Abstract
Background: The Morel-Lavallee lesion (MLL) is a closed internal degloving injury that results from shearing of the skin and subcutaneous tissue from the underlying fascia. Disruption of the perforating blood vessels and lymphatics results in a lesion filled with serosanguinous fluid and necrotized fat. MLLs are most commonly described in association with pelvic and lower extremity trauma, and there are limited reports of these lesions in other locations. Methods: This case report describes a 58-year-old male referred from his primary care physician with a soft tissue mass in the upper arm. Careful history discovered prior trauma with extensive bruising and MRI revealed a large encapsulated mass consistent with MLL. Results: An open debridement with excision of pseudocapsule was performed. Meticulous closure over a drain was performed and the patient healed without complication or recurrence. Intra-operative cultures were negative and pathology was consistent with MLL. Conclusion: MLL should always be considered in the setting of previous trauma regardless the location. In the chronic setting an open approach with excision of pseudocapsule can have an acceptable result.
Keywords: Morel, Lavallee, internal degloving, soft tissue mass, cyst
Introduction
The French physician Maurice Morel-Lavallee first described posttraumatic fluid collections about the hip in 1863.5 Letournel and Judet subsequently coined the term Morel-Lavallee lesion (MLL) in their classic text on acetabular fractures.4 These injuries are caused by shearing of the subcutaneous tissues from the underlying muscular fascia resulting in the accumulation of necrotic fat and blood. The clinical picture of the lesion depends on the contents and time since trauma. MLL should be suspected when a fluctuant area of skin is found in an area that was previously exposed to trauma. Examination demonstrates soft tissue swelling, contour deformity, bruising, skin hypermobility, and decreased skin sensation. Initially it can be difficult to distinguish an MLL from soft tissue contusion, and the diagnosis is missed one-third of the time.3 In chronic injuries, the skin changes may have resolved, resulting in a more benign presentation.
In pelvic trauma, when the lesion is overlooked and not treated, bacterial colonization can occur resulting in a relative risk of surgical site infection that is eight times higher than with those without a lesion.3 Early diagnosis is critical to prevent infection,7 and less invasive treatment protocols may be effective in the acute period prior to pseudocapsule formation.1 Vanhegan et al performed a review of the literature in PubMed using the words “Morel Lavallee” and reported the details of 204 lesions in 195 patients.9 The most common locations were the hip, thigh, pelvis, and knee. Less common locations include the gluteal region, lumbosacral spine, abdomen, calf, and head. No upper extremity cases were reported.9 A more recent case series from the Mayo Clinic describes their experience with trauma patients presenting with soft tissue fluid collections consistent with MLLs. They report 87 cases in total, with 2 identified in the shoulder and 2 in the elbow.6 The details of these upper extremity cases were not presented, and it is unknown whether the same infection risk exists with MLLs of the upper extremity. We describe a 58-year-old male with an MLL in the upper extremity following a rollover automobile accident with his arm trapped out the window.
Case Report
A 58-year-old male presented to an outside trauma hospital after a rollover motor vehicle accident where his left arm was hanging out of the window. Extensive soft tissue bruising was seen in the acute period (Figure 1) but an MLL was not identified. He sustained an ipsilataral medial epicondyle fracture and index finger metacarpal fracture. Both were managed with open reduction and internal fixation. Neither surgical approach involved the area of soft tissue compromise. Ten months after his injury, he returned to his primary care doctor complaining of a large mass in the posterior proximal arm. The mass was minimally painful but not associated with any dysfunction. It was, however, cosmetically unpleasing. There were no systemic symptoms. The patient was referred to the hand surgery service for further evaluation and treatment.
Figure 1.

Patient’s photograph from home demonstrating extensive bruising of the posterior arm.
