Invasive candidiasis is a serious complication in the intensive care unit (ICU), with high morbidity and mortality up to 90% in patients with septic shock (1). The epidemiology of Candida infections is continuously changing, also in relation to the timing of acquisition, with increasing data on early diagnosis after ICU admission (2, 3). By a clinical point of view, early and appropriate treatment is the key for a significant reduction in mortality and, by converse, up to 70% of critically ill patients receive systemic antifungal therapy although they have no documented invasive fungal infection, suggesting an urgent need for antifungal stewardship strategies (4–11). However, several diagnostic strategies that have benn studied for early and appropriate treatment of invasive candidiasis have been studied and are hereafter briefly discussed.
In the early 1990s, Pittet et al. (9) defined the Candida Colonization Index (CI) as the daily determination as the ratio of the number of distinct body sites colonized with identical strains over the total number of body sites tested in 29 patients at high risk of Candida infection. At that time, the proposed colonization index had high positive predictive values (66–100%). However, the CI has not been validated in large multicenter trials and its validity has been suggested almost exclusively in surgical patients (7–9, 12). In the setting of intra-abdominal candidiasis (IAC), multifocal colonization may not be required to significantly affect the peritoneum from an abdominal source, especially with suture dehiscence and anastomotic leakages (13). Moreover, the CI is expensive and time consuming, and further critics are represented by the low accuracy (11), such as? The failure to substantial guide empiric treatment (14) and the evidence of a lower use of antifungals when clinicians were not provided with CI (15, 16).
The Candida Score (CS) combined in a predictive clinical the results of a prospective cohort study, where surgery, multifocal colonization, total parenteral nutrition and severe sepsis predicted invasive candidiasis, with 81% of sensitivity and 74% of specificity and a had negative predictive value (NPV) of 98% (17). The accuracy of a CS ≥3 was greater than that of a CI ≥0.5. Questions on practical use of CS were quickly appreciated: has the financial burden of the antifungal treatment increased? Is the acute change of CS more important than the score itself?
Other Authors proposed a predictive rule for the likelihood of Candida involvement, especially in peritonitis, based on four risk factors: female sex, upper gastrointestinal injury or surgery, cardiovascular failure and previous antimicrobial therapy (18). With ≥3 risk factors the prediction of invasive intrabdominal candidiasis (IAC) had a sensitivity, specificity, positive predictive value (PPV) and NPV of 84%, 50%, 67% and 72%, respectively. Ostrosky-Zeichner et al. created a clinical prediction rule to identify patients at risk of invasive candidiasis including the parameters of ICU stay ≥4 days, mechanical ventilation, central venous catheter and broad spectrum antibiotics plus an additional risk factor (19).
However, despite a progressive improvement in the accuracy of these rules and a better PPV compared to CI and CS, so far no studies validated their systematic clinical usefulness (20). CI, CS and other predictive rules have been specifically developed by using their PPV for the early identification of high-risk patients, but their NPV is definitely much more significant (21). The low level of evidence attributed by experts to the risk-based strategies in consensus guidelines may be explained by the laborious nature of the clinical use and the lack of solid clinical data (22–24).
An innovative way to diagnostic approach of these infections is by utilizing biomarkers in addition to CS, CI and predictive rules in order to guide antifungal therapy (17, 25). Although blood cultures are still considered the gold standard for diagnosis, it has been shown that they are negative in up to 50% of cases (26). Thus, non-culture diagnostic techniques based on serological biomarkers detecting fungal cell components and/or antibodies directed against these components have been investigated (26). All these diagnostic tests may diagnose candidiasis earlier than clinical or culture-based measures.
Amongst biomarkers, mannan antigen and antigen-antibodies complex showed a higher sensitivity and specificity when combined together (27). In a meta-analysis of 14 studies, seven of which were performed in non-neutropenic critically ill patients, the sensitivity and specificity of mannan and anti-mannan IgG were 58% and 93%, and 59% and 83%, respectively. Values for the combined assay were 83 and 86%, with best performances for C. albicans, C. glabrata, and C. tropicalis infection (27).
