Abstract
Obesity has become a truly global epidemic, affecting all age groups, all populations, and countries of all income levels. To date, existing policies and interventions have not reversed these trends, suggesting that innovative approaches are needed to transform obesity prevention and control. There are a number of indications that the obesity epidemic is a systems problem, as opposed to a simple problem with a linear cause-and-effect relationship. What may be needed to successfully address obesity is an approach that considers the entire system when making any important decision, observation, or change. A systems approach to obesity prevention and control has many benefits, including the potential to further understand indirect effects or to test policies virtually before implementing them in the real world. Discussed here are 5 key efforts to implement a systems approach for obesity prevention: 1) utilize more global approaches; 2) bring new experts from disciplines that do not traditionally work with obesity to share experiences and ideas with obesity experts; 3) utilize systems methods, such as systems mapping and modeling; 4) modify and combine traditional approaches to achieve a stronger systems orientation; and 5) bridge existing gaps between research, education, policy, and action. This article also provides an example of how a systems approach has been used to convene a multidisciplinary team and conduct systems mapping and modeling as part of an obesity prevention program in Baltimore, Maryland.
Keywords: global health, modeling, obesity, systems science
INTRODUCTION
Obesity has become a truly global epidemic, affecting all age groups, all populations, and countries of all income levels.1,2 Worldwide, over 1.9 billion people are obese,3 with approximately 10% of children aged 5 to 17 years overweight in 20044 and 40 million preschool children overweight in 2008.5 Many countries in nearly all continents have either high or rising obesity rates,2,3 and 65% of the world’s population lives in a country where overweight or obesity causes more mortality than underweight.3 In the United States, approximately 70% of adults and 32% of children are overweight or obese, with a continuing rising trend.6,7 To date, existing policies and interventions have not reversed these trends, suggesting that new innovative approaches are needed to transform obesity prevention and control.8 As a 2013 Institute of Medicine report suggested, what may be needed is a systems approach to addressing obesity.9 In this paper, we introduce the concept of a system and posit that obesity is a systems problem. We then describe what is meant by a systems approach, detail the benefits of such an approach, discuss 5 key efforts that comprise a systems approach to obesity, and offer an example of a systems approach to obesity prevention in Baltimore.
WHAT IS A SYSTEM?
A system is composed of a group of different components that are interconnected; these components interact with and affect one another. Examples of natural and human-made systems include meteorological, biological, transportation, manufacturing, financial, health care, and food systems. In a food system, for example, the type of food available in a neighborhood depends on what is sold by retailers such as grocery and corner stores. The offerings of grocery and corner stores depend on the offerings of their wholesale suppliers, which may change according to the demand for different types of food. The demand for different types of food is affected, in turn, by the relative prices of foods, advertising, and social connections, which are affected, in turn, by food producers and processors, which are affected, in turn, by economic conditions. These components and the relationships between them interact in many complex ways that go beyond single cause-and-effect relationships.
The hallmark of a system is that none of its parts is completely independent. Instead, properties of a system are interconnected, influencing one another in a variety of manners, both obvious and subtle. As such, before a larger system can be fully explained, each of its component parts and their interactions must be understood.10 Significant perturbation of one part tends to have reverberations throughout other parts of the system. Therefore, unless the system is well understood, it can be challenging to identify the root cause of an observed phenomenon or to predict the effects of an intervention. An example of a problem for which it is difficult to identify the root cause is the lack of nutritious food options in low-income urban areas.11,12 A shortage of apples on a farm, for instance, may decrease the apple supply and increase the cost for storeowners to stock apples. As a result, perhaps only larger supermarkets can afford the added cost of stocking the apples, as opposed to smaller grocers in marginalized communities. Should a small grocer find the means to stock apples, the increased cost would likely be passed on to the customer. If the apples do not sell because of their high price, this could result in wasted food and discourage the storeowner from stocking apples in the future. Unless one knows how this particular food system works, finding the root cause of an observed phenomenon can be difficult. In this example, is the lack of apples the result of stores changing their business practices, or the result of the wholesalers or food producers changing theirs? Properly diagnosing and addressing such a problem requires an understanding of the components of the food system and the connections between these components.
Despite the interconnectedness of the components of a system, a systems approach requires that the researcher set boundaries on the system. The boundaries of a system distinguish it from other systems by defining which components are included and which are excluded. The boundaries of a system may refer to geography, concepts, or processes. Since many systems are highly interconnected with each other, boundaries may not always be clearly defined. Decisions about system boundaries should be driven by the research question or problem being considered. Following the Principle of Parsimony, one would draw boundaries in a way that accounts for the vast majority (>80%) of the components and relationships that are relevant to the research question or problem, with some components inevitably excluded. For example, when considering a change in school vending machines, one might draw boundaries around not just the school but also the surrounding neighborhood because children may seek food from nearby sources; the boundary might exclude food stores in a different city if the children are unlikely to seek food from far away.
WHY OBESITY IS A SYSTEMS PROBLEM
There are a number of indications that the obesity epidemic is a systems problem, as opposed to a simple problem with linear cause-and-effect relationships, and that it, therefore, requires a systems approach.13,14 Described here are several indications that obesity is a systems problem: global scope, heterogeneous patterns, wide-ranging impacts, lack of a single cause, and the failure of single solutions.
Global scope
Obesity has become a global epidemic, spreading to a great diversity of countries and populations.1 Even many low-income countries that have continued to struggle with undernutrition are now facing obesity.1,15 The diverse characteristics of the wide range of countries affected by obesity suggests that a simple individual factor, such as excess food, is insufficient to explain the epidemic and a more holistic approach is needed to understand the system underlying this issue.
Heterogeneous patterns
Within countries affected by the epidemic, obesity displays heterogeneous patterns that are not easily explainable.1,2 Obesity prevalence began rising much more precipitously in the 1980s than in previous decades, with the prevalence more than doubling since 1980.2,3 But the rate of this rise was not equal among different countries or even among countries in relatively close proximity. In fact, within a given country, obesity trends often vary substantially among different subpopulations. In the United States, for example, greater increases have occurred in certain inner-city locations and among certain socioeconomic groups.7 These complex patterns are not consistent with a simple cause-and-effect relationship.
