Abstract
The aim of this study is to evaluate the effect of diabetes disease management program (DMP) on glycemic control in type 1 diabetes mellitus (T1DM) patients in Shantou China.
A sample of 240 participants recruited from 3C study Shantou subgroup was followed up in DMP for 3 years. The DMP provided self-management education, individualized therapy plan, diabetes complications screening, and laboratory examination periodical according to clinical practice guidelines. Primary outcomes were changes in hemoglobin A1C (HbA1c).
Two hundred one of the participants completed the follow-up. There was a significant decrease in the HbA1c levels after DMP implemented. The mean (± SD) pre- and post-intervention HbA1c levels were 10.26% ± 3.30% and 8.57% ± 1.57% respectively with a P value <0.001. General linear mixed model analyse demonstrated that changes in glycemic control were associated with insulin treatment regimen, frequency of Self-Monitoring of Blood Glucose (SMBG), diabetes diet adherence, physical activity, and duration of diabetes.
DMP helped to improve glycemic control and should be general implemented in China's T1DM. Individuals with basal-bolus regimen (multiple daily injections or pump therapy), more frequency of SMBG, following a diabetes diet, more physical activity, shorter diabetes duration may derive greater benefits from DMP.
Keywords: 3C study, disease management program, metabolic control, type 1 diabetes mellitus
1. Introduction
The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications studies have confirmed that strict control of blood glucose can significantly reduce and delay diabetes complications and improve the quality of life of patients.[1–3] Based on DCCT/EDIC and other studies, the target hemoglobin A1C (HbA1c) for all children and adolescents is recommended to be less than 7.5%, and less than 7% for adults.[4–6] However, a 2011 study by the International Diabetes Federation (IDF) investigating coverage, cost and care of type 1 diabetes mellitus (T1DM) in China (3C study) showed a very poor glycemic control in China; median HbA1c levels in both centers (Beijing and Shantou) were 8.50%, with 9.97% in Shantou,[7–14] which are not only much higher than the target HbA1c in guidelines, but also elevated compared with the amounts in developed countries.[15–17] How to improve metabolic control, and reduce the gap between patients and guide them is an urgent task for the prevention and treatment of type 1 diabetes in China.
To improve glycemic control, the type 1 diabetes disease management program (DMP) was established in Shantou center after the 3C study, according to chronic disease management systems (CDMS) and clinical practice guidelines (CPGs). Although the DMP has been used in diabetes improvement projects in many developed countries, it has never been tested in China. There is a lack of empirical evidence even for short-term efficacy of DMP for T1DM in China. The effects of DMP on glycemic control remain unexplored. The factors that influence glycemic control remain also unidentified. The aims of this study were to evaluate the effects of DMP on glycemic control in individuals with T1DM from the 3C study Shantou Center during the 3 years of follow-up, and to determine the influencing factors associated with glycemic improvement. We hypothesized that DMP implementation would lead to glycemic improvement and some controllable influencing factors identified could guide clinical management.
2. Design and methods
2.1. Design
The DMP was evaluated by a prospective cohort study using a before-and-after self-control design starting in April 2012; the patients were followed up until April 2015. The primary outcome was HbA1c level change. Secondary outcomes included changes of acute complication incidence, self-care activities, compliance rate for low-density lipoprotein cholesterol (LDL), insulin regimen, and insulin dose. The study was approved by the ethics committee of the First Affiliated Hospital of Shantou University Medical College, and the procedures conformed to the tenets of the Declaration of Helsinki. All participants provided signed informed consent.
2.2. Participants
The participants were recruited from the 3C study Shantou subgroup. T1DM patients who accepted long-time follow-up were recruited as participants; those with hearing, visual, physical, or mental impairment were excluded. Finally, 240 individuals were enrolled in this study, and divided into several groups according to age levels to receive DMP in the First Affiliated Hospital of Shantou University Medical College.