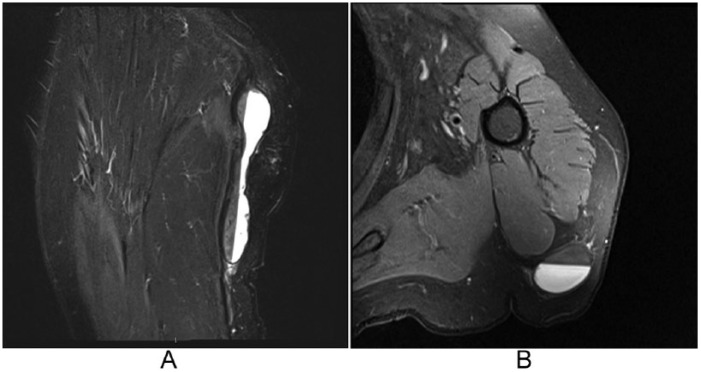
On examination, there was a fluctuant, mobile, nontender subcutaneous mass 3 cm in width by 11 cm in length without overlying skin changes. Ultrasound revealed a complex subcutaneous fluid collection within a thickened nodular capsule. Magnetic resonance imaging (MRI; Figure 2) further characterized the mass as a well-circumscribed, peripherally enhancing, suprafascial mass, with a well-delineated fat/fluid level. Additional questioning in our clinic revealed the history of trauma. Based on the history, examination, and radiographic findings, there was a high suspicion for an MLL.
Figure 2.
STIR sagittal (A) and T2 weighted axial (B) magnetic resonance imaging demonstrating a prominent fluid-fluid level and distinct low-signal-intensity capsule.
Note. STIR = short tau inversion recovery.
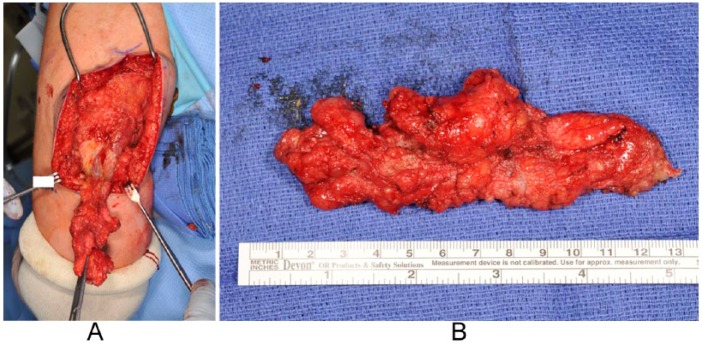
Surgical management was undertaken with a direct posterior approach. Sharp dissection was taken down until the pseudocapsule was identified. The pseudocapsule was dissected off the underlying fascia and excised en bloc (Figure 3). During excision, the pseudocapsule was violated and the mass was found to be filled with a thick serous fluid mixed with necrotic debris. A drain was placed exiting the superior aspect of the wound and the dead space and skin were closed meticulously with absorbable sutures in a layered fashion. A compressive dressing was then applied from the wrist up.
Figure 3.
(A) The pseudocapsule was dissected off the underlying fascia en bloc. (B) The final specimen.
Intraoperative cultures did not have any growth at final follow-up. The pathologic evaluation demonstrated fibroadipose tissue with a central cavity filled with a foreign body giant cell reaction and necrotic debris. The drain was removed 72 hours postoperatively. Wound healing was uncomplicated and no fluid re-accumulation was seen at 6-month follow-up.
Discussion
This case highlights a previously poorly described location for an MLL. Although the location was unique, and the presentation was late, the early features were characteristic. Review of the history revealed a high-energy motor vehicle crash, and there was significant early bruising as evidenced in Figure 1. His chronic examination was characteristic, and like so many lower extremity MLLs, the diagnosis was initially missed. Suzuki et al highlighted the importance of early identification of lesions when associated with acetabular fractures.7 Due to this, they recommend open or percutaneous treatment of the lesion and to avoid a direct approach through the affected area if fracture fixation is indicated. In this case, there was no underlying bony injury that required surgery, and this may have prevented the significant morbidity that is seen when operating through these lesions in other parts of the body.