Wide-ranging impacts
Obesity also has wide-ranging and complex consequences. One aspect of obesity that creates complexity is the time lag. Changes in weight may develop over a long period of time16; additionally, there may be a lag between a change in weight and the manifestation of outcomes.17 These outcomes go beyond direct effects such as hypertension, atherosclerosis, type 2 diabetes, and cancer and include bullying, depression, and low self-esteem.18–20 In other words, the impacts of obesity are wide ranging and include biological, psychological, and social effects that influence aspects of life such as physical health, sleep patterns, productivity, social interactions, and feelings of self worth. This multitude of complex consequences results in considerable disease and cost burden to individuals, society, and third-party payers.21
Complex causes
In addition to complex consequences, obesity displays complex causes. Research efforts have failed to identify a single cause of the obesity epidemic.22 In fact, evidence suggests that multiple factors acting at different scales may be contributing. Figure 1 shows different scales relevant to obesity, including genetics, biology, individual behaviors, social network dynamics, the environment, and larger societal forces. The biological scale includes physiologic processes such as leptin sensitivity and individual metabolism. Individual behaviors include dietary and physical activity choices, while social networks dynamics include connections to family and friends, which may also influence individual behaviors. The environmental scale includes food availability, green spaces for physical activity, and neighborhood safety. Larger societal forces include economics, policy, education, health awareness, and culture. Each of these scales has different factors either directly or indirectly associated with obesity. For example, food marketing practices and reductions in physical activity are 2 “forces” frequently cited as reasons for the increase in obesity.22 However, both of these forces incorporate factors from different scales. Marketing influences the built environment by determining product placement and the availability of certain foods. Features of the built environment such as the location of parks and recreation centers affect the propensity of individuals to engage in physical activity. Both marketing and the built environment are driven by societal forces such as economics. Marketing messages can be mediated by social dynamics, influencing their effect on dietary or physical activity habits. Marketing messages can also differ in their impact according to an individual’s psychological factors, such as their beliefs and biases. Individual biology and genetics mediate the translation of energy intake and expenditure to changes in body mass index.23 Moreover, a person’s environment influences his or her genetic expression during development (i.e., epigenetics).22
Figure 1.
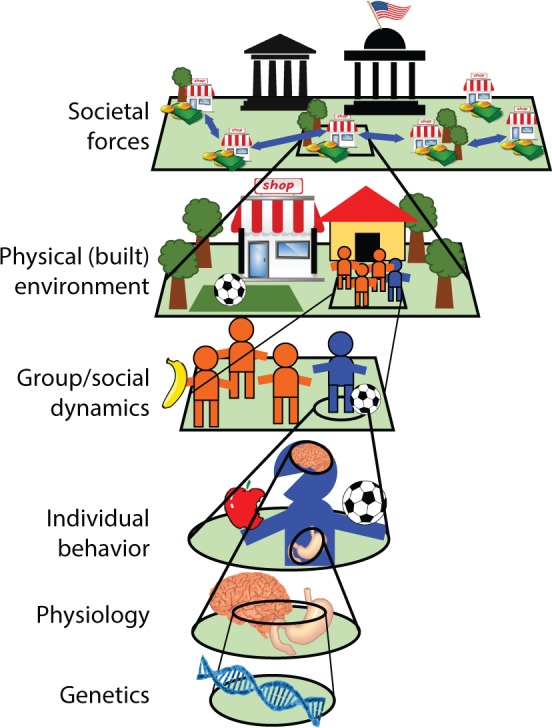
Illustration of how multiple factors acting across a range of scales can contribute to obesity.
These are just some of the multiscale factors that may be involved; others continue to emerge, such as medication use.24 Of course, some of these may be mediators and not necessarily originating causes, but how all of these factors fit together in a system remains to be elucidated. While extensive knowledge exists regarding some of the microprocesses within a given scale, a scientific framework that integrates these pieces of knowledge in a useful way is lacking. For example, there is in-depth knowledge of specific epigenetic and psychological phenomena and information on how policies and environments are linked to behaviors and health outcomes, but without bringing these data together, it is difficult to understand the inconsistencies observed in parts of the system. This may result in important causes, mediators, and other dynamics in the system being missed.
It should be noted that the relationship between any 2 factors is not always straightforward. For example, in 2 recent reviews, Salvy et al. examined peer influences on diet25 and physical activity26 behaviors of children and adolescents. The physical activity–focused review suggests that peers can both increase physical activity (through motivation and the rewarding value and normative nature of physical activity) and decrease physical activity (through ostracism, peer victimization, or isolation).26 The dietary behavior–focused review concluded that the presence of peers can both increase the energy intake of adolescents (through social facilitation and emulation of others’ behavior) and decrease energy intake (through the promotion of healthy eating norms among friends).25
An existing framework to describe the complex causes of obesity is the 6 Cs conceptual model. Building on Bronfenbrenner’s ecological model of human development,27 Harrison et al.28 reviewed the literature and developed the 6 Cs conceptual model of childhood obesity to summarize the factors with the greatest importance for the developing child. The 6 “Cs” included in the model are cell (genetic predispositions and other biological factors), child (characteristics of the child), clan (family characteristics), community (peers, schools, and other institutional factors specific to an early adolescent’s social world outside of the home), country (state and national policies, programs, and priorities), and culture (norms, myths, and biases that guide behavior). None of these 6 Cs is solely responsible for obesity, and the 6 Cs all interact with each other in complex ways.
No single solution
A final indication that obesity is a systems problem is that solutions addressing a single cause have not been successful. Despite the emergence of many different diets, exercise programs, and procedures targeting a single cause, obesity rates have continued to rise worldwide.3 Meanwhile, multilevel, multicomponent interventions have tended to be more successful.29–32 For example, multicomponent interventions that included culturally targeted and tailored components (e.g., health education, diet, physical activity, reduced screen time, behavioral skills, and motivation groups) have shown a greater impact on health behaviors associated with obesity in minority youth than the individual components in isolation.31
Benefits of a systems approach for policy and interventions
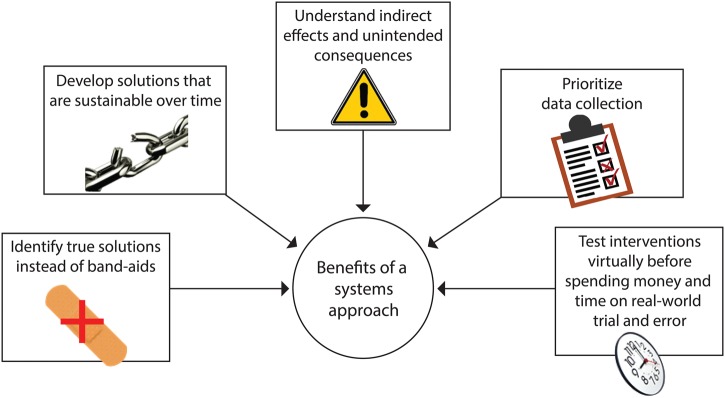
A systems approach takes the entire system into consideration when making any important decision, observation, or change. Fields such as air traffic control, transportation, manufacturing, and finance have used different methods to better understand and represent systems before making decisions.33,34 This section describes the benefits of using a systems approach for policy and interventions. As shown in Figure 2, a systems approach can facilitate the identification of true solutions, assess the long-term sustainability of solutions, understand indirect effects and unintended consequences, inform the prioritization of data collection, and test interventions virtually before implementing them in the real world.
