Abstract
Background:
The objective of the present study was to explore the efficacy of internet-based intervention on quality of life of patients with chronic post-surgical pain (CPSP).
Methods:
A retrospective analysis was performed on 81 patients diagnosed with CPSP after radical resection for lung cancer between January 2013 and July 2014. They were enrolled either as part of the conventional care group which included 40 cases or the internet-based pain intervention group which included 41 cases. The patients in the conventional care group were treated weekly in the outpatient clinic, while patients in internet-based group were treated via smartphone or the internet. The 36-Item Short Form Health Survey (SF-36) was utilized to assess the quality of life of patients who were suffering from CPSP, 1 month and 3 months after therapy.
Results:
The patients in the internet-based pain intervention group demonstrated similar health-related qualities of life and overall satisfaction rates compared with the conventional care group (P>0.05).
Conclusion:
Internet-based pain management is a suitable option to improve the quality of life of patients with CPSP after radical resection for lung cancer.
Keywords: Internet-based pain intervention, Chronic post-surgical pain, Quality of life
Introduction
Modern medical philosophy is targeted at the overall diagnosis and treatment of patients in all areas including physiological, psychological and societal (1). This includes building favorable physician-patient relationships to help patients rehabilitating normal social function. Postoperative pain greatly affects quality of life. Some patients suffer continued widespread pain following thoracotomy. This is known as Chronic Post-surgical pain (CPSP) if the pain lasts for over 3 months (2). Standard clinical treatment and pain intervention calls for several resources, and common analgesic drugs are far from satisfactory. Remote treatment via internet was reported as effective for CPSP (3).
From January 2013, continuous follow-up cooperation systems were established on smart phones and internet, with the caregivers or the patients. The Emergency Department of our hospital carried out remote treatment guidance and pain intervention for those who suffered from post-thoracotomy pain. Our results imply that effective remote pain intervention helps to improve the quality of life of patients with CPSP.
Methods
Patients
Patients who underwent radical resection for lung cancer between January 2013 and July 2014 were retrospectively analyzed. The inclusion criteria included definitive pathological diagnosis, no postoperative complications (chylothorax, thrombosis or pulmonary atelectasis). The exclusion criteria included history of other surgery or trauma, herpes zoster, intervertebral disc disease or chest or back pain history, tumor recurrence or metastasis, refusal to follow-up at outpatient clinic or via the internet, or lack of complete data. Eighty-one patients with CPSP who underwent radical resection for lung cancer under general anesthesia were followed up for 3 months. Patient-controlled analgesia pumps (1μg/ml, Fentanyl) were used for postoperative pain management for 48 h.
Subsequently, according to visual analogue score (VAS) of pain, pethidine was injected intramuscularly (25–50 mg per patient). Based on method of postoperative pain management, patients were divided into two groups: 40 cases in the control group who received conventional treatment, and 41 cases in the observation group who received remote symptom-triggered pain intervention. General patient characteristics were shown in Table 1. Informed consent was obtained from each patient and this study was approved by local Ethics Committee.
Table 1:
General characteristics of patients
| Variable | Conventional treatment group (n=40) | Remote pain intervention group (n=41) | P |
|---|---|---|---|
| Age (yr) | 61.7±9.1 | 60.8±7.5 | 0.096 |
| Gender | 0.948 | ||
| Male | 29 | 31 | |
| Female | 11 | 10 | |
| BMI | 25.1±1.9 | 24.9±1.8 | 0.061 |
| Surgical procedure | |||
| Thoracotomy | 12 | 15 | 0.694 |
| Thoracoscopic surgery | 28 | 26 | |
| Incision length (cm) | 14.9±10.8 | 15.1±11.9 | 0.179 |
| Operative time (min) | 125.6±30.2 | 127.3±31.7 | 0.056 |
| Duration of thoracic drainage tubes(d) | 3.9±2.7 | 3.7±2.1 | 0.611 |
| Postoperative hospital stay(d) | 11.7±2.6 | 11.5±2.6 | 0.185 |
| Patient satisfaction rate | 72.5% (29/40) | 90.2% (37/41) | 0.045 |
Treatment procedures
Conventional treatment group: patients were followed up in the emergency department or outpatient clinic on a weekly basis, who received treatment adjustments and psychological interventions. Their daily diet, frequency of deep breathing and coughing and psychological states were assessed, and the indicators associated with quality of life, such as pain, fatigue, depression, anxiety and insomnia were monitored as well. Patients were specifically educated for lifestyle adjustment, physiotherapy, rehabilitation and avoiding drug abuse or misuse. Targeted instructions were obtained from psychologists, so that the favorable physician-patient relationships were maintained and negative psychological reactions were averted. As for patients with poor self-control, the hospital-family-society cooperation system were applied to deliver guidelines of physiological and life support. Through communication and instruction, patients gradually restored their normal societal function.
