Abstract
Background
Brain injuries induced by hypoxia-ischemia in neonates contribute to increased mortality and lifelong neurological dysfunction. The specific PKR inhibitor C16 has been previously demonstrated to exert a neuroprotective role in adult brain injuries. However, there is no recent study available concerning its protective role in hypoxia-ischemia-induced immature brain damage. Therefore, we investigated whether C16 protects against neonatal hypoxia-ischemia injuries in a neonatal rat model.
Material/Methods
Postnatal day 7 (P7) rats were used to establish classical hypoxia-ischemia animal models, and C16 postconditioning with 100 ug/kg was performed immediately after hypoxia. Western blot analysis was performed to quantify the phosphorylation of the PKR at 0 h, 3 h, 6 h, 12 h, 24 h, and phosphorylation of NF-κB 24h after hypoxia exposure. The TTC stain for infarction area and TUNEL stain for apoptotic cells were assayed 24 h after the brain hypoxia. Gene expression of IL-1β, IL-6, and TNF-α was performed at 3 h, 6 h, 12 h, and 24 h.
Results
The level of PKR autophosphorylation was increased dramatically, especially at 3 h (C16 group vs. HI group, P<0.01). Intraperitoneal C16 administration reduced the infarct volume and apoptosis ratio after this insult (C16 group vs. HI group<0.01), and C16 reduced proinflammatory cytokines mRNA expression, partly through inhibiting NF-κB activation (C16 group vs. HI group<0.05).
Conclusions
C16 can protect immature rats against hypoxia-ischemia-induced brain damage by modulating neuroinflammation.
MeSH Keywords: Brain Injuries; eIF-2 Kinase; Hypoxia-Ischemia, Brain; Infant, Newborn; Neuroprotective Agents
Background
Perinatal hypoxia-ischemia (HI) and subsequent brain injuries are major causes of mortality and lifelong neurological impairments in infants and children [1,2]. Despite advancements in the technology of obstetric monitoring and neonatal care, the incidence of neonatal HI is as high as 1 in 4000 live births [3]. Even when survived, long-term follow-up shows that 60% of survivors are neurologically or cognitively abnormal (e.g., lifelong cerebral palsy or epilepsy, as well as cognitive, motor, and behavioral disorders) [4]. Therefore, there is an urgent need to find efficient ways to reverse the permanent damages caused by this insult.
As previous studies showed, neuroinflammation plays a critical role during the progression of HI injuries. Proinflammatory cytokines, especially TNF-α and IL-1β, were increased significantly in plasma and cerebrospinal fluid after neonatal HI [2,5,6]. Furthermore, activated protein, secreted by activated microglia and other cells, bind to receptors on receptor-expressing cells (e.g., neurons and oligodendroglial cells), starting the death-inducing signaling complex (DISC) and triggering apoptotic and necrotic pathways [7]. While many interventions, such as induction of hypothermia and use of glutamate receptor antagonists, have been explored for potential neuroprotection against ischemia, the clinical effects have not been very significant [4]. Therefore, efficient agents to manage the uncontrolled cytokines storm and reverse the permanent damages caused by this insult are urgently needed.
The double-stranded RNA (dsRNA)-dependent protein kinase (PKR), an interferon-inducible protein kinase, is characterized as a component in regulating immune responses through autophosphorylation [8,9]. Most in vitro and in vivo studies have focused on its antiviral activity by directly reducing virus replication [10,11]. However according to Lu et al., activated PKR also promotes cytokines (IL-1β and IL-18) production through interacting directly with inflammasome components, partly depending on the NF-κB pathway [8]. Several studies have shown that PKR participates in neurodegenerative processes with neurotoxicity [12,13]. Peel and Couturier considered PKR as an early biomarker of neuronal cell death in Alzheimer disease [14, 15]. All of the information provided above suggests that using the specific pharmacological PKR inhibitor is a potential strategy against neuroinflammation.
Therefore, in the present study, we aimed to assess PKR activation and investigate whether the PKR specific inhibitor C16 exerts its neuroprotection function in a neonatal HI model.