Figure 2.
Benefits of a systems approach for policy and interventions.
When problems arise, a systems approach can facilitate the search for solutions that address the root cause, rather than “band-aids.” When a decision maker does not know the root cause or even the wide-ranging ramifications of a problem, the chosen tactic may not completely solve the problem. Such a tactic may cover up the problem without providing a real solution. Additionally, “band-aid solutions” may offer solutions that work only for some people, such as those that can most readily change their behavior. Thus, a risk is that these types of solutions may only exacerbate health disparities. For example, simply encouraging people to eat healthier foods may work for some people if they have access to healthy foods and have the time and resources to purchase and prepare these foods. However, many people may not have access to healthy foods.35 The stores around them may not stock enough fruits and vegetables. Other daily stresses may not afford them enough time to shop and cook. Even if they live close to stores that sell healthy food, they may not have enough funds to purchase healthier options. Therefore, educational campaigns may help, but they do not fundamentally improve the food environment. Another example is removing soda machines from schools, which may decrease soda purchases inside the school but could simply shift soda purchasing to locations outside the school.36
A systems approach allows a decision maker to assess the long-term sustainability of a solution. When the underlying cause of a problem is not addressed, a “solution” may work temporarily but lose effectiveness as time and current circumstances pass. For example, providing temporary incentives for stores to stock healthier food options may change the stores’ stocking patterns for a period of time. However, if stores lack the infrastructure (such as adequate refrigeration for perishable produce) and consumer demand to maintain such inventories, they may soon opt to stock foods that can be stored for longer periods of time and have greater demand from patrons, such as energy-dense snack foods.
Indirect effects and unintended consequences can be identified through a systems approach. A decision maker may underestimate a problem, not realizing its full impact over time. For instance, decision makers may not realize the full impact of a poor food environment because the change in overweight and obesity prevalence may occur gradually over time, and reversing such trends may take considerable time and effort. Not realizing the full impact of a change can also skew a person’s choices among alternatives; in other words, he or she may not fairly compare the potential impact of each choice. When a person does not know the full impact of different choices, even well-meaning efforts can lead to unintended consequences. For example, increasing requirements for store owners to stock healthy foods without ensuring they can maintain or increase their profits may motivate them to relocate, further reducing food options and worsening the food environment.
A systems approach can inform the prioritization of data collection in order to avoid collecting superfluous or even misleading information. Collecting data requires time, effort, and resources, necessitating difficult choices about what data to collect; collecting all data on a system is prohibitively expensive and unfeasible. Furthermore, biases may influence decision makers to prioritize certain economic or political factors over others. Modeling in a multidisciplinary team can reduce the effects of individual biases and make decisions and outcomes more explicit and transparent. Understanding the system can thereby help guide and prioritize data collection. For example, evaluating all of the ongoing dietary and physical activity behaviors in a location may be prohibitively expensive. With constrained resources, what are the highest-impact data that should be collected? What information would best help decision-making and lead to meaningful change? What data would give the most accurate picture of the system as opposed to only 1 part of the system?
Lastly, a systems approach allows a decision maker to virtually test an intervention before implementing it in the real world, which requires time, effort, and resources. When the system is not well understood, designing and refining effective interventions may take longer. The intervention designer may have to rely on trial and error to learn how to tailor the intervention appropriately, and initial attempts may yield surprising results. For instance, while some obesity prevention interventions entail removing soda vending machines from schools, Taber et al.36 found that students in schools without vending machines were actually more likely to consume additional servings of soda per week and to consume fast food more frequently. This association was limited to areas where soda and restaurant foods were not taxed, and this heterogeneity of results suggests that vending machines are just one of many interacting components within a complex system. In the case of school vending machines, systems modeling may have allowed researchers to identify unintended consequences and to tailor the intervention accordingly prior to implementation.
A SYSTEMS APPROACH TO OBESITY
While many industries have long used systems approaches, adoption of systems approaches in the field of obesity prevention and control has lagged by comparison. A similar lag can be seen in other areas of health and public health, but systems approaches have made some inroads in infectious disease prevention and control, helping decision makers understand the spread of infectious diseases in a given location, the consequences of infectious disease, and the potential impact of various control measures.37–44
What are the reasons for the lag in systems approaches to obesity? One reason may be that obesity, until recently, has been viewed as more of an individual patient problem rather than a broader public health problem. The recognition that obesity is now a global epidemic may be changing that viewpoint. Emerging evidence supports the importance of other factors beyond the individual.45,46 Another reason may be a lack of familiarity with systems methods, which in part stems from education and training. Although basic mathematical modeling is a required course for many business and engineering education programs, training in systems approaches has not traditionally been a part of education in nutrition, medicine, public health, and health policy. While each field has its nuances, problems in nutrition, medicine, and public health may be very amenable to systems approaches as long as the approaches and methods are modified accordingly. Many of the same general challenges exist across different fields, such as uncertainty, data gaps, multiple stakeholders, and resource constraints. What is different across fields is the nature and the degree of these challenges. In many ways, the very high stakes (e.g., cost, morbidity, and mortality) and the complexity of the issues with the obesity epidemic make a systems approach all the more important. There may also be a perception that systems methods would somehow replace decision makers or more traditional methods; for example, would decisions be made by computers or by those without the requisite knowledge and experience? As illustrated later, systems methods can facilitate current methods of decision-making rather than displace them.
Given that the field of obesity prevention and control lags in its utilization of a systems approach, the following 5 efforts would facilitate the adoption of such an approach:
Effort 1: utilizing more global approaches
One part of the systems approach is understanding that obesity has become a global problem. Countries throughout the world are becoming increasingly interlinked through travel, communications, manufacturing practices, food systems, and the spread of different sociobehavioral norms. This interconnectivity means that changes in 1 country may percolate throughout other countries and may be mediated differently by the context of each country. Therefore, approaches to the obesity epidemic may need to increasingly consider these global systems of interconnectivity and involve cooperation among stakeholders from different countries. To date, compared to other global health initiatives such as smallpox eradication or pandemic influenza preparedness and response,47–53 there has been relatively less international coordination. The amount of funding and the number of initiatives that have crossed country borders have been limited. Many of the formal obesity prevention and control initiatives have been at a more local scale. The sugar-sweetened beverage tax in Mexico is a notable exception in the amount of international attention that it has received.