Remote pain intervention group: Patients received the same therapy as the control group without going to the hospital. We maintained continued relationships with patients via telephone and the internet. In this fashion, remote psychological support and pain related education were conducted and patient compliance was improved. Patients involved in the study understood detailed questionnaires without misunderstandings. Using a 36-item Short Health Survey (SF-36), general quality of life was analyzed before, 1 month and 3 month after treatment. SF-36 included physical function (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE) and mental health (MH). Each program was compared respectively after evaluation.
Statistical analysis
Data was analyzed using SPSS 19.0 software (Chicago, IL, USA). Data was expressed as mean ±standard deviation. Continuous variable data was assessed by student’s t-test or Mann-Whitney U-test among groups, while categorical variables data was assessed using chi-square test or Fisher exact test. Differences were considered as statistically significant if P<0.05.
Results
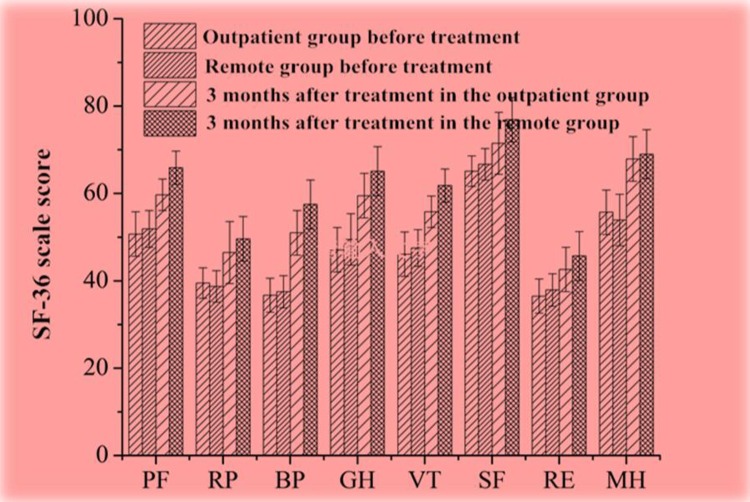
The general parameters of the 81 patients between both groups, such as gender, age, body weight index (BMI), operation procedures, incision lengths, operative time, postoperative duration of thoracic drainage tubes, and SF-36 questionnaires before treatment indicated no significant differences (P>0.05) (Table 1 and Fig. 2).
Fig. 2:
The SF-36 scores of patients with CPSP before and after treatment Comparison between groups indicated no significant differences (P>0.05)
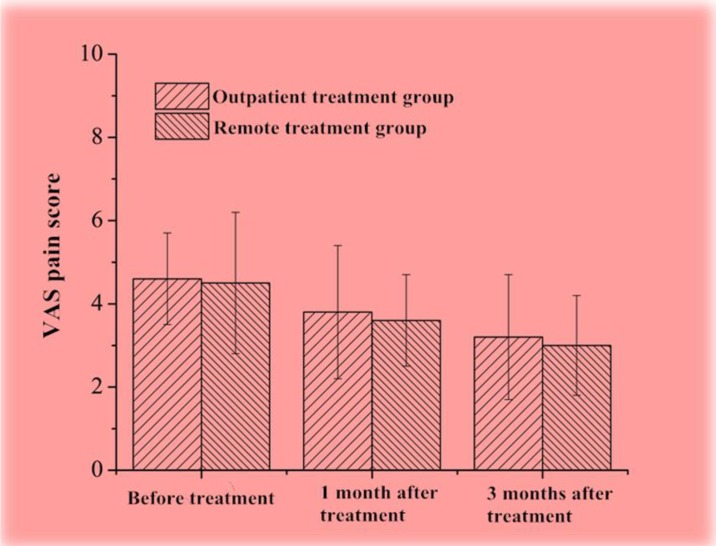
Both groups scored similarly in VAS and showed no significant differences before treatment, or one and three months after treatment (P>0.05). Three months after therapy, the overall satisfaction rate of the remote group reached 90.2%, which was significantly higher than that in the control group (72.5%, P<0.05). Furthermore, patients with CPSP in the remote therapy group scored lower in VAS and higher in SF-36 than that in the control group, but there was no significant difference (P>0.05) (Fig. 1). Patients who received remote pain control and psychological intervention maintained a higher quality of life. Notably, SF-36 score of patients with CPSP was less than 60 which indicated poor quality of life, therefore, proper therapy was truly needed for CPSP patients.