2.3. Interventions
Each participant was evaluated once a month and more often if indicated. The management team consisted of diabetologists, dietitians, educators, psychological therapists, and nurses with expertise on diabetes, who followed the management regulations prescribed in the CPGs accurately, building a private personal database for every individual with established T1DM. As there were no Chinese guidelines for type 1 diabetes in 2012, we used the International Diabetes Federation/International Society for Pediatric and Adolescent Diabetes (IDF/ISPAD) Guidelines for Diabetes in Childhood and Adolescence, 2011[7] as well as the American Diabetes Association (ADA) Medical Standards (2012)[8] and the International Standards for Diabetes management (2009).[9] Six management items were performed. Self-management education: each patient and parents (for patients under the age of 18) attended a diabetes education class lasting 4 hours each month, underwent evaluation for education efficiency, took diabetes education booklets home, and received diabetes information via smartphones. Self-monitoring of blood glucose (SMBG): a glucometer (Johnson & Johnson Onetouch Ultra, American) and 100 test strips each year were freely provided to each patient in DMP. Every patient and parents must master assessment and monitoring skills for glycemic control. Nutrition therapy: experienced dietitians conducted nutrition therapy into diabetes management and education by using the foodstuff substitution method according to ADA and ISPAD guidelines. Physical activity: patients were advised to perform at least 150 min/week of moderate-intensity aerobic physical activity (50%–70% of maximum heart rate), spread over at least 3 days/wk with not more than 2 consecutive days without exercise. Health care providers provided individualized exercise therapy plan according to patient age, heat rate, and other health conditions. Patient-centered self-management: diabetologists proposed individualized blood glucose target and therapy management for each patient with T1DM according to ISPAD and ADA guidelines. During follow-up diabetologists adapted their therapy management to blood glucose data, insulin administration, and economic status. Regular testing of blood glucose and lipid levels, as well as acute and chronic complications, according to ISPAD and ADA guidelines.
2.4. Data collect and measurements
At each visit, blood pressure, body weight, height, waist-to-hip ratio, and laboratory measurements were performed according to routine protocols. Treatment compliance and self-care including drug use, insulin dosage and injection, SMBG, and life-style modification were recorded by doctors during clinical visits. Lab tests and diabetes complications were screened at each scheduled visit. HbA1c, urinary albumin/creatinine ratio (ACR), and urinary ketone bodies were assessed every 3 months. Lipid levels and ophthalmic fundus examination were assessed every 12 months. HbA1c levels were measured by the Dry immune markers scattering quantitative method with a point-of-care testing analyzer (Afinion AS100, Norway).
2.5. Statistical analysis
Means and standard deviations or percentages were calculated for various variables. T test was used to assess differences in means between 2 groups; χ2 test was used for categorical variables. A linear mixed model was fitted to identify predictors of HbA1c improvement at 36 months of follow-up. Data from different visits over time were analyzed in a repeated measurements model. A linear mixed model included the following independent variables: gender, age, duration, education level, average monthly family income, type of medical insurance, type of habitat, frequency of SMBG, days of diabetes diet compliance in the last week, physical activity ≥150 min/wk or not, presence or absence of diabetic ketoacidosis (DKA) at onset, presence or absence of a family history of diabetes, insulin dose, and insulin regimen.
A total of 240 individuals with T1DM were enrolled, including 201 who completed follow-up for 3 years. Thirty-nine cases were lost to follow-up, including 14 for immigration reasons and 25 who were out of touch. To avoid loss of effective information, data from the 39 cases lost to follow-up were included in baseline demographic (Table 1) and mixed linear regression (Table 2) analyses. Nevertheless, the 39 cases were excluded from the final dataset (Table 3) and comparisons between baseline and follow-up data (Table 4 and Fig. 1), to avoid information bias.
Table 1.
Profile of participants.
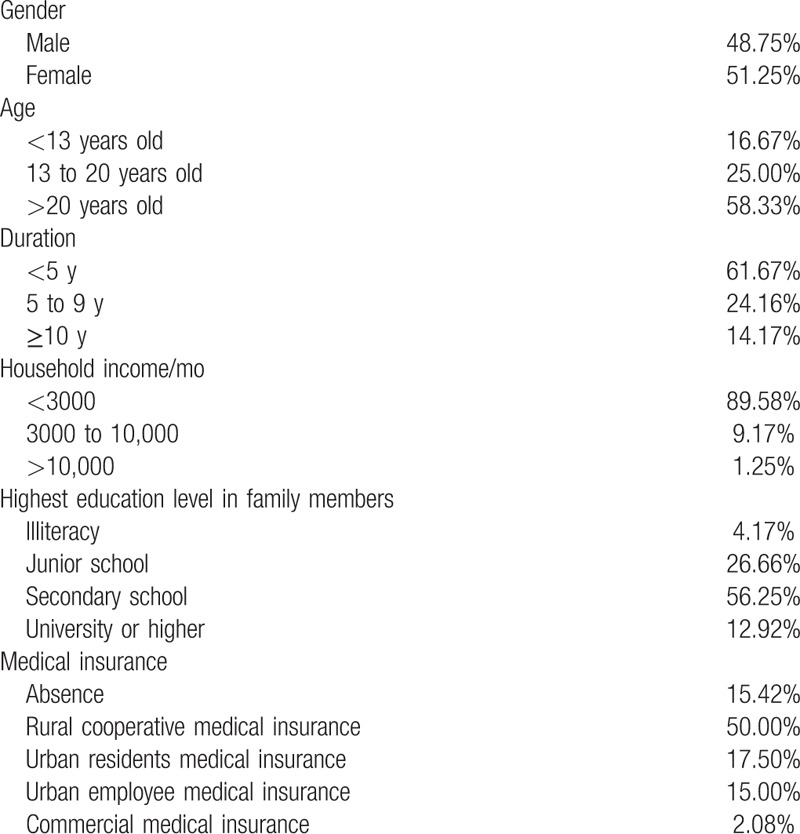
Table 2.