Effort 2: cultivating expertise from multiple disciplines
The great systems challenges of our history have required multidisciplinary teams. For instance, in the Space Shuttle program in the United States, experts in aerospace engineering worked alongside nutrition experts who helped understand food and beverage requirements for astronauts, psychologists who elucidated the stresses that astronauts may face, and experts from many other disciplines to ensure that the astronauts’ environments could facilitate their performance.54 Neglecting to include any of these experts could have led to an oversight that would have inhibited the mission’s success. Similarly, to address obesity, many disciplines that have not traditionally dealt with obesity, such as engineering and computer science, can bring important new perspectives and methodological approaches. However, they will need guidance from experts with deep knowledge in the fields most traditionally relevant to obesity – nutrition, epidemiology, and psychology – because many of the associated issues are much more complicated than they initially appear.
Effort 3: utilizing systems methods
Two key tools for understanding a system are systems mapping and systems modeling. In this section these methods are described, examples of their applications are provided, and new directions in this area of research are discussed. A critical first step of a systems approach is to delineate an overall picture of the entire system. Systems mapping shows how different parts of a system fit together and interact. To begin, a consensus on the boundaries and components of a system must be reached. This may entail collecting stakeholders together in a group mapping exercise to offer suggestions and then discuss which components should be included and excluded. Identifying the components of a system, in itself, can be enlightening. At first glance, people may not realize that certain people, groups, organizations, or other factors play a role in the system. After the components are identified, the team determines how these components may be interrelated. For example, what effect does a single school have on a larger food system? A school can provide food through meal programs, advocate for stores around its neighborhood to sell particular types of food, and teach children to adjust their food-purchasing behaviors. A team can use different platforms to visualize these components and relationships, such as drawing influence, network, or causal loop diagrams on a poster, a whiteboard, or a computer screen. A number of software packages are available to help with such diagrams (e.g., STELLA, Vensim, and Powersim).
It can be particularly helpful to convene multidisciplinary groups to inform the systems mapping process because 1 person or discipline may not have the expertise necessary to understand all parts of the system. For example, when mapping a food system, an urban planner can describe how the location of different food sources such as grocery stores could affect access. An economist can quantify the relationship between pricing and demand for different food items. An operations researcher can outline the food supply chain and links between the manufacturers, suppliers, and retailers. An agricultural specialist can shed light on the determinants of crop size. A sociologist can elucidate how different social influences such as peers may change purchasing behavior, which in turn, would affect what the food retailers stock. Nutrition experts can identify how the consumption of certain foods may affect the population’s health.
A second methodology is systems modeling, in which computer programs based on mathematical equations are used to represent the components, relationships, and processes in a system. Systems mapping, as described above, frequently precedes the modeling process. Informed by the research question of interest, modelers can define the system and set its boundaries. Additionally, modelers can determine inputs to populate the model by drawing from available data, existing literature, established theories, and input from field experts. While systems models are, by definition, simplified representations of reality, an important aspect of developing a systems model is to add to the validation of the model at each step. Model development and validation occur in a stepwise, iterative manner. At each stage of development, showing the model to key stakeholders can improve the model’s face validity (i.e., do the stakeholders agree that the model represents what it is supposed to represent?). Running the model and comparing the results to real-world findings and similar studies can improve the model’s criterion validity (i.e., do the data show that the model is consistent with real-world findings?). Validated models can then essentially serve as “virtual laboratories” to examine how a system operates and test the effects of different changes within the system. An example of computational modeling is air traffic control systems. Air traffic control systems combine information from different sources (such as data on the weather, the environment, runway capacity, and plane location) with information on how these factors work together (such as data-driven knowledge of how weather patterns impact flight times and routes). A computational simulation model is then used to represent all the components and processes of the system in order to help users view the system as a whole and make appropriate decisions. Even though it may not function perfectly – for example, travelers may still experience delays – modern air travel would not be possible without air traffic control systems. These computational systems allow us to coordinate daily operations, diagnose vulnerabilities in the system, and anticipate the impact of new technologies or changing circumstances (e.g., delays due to mechanical issues or weather events).
Although there have been some initial applications, the use of systems methods to address food, nutrition, and obesity issues is still relatively nascent. Some investigators have used modeling approaches to evaluate specific parts of relevant systems to generate theoretical insights. A specific method that has been used is social network analysis, which characterizes how people are connected with each other and examines how these connections can influence diet, physical activity, and obesity. Social network analysis uses nodes to represent people, groups, or organizations; lines drawn between the nodes (otherwise known as edges or ties) represent social connections. This serves not only to visually demonstrate how people are connected, but also to characterize patterns of connections and analyze how these may correlate with the spread of behaviors and health outcomes.55 Such analyses have shown that socially connected individuals tend to have similar eating patterns56 and similar physical activity57 behaviors. These findings may help explain why studying the social networks of participants in the Framingham Heart Study revealed “clusters” of obese persons, indicating that people with social connections to obese individuals are more likely to become obese themselves.58
Systems modeling is also used to represent ways in which people can be influenced by other people and by their environments over time. A modeling method that can represent aspects of individual behavior and decision-making in the context of a broader social environment is an agent-based model (ABM). An ABM typically consists of computer agents representing people, animals, or objects. What distinguishes an ABM is that each agent is autonomous (meaning that they perform decision-making) and displays complex adaptive behaviors (meaning that they learn and can change their decision-making over time). ABMs simulate the simultaneous interactions of multiple agents to recreate and predict complex phenomena and processes. Studies using ABMs have provided insight into the determinants of individual food consumption behaviors, which can be influenced by early exposures to certain foods that have a “lock-in” effect,59 as well as by peer influence among high schoolers.60 Other studies have utilized systems models to translate changes on one scale (e.g., individual) to other scales (e.g., population), such as a system dynamics model developed by Fallah-Fini et al.61 that captured the relationship between individual energy gaps and population-level trends in obesity.
Applying systems models to test potential interventions can inform programs and policies. Such studies may help identify which interventions – or combinations thereof – may be most impactful in a given setting. When using an ABM to compare access to supermarkets, physical activity infrastructure, and school quality, Orr et al.62 found that all 3 interventions decreased disparities in body mass index between black and white populations but noted nuances such as some interventions varying in their impact over time or having synergistic effects with other interventions. One such interaction between interventions was also present in an ABM developed by Auchincloss et al.,63 which showed that increasing both access to affordable healthy foods and preferences for such foods was necessary to reduce disparities in diet between households of different income levels. Systems modeling can identify circumstances that may cause a particular intervention to be more or less successful, as Li et al.64 found that the influence of a nutrition education campaign on individuals’ food choices varied between neighborhoods depending on social norms.