Material and Methods
Animals and materials
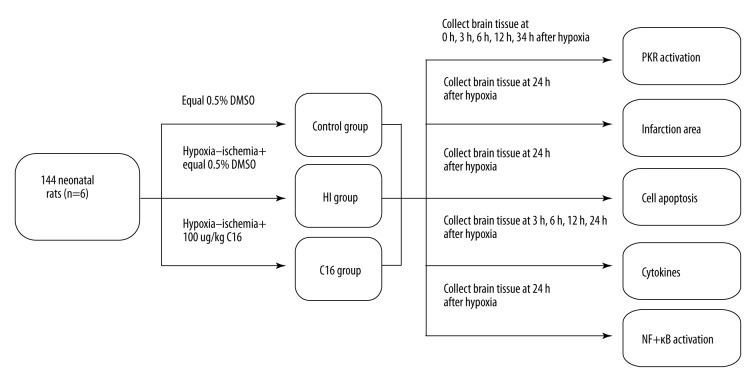
As in a previous study, maturation of the brain in a 7-day-old rat is similar to that of the human newborn brain [16]. We used male postnatal day 7 Sprague-Dawley rats (weight 12–18 g) from the Second Military Medical University to carry out this study. Rat pups were housed with their mother under a12-h light/dark cycle at 24±1°C with 40–80% humidity. All rat pups had free access to chow and water throughout the study. The experiments were approved by the Institutional Animal Care and Use Committee of Changhai hospital (Approval number CH20130723-18). Imidazole-oxindole PKR inhibitor C16 (CAS: 608512-97-6, purity >98%, molecular formula C13H8N4OS) was purchased from Sigma-Aldrich corporation and dissolved in 0.5% DMSO. The experiment work-flow is shown in Figure 1.
Figure 1.
The flow chart of the study.
Neonatal HI model establishment and drug treatment
Hypoxia-ischemia was induced as previously described, with slight modifications [17]. In the Model group (HI group), the pups were anesthetized by 1.5% sevoflurane, and then the left common carotid artery was exposed, isolated, and permanent ligated using #5 silk. After surgery, the pups were allowed to recover for 1.5 h and then they were placed in a container perfused with 8% humidified oxygen (balanced with 92% nitrogen) for 2 h to induce neonatal hypoxia-ischemia injury. C16 group pups, selected from the same litters as the model rats, received anesthesia and underwent isolation of the artery with permanent ligation. Immediately after the hypoxic exposure, the pups were injected intraperitoneally with C16. During our study, we tried several dosages of C16 (10 ug/kg, 50 ug/kg, 100 ug/kg, and 200 ug/kg). Control group pups received a neck incision and equal 0.5% DMSO i.p. without hypoxia or ischemia. Brain tissues were harvested at designated time points for analysis.
Measurement of PKR activation in the hypoxia-ischemia brain tissue
Pups in each group were decapitated after being narcotized with sevoflurane. The damaged brain tissue (left brain tissues) were obtained at different time points (0 h, 3 h, 6 h, 12 h, and 24 h) after hypoxia.
PKR activation was reflected by the level of PKR phosphorylation through Western blotting. Brain tissues from each group were collected and homogenized into lysis buffer (Thermo, USA). According to our previous study [18], after quantification, equal amounts of protein extracts were separated discontinuously onto 10% polyacrylamide gels (Life Technologies, Carlsbad, CA) and transferred to nitrocellulose membranes and then cultured with anti-phosphorylated PKR and PKR antibodies (Cell Signaling Technology, Danvers, MA) with a 1:500 dilution ratio of monoclonal antibody. Protein bands were demonstrated using an enhanced chemiluminescence (ECL) Western blot kit (Thermo USA).
The ratio of pPKR/PKR was calculated to assess the level of PKR activation.
Effects of C16 on brain infarct volume in the brain tissues induced by hypoxia and ischemia
As described previously [19], 2,3,5-triphenyltetrazolium chloride (TTC) staining was performed with minor modifications. Briefly, the brains were quickly removed 24 h after the HI model was established and frozen for 30 min after decapitation, and 2-mm intervals from the optic chiasm were cut into 5 serial coronal sections. After incubation in 1% TTC in phosphate-buffered saline (PBS) for 8 min at 37°C, the brain slices were fixed in 4% formaldehyde in PBS for 24 h. At 24 h after fixation, the brain slices were photographed with a digital camera (SONY DSC-W150, Japan). The area of each section was calculated by an image analysis system.