Fig. 1:
The VAS scores of patients with CPSP before and after treatment Comparison between groups indicated no significant differences (P>0.05)
Discussion
Quality of life affects physician-patient relationship as well as overall patient satisfaction. One fourth of patients suffer from CPSP after thoracotomy, and one third of them are accompanied by neuralgia, which dramatically decreases their quality of life. The risk factors, including age (< 60), gender (female) and duration of thoracic tube drainage were demonstrated (4). Neurotrosis and hyper-stimulation was induced by instrument such as thoracic drainage tubes, as injury of the intercostal nerve is the predominant mechanism of CPSP (5). Biological, physiological and societal analyses indicated that CPSP was associated with depression, psychological vulnerability and stress (6). Therefore, regular pain intervention might relieve or decrease CPSP.
From January 2013, patients with CPSP were treated remotely by telephone or the internet. According to preliminary analysis, remote pain intervention could not only help to better physician-patient relationship, but also reduce the use of medical resources. Clinical trials led by Jahn et al. showed that the self-controlled pain management of cancer patients was improved by psychological and medical direction (7). Grondin et al. proposed patient and family-centered pain management and psychological support, which improved pain management, lowered anxiety, and facilitated the use of coping strategies (8). Remote intervention is convenient for community care and saves on medical resources (9). Pain intervention by telephone or internet provided extended service for patients with CPSP (10). A clinical trial concluded that internet-based communication avoided drug abuse and misuse, and ameliorated overall satisfaction rate (11). Furthermore, remote psychological intervention could relieve CPSP, depression and anxiety. The effect of conventional and internet-based therapy was similar (12). Cognitive-behavioral therapy through the internet achieved better results than face-to-face communication (13), which supports our results.
Psychological therapies was traditionally performed face to face, while remote intervention via the internet could effectively reduce the intensity or severity of pain, and satisfaction with these treatments was generally positive (14). Internet-delivered interventions are emerging as a strategy to break the barriers for care of individuals with chronic pain, and a large trial of internet-delivered cognitive-behavioral therapy for pediatric chronic pain patients demonstrated that internet-delivered intervention produced a number of beneficial effects (15). A pilot study indicated that 16 weeks of Intensive Short-Term Dynamic Psychotherapy delivered by Skype could significantly reduce the intensity of idiopathic pain (16). However, patients with chronic pain display a relatively low acceptance of internet-based interventions, which can be substantially increased by a short instruction video about the remote intervention procedure (17).
Conclusion
Our preliminary analysis showed that remote pain intervention via telephone or internet was helpful to improve the long-term quality of life for patients with CPSP. Not only did this share the same efficacy as regular face-to-face therapy in hospital, but also it cut down the time and expenses. Remote therapy deserves wider application. A limitation of this study was the relatively small sample size. Multi-center, large-scaled and randomized controlled studies are needed to verify our conclusions.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
The authors declare that there is no conflict of interest.