While such work has helped generate theoretical insights, the current body of literature only scratches the surface of how systems models can be used. Next possible steps include developing new ways of representing various factors and processes, building increasingly complex systems models with more real-world data and realistic representations, expanding the types and aspects of relevant systems covered by the model, and expanding the use of systems models in decision-making. As mentioned previously, systems methods such as systems mapping and modeling have the potential to transform obesity prevention and control as they have other fields. However, direct transfer of systems methods and tools to obesity may not be adequate; modifications will be required due to some key differences between obesity prevention and other fields. This could be accomplished in several ways, depending on the question of interest and the tools available: New models and methods may need to be developed or existing models and methods may need to be altered. Many systems models would have to effectively combine economic, operational, epidemiological, and clinical aspects of obesity prevention and control. Unlike manufacturing systems where the objective may be to maximize output while minimizing cost, with a food system, one may need to optimize a broader and different set of measures. It is also necessary to adapt existing systems models to incorporate structures and outcomes more relevant to nutrition and health. For example, some existing models of food supply focus on operational measures such as lead time, stockouts, and profits, but they do not translate such measures to nutrition and health outcomes.65–67
Another frontier is bringing systems modeling closer to decision makers by making models easier for nonmodelers to understand, training nonmodelers to have increased literacy in systems models, and making models more relevant by expanding their applications. This will include developing a generation of decision makers who are conversant in systems methods and can implement more systems-oriented policies. For example, Hawkes et al.68 recommended policies intended to not only change consumer behavior, but to also induce a response from the food system, such as nutrition labels that can provide information to consumers as well as stimulate product reformulation. Policies such as this, which work at the systems level, are more likely to be developed when policy makers are conversant in a systems approach.
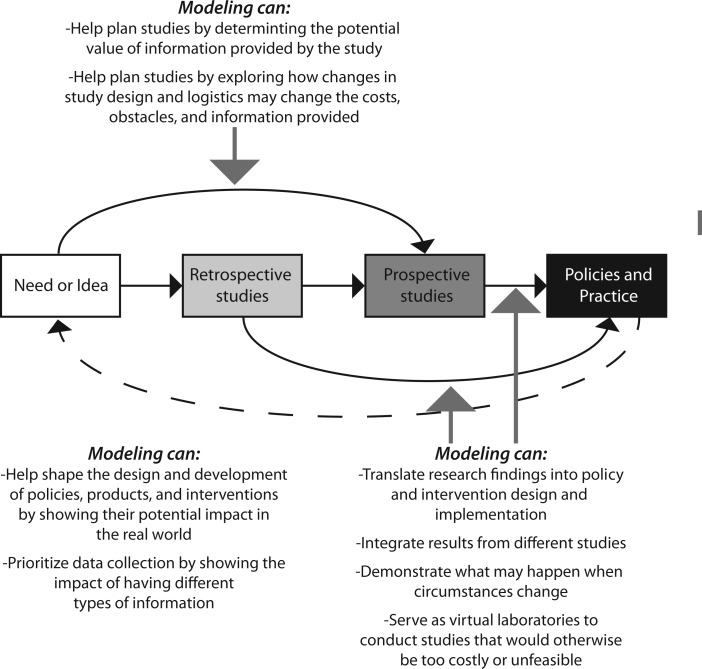
Effort 4: applying a systems orientation to traditional approaches
Systems approaches do not have to replace traditional public health methods. In fact, systems methods can help bridge and enhance existing methods (Figure 3). Modeling can help plan retrospective and prospective studies by assisting with logistics, forecasting possible outcomes, and estimating the value of the additional data these studies will provide. Modeling can extend results from retrospective and prospective studies to other locations and circumstances. Modeling can also help combine results from different retrospective and prospective studies. Additionally, modeling can assist with translating results from retrospective and prospective studies to real-world decision-making regarding policies and interventions.
Figure 3.
Illustration of how modeling acts as a bridge to translation.
Effort 5: bridging research, education, policy, and action
Bringing systems approaches to obesity prevention and control involves shifts in research, education, policy, and action. As mentioned earlier, systems approaches have not traditionally been part of educational programs in obesity-related disciplines. Therefore, newly minted researchers, clinicians, and policy makers are not entering their careers conversant in systems thinking. Similarly, research that does not account for systems may not generate innovations that are as policy-relevant as they could be. Finally, when clinicians, policy makers, and other decision makers do not have systems in mind, they may not see the connections between research efforts and their decision-making. All of these activities should not be separate but instead need to synergize with each other. For example, researchers who understand clinical and policy considerations may be able to pursue more impactful lines of inquiry, and policy makers who are comfortable interpreting research can identify innovations that are useful for their given contexts.
Bridging research, education, and policy can be achieved through a number of strategies. Systems science experts can provide training for health professionals and decision makers in systems thinking; for example, training could cover the importance of a systems approach, methods in systems science, and how systems thinking can be incorporated into respective fields of work. Systems scientists may also work with researchers and decision makers to develop systems models to better understand questions or policies related to a particular system, such as understanding the major driving factors, exploring the potential consequences of intervening in a system, and identifying unintended consequences. For example, some are interested in adapting warning labels on sugar-sweetened beverages, similar to those previously used to deter cigarette smoking. Systems science approaches can help decision makers identify strategies that would make such a policy most impactful, such as utilizing the most effective label placement and reaching an appropriate target audience.