Effects of C16 on the counts of apoptotic cells in the cerebral cortex and hippocampus
At 24 h after the HI model was established, pups were anesthetized and the brain tissues were perfused with 4% formaldehyde in 0.1M phosphate buffer through the left heart chamber for 1 min. After that, the brain tissues were rapidly removed and fixed in 4% formaldehyde for 24 h. According to our previous study, sections (4–5 μm) were deparaffinized in xylene, rehydrated in decreasing concentrations of ethanol, and stained using the FragEL™ DNA Fragmentation Detection Kit (Merk, USA). We used IOD/area to quantify the level of apoptosis in the brain tissues.
Real-time PCR assay
Total RNA was isolated from the brain and by using TRIzol (Invitrogen, USA) according to the manufacturer’s protocol. cDNA was synthesized with SuperScript Reverse Transcriptase (Invitrogen). RNA was quantified using an ultraviolet spectrophotometer at 260 nm. PCR was performed with the iQ5 Real-Time PCR Detection System (Bio-Rad Laboratories, Veenendaal, The Netherlands) for TNF-α, IL-1β, and IL-6 using the following primers: TNF-α (Forward, 5′-AAGCCCGTAGCC CACGTCGTA-3′ and Reverse, 3′-GCCCGCAATCCAGGCCACTAC-5′), IL-1β (Forward, 5′-CCAGGATGAGGACCCAAGCA -3′ and Reverse, 3′-TCCCGACC ATTGCTGTTTCC -5′), IL-6 (Forward, 5′-CTAGGAAGAACTGGCAATATG -3′ and Reverse, 3′-AAACCATCTGGCTAGGTAAGA -5′). GAPDH (Forward, 5′-ATCGTGGGCCGCCCTAGGCA C -3′ and Reverse, 3′-ACGTACATGGCTGGGGTGTTG -5′). The amplified transcripts were quantified in comparison to a standard curve, using GAPDH as the internal control.
Western blot
NF-κB activation was assessed via Western blotting. Pups were narcotized with sevoflurane 24 h after the HI model was established. Brain tissues were collected and homogenized in lysis buffer (Thermo, USA). According to our previous study [20], after quantification, equal amounts of protein extracts were separated discontinuously onto 10% polyacrylamide gels (Life Technologies, Carlsbad, CA, USA) and transferred to nitrocellulose membranes and then cultured with anti-phosphorylated NF-κB p65 and anti- NF-κB p65 antibodies (Cell Signaling Technology, Danvers, MA) with a 1:1000 dilution ration of monoclonal antibody. Protein bands were demonstrated by enhanced chemiluminescence (ECL) Western blot kit (Thermo USA). Signals were densitometrically assessed and normalized to β-actin signals.
Statistical analysis
Data are presented as the mean ± standard deviation (mean ±SD). The differences between groups were analyzed by one-way analysis of variance (ANOVA), followed by Tukey’s multiple comparison test or unpaired Student’s t-test for comparisons of 2 groups. All data were analyzed using Prism 5.0 (GraphPad Software, USA). P<0.05 was considered statistically significant.
Results
The level of PKR phosphorylation was increased in neonatal HI rat models
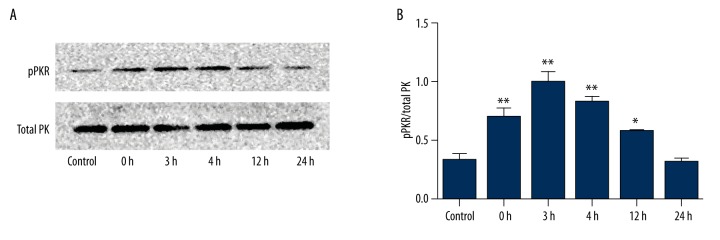
As noted, the serine and threonine protein kinase PKR can be activated by inflammatory responses, such as those induced by bacterial infection and necrosis. In our study, we took the HI brain tissue at 0 h, 3 h, 6 h, 12 h, and 24 h after model establishment and detected the activation of PKR through Western blotting (Figure 2). As expected, PKR phosphorylation was induced by hypoxia-ischemia in neonatal rat models. As the results showed, compared with the Control group (0.330±0.086), the ratio of pPKR/PKR was increased and reached the peak at 3 h (1.001±0.143) after model establishment (Control group vs. HI group 3 h, P<0.01).
Figure 2.
The level of PKR autophosphorylation in neonatal brain I induced by hypoxia-ischemia. The level of PKR autophosphorylation were detected at different time points (0 h, 3 h, 6 h, 12 h, and 24 h) after model establishment (A) Representative images of phosphorylated and total forms of PKR. (B) Ratio of pPKR/PKR calculated from the densitometric analyses of blots. * P<0.05 vs. Control group, ** P<0.01 vs. Control group.