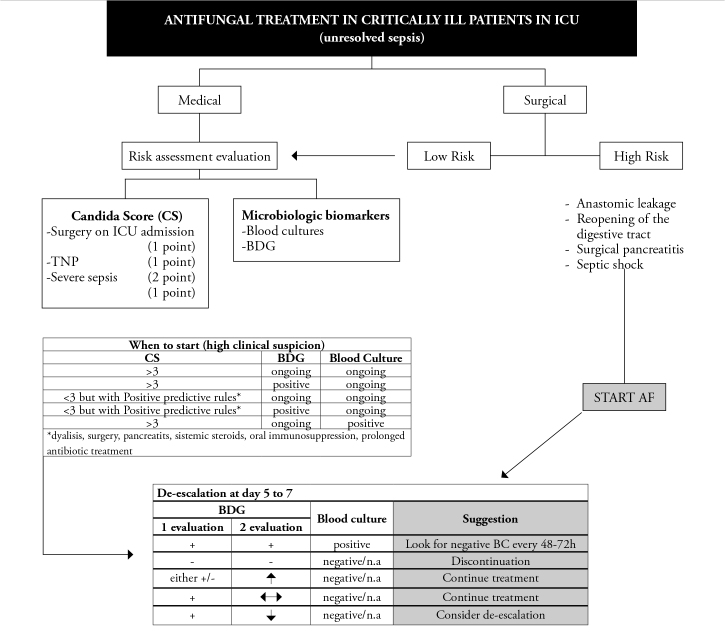
The 1,3-beta-D-glucan (BG) is a fungal cell wall antigen that can be detected in blood of patients with a sensitivity of 56–93% and a specificity of 71–100% for candidiasis (28). In a recent meta-analysis of 11 studies, the sensitivity and specificity of BG for the diagnosis of IC were 57–97% and 56–93%, respectively (28). Thanks to its high NPV, BG is potentially useful for the therapy decision-making process and discontinuing of empirical antifungal therapy, a practice known as de-escalation and reinforced by the most recent guidelines (23, 24). An integrated strategy with BG and CS helped to withhold or discontinue treatment, saving precious money without increasing mortality in 198 severely ill patients admitted to ICU with sepsis and a CS≥3 (29). In patients with suspected IAC, Tissot et al. compared the diagnostic accuracy of BG to CS and CI in high-risk surgical ICU patients (abdominal surgery or acute pancreatitis and ICU stay ≥72h) (30). The results showed that in patients with recurrent GI tract perforation, BG ≥80 pg/mL discriminated IAC from colonization with 72% PPV and 80% NPV and was superior to CI and CS (30). Moreover, BG determination preceded microbiological documentation of IAC with intra-abdominal cultures and start of antifungal therapy by a median of five and six days, respectively, suggesting a potential role on a pre-emptive basis (30). Also, BG kinetics reflected severity of infection, response to antifungal therapy and clinical outcome, suggesting that BG can be used as a reliable marker to stop or de-escalate antifungal treatment (Figure 1) (31). Molecular-based diagnostic tests can potentially be very sensitive in detecting an invasive fungal infection and may provide results more rapidly than standard diagnostic procedures, but so far few data are available and they are not yet recommended, because of the heterogeneity of the available results, the lack of reliable reference standards and differences in techniques (26, 32, 33).
Figure 1.
Algorithm of antifungal treatment possible de-escalation strategies in ICU patients [Modified from Eggimann et al. (31)]
TNP: total parenteral nutrition; BDG: beta-D-glucan; AF: antifungal; + : positive (>80 pg/mL); −: negative
In conclusion, we have multiple predictive tools for invasive candidiasis, which may suggest how and when to start empiric antifungal treatment in critically ill patients. However, since the effect of these common antifungal strategies in non-neutropenic critically ill patients on mortality was criticized (34, 35), it may be reasonable to use these strategies acknowledging that, from an antifungal stewardship approach, de-escalation is the key!
Main topic of this debate will be “untargeted antifungal treatment”.
Should we start antifungal treatment before the IFI diagnosis? If yes, which criteria?
Are there indeed any criteria for starting empirical antifungal treatment in icu patients?
What has the experience in the antifungal treatment has shown us? any change of the paradigmas?
Another question may be: “which antifungal”? (there is a -almost commercial-competition).
What is the duration of antifungal treatment?
