Abstract
Objective
Multimodal analgesic methods are preferred for the treatment of postoperative pain; as a result, the additive effects of analgesics are provided while probable side effects are avoided. The current study aimed to compare the effects of the combination of dexketoprofen and paracetamol with regard to postoperative pain therapy.
Methods
Ninety-six patients who underwent non-malignant gynaecological laparotomy operations were included in this study. Patients were randomized into 3 groups. Group D received 50 mg intravenous dexketoprofen 15 minutes before the end of the operation and 8 and 16 hours after the operation. Group P received 1 g intravenous paracetamol and Group DP received the combination of 500 mg paracetamol and 25 mg dexketoprofen at the same time intervals. All patients received morphine infusion after operation. Total morphine consumption at 24 hours, visual analog scale, patient satisfaction and side effects were investigated.
Results
Comparison of the visual analog scale scores revealed that the Group DP presented lower scores at 24th hours compared to the other groups; and the difference between Group DP and Group D was statistically significant. Total morphine consumption was not significantly different between the three groups. The minimum number of side effects was observed in the Group DP.
Conclusion
Co-administration of paracetamol, dexketoprofen and morphine provided good analgesia and fewer side effects in gynaecological abdominal surgery.
Keywords: Postoperative pain, dexketoprofen, paracetamol, multimodal analgesia
Introduction
Postoperative pain is one of the most important factors contributing to increased morbidity and mortality after surgery. Rapid and effective pain therapy decreases the duration of hospital stay and enables patients to return more quickly to their normal daily activities. Numerous methods and drugs are used for analgesia. Particularly, in the case of abdominal surgery, there may be many drawbacks or limitations to the preferred analgesics during the postoperative period; for example, non-steroidal anti-inflammatory drugs (NSAIDs) can cause gastrointestinal problems and increased bleeding due to surgery and opioids can lead to constipation, respiratory depression and nausea or vomiting. To overcome these problematic issues, multimodal analgesic methods are preferred because the additive effects of analgesics can be obtained while the side effects are minimized. Much smaller doses are also needed for multi-modal analgesic techniques (1). The incidence of side effects resulting from opioids may also be decreased by the co-administration of paracetamol and combinations of opioids and NSAIDs (2). In addition, a variety of mechanisms have been shown to contribute to achieving these synergistic effects provided by multimodal analgesia.
Dexketoprofen trometamol is a non-selective NSAID of the aryl-propionic acid group containing the active S enantiomer of racemic ketoprofen. Dexketoprofen acts either peripherally at the lesion site or centrally on the central nervous system and its gastrointestinal side effects are low (3). Recently, the parenteral form, which provides a more rapid onset of action, was introduced commercially.
Paracetamol provides its analgesic effect through central anti-nociceptive actions, specifically with the inhibition of cyclooxygenase-3 (COX-3), which is a variant of cyclo-oxygenase-1 (COX-1) (4). In addition, there is evidence that paracetamol activates serotoninergic descending pathways that inhibit nociceptive signal transmission within the spinal cord (5). The most significant advantage of paracetamol is that it does not cause gastrointestinal bleeding or dyspepsia.
In this study, by evaluating patients with a high level of postoperative pain, we sought to evaluate the analgesic efficacy and side effect profile of intravenous dexketoprofen trometamol and intravenous paracetamol and/or the combination of these two drugs when they were added to morphine following peritoneal closure associated with gynaecological laparotomy operations.
Methods
After approval was received from the faculty ethics committee, and informed consent was obtained from the patients, 96 patients who were classified as ASA I–II and underwent elective non-malignant gynaecological laparotomy operations were included in this study. The primary exclusion criteria were as follows: any known heart, kidney, liver or haematological disease; allergy to the studied drugs; chronic pain history; routine analgesic use; ingestion/administration of the studied drugs in the previous 24 h and lack of consent or cooperation uncooperative behaviour. The secondary exclusion criteria were as follows: difficult extubation, intraoperative excessive bleeding and surgical complications.
During the preoperative visit, all patients were fully informed about the PCA device (patient-controlled analgesia, Abbott Pain Management Provider, Chicago) and the visual analogue scale used to assess pain (VAS; 0=no pain, 10=most severe pain).