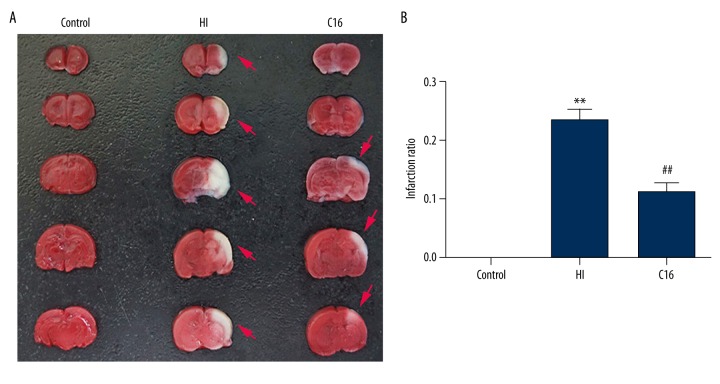
C16 administration decreased the brain infarct volume
On the basis of previous studies, we consider C16 as the specific PKR inhibitor. We examined whether it could reduce the brain infarct volume after hypoxia-ischemia induction. Surprisingly, C16 (10 ug/kg and 50 ug/kg) did not exert its protective role, as confirmed by TTC staining (data not shown). Administration of C16 at 200 ug/kg was shown to be lethal. Therefore, we chose 100 ug/kg in the following experiment. As shown in Figure 3A, the infarct range of the HI group, defined as the readily visible white region, reached the hippocampus. However, C16 administration reduced the infarct volume and limited it in the cortex. TTC staining showed that the infract ratio was increased significantly compared with the HI group (0.236±0.071), and intraperitoneal C16 injection decreased the infract ratio dramatically (0.093±0.049). This strongly indicates that PKR inhibition protects neonatal rats from hypoxia-ischemia-induced brain injuries (Control group vs. HI group, P<0.01 and C16 group vs. HI group, P<0.01).
Figure 3.
The effects of C16 administration on brain tissue loss at 24 h after hypoxia-ischemia. (A) Representative samples of TTC-stained coronal sections were obtained 24 h after hypoxia-ischemia. Notable cerebral infarction region was observed in the HI group. (B) After HI, the infarct ratio was increased dramatically, and the infarct ratio was clearly lower after intraperitoneal C16 administration. ** P<0.01 vs. Control group, ## P<0.01 vs. HI group.
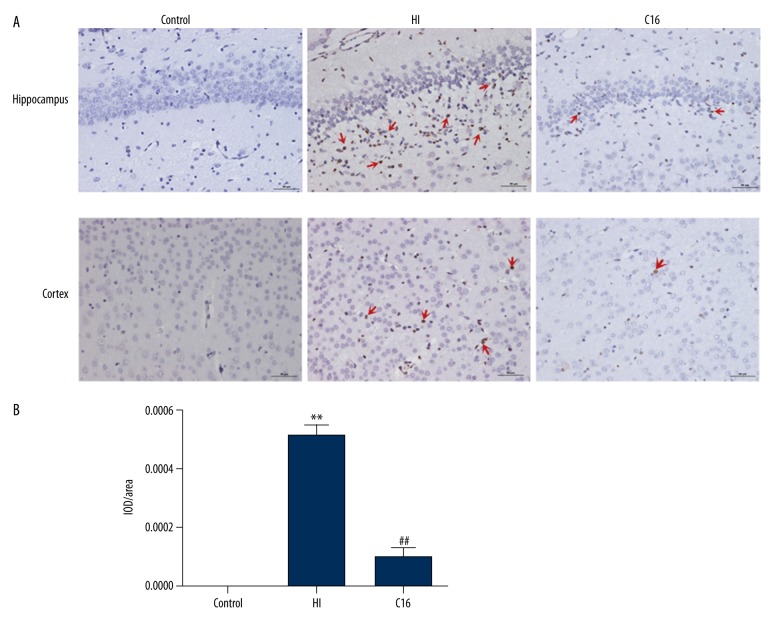
C16 treatment attenuated neuronal cell apoptosis
According to a previous study, neuron apoptosis induced by HI was associated with brain dysfunction [21]. On the basis of our previous study, we used TUNEL staining to calculate the apoptotic levels in the brain tissues. As Figure 4 shows, niger-brown staining represents apoptotic cells. Brain tissues that had HI injury demonstrated severe apoptosis, while C16 reduced the percent of neuron apoptosis, especially in the cortex and the hippocampus. According to the TUNEL images, we used IOD/area to quantify the level of apoptosis in the brain tissues. The IOD/area was markedly decreased in the C16 group (0.000101±0.000099) as compared with the HI group (0.000512±0.000121) (Control group vs. HI group P<0.01 and C16 group vs. HI group P<0.01). However, there was also a significant difference between the Control group and the C16 group (C16 group vs. Control group P<0.05).