EXAMPLE OF A SYSTEMS APPROACH TO OBESITY
A practical example of taking a systems approach to obesity prevention and control has been the Global Obesity Prevention Center’s (GOPC) ongoing work in Baltimore, Maryland. The Baltimore Metropolitan Area, a large socioeconomically and racially/ethnically diverse area, has higher obesity rates than the United States’ average, with more than 68% of adults69 and 38% of children estimated to be overweight or obese.70 The GOPC’s Baltimore Project (B’More Healthy Communities for Kids71,72) has taken a systems approach to try to stem rising rates of obesity among early adolescents in some of Baltimore’s low-income neighborhoods. The interest in this age group emerged from the finding that early adolescence (between the ages of 10 and 14 years) is 1 of the 3 developmental periods during which youth are likely to experience rapid weight gain.73 Additionally, as children enter adolescence, they experience increasing financial independence and autonomy when making food choices. Overweight adolescents are much more likely to become obese adults. If obese at age 10, males have a 37% probability and females a 52% probability of being obese at age 35 (77% for males and 68% for females at age 18).74
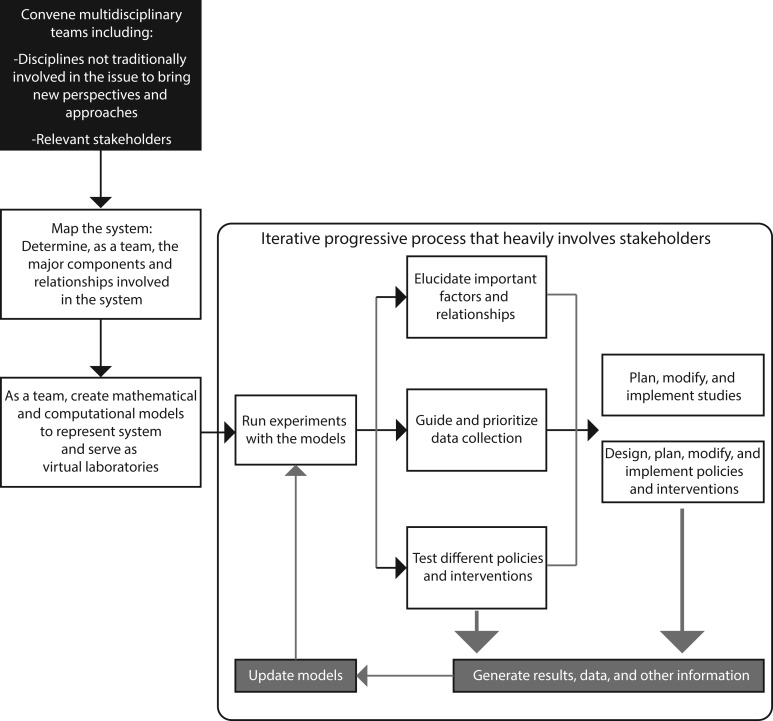
Figure 4 shows the process involved in a systems approach to obesity control. The first step is to convene multidisciplinary teams to help better understand what is causing obesity in a given population and location. In Baltimore, this occurred with the GOPC forming a Baltimore Policy Working Group, which included GOPC experts from a variety of disciplines including operations research, civil engineering, health policy, and nutrition working in collaboration with nearly 40 participants from the Baltimore community. These community representatives included municipal entities such as the City Council, the Baltimore Food Policy Initiative, the Baltimore City Health Department, Baltimore City Public Schools, and Baltimore City Department of Recreation and Parks; nonprofit organizations such as the Baltimore Partnership to End Childhood Hunger and the Family League of Baltimore; food wholesalers; and academic partners such as the Johns Hopkins Center for a Livable Future.
Figure 4.
Illustration of how a systems approach iteratively brings together various disciplines, stakeholders, and methods.
A second step is to develop computational models to represent the relevant systems at work. In Baltimore, GOPC Members developed the Baltimore Low Income Food Environment (BLIFE) model,72 an ABM representing low-income inner-city neighborhoods that have been designated as food deserts (i.e., locations with relatively low access to healthy foods and beverages) and their early adolescent inhabitants. For example, the GOPC team developed the BLIFE model to aid Baltimore City policy makers and stakeholders in exploring the factors leading to obesity among school-age children. Each child in this ABM is represented by a computational agent and has a gender, age, weight, height, and a healthy-to-nonhealthy food preference ratio that governs the types of food that the agent seeks. Each simulated day, the child agents move virtually from their households to their assigned schools and then to various food sources and recreation locations after school before returning home. Although the simulated movements are virtual, the model is geospatially explicit and the locations for places such as schools, corner stores, and recreation centers are based on real geographic data for the modeled area. The agents expend calories by walking between locations and by exercising at recreation centers (based on data for the child’s age and gender). They consume calories by eating at different food sources, with the caloric intake depending on the food offerings available at a given food source. Agents have a set of decision points throughout the day, and parameters associated with these decision points are informed by a range of data sources including the US Census, National Health and Nutrition Examination Survey, InfoUSA, and expert input. Each agent has an embedded temporal difference reward-learning model that reinforces habits59; for example, choosing unhealthy food will reinforce such behavior and lead to a higher probability of choosing unhealthy food later. Each agent also has an embedded metabolic model that represents the metabolic processes that link caloric intake and expenditures to changes in body mass index and perturb age- and gender-specific US Centers for Disease Control and Prevention growth curves.75 Excess caloric intake translates to an increase in the BMI over the standard growth curve. The BLIFE Model has served as a “virtual laboratory” to better understand the system that includes the food environment, the physical activity environment, and the early adolescent population and to test different possible interventions within the safety of a computer before attempting to implement them in the real world.
As Figure 4 shows, the systems models can then help tailor appropriate field studies and, ultimately, the design and implementation of interventions. These field studies and interventions, if accompanied by data collection, can then update and further refine existing systems models. The GOPC is also conducting multilevel systems community interventions including cooking classes, peer mentoring, advertisements to promote healthier eating choices, and incentives for store owners to stock more healthy foods. Data from these studies can be incorporated into BLIFE, which can then provide forecasting for policy makers grounded in more real-world data.
As Figure 4 also shows, this systems approach is iterative. While the initial version of a systems model like BLIFE may be based on more limited initial data, the cycle seen in Figure 4 progressively moves the model to become increasingly representative of the actual system. This emphasizes that perfect data are not needed to begin constructing a systems model. The actual process of building the model can help stakeholders better understand the system, raise important questions, and guide data collection. The value of a systems model does not necessarily lie in data alone, and even a model that is relatively data poor can be very informative. Involving key stakeholders in the modeling process from the beginning helps researchers to better understand the system and helps stakeholders to better understand the utility and the findings of the model.
CONCLUSION
The obesity epidemic has continued to spread worldwide, suggesting that policies and interventions to date have not been fully effective. The characteristics of the obesity epidemic suggest it is a systems problem that could benefit from a systems approach. Systems approaches have transformed many industries and professions and new systems approaches and methods have the potential to similarly transform obesity prevention and control. A systems approach to obesity entails 5 key strategies: a global approach; interdisciplinary collaboration; utilization of new systems methods; modifications of existing methods; and bridging research, education, policy, and action.
Acknowledgments
The articles in this supplement were presented as part of the Tenth Nestlé Nutrition Conference on Research Perspectives for Prevention of Diabetes: Environment, Lifestyles, and Nutrition, held in Mexico City on November 12 and 13, 2014. The conference was organized by the Nestlé Nutrition Fund of the Mexican Health Foundation, the National Institute of Medicine, and Nutrition Salvador Zubirán. The supplement coordinators are Ernestina Polo-Oteyza, Mexican Health Foundation, and Héctor Bourges-Rodríguez and Carlos Aguilar-Salinas, National Institute of Medicine and Nutrition Salvador Zubirán, Mexico.