What is the role of these issues on morbidity, mortality and cost?
Nahit Çakar
Associate Editor
References
- 1.Bassetti M, Righi E, Ansaldi F, Merelli M, Trucchi C, De Pascale G, et al. A multicenter study of septic shock due to candidemia: outcomes and predictors of mortality. Intensive Care Med. 2014;40:839–45. doi: 10.1007/s00134-014-3310-z. https://doi.org/10.1007/s00134-014-3310-z. [DOI] [PubMed] [Google Scholar]
- 2.De Rosa FG, Trecarichi EM, Montrucchio C, Losito AR, Raviolo S, Posteraro B, et al. Mortality in patients with early- or late-onset candidaemia. J Antimicrob Chemother. 2013;68:927–35. doi: 10.1093/jac/dks480. https://doi.org/10.1093/jac/dks480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M, et al. Incidence, characteristics and outcome of ICU-acquired candidemia in India. Intensive Care Med. 2015;41:285–95. doi: 10.1007/s00134-014-3603-2. https://doi.org/10.1007/s00134-014-3603-2. [DOI] [PubMed] [Google Scholar]
- 4.Lortholary O, Desnos-Ollivier M, Sitbon K, Fontanet A, Bretagne S, Dromer F French Mycosis Study Group. Recent exposure to caspofungin or fluconazole influences the epidemiology of candidemia: a prospective multicenter study involving 2,441 patients. Antimicrob Agents Chemother. 2011;55:532–8. doi: 10.1128/AAC.01128-10. https://doi.org/10.1128/AAC.01128-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamdy RF, Zaoutis TE, Seo SK. Antifungal stewardship considerations for adults and pediatrics. Virulence. 2016;2:1–15. doi: 10.1080/21505594.2016.1226721. https://doi.org/10.1080/21505594.2016.1226721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Rosa FG, Corcione S, Filippini C, Raviolo S, Fossati L, Montrucchio C, et al. The Effect on mortality of fluconazole or echinocandins treatment in candidemia in internal medicine wards. PLoS One. 2015;10:e0125149. doi: 10.1371/journal.pone.0125149. https://doi.org/10.1371/journal.pone.0125149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charles PE, Doise JM, Quenot JP, Aube H, Dalle F, Chavanet P, et al. Candidemia in critically ill patients: difference of outcome between medical and surgical patients. Intensive Care Med. 2003;29:2162–9. doi: 10.1007/s00134-003-2002-x. https://doi.org/10.1007/s00134-003-2002-x. [DOI] [PubMed] [Google Scholar]
- 8.Yazdanparast K, Auger P, Marchand R, Carrier M, Cartier R. Predictive value of Candida colonization index in 131 patients undergoing two different cardiovascular surgical procedures. J Cardiovasc Surg. 2001;42:339–43. [PubMed] [Google Scholar]
- 9.Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R. Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg. 1994;220:751–8. doi: 10.1097/00000658-199412000-00008. https://doi.org/10.1097/00000658-199412000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eggimann P, Pittet D. Candida colonization index and subsequent infection in critically ill surgical patients: 20 years later. Intensive Care Med. 2014;40:1429e1448. doi: 10.1007/s00134-014-3355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Posteraro B, De Pascale G, Tumbarello M, Torelli R, Pennisi MA, Bello G, et al. Early diagnosis of candidemia in intensive care unit patients with sepsis: a prospective comparison of (1—>3)-β-D-glucan assay, Candida score, and colonization index. Crit Care. 2011;15:R249. doi: 10.1186/cc10507. https://doi.org/10.1186/cc10507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Senn L, Eggimann P, Ksontini R, Pascual A, Demartines N, Bille J, et al. Caspofungin for prevention of intraabdominal candidiasis in high-risk surgical patients. Intensive Care Med. 2009;35:903–8. doi: 10.1007/s00134-009-1405-8. https://doi.org/10.1007/s00134-009-1405-8. [DOI] [PubMed] [Google Scholar]