Figure 4.
The effects of C16 postconditioning on apoptosis of brain tissues at 24 h after hypoxia-ischemia. (A) Representative samples of TUNEL-stained coronal sections. TUNEL-positive cells showed niger-brown staining (arrow). (B) The IOD/area in the HI group was significantly elevated, while the C16 group showed a dramatic downregulation. ** P<0.01 vs. Control group, ## P<0.01 vs. HI group.
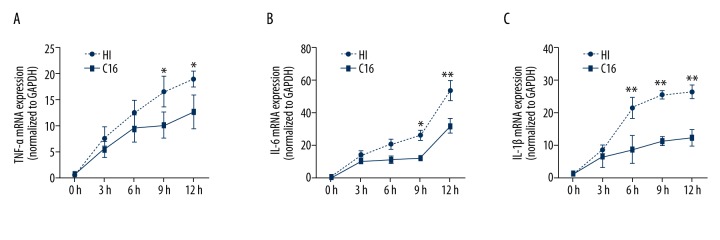
C16 intraperitoneal injection alleviated brain cytokines mRNA expression
PKR is involved in the regulation of the expression of a wide range of cytokines, as PKR inhibition greatly decreased IL-1β, IL-6, and TNF-α production in various models [8,12,22]. Unbalanced neuroinflammation is a major mechanism in cerebrum hypoxia-ischemia injury. In our study, we investigated if the specific PKR inhibitor C16 could alleviate cytokines secretion. The result showed that gene expression of cytokines (TNF-α, IL-6, and IL-1β) was clearly increased in the HI group, and each of them peaked at 24 h (C16 group vs. HI group P<0.05), 24 h (C16 group vs. HI group, P<0.01), and 6 h (C16 group vs. HI group, P<0.01), which was obviously reduced by C16 (Figure 5).
Figure 5.
C16 administration modulated the cytokines mRNA expression. Cytokines mRNA were detected at different time points (0 h, 3 h, 6 h, 12 h, and 24 h) after model establishment. (A) TNF-α, (B) IL-1β, (C) IL-6. Inflammatory cytokines mRNA expression levels increased gradually from 0 h to 24 h, while C16 postconditioning restrained the cytokines mRNA expression. * P<0.05 vs. C16 group. ** P<0.01 vs. C16 group.
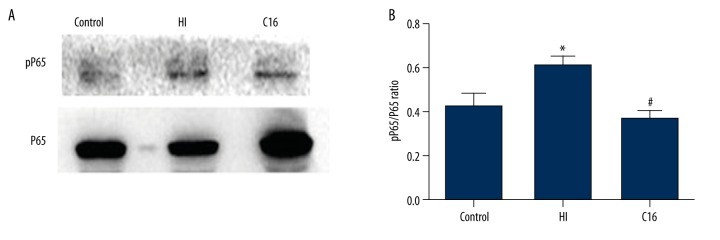
C16 administration decreases phosphorylation of NF-κB in HI brain tissues
NF-κB activation is one of main pathways in HI brain injury pathologies [21]. Interestingly, several studies found that PKR can induce phosphorylation of NF-κB, accompanied with inflammation and apoptosis [23,24]. In our present study, it was clear that C16 dramatically suppressed the phosphorylation of p65 (C16 group 0.373±0.072) compared with the HI group (HI group 0.611±0.082), showing that C16 inhibited inflammatory responses through suppressing NF-κB activation (C16 group vs. HI group P<0.01) (Figure 6).
Figure 6.
The effects of C16 on NF-κB activity at 24 h after hypoxia-ischemia. (A) Representative images of pP65 and P65. (B) The phosphorylation levels of P65 were increased in the HI group, while in the C16 group the expression levels of pP65 were restrained. * P<0.05 vs. Control group, # P<0.05 vs. HI group.