There is a general consensus in the literature that the treatment protocol should be based on the time from injury until presentation. In the acute period (<1 month), compression, aspiration, or incision and drain placement can be considered. The location of the lesion may also play a role because it determines the ease of applying effective compression. Dawre et al proposed a treatment algorithm based on the acuity of the lesion.1 For acute lesions without an associated injury requiring surgery, treatment options include compression dressing with or without sclerotherapy. If unsuccessful, percutaneous drainage is attempted. If there is recurrence, open debridement is then indicated. For chronic lesions, percutaneous drainage with sclerotherapy is first attempted. Failure leads to open drainage with secondary closure.
A recent study from the Mayo Clinic found that a high-energy mechanism and high-volume fluid collection were associated with recurrence.6 Interestingly, chronicity was not associated with recurrence rates. They therefore proposed a protocol in which they initially perform an aspiration of all lesions. If the aspirate is less than 50 cc, they apply a compressive dressing and observe. If it is greater than 50 cc, surgical excision with closure over a drain is performed. They highlighted some of the challenges to this approach. In the acute period, there is the tendency for necrotic fat and debris or organizing hematoma to prevent aspiration. In the chronic phase, the formation of a pseudocapsule may prevent the obliteration of the cavity.
Tseng and Tornetta describe their experience with early percutaneous management of MLLs associated with pelvic and acetabular fractures.8 Their technique involves making 2 small incisions at opposing ends of the lesion, draining the hematoma, performing brush debridement through these incisions, irrigating the necrotic debris with pulse lavage, and maintaining a drain until output is less than 30 cc in a 24-hour period.
Hak et al favor an aggressive surgical approach with an incision centered over the lesion, serial debridement, and open packing with delayed primary closure. This approach is aimed to decrease the unacceptably high infection rates they found in their experience with pelvic and acetabular fractures.2
In the currently discussed case, we chose operative management because it was a chronic lesion with a well-established pseudocapsule. A meticulous layered closure over a drain was performed, and the patient has healed without recurrence at 6-month follow-up. If identified in the acute period, a less invasive approach could have been used and a shorter treatment course would have been likely. It is important to be aware that although uncommon, MLLs can present in any location, and in some cases, a missed diagnosis can have significant consequences.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients included in the study.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Dawre S, Gupta S, Gupta AK. The Morel-Lavallee lesion: a review and a proposed algorithmic approach. Eur J Plast Surg. 2012;35:489-494. [Google Scholar]
- 2. Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallee lesion. J Trauma. 1997;42(6):1046-1051. [DOI] [PubMed] [Google Scholar]
- 3. Hudson DA, Knottenbelt JD, Krige JE. Closed degloving injuries: results following conservative surgery. Plast Reconstr Surg. 1992;89(5):853-855. [DOI] [PubMed] [Google Scholar]
- 4. Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. Berlin, Germany: Springer; 1993. [Google Scholar]
- 5. Morel-Lavallee. Decollements traumatiques de la peau et des couches sous jacentes. Arch Gen Med. 1863;1:20-38, 172,-200, 300-332. [Google Scholar]
- 6. Nickerson TP, Zielinski MD, Jenkins DH, Schiller HJ. The Mayo Clinic experience with Morel-Lavallee lesions: establishment of a practice management guideline. J Trauma Acute Care Surg. 2014;76(2):493-497. [DOI] [PubMed] [Google Scholar]
- 7. Suzuki T, Morgan SJ, Smith WR, Stahel PF, Gillani SA, Hak DJ. Postoperative surgical site infection following acetabular fracture fixation. Injury. 2010;41(4):396-399. [DOI] [PubMed] [Google Scholar]
- 8. Tseng S, Tornetta P., III Percutaneous management of Morel-Lavallee lesions. J Bone Jt Surg Am. 2006;88(1):92-96. [DOI] [PubMed] [Google Scholar]
- 9. Vanhegan IS, Dala-Ali B, Verhelst L, Mallucci P, Haddad FS. The Morel-Lavallee lesion as a rare differential diagnosis for recalcitrant bursitis of the knee: case report and literature review. Case Rep Orthop. 2012;2012:ID 593193. [DOI] [PMC free article] [PubMed] [Google Scholar]