- 13.Bassetti M, Marchetti M, Chakrabarti A, Colizza S, Garnacho-Montero J, Kett DH, et al. A research agenda on the management of intra-abdominal candidiasis: results from a consensus of multinational experts. Intensive Care Med. 2013;39:2092–106. doi: 10.1007/s00134-013-3109-3. https://doi.org/10.1007/s00134-013-3109-3. [DOI] [PubMed] [Google Scholar]
- 14.Troughton JA, Browne G, McAuley DF, Walker MJ, Patterson CC, McMullan R. Prior colonisation with Candida species fails to guide empirical therapy for candidaemia in critically ill adults. J Infect. 2010;61:403–9. doi: 10.1016/j.jinf.2010.08.013. https://doi.org/10.1016/j.jinf.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Barenfanger J, Arakere P, Cruz RD, Imran A, Drake C, Lawhorn J, et al. Improved outcomes associated with limiting identification of Candida spp. in respiratory secretions. J Clin Microbiol. 2003;41:5645–9. doi: 10.1128/JCM.41.12.5645-5649.2003. https://doi.org/10.1128/JCM.41.12.5645-5649.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Timsit J, Azoulay E, Schwebel C, Charles PE, Cornet M, Souweine B, et al. for the EMPIRICUS Trial Group. Empirical Micafungin Treatment and Survival Without Invasive Fungal Infection in Adults With ICU-Acquired Sepsis, Candida Colonization, and Multiple Organ FailureThe EMPIRICUS Randomized Clinical Trial. JAMA. 2016;316:1555–64. doi: 10.1001/jama.2016.14655. https://doi.org/10.1001/jama.2016.14655. [DOI] [PubMed] [Google Scholar]
- 17.Leon C, Ruiz-Santana S, Saavedra P, Galvan B, Blanco A, Castro C, et al. Usefulness of the “Candida score” for discriminating between Candida colonization and invasive candidiasis in non-neutropenic critically ill patients: a prospective multicenter study. Crit Care Med. 2009;37:1624–33. doi: 10.1097/CCM.0b013e31819daa14. https://doi.org/10.1097/CCM.0b013e31819daa14. [DOI] [PubMed] [Google Scholar]
- 18.Dupont H, Bourichon A, Paugam-Burtz C, Mantz J, Desmonts JM. Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis? Crit Care Med. 2003;31:752–7. doi: 10.1097/01.CCM.0000053525.49267.77. https://doi.org/10.1097/01.CCM.0000053525.49267.77. [DOI] [PubMed] [Google Scholar]
- 19.Ostrosky-Zeichner L, Pappas PG, Shoham S, Reboli A, Barron MA, Sims C, et al. Improvement of a clinical prediction rule for clinical trials on prophylaxis for invasive candidiasis in the intensive care unit. Mycoses. 2011;54:46–51. doi: 10.1111/j.1439-0507.2009.01756.x. https://doi.org/10.1111/j.1439-0507.2009.01756.x. [DOI] [PubMed] [Google Scholar]
- 20.Ostrosky-Zeichner L, Shoham S, Vazquez J, Reboli A, Betts R, Barron MA, et al. MSG-01: a randomized, double-blind, placebocontrolled trial of caspofungin prophylaxis followed by preemptive therapy for invasive candidiasis in highrisk adults in the critical care setting. Clin Infect Dis. 2014;58:1219–26. doi: 10.1093/cid/ciu074. https://doi.org/10.1093/cid/ciu074. [DOI] [PubMed] [Google Scholar]
- 21.Eggimann P, Ostrosky-Zeichner L. Early antifungal intervention strategies in ICU patients. Curr Opin Crit Care. 2010;16:465–9. doi: 10.1097/MCC.0b013e32833e0487. https://doi.org/10.1097/MCC.0b013e32833e0487. [DOI] [PubMed] [Google Scholar]
- 22.Azoulay E, Dupont H, Tabah A, Lortholary O, Stahl JP, Francais A, et al. Systemic antifungal therapy in critically ill patients without invasive fungal infection. Crit Care Med. 2012;40:813e822. doi: 10.1097/CCM.0b013e318236f297. [DOI] [PubMed] [Google Scholar]