Discussion
In healthy humans, infancy is a crucial time for brain development, as axons undergo rapid myelination during the first year of life. Axons then reach adult levels of myelination at approximately 18 months of age [25]. However, this may be perturbed by perinatal hypoxia-ischemia (HI). This perturbation can lead to lifelong brain injury or death. It is therefore quite crucial to better understand the perinatal hypoxia-ischemia (HI) mechanisms and develop an efficient treatment. In our present study, we are the first to report that PKR autophosphorylation play an important role in the HI-induced brain damages, and C16, a PKR-specific inhibitor, exerts a protective role during the development of HI injuries through suppressing inflammatory responses by modulating NF-κB activation. It could be a new target for a cure.
PKR is a ubiquitously expressed serine/threonine protein kinase, and it plays a role in many kinds of disease (e.g., diabetes and cancer) [9,26]. Interestingly, under the stimulation of Aβ peptide, which is secreted during Alzheimer disease, PKR was activated and subsequently triggered activated cells death by apoptosis [14,15]. Therefore, explored whether PKR contributes to the hypoxia-ischemia brain injuries in neonatal rats. As expected, we found that the level of PKR autophosphorylation increased dramatically after left common carotid artery ligation. The phosphorylation level was further elevated after rats were subjected to hypoxia-ischemia and peaked at 3 h after insult (Figure 2). These exciting results remind us that PKR is involved in the evolution of brain injuries. On the basis of the current understanding of PKR, we proposed to use C16 to investigate the neuroprotective effects in a neonatal hypoxia-ischemia rat model.
Infarct volume in the brains, which was detected by TTC staining, have been verified to have a high degree of correlation with the severity of injuries [27,28]. In our study, the notable white region in the HI group was larger than in the Control group, while C16 reduced the infarct area at 24 h (Figure 3). These beneficial phenomena confirmed that C16 administration improved the pathological change caused by HI injuries, and it was in accordance with our initial hypothesis. In addition, hypoxia-ischemia induced neuronal cell apoptosis, especially in the hippocampus, and intraperitoneal C16 injection reduced the ratio of TUNEL-positive cells in the images of the hippocampus and cortex. It is obvious that the specific PKR inhibitor C16 exerts a neuroprotective effect in a neonatal hypoxia-ischemia rat model.
Neuroinflammation is an important pathogenesis in hypoxia-ischemia brain injury [29], and Tronel et al. proved that C16 exerts a neuroprotective function in an acute excitotoxic rat model by preventing apoptosis and IL-1β production [30]. We examined the variation of proinflammatory cytokines at different time points. As Figure 5 shows, cytokines mRNA in brain tissues were upregulated after hypoxia-ischemia, including TNF-α, IL-1β, and IL-6, and C16 administration reduced cytokines mRNA expression. These findings are consistent with the inflammation-related property of PKR mentioned previously.
According to Zamanian and Gil [23,24], PKR modulates the inflammation and immune responses through several signaling pathways. The NF-κB pathway was reported to have a close association with PKR activation [31]. As speculated, intraperitoneal C16 administration restrained NF-κB activation. This may partly explain the cytokines production induced by hypoxia-ischemia.
In the present study, the main difficulty was the choice of dosage of C16. We tried several dosages as described by Sabrina [32], but C16 (10 ug/kg and 50 ug/kg) did not exert its protective role, as confirmed by TTC staining (data not shown). Administration of C16 at 200 ug/kg was shown to be lethal, which was different from Sabrina’s study. This may be because our rats were exposed to hypoxia-ischemia insult, while rats in their study did not have any insult. Our dosage of C16 was also different from that in Tronel’s study because we used totally different models, and we used neonatal rats while they used adult rats [30].
Conclusions
Our findings indicate that the specific PKR inhibitor C16 exerts anti- neuroinflammation and anti-apoptosis properties in neonatal HI brain injury through regulating activation of the PKR/NF-κB pathway, which may suggest a new target for reversing or alleviating the damage caused by hypoxia-ischemia insult.
Footnotes
Conflict of interests
The authors declare that there are no conflicts of interests regarding the publication of this paper.