All patients received premedication with intramuscular (im) 0.01 mg kg−1 midazolam 45 min prior to surgery. In the operating room, the patients were monitored for electrocardiogram (ECG) trace, peripheral oxygen saturation (SpO2), non-invasive blood pressure and end-tidal carbon dioxide (ETCO2). All patients received sodium thiopental (4–5 mg kg−1), fentanyl 1 μgr kg−1 and vecuronium 0.1 mg kg−1 for anaesthetic induction. Endotracheal intubation was performed and anaesthesia maintenance was provided by 1–2% sevoflurane and 50% N2O/O2. Fentanyl was administered during the last 30 min of surgery.
The patients were randomized into 3 groups using the closed envelope method. Group D received 50 mg intravenous (iv) dexketoprofen trometamol 15 min before the end of surgery and at 8 h and 16 h after the operation. Group P received 1 g iv paracetamol and group DP received the combination of 500 mg paracetamol and 25 mg dexketoprofen trometamol at the same time intervals. All drugs were prepared by the investigators before the operations. The study drugs were added to 100 mL saline solutions and the numbers and administration times were written on these prepared solutions. The drugs were administered by an anaesthetist who was blinded to the patient grouping. All patients received morphine infusion using a PCA device (bolus dose 2 mg, lock-up duration 10 min), which was initiated at the postoperative care unit. This infusion was administered for 24 h. At the end of the 24th h, the PCA infusion was continued only if the patient demonstrated a pain score >4 on the VAS.
The analgesic demand time, VAS scores at 1, 3, 6, 12, 18 and 24 h postoperatively, level of bleeding from drains in the abdomen, amount of total morphine consumed and morphine and fentanyl amounts were also recorded. This assessment was made by an investigator blinded to which patients were given the drug. In addition, all patients were followed in terms of nausea/vomiting (0=no nausea, 1=nausea present, 2=vomit present), dyspepsia, gastric bleeding or any other possible complications. Satisfaction scores for pain therapies were also recorded (1=very good, 2=good, 3=not bad, 4=bad, 5=very bad). If the postoperative nausea/vomiting score was 2 or higher, 10 mg iv metoclopramide was administered.
In a recent study, dexketoprofen administration was shown to decrease the need for opioids by 40% after abdominal hysterectomy (3). On the basis of this previous study, power analysis was performed according to the assumption of a 40% difference between groups in terms of opioid consumption (α=0.05 and β=0.20). For each group, 25 cases were deemed a sufficient number of patients.
Statistical analysis
The Statistical Package for the Social Sciences 13.0 (SPSS Inc.; Chicago, IL, USA) for Windows statistical package was used for all analyses. Patient characteristics, procedure duration, pain scores, postoperative morphine consumption, time to first postoperative analgesic, additional fentanyl use and patient satisfaction were analysed using an analysis of variance, the Kruskal-Wallis test, and the χ2-test where appropriate. Numerical data were assessed for a normal distribution using a one-way ANOVA. Significance was determined at the p<0.05 level. The results are given as medians (range) for non-parametric data and as the mean ± standard deviation (SD) for continuous data.
Results
The patients’ demographic data, anaesthesia duration and surgery duration were similar in all groups (Table 1). One patient from Group D (n=31) was excluded due to violation of the protocol; 2 patients from Group P (n=30) were excluded due to surgical complications and 2 patients from Group DP (n=30) were excluded due to lack of co-operation.
Table 1.
Patient characteristics and duration of surgery and anaesthesia
| Groups | ||||
|---|---|---|---|---|
| Group D (n=31) Mean±SD | Group P (n=30) Mean±SD | Group DP (n=30) Mean±SD | p | |
| Age (yr) | 49.6±12.2 | 47.9±13.4 | 50.2±12.9 | 0.568 |
| Weight (kg) | 72.3±18.2 | 71.5±14.6 | 72.3±14.3 | 0.541 |
| Duration of surgery (min) | 95.6±26.7 | 98.6±22.8 | 107.3±20.7 | 0.139 |
| Duration of anaesthesia (min) | 111.2±28.6 | 112.1±23.4 | 117.6±19.1 | 0.437 |
There were no differences between groups in terms of fentanyl usage during the surgical period. When we compared the groups’ VAS scores, we found that the paracetamol and dexketoprofen group (group DP) presented lower scores at 24th h after surgery than both groups D and P. The difference between group DP and group D was statistically significant (p<0.05) (Figure 1). Although the first postoperative analgesic requirement time was higher in group DP than in both of the other groups, the difference was not statistically significant (35.5 vs. 32.4 and 33, respectively) (p>0.05). Also, there were no significant differences between groups in terms of the total morphine consumption (p>0.05) (Table 2). The analgesic satisfaction score in all three groups are shown in Figure 2. There was no significant difference between the satisfaction scores of the 3 groups. The amount of postoperative bleeding was similar in all groups.