Funding. The conference and this supplement were funded by the Nestlé Nutrition Fund of the Mexican Foundation for Health. B.Y. Lee and J. Gittelsohn received travel support from the Nestle Foundation to attend the Tenth Nestlé Nutrition Conference on Research Perspectives for Prevention of Diabetes: Environment, Lifestyles, and Nutrition. This publication was additionally supported by the Global Obesity Prevention Center at Johns Hopkins; the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD); the Office of the Director, National Institutes of Health (OD), under award number U54HD070725; the Agency for Healthcare Research and Quality via award number R01HS023317; and NICHD via award number U01 HD086861. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of interest. The authors have no relevant interests to declare.
References
- 1.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly T, Yang W, Chen CS, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32:1431–1437. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Media Centre: Obesity and Overweight. 2015. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed June 1, 2015. [Google Scholar]
- 4.Ahmad QI, Ahmad CB, Ahmad SM. Childhood obesity. Indian J Endocrinol Metabol. 2010;14:19–25. [PMC free article] [PubMed] [Google Scholar]
- 5.de Onis M, Blossner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92:1257–1264. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. J Am Med Assoc. 2012;307:483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. J Am Med Assoc. 2012;307:491–497. [DOI] [PubMed] [Google Scholar]
- 8.Roberto CA, Swinburn BA, Hawkes C, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385:2400–2409. [DOI] [PubMed] [Google Scholar]
- 9.Committee on Evaluating Progress of Obesity Prevention Efforts, Food and Nutrition Board, Institute of Medicine. Evaluating Obesity Prevention Efforts: A Plan for Measuring Progress. Washington, DC: National Academies Press; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Ann Rev Public Health. 2012;33:357–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prevent Med. 2009;36:74–81, e10. [DOI] [PubMed] [Google Scholar]
- 12.Lee SH, Rowan MT, Powell LM, et al. Characteristics of prepared food sources in low-income neighborhoods of Baltimore City. Ecol Food Nutr. 2010;49:409–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bures RM, Mabry PL, Orleans CT, et al. Systems science: a tool for understanding obesity. Am J Public Health. 2014;104:1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: science, policy, and action. Lancet. 2011;378:838–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McTigue KM, Garrett JM, Popkin BM. The natural history of the development of obesity in a cohort of young US adults between 1981 and 1998. Ann Int Med. 2002;136:857–864. [DOI] [PubMed] [Google Scholar]
- 17.Chiolero A, Paradis G, Madeleine G, et al. Discordant secular trends in elevated blood pressure and obesity in children and adolescents in a rapidly developing country. Circulation. 2009;119:558–565. [DOI] [PubMed] [Google Scholar]
- 18.Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. J Am Med Assoc. 2013;309:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glass TA. Social class and child health: our complexity complex. In: Landsdale NS, McHale SM, Booth A, eds. Families and Child Health. New York: Springer Science; 2013:143–154. [Google Scholar]
- 20.Dixon JB. The effect of obesity on health outcomes. Mol Cell Endocrinol. 2010;316:104–108. [DOI] [PubMed] [Google Scholar]
- 21.Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31:219–230. [DOI] [PubMed] [Google Scholar]
- 22.McAllister EJ, Dhurandhar NV, Keith SW, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009;49:868–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell CG, Walley AJ, Froguel P. The genetics of human obesity. Nat Rev Genet. 2005;6:221–234. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz BS, Bailey-Davis L, Bandeen-Roche K, et al. Attention deficit disorder, stimulant use, and childhood body mass index trajectory. Pediatrics. 2014;133:668–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salvy SJ, de la Haye K, Bowker JC, et al. Influence of peers and friends on children's and adolescents' eating and activity behaviors. Physiol Behav. 2012;106:369–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salvy SJ, Bowker JC, Germeroth L, et al. Influence of peers and friends on overweight/obese youths' physical activity. Exercise Sport Sci Rev. 2012;40:127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bronfenbrenner U, Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 2009. [Google Scholar]
- 28.Harrison K, Bost KK, McBride BA, et al. Toward a development conceptualization of contributors to overweight ans obesity in childhood: the six-C's model. Child Dev Perspect. 2011;5:50–58. [Google Scholar]
- 29.Gittelsohn J, Lee K. Integrating educational, environmental and behavioral economic strategies to maximize intervention effectiveness to prevent obesity. Appl Econ Perspect Policy. 2013;35. [Google Scholar]
- 30.Hollar D, Lombardo M, Lopez-Mitnik G, et al. Effective multi-level, multi-sector, school-based obesity prevention programming improves weight, blood pressure, and academic performance, especially among low-income, minority children. J Health Care Poor Underserved. 2010;21(2 Suppl):93–108. [DOI] [PubMed] [Google Scholar]
- 31.Wilson DK. New perspective on health disparities and obesity interventions in youth. J Pediatric Psychol. 2009;34:231–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Economos CD, Hyatt RR, Must A, et al. Shape Up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prevent Med. 2013;57:322–327. [DOI] [PubMed] [Google Scholar]
- 33.Quarteroni A. Mathematical Models in Science and Engineering. Notices AMS. 2009;56:10–19. [Google Scholar]
- 34.Allen TT. Introduction to Discrete Event Simulation and Agent-Based Modeling: Voting Systems, Health Care, Military, and Manufacturing. London: Springer; 2011. [Google Scholar]
- 35.Coleman-Jensen A, Gergory C, Singh A. Household Food Security in the United States in 2013. United States Department of Agriculture, Economic Research Service, Washington, DC; 2014. [Google Scholar]
- 36.Taber DR, Chriqui JF, Vuillaume R, et al. How state taxes and policies targeting soda consumption modify the association between school vending machines and student dietary behaviors: a cross-sectional analysis. PloS One. 2014;9:e98249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown ST, Tai JH, Bailey RR, et al. Would school closure for the 2009 H1N1 influenza epidemic have been worth the cost?: a computational simulation of Pennsylvania. BMC Public Health. 2011;11:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee BY, Brown ST, Bailey RR, et al. The benefits to all of ensuring equal and timely access to influenza vaccines in poor communities. Health Affairs. 2011;30:1141–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee BY, Haidari LA, Lee MS. Modelling during an emergency: the 2009 H1N1 influenza pandemic. Clin Microbiol Infect. 2013;19:1014–1022. [DOI] [PubMed] [Google Scholar]