Source of support: This work was supported by Grants 81371219 from the National Natural Science Foundation of China and 201440440 from the Shanghai Health Bureau Scientific Research Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
References
- 1.Vannucci RC, Connor JR, Mauger DT, et al. Rat model of perinatal hypoxic-ischemic brain damage. J Neurosci Res. 1999;55(2):158–63. doi: 10.1002/(SICI)1097-4547(19990115)55:2<158::AID-JNR3>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 2.Ferriero DM. Neonatal brain injury. N Engl J Med. 2004;351(19):1985–95. doi: 10.1056/NEJMra041996. [DOI] [PubMed] [Google Scholar]
- 3.Nelson KB, Lynch JK. Stroke in newborn infants. Lancet Neurol. 2004;3(3):150–58. doi: 10.1016/S1474-4422(04)00679-9. [DOI] [PubMed] [Google Scholar]
- 4.Zhao P, Zuo Z. Isoflurane preconditioning induces neuroprotection that is inducible nitric oxide synthase-dependent in neonatal rats. Anesthesiology. 2004;101(3):695–703. doi: 10.1097/00000542-200409000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Payton KS, Sheldon RA, Mack DW, et al. Antioxidant status alters levels of Fas-associated death domain-like IL-1β-converting enzyme inhibitory protein following neonatal hypoxia-ischemia. Dev Neurosci. 2007;29(4–5):403–11. doi: 10.1159/000105481. [DOI] [PubMed] [Google Scholar]
- 6.Yuan X, Ghosh N, McFadden B, et al. Hypothermia modulates cytokine responses after neonatal rat hypoxic-ischemic injury and reduces brain damage. ASN Neuro. 2014;6(6) doi: 10.1177/1759091414558418. pii: 1759091414558418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thornton C, Rousset CI, Kichev A, et al. Molecular mechanisms of neonatal brain injury. Neurol Res Int. 2012;2012:506320. doi: 10.1155/2012/506320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu B, Nakamura T, Inouye K, et al. Novel role of PKR in inflammasome activation and HMGB1 release. Nature. 2012;488(7413):670–74. doi: 10.1038/nature11290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakamura T, Furuhashi M, Li P, et al. Double-stranded RNA-dependent protein kinase links pathogen sensing with stress and metabolic homeostasis. Cell. 2010;140(3):338–48. doi: 10.1016/j.cell.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia MA, Gil J, Ventoso I, et al. Impact of protein kinase PKR in cell biology: From antiviral to antiproliferative action. Microbiol Mol Biol Rev. 2006;70(4):1032–60. doi: 10.1128/MMBR.00027-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang R, Tang D. PKR-dependent inflammatory signals. Sci Signal. 2012;5(247):pe47. doi: 10.1126/scisignal.2003511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Couturier J, Paccalin M, Lafay-Chebassier C, et al. Pharmacological inhibition of PKR in APPswePS1dE9 mice transiently prevents inflammation at 12 months of age but increases Abeta42 levels in the late stages of the Alzheimer’s disease. Curr Alzheimer Res. 2012;9(3):344–60. doi: 10.2174/156720512800107582. [DOI] [PubMed] [Google Scholar]
- 13.Page G, Rioux Bilan A, Ingrand S, et al. Activated double-stranded RNA-dependent protein kinase and neuronal death in models of Alzheimer’s disease. Neuroscience. 2006;139(4):1343–54. doi: 10.1016/j.neuroscience.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 14.Peel AL. PKR activation in neurodegenerative disease. J Neuropathol Exp Neurol. 2004;63(2):97–105. doi: 10.1093/jnen/63.2.97. [DOI] [PubMed] [Google Scholar]
- 15.Couturier J, Paccalin M, Morel M, et al. Prevention of the beta-amyloid peptide-induced inflammatory process by inhibition of double-stranded RNA-dependent protein kinase in primary murine mixed co-cultures. J Neuroinflammation. 2011;8:72. doi: 10.1186/1742-2094-8-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hagberg H, Bona E, Gilland E, Puka-Sundvall M. Hypoxia-ischaemia model in the 7-day-old rat: Possibilities and shortcomings. Acta Paediatr Suppl. 1997;422:85–88. doi: 10.1111/j.1651-2227.1997.tb18353.x. [DOI] [PubMed] [Google Scholar]