- 23.Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:e1–50. doi: 10.1093/cid/civ933. https://doi.org/10.1093/cid/civ1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, et al. ESCMID Fungal Infection Study Group. ESCMID guideline for the diagnosis and management of Candida diseases 2012: nonneutropenic adult patients. Clin Microbiol Infect. 2012;18:19e37. doi: 10.1111/1469-0691.12039. [DOI] [PubMed] [Google Scholar]
- 25.Ostrosky-Zeichner L, Sable C, Sobel J, Alexander BD, Donowitz G, Kan V, et al. Multicenter retrospective development and validation of a clinical prediction rule for nosocomial invasive candidiasis in the intensive care setting. Eur J Clin Microbiol Infect Dis. 2007;26:271–6. doi: 10.1007/s10096-007-0270-z. https://doi.org/10.1007/s10096-007-0270-z. [DOI] [PubMed] [Google Scholar]
- 26.Scudeller L, Viscoli C, Menichetti F, del Bono V, Cristini F, Tascini C, et al. ITALIC Group. An Italian consensus for invasive candidiasis management (ITALIC) Infection. 2014;42:263–79. doi: 10.1007/s15010-013-0558-0. https://doi.org/10.1007/s15010-013-0577-x. [DOI] [PubMed] [Google Scholar]
- 27.Mikulska M, Calandra T, Sanguinetti M, Poulain D, Viscoli C. The use of mannan antigen and anti-mannan antibodies in the diagnosis of invasive candidiasis: recommendations from the Third European Conference on Infections in Leukemia. Crit Care. 2010;14:R222. doi: 10.1186/cc9365. https://doi.org/10.1186/cc9365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karageorgopoulos DE, Vouloumanou EK, Ntziora F, Michalopoulos A, Rafailidis PI, Falagas ME. b-DGlucan assay for the diagnosis of invasive fungal infections: a metaanalysis. Clin Infect Dis. 2011;52:750–70. doi: 10.1093/cid/ciq206. https://doi.org/10.1093/cid/ciq206. [DOI] [PubMed] [Google Scholar]
- 29.Posteraro B, Tumbarello M, De Pascale G, Liberto E, Vallecoccia MS, De Carolis E, et al. (1,3)-β-d-Glucan-based antifungal treatment in critically ill adults at high risk of candidaemia: an observational study. J Antimicrob Chemother. 2016;71:2262–9. doi: 10.1093/jac/dkw112. https://doi.org/10.1093/jac/dkw112. [DOI] [PubMed] [Google Scholar]
- 30.Tissot F, Lamoth F, Hauser PM, Orasch C, Flückiger U, Siegemund M, et al. Beta-glucan antigenemia anticipates diagnosis of blood culture-negative intraabdominal candidiasis. Am J Resp Crit Care Med. 2013;188:1100e1109. doi: 10.1164/rccm.201211-2069OC. [DOI] [PubMed] [Google Scholar]
- 31.Eggimann P, Que YA, Revelly JP, Pagani JL. Preventing invasive candida infections. Where could we do better? J Hosp Infect. 2015;89:302–8. doi: 10.1016/j.jhin.2014.11.006. https://doi.org/10.1016/j.jhin.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Avni T, Leibovici L, Paul M. PCR diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol. 2011;49:665–70. doi: 10.1128/JCM.01602-10. https://doi.org/10.1128/JCM.01602-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nguyen MH, Wissel MC, Shields RK, Salomoni MA, Hao B, Press EG, et al. Performance of Candida real-time polymerase chain reaction, beta-D-glucan assay, and blood cultures in the diagnosis of invasive candidiasis. Clin Infect Dis. 2012;54:1240–8. doi: 10.1093/cid/cis200. https://doi.org/10.1093/cid/cis200. [DOI] [PubMed] [Google Scholar]
- 34.Cortegiani A, Russotto V, Maggiore A, Attanasio M, Naro AR, Raineri SM, et al. Antifungal agents for preventing fungal infections in non-neutropenic critically ill patients. Cochrane Database Syst Rev. 2016:CD004920. doi: 10.1002/14651858.CD004920.pub3. https://doi.org/10.1002/14651858.cd004920.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cortegiani A, Russotto V, Raineri SM, Giarratano A. The paradox of the evidence about invasive fungal infection prevention. Crit Care. 2016;20:114. doi: 10.1186/s13054-016-1284-7. https://doi.org/10.1186/s13054-016-1284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]