Figure 1.
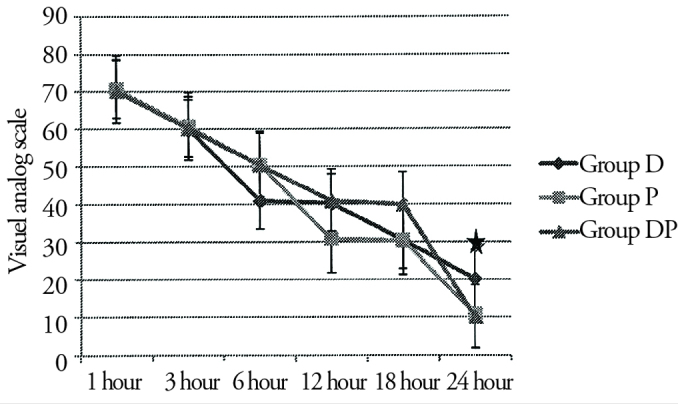
Visual analog scale of patients (mean±SD)
*p<0.05
Table 2.
Values of the first postoperative analgesic requirement time and total morphine consumption in patients
| Groups | ||||
|---|---|---|---|---|
| Group D (n=31) Mean±SD | Group P (n=30) Mean±SD | Group DP (n=30) Mean±SD | p | |
| The first postoperative analgesic requirement time (minute) | 32.4±11.1 | 33±12.1 | 35.5±10.4 | 0.523 |
| Total morphine consumption (mg) | 29±12.5 | 30.3±9.9 | 30.4±10.4 | 0.970 |
Figure 2.
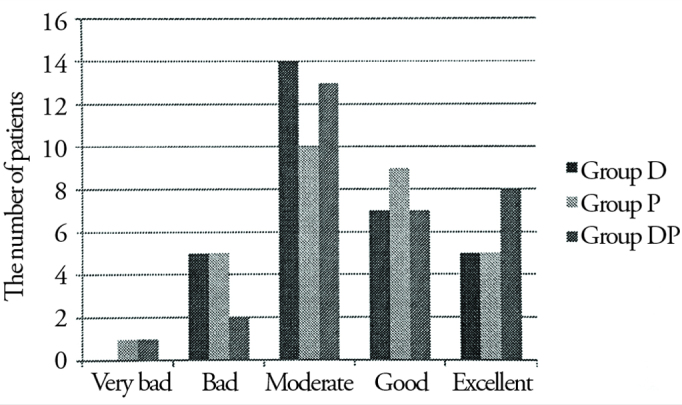
Patients satisfaction
In regards to adverse effects, there were 7 patients in Group D with nausea as well as 5 patients with vomiting within all patients and in Group D 2 patients who required treatment with metoclopramide. Group P presented 7 patients with nausea, 5 patients with vomiting, and 4 who were treated with metoclopramide. Group DP presented 3 patients with nausea, 3 patients with vomiting, and 2 who were treated with metoclopramide. All groups had same number of patients in terms of dyspepsia (Table 3).
Table 3.
Side effects
| Groups | |||
|---|---|---|---|
| Group D (n=31) (+/−) (%) | Group P (n=30) (+/−) (%) | Group DP (n=30) (+/−) (%) | |
| Nausea | 7/24 (22.5%) | 7/23 (23%) | 3/27 (10%) |
| Vomiting | 5/26 (16%) | 5/25 (16%) | 3/27 (10%) |
| Dyspepsia | 3/28 (9.6%) | 2/28 (6.6%) | 3/27 (10%) |
| Gastrointestinal bleeding | 0/31 | 0/30 | 0/30 |
| Total | 15 (48.5%) | 14 (48.1%) | 9 (30%) |
Discussion
In our study, there was no significant difference in analgesic efficacy between paracetamol and dexketoprofen trometamol alone. When paracetamol and dexketoprofen were administered together in the late post-operative period, more effective analgesia was observed.