- 40.Lee BY, Cakouros BE, Assi TM, et al. The impact of making vaccines thermostable in Niger's vaccine supply chain. Vaccine. 2012;30:5637–5643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bartsch SM, Huang SS, Wong KF, et al. The spread and control of norovirus outbreaks among hospitals in a region: a simulation model. Open Forum Infect Dis. 2014;1:ofu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee BY, Yilmaz SL, Wong KF, et al. Modeling the regional spread and control of vancomycin-resistant enterococci. Am J Infect Control. 2013;41:668–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee BY, Schreiber B, Wateska AR, et al. The Benin experience: how computational modeling can assist major vaccine policy changes in low and middle income countries. Vaccine. 2015;33:2858–2861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee BY, Assi TM, Rookkapan K, et al. Replacing the measles ten-dose vaccine presentation with the single-dose presentation in Thailand. Vaccine. 2011;29:3811–3817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giskes K, van Lenthe F, Avendano-Pabon M, et al. A systematic review of environmental factors and obesogenic dietary intakes among adults: are we getting closer to understanding obesogenic environments? Obes Rev. 2011;12(5):e95–e106. [DOI] [PubMed] [Google Scholar]
- 46.Chou S-Y, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23:565–587. [DOI] [PubMed] [Google Scholar]
- 47.Brown ST, Tai JHY, Bailey RR, et al. Would school closure for the 2009 H1N1 influenza epidemic have been worth the cost? A computational simulation of Pennsylvania BMC Public Health. 2011;11:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee BY, Bailey RR, Wiringa AE, et al. Economics of employer-sponsored workplace vaccination to prevent pandemic and seasonal influenza. Vaccine. 2010;28:5952–5959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee BY, Bailey RR, Wiringa AE, et al. Antiviral medications for pregnant women for pandemic and seasonal influenza: an economic computer model. Obstet Gynecol. 2009;114:971–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee BY, Brown ST, Bailey RR, et al. The benefits to all of ensuring equal and timely access to influenza vaccines in poor communities. Health Affairs. 2011;30:1141–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee BY, Brown ST, Cooley P, et al. Vaccination deep into a pandemic wave: potential mechanisms for a “third wave” and the impact of vaccination. Am J Prevent Med. 2010;39:e21–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee BY, Brown ST, Cooley P, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. 2010;16:252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee BY, Brown ST, Cooley PC, et al. A computer simulation of employee vaccination to mitigate an influenza epidemic. Am J Prevent Med. 2010;38:247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harrison A, Fiedler E. Introduction: psychology and the U.S. Space Program. In: Vakoch D, ed. Psychology of Space Exploration. Washington, DC: National Aeronautics and Space Administration Office of Communications History Program Office; 2011:1–16. [Google Scholar]
- 55.Borgatti SP, Mehra A, Brass DJ, et al. Network analysis in the social sciences. Science. 2009;323:892–895. [DOI] [PubMed] [Google Scholar]
- 56.Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101:2170–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de la Haye K, Robins G, Mohr P, et al. How physical activity shapes, and is shaped by, adolescent friendships. Soc Sci Med. 2011;73:719–728. [DOI] [PubMed] [Google Scholar]
- 58.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New Engl J Med. 2007;357:370–379. [DOI] [PubMed] [Google Scholar]
- 59.Hammond RA, Ornstein JT, Fellows LK, et al. A model of food reward learning with dynamic reward exposure. Front Comput Neurosc. 2011;6:82–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang J, Tong L, Lamberson PJ, et al. Leveraging social influence to address overweight and obesity using agent-based models: the role of adolescent social networks. Soc Sci Med. 2015;125:203–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fallah-Fini S, Rahmandad H, Huang TT-K, et al. Modeling US adult obesity trends: a system dynamics model for estimating energy imbalance gap. Am J Public Health. 2014;104:1230–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Orr MG, Kaplan GA, Galea S. Neighbourhood food, physical activity, and educational environments and black/white disparities in obesity: a complex systems simulation analysis. J Epidemiol Commun Health. 2016;70:862–867. [DOI] [PubMed] [Google Scholar]
- 63.Auchincloss AH, Riolo RL, Brown DG, et al. An agent-based model of income inequalities in diet in the context of residential segregation. Am J Prevent Med. 2011;40:303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li Y, Zhang D, Pagan JA. Social norms and the consumption of fruits and vegetables across New York City Neighborhoods. J Urban Health. 2016;93:244–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kumar S, Nigmatullin A. A system dynamics analysis of food supply chains - a case study with non-perishable products. Simulation Modelling Pract Theory. 2011;19:2151–2168. [Google Scholar]
- 66.Minegishi S, Thiel D. System dynamics modeling and simulation of a particular food supply chain. Simulation Practice Theory. 2000;8:321–339. [Google Scholar]
- 67.Georgiadia P, Vlachos D, Iakovou E. A system dynamics modeling framework for the strategic supply chain management of food chains. J Food Eng. 2005;70:351–364. [Google Scholar]
- 68.Hawkes C, Smith TG, Jewell J, et al. Smart food policies for obesity prevention. Lancet. 2015;385:2410–2421. [DOI] [PubMed] [Google Scholar]
- 69.Maryland Department of Health and Mental Hygiene; Family Health Administration; Center for Preventative Services. Behavior Risk Factor Surveillance System, Maryland BRFSS State of the State Report: 2005 Survey Results on Maryland Healthy Behaviors and Lifestyles. Maryland Department of Health and Mental Hygiene, Baltimore, Maryland; 2007. [Google Scholar]
- 70.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance–United States, 2007. MMWR Surveill Summ (Washington, DC: 2002). 2008;57:1–131. [PubMed] [Google Scholar]
- 71.Gittelsohn J, Anderson Steeves E, et al. B'More Healthy Communities for Kids: design of a multi-level intervention for obesity prevention for low-income African American children. BMC Public Health. 2014;14:942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gittelsohn J, Mui Y, Adam A, et al. Incorporating systems science principles into the development of obesity prevention interventions: priniciple, benefits, and challenges. Curr Obes Rep. 2015;4:174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59:955–959. [DOI] [PubMed] [Google Scholar]
- 74.Guo SS, Wu W, Chumlea WC, et al. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76:653–658. [DOI] [PubMed] [Google Scholar]
- 75.National Center for Health Statistics, Centers for Disease Control and Prevention. 2000. CDC Growth Charts for the United States: Methods and Development. Centers for Disease Control and Prevention, Atlanta, Georgia; 2002. [Google Scholar]