Linear mixed models to estimate strength of study variables to predict improvements of glycemic control in DMP from baseline to 36 months follow-up.
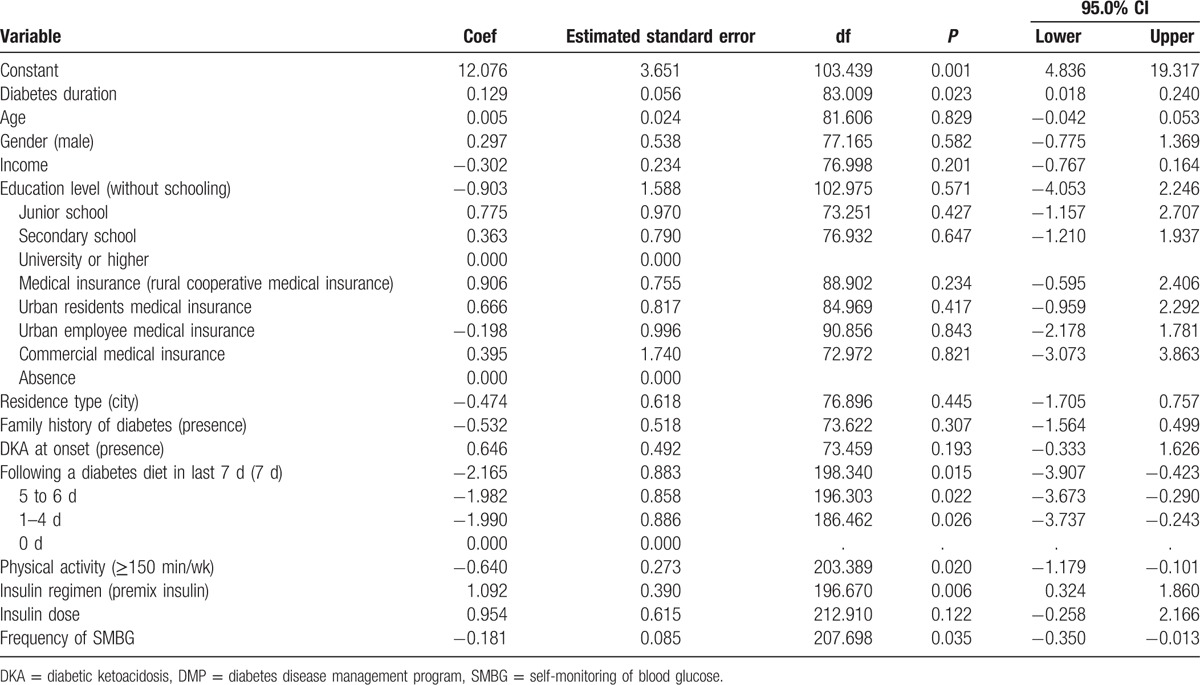
Table 3.
Changes in primary and secondary outcome measures over 36 mo in DMP.
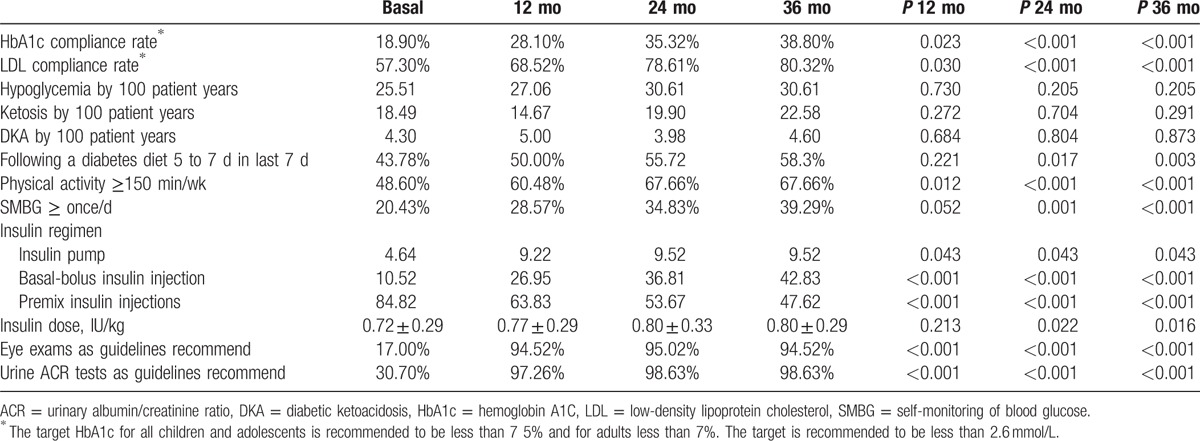
Table 4.