A variety of analgesic agents, such as opioids and NSAIDs, are used during the postoperative period. Although opioid analgesics are the traditional first line treatment in this setting, they have the potential to cause adverse events, which often leads to reluctance to increase the dose to achieve adequate analgesia. Anesthesiologists and surgeons are increasingly turning to non-opioid analgesic techniques as adjuvants for managing pain during the postoperative period. NSAIDs provide effective analgesia in patients with acute pain, either as a substitute for or as an adjunct to opioids (6). Moreover, NSAID agents deliver both central and peripheral analgesic effects in addition to their anti-inflammatory actions, and these drugs also have pre-emptive analgesic effects and are better tolerated than opioids (7). Nevertheless, NSAID agents can have adverse effects on the haematological, gastrointestinal and renal systems, which is the reason for drawbacking of NSAID agents during the postoperative period.
A more rapid onset of action, which is important in acute postoperative pain, is the main purpose for selecting dexketoprofen among other NSAID agents. Animal studies have shown that the analgesic and anti-inflammatory effects of dexketoprofen are at least twice as potent as those of ketoprofen (8). Also in the literature, some studies have indicated that the postoperative use of (oral, im or iv) dexketoprofen decreases the consumption of tramadol or morphine (9, 10).
The analgesic efficacy and reliability of paracetamol is very well established. Since the iv form of paracetamol was made available in our country, it has become increasingly preferred for postoperative analgesia. Brodner et al. (11) compared iv paracetamol (1 g, 4 times daily), dipyrone (1 g, 4 times daily) and parecoxibin (40 g, twice daily) in cases of minor-to-moderate surgeries; and these authors found that paracetamol demonstrated similar analgesic efficacy compared with the other two agents during the postoperative period.
Paracetamol, NSAIDs and opioids can also be used in combination. Uzun et al. (12) compared paracetamol + morphine vs. paracetamol + metamizole + morphine during the post-operative period after lumbar disc surgery and concluded that the addition of metamizole led to significantly better results. In another study comparing paracetamol + diclofenac vs. paracetamol + placebo during the post-operative period after mastectomy surgery, the authors concluded that the addition of diclofenac led to significantly better results (13). Although the combination doses of these two drugs are the same as those used in single-drug treatment, better analgesia is achieved with the combination. Nevertheless, the adverse effects of NSAIDs cannot be avoided. The aim of combination drug treatment is to achieve synergistic actions and fewer side effects. We sought to decrease the doses of both dexketoprofen and paracetamol in Group DP, as better analgesia and fewer side effects represented our primary goal. Indeed, at the end of our study, we observed that 24th h VAS scores of Group DP were significantly lower than those of the other groups. Additionally, the nausea and vomiting side effects were significantly lower in this group, which may have been due to the decreased doses of the study drugs in Group DP.
Miranda et al. (14) also evaluated the combination of paracetamol and NSAID agents, and they concluded that there were supra-additive and synergistic actions. These results may reduce the concerns about the potential side effects of NSAIDs, such as gastric irritation, gastric bleeding and impaired coagulation. Therefore, this experimental study suggested that decreased doses of these combination drugs may lead to reduced side effects. Similarly, less adverse effects were seen in Group DP.
In our study, there was no significant difference between the satisfaction scores of the 3 groups. However, the number of patients with an ‘excellent’ satisfaction score was slightly higher in Group DP, which may have been associated with the lower incidence of nausea/vomiting. NSAIDs are known to have side effects on the gastrointestinal system, including dyspepsia, gastric ulcer-erosion and peptic discomfort and lower drug doses may, therefore, reduce these effects. In addition, lower doses of these drugs may also decrease treatment expenses.