References
- 1. Papathanasiou I, Sklavou M, Kourkouta L. (2013). Holistic nursing care: theories and perspectives. Am J Nurs Sci, 2( 1): 1–5. [Google Scholar]
- 2. Peng Z, Li H, Zhang C, Qian X, Feng Z, Zhu S. (2014). A retrospective study of chronic post-surgical pain following thoracic surgery: prevalence, risk factors, incidence of neuropathic component, and impact on quality of life. PLoS One, 9( 2): e90014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Trompetter HR, Bohlmeijer ET, Veehof MM, Schreurs KM. (2015). Internet-based guided self-help intervention for chronic pain based on Acceptance and Commitment Therapy: a randomized controlled trial. J Behav Med, 38( 1): 66–80. [DOI] [PubMed] [Google Scholar]
- 4. VanDenKerkhof EG, Peters ML, Bruce J. (2013). Chronic pain after surgery: time for standardization? A framework to establish core risk factor and outcome domains for epidemiological studies. Clin J Pain, 29( 1): 2–8. [DOI] [PubMed] [Google Scholar]
- 5. Wildgaard K, Ringsted TK, Ravn J, Werner MU, Kehlet H. (2013). Late sensory changes following chest drain insertion during thoracotomy. Acta Anaesthesiol Scand, 57( 6): 776–783. [DOI] [PubMed] [Google Scholar]
- 6. Hinrichs-Rocker A, Schulz K, Järvinen I, Lefering R, Simanski C, Neugebauer EA. (2009). Psychosocial predictors and correlates for chronic post-surgical pain (CPSP)-a systematic review. Eur J Pain, 2009, 13 (7): 719– 730. [DOI] [PubMed] [Google Scholar]
- 7. Jahn P, Kuss O, Schmidt H, Bauer A, Kitzmantel M, Jordan K, Krasemann S, Landenberger M. (2014). Improvement of pain-related self-management for cancer patients through a modular transitional nursing intervention: a cluster-randomized multicenter trial. Pain, 155( 4): 746–754. [DOI] [PubMed] [Google Scholar]
- 8. Grondin F, Bourgault P, Bolduc N. (2014). Intervention focused on the patient and family for better postoperative pain relief. Pain Manag Nurs, 15( 1): 76–86. [DOI] [PubMed] [Google Scholar]
- 9. Eaton LH, Gordon DB, Wyant S, Theodore BR, Meins AR, Rue T, Towle C, Tauben D, Doorenbos AZ. (2014). Development and implementation of a telehealth-enhanced intervention for pain and symptom management. Contemp Clin Trials, 38( 2): 213–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kristjánsdóttir OB, Fors EA, Eide E, Finset A, Stensrud TL, van Dulmen S, Wigers SH, Eide H. (2013). A smartphone-based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: randomized controlled trial. J Med Internet Res, 2013, 15 (1): e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Riva S, Camerini AL, Allam A, Schulz PJ. (2014). Interactive sections of an Internet-based intervention increase empowerment of chronic back pain patients: randomized controlled trial. J Med Internet Res, 16( 8): e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eccleston C, Fisher E, Craig L, Duggan GB, Rosser BA, Keogh E. (2014). Psychological therapies (Internet-delivered) for the management of chronic pain in adults. Cochrane Database Syst Rev, (2): CD010152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Boer MJ, Versteegen GJ, Vermeulen KM, Sanderman R, Struys MM. (2014). A randomized controlled trial of an Internet-based cognitive-behavioral intervention for non-specific chronic pain: an effectiveness and cost-effectiveness study. Eur J Pain, 18( 10): 1440–1451. [DOI] [PubMed] [Google Scholar]
- 14. Fisher E, Law E, Palermo TM, Eccleston C. (2015). Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents . Cochrane Database Syst Rev, (3): CD011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Palermo TM, Law EF, Fales J, Bromberg MH, Jessen-Fiddick T, Tai G. (2016). Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. Pain, 157( 1): 174–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chavooshi B, Mohammadkhani P, Dolatshahi B. (2016). A Randomized Double-Blind Controlled Trial Comparing Davanloo Intensive Short-Term Dynamic Psychotherapy as Internet-Delivered Vs Treatment as Usual for Medically Unexplained Pain: A 6-Month Pilot Study. Psychosomatics, 57( 3): 292–300. [DOI] [PubMed] [Google Scholar]
- 17. Baumeister H, Seifferth H, Lin J, Nowoczin L, Lüking M, Ebert D. (2015). Impact of an Acceptance Facilitating Intervention on Patients’ Acceptance of Internet-based Pain Interventions: A Randomized Controlled Trial. Clin J Pain, 31( 6): 528–35. [DOI] [PubMed] [Google Scholar]