- 17.Ashwal S, Tone B, Tian HR, et al. Core and penumbral nitric oxide synthase activity during cerebral ischemia and reperfusion in the rat pup. Pediatr Res. 1999;46(4):390–400. doi: 10.1203/00006450-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Bao S, Zou Y, Wang B, et al. Ginsenoside Rg1 improves lipopolysaccharide-induced acute lung injury by inhibiting inflammatory responses and modulating infiltration of M2 macrophages. Int Immunopharmacol. 2015;28(1):429–34. doi: 10.1016/j.intimp.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 19.Cai J, Kang Z, Liu K, et al. Neuroprotective effects of hydrogen saline in neonatal hypoxia-ischemia rat model. Brain Res. 2009;1256:129–37. doi: 10.1016/j.brainres.2008.11.048. [DOI] [PubMed] [Google Scholar]
- 20.Cao L, Zou Y, Zhu J, et al. Ginsenoside Rg1 attenuates concanavalin A-induced hepatitis in mice through inhibition of cytokine secretion and lymphocyte infiltration. Mol Cell Biochem. 2013;380(1–2):203–10. doi: 10.1007/s11010-013-1674-y. [DOI] [PubMed] [Google Scholar]
- 21.Askalan R, Gabarin N, Armstrong EA, et al. Mechanisms of neurodegeneration after severe hypoxic-ischemic injury in the neonatal rat brain. Brain Res. 2015;1629:94–103. doi: 10.1016/j.brainres.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 22.Faria MS, Calegari-Silva TC, de Carvalho Vivarini A, et al. Role of protein kinase R in the killing of Leishmania major by macrophages in response to neutrophil elastase and TLR4 via TNFalpha and IFNbeta. FASEB J. 2014;28(7):3050–63. doi: 10.1096/fj.13-245126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zamanian-Daryoush M, Mogensen TH, DiDonato JA, Williams BR. NF-kappaB activation by double-stranded-RNA-activated protein kinase (PKR) is mediated through NF-kappaB-inducing kinase and IkappaB kinase. Mol Cell Biol. 2000;20(4):1278–90. doi: 10.1128/mcb.20.4.1278-1290.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gil J, Esteban M. Induction of apoptosis by the dsRNA-dependent protein kinase (PKR): Mechanism of action. Apoptosis. 2000;5(2):107–14. doi: 10.1023/a:1009664109241. [DOI] [PubMed] [Google Scholar]
- 25.Zhao H, Yin Z, Li K, et al. Mechanical characterization of immature porcine brainstem in tension at dynamic strain rates. Med Sci Monit Basic Res. 2016;22:6–13. doi: 10.12659/MSMBR.896368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marchal JA, Lopez GJ, Peran M, et al. The impact of PKR activation: From neurodegeneration to cancer. FASEB J. 2014;28(5):1965–74. doi: 10.1096/fj.13-248294. [DOI] [PubMed] [Google Scholar]
- 27.Li X, Zhang J, Zhu X, et al. Effects of progesterone on hippocampal ultrastructure and expression of inflammatory mediators in neonatal rats with hypoxic-ischemic brain injury. Exp Ther Med. 2014;7(5):1311–16. doi: 10.3892/etm.2014.1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X, Song L, Cheng X, et al. Carnosine pretreatment protects against hypoxia-ischemia brain damage in the neonatal rat model. Eur J Pharmacol. 2011;667(1–3):202–7. doi: 10.1016/j.ejphar.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Carty ML, Wixey JA, Reinebrant HE, et al. Ibuprofen inhibits neuroinflammation and attenuates white matter damage following hypoxia-ischemia in the immature rodent brain. Brain Res. 2011;1402:9–19. doi: 10.1016/j.brainres.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Tronel C, Page G, Bodard S, et al. The specific PKR inhibitor C16 prevents apoptosis and IL-1b production in an acute excitotoxic rat model with a neuroinflammatory component. Neurochem Int. 2014;(64):73–83. doi: 10.1016/j.neuint.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 31.Kumar A, Haque J, Lacoste J, et al. Double-stranded RNA-dependent protein kinase activates transcription factor NF-kappa B by phosphorylating I kappa B. Proc Natl Acad Sci USA. 1994;91(14):6288–92. doi: 10.1073/pnas.91.14.6288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ingrand S, Barrier L, Lafay-Chebassier C, et al. The oxindole/imidazole derivative C16 reduces in vivo brain PKR activation. FEBS Lett. 2007;581(23):4473–78. doi: 10.1016/j.febslet.2007.08.022. [DOI] [PubMed] [Google Scholar]