381–7. doi: 10.1016/j.whi.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wallace ME, Mendola P, Liu D, Grantz KL. Joint effects of structural racism and income inequality on small-for-gestational-age birth. Am J Public Health. 2015;105:1681–1688. doi: 10.2105/AJPH.2015.302613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atkins R. Instruments measuring perceived racism/racial discrimination: review and critique of factor analytic techniques. Int J Health Serv. 2014;44:711–734. doi: 10.2190/HS.44.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30:1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- 39.Forman T, Williams D, Jackson J. Race, place, and discrimination. Perspectives on Social Problems. 1997;9:231–261. [Google Scholar]
- 40.Harrell SP. Unpublished manuscript. Los Angeles: California School of Professional Psychology; 1997. The racism and life experience scales (RALES) [Google Scholar]
- 41.McNeilly MD, Anderson NB, Armstead CA, et al. The perceived racism scale: a multidimensional assessment of the experience of white racism among African Americans. Ethn Dis. 1996;6:154–166. [PubMed] [Google Scholar]
- 42.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Glaser R, Kiecolt-Glaser J. How stress damages immune system and health. Discov Med. 2005;5:165–169. [PubMed] [Google Scholar]
- 44.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc Sci Med. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 45.Bell JF, Zimmerman FJ, Mayer JD, Almgren GR, Huebner CE. Associations between residential segregation and smoking during pregnancy among urban African-American women. J Urban Health. 2007;84:372–388. doi: 10.1007/s11524-006-9152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63:3013–3029. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 47.Passel JS, Cohn DUS. Population projections: 2005–2050. Washington, DC: Pew Hispanic Center; 2008. [Google Scholar]
- 48.Osypuk TL. Invited commentary: integrating a life-course perspective and social theory to advance research on residential segregation and health. Am J Epidemiol. 2013;177:310–315. doi: 10.1093/aje/kws371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002;31:1235–1239. doi: 10.1093/ije/31.6.1235. [DOI] [PubMed] [Google Scholar]
- 50.Dominguez TP, Strong EF, Krieger N, Gillman MW, Rich-Edwards JW. Differences in the self-reported racism experiences of US-born and foreign-born black pregnant women. Soc Sci Med. 2009;69:258–265. doi: 10.1016/j.socscimed.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Krieger N. Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, and current controversies: an ecosocial perspective. Am J Public Health. 2008;98:S20–25. doi: 10.2105/ajph.98.supplement_1.s20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57 doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behav Immun. 2010;24:438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coussons-Read ME, Okun ML, Nettles CD. Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain Behav Immun. 2007;21:343–350. doi: 10.1016/j.bbi.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 56.Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The multi-ethnic study of atherosclerosis. Soc Sci Med. 2009;69:110–120. doi: 10.1016/j.socscimed.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Institute of Medicine. Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C: The National Academies Press; 2003. Unequal Treatment. [PubMed] [Google Scholar]
- 58.Horowitz CR, Robinson M, Seifer S. Community-based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009;119:2633–2642. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Olds DL, Kitzman HJ, Cole RE, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164:419–424. doi: 10.1001/archpediatrics.2010.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sharps P, Alhusen JL, Bullock L, et al. Engaging and retaining abused women in perinatal home visitation programs. Pediatrics. 2013;132(Suppl 2):S134–139. doi: 10.1542/peds.2013-1021L. [DOI] [PMC free article] [PubMed] [Google Scholar]