Conclusion
Our study showed that lower doses of dexketoprofen combined with paracetamol resulted in improved VAS scores at 24th h after surgery when compared with either drug administered alone. Although the low value of a does not show that combination therapy is better, when the pain values are taken into account, lower doses of these combination drugs may have the advantages of reduced cost and fewer side effects. Thus, in daily routine practice, drug combinations may be preferred.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Eskişehir Osmangazi University School of Medicine.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - D.C.; Design - D.C., M.S.G.; Supervision - A.B.; Resources - D.C.; Materials - D.C.; Data Collection and/or Processing - D.C.; Analysis and/or Interpretation - D.C., A.B.; Literature Search - D.C.; Writing Manuscript - D.C.; Critical Review - A.B., M.S.G.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Kiliçaslan A, Tuncer S, Yüceaktaş A, Uyar M, Reisli R. The effects of intravenous paracetamol on postoperative analgesia and tramadol consumption in caesarean operations. Agri. 2010;22:7–12. [PubMed] [Google Scholar]
- 2.Keskinbora K. Opioid Analgesics. In: Erdine Serdar., editor. Pain. Istanbul: Nobel; 2007. pp. 581–604. [Google Scholar]
- 3.Tuncer S, Reisli R, Kececioglu M, Erol A. The effects of intravenous dexketoprofen on postoperative analgesia and morphine consumption in patients undergoing abdominal hysterectomy. Agri. 2010;22:98–102. [PubMed] [Google Scholar]
- 4.Chandrasekharan NV, Dai H, Roos KL, Evanson NK, Tomsik J, Elton TS, et al. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophene and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad Sci USA. 2002;99:13926–31. doi: 10.1073/pnas.162468699. https://doi.org/10.1073/pnas.162468699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Remy C, Marret E, Bonnet F. State of the art of paracetamol in acute pain therapy. Curr Opin Anaesthesiol. 2006;19:562–5. doi: 10.1097/01.aco.0000245285.30282.70. https://doi.org/10.1097/01.aco.0000245285.30282.70. [DOI] [PubMed] [Google Scholar]
- 6.Bilir A, Gulec S, Turgut M, Cetinkaya D, Erkan A, Kurt I. Lornoxicam in extracorporeal shock-wave lithotripsy; comparison with tenoxicam and placebo in terms of analgesic consumption. Scand J Urol Nephrol. 2008;42:143–7. doi: 10.1080/00365590701225988. https://doi.org/10.1080/00365590701225988. [DOI] [PubMed] [Google Scholar]
- 7.Gilron I, Milne B, Hong M. Cyclooxgenase-2 inhibitors in postoperative pain management: current evidence and future directions. Anesthesiology. 2003;99:1198–208. doi: 10.1097/00000542-200311000-00029. https://doi.org/10.1097/00000542-200311000-00029. [DOI] [PubMed] [Google Scholar]
- 8.Cabré F, Fernández MF, Calvo L, Ferrer X, García ML, Mauleón D. Analgesic, anti-inflammatory, and antipyretic effects of S(+)-ketoprofen in vivo. J Clin Pharmacol. 1998;38:3S–10S. [PubMed] [Google Scholar]
- 9.Hanna MH, Elliott KM, Stuart-Taylor ME, Roberts DR, Buggy D, Arthurs GJ. Comparative study of analgesic efficacy and morphine-sparing effect of intramuscular dexketoprofen trometamol with ketoprofen or placebo after major orthopaedic surgery. Br J Clin Pharmacol. 2003;55:126–33. doi: 10.1046/j.1365-2125.2003.01727.x. https://doi.org/10.1046/j.1365-2125.2003.01727.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tuncer S, Tavlan A, Köstekci H, Reisli R, Otelcioğlu S. Dexketoprofen for postoperative pain relief. Agri. 2006;18:30–5. [PubMed] [Google Scholar]
- 11.Brodner G, Gogarten W, Van Aken H, Hahnenkamp K, Wempe C, Freise H, et al. Efficacy of intravenous paracetamol compared to dipyrone and parecoxib for postoperative pain management after minor-to-intermediate surgery: a randomised, double-blind trial. Eur J Anaesthesiol. 2011;28:125–32. doi: 10.1097/EJA.0b013e32833fedfa. https://doi.org/10.1097/EJA.0b013e32833fedfa. [DOI] [PubMed] [Google Scholar]
- 12.Uzun S, Aycan IO, Erden IA, Sahin A, Aypar U. The addition of metamizole to morphine and paracetamol improves early postoperative analgesia and patient satisfaction after lumbar disc surgery. Turk Neurosurg. 2010;20:341–7. doi: 10.5137/1019-5149.JTN.3081-10.3. https://doi.org/10.5137/1019-5149.jtn.3081-10.3. [DOI] [PubMed] [Google Scholar]
- 13.Legeby M, Sandelin K, Wickman M, Olafsson C. Analgesic efficacy of diclofenac in combination with morphine and paracetamol after mastectomy and immediate breast reconstruction. Acta Anaesthesiol Scand. 2005;49:1360–6. doi: 10.1111/j.1399-6576.2005.00811.x. https://doi.org/10.1111/j.1399-6576.2005.00811.x. [DOI] [PubMed] [Google Scholar]
- 14.Miranda HF, Puig MM, Prieto JC, Pinardi G. Synergism between paracetamol and nonsteroidal anti-inflammatory drugs in experimental acute pain. Pain. 2006;121:22–8. doi: 10.1016/j.pain.2005.11.012. https://doi.org/10.1016/j.pain.2005.11.012. [DOI] [PubMed] [Google Scholar]