Changes in HbA1c from basal to 36 mo stratified by different insulin treatment.
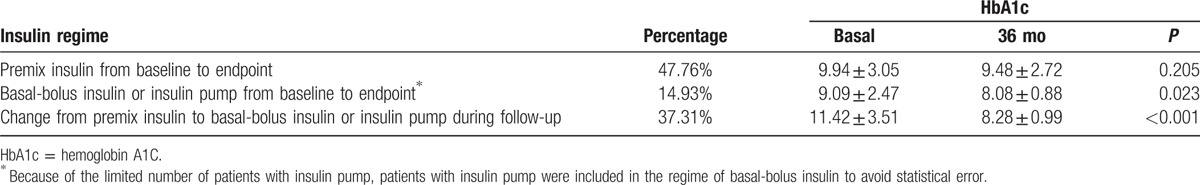
Figure 1.
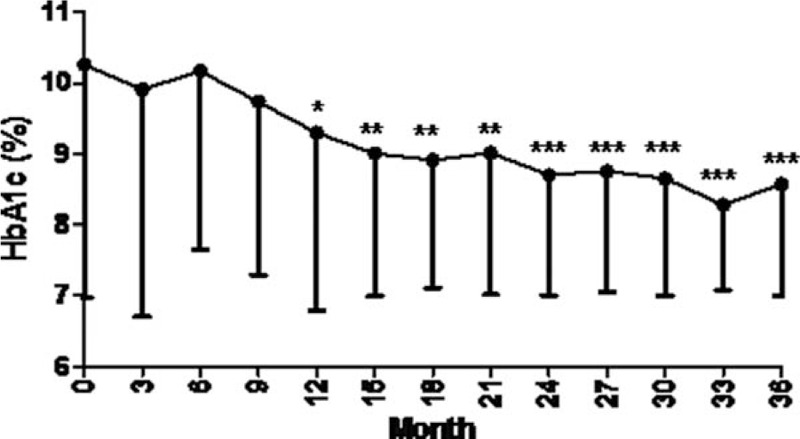
Changes in HbA1c levels over 36 months in DMP. ∗P <0.05, ∗∗P <0.01, ∗∗∗P <0.001 compared with baseline HbA1c. There were 201 cases, excluding those lost to follow-up. DMP = diabetes disease management program, HbA1c = hemoglobin A1C.
3. Results
A total of 240 individuals with T1DM were enrolled, and 201 completed 3-year follow-up. Demographic and clinical characteristics of the study population are shown in Table 1. At baseline, median age was 24.77 years, with a median T1DM duration of 5.12 years. Most participants had low income and low education level, and were predominantly from rural areas, similar to data of 3C study.
Changes in primary and secondary outcome measures over 3 years in DMP are shown in Table 3 and Figure 1. After interventions, there was a significant decrease in HbA1c levels from baseline to final values at 36 months. Mean pre- and postintervention HbA1c levels were 10.26% ± 3.30% and 8.57% ± 1.57%, respectively (P <0.001). 38.80% of individuals achieved target HbA1c and 70.53% showed improved overall glycemic control at the trial endpoint. Percent population with LDL-C <2.6 mmol/L increased from 57.30% to 80.32% (P <0.001). There were no significant differences in incidence rates of acute complications between baseline and postintervention. Specifically, the incidence of hypoglycemia was not significantly increased. According to diabetes self-management, significantly increased proportions were found in diabetes diet compliance, exercise, SMBG, basal-bolus insulin treatment, and complication screening according to CPGs.
Furthermore, linear mixed models were used to identify predictors of improvement in glycemic control (Table 2). The factors associated with glycemic improvement were insulin treatment regimen, frequency of SMBG, diabetes diet adherence, physical activity, and duration of diabetes. Participants with basal-bolus approach, higher frequency of SMBG, higher diabetes diet compliance, more physical activity, shorter diabetes duration exhibited greater improvement in glycemic control in DMP. No other variables were significantly associated with changes in HbA1c. Insulin treatment regimen had the strongest correlation with HbA1c (P = 0.06) among relevant factors.
Since insulin treatment had the strongest correlation with HbA1c, we further analyzed the effects of different insulin regimens on glycemic control. As shown in Table 4, individuals with basal-bolus insulin regimen had better glycemic control compared with those with premix insulin regimen. Among them, the individuals who changed insulin treatment from premix to basal-bolus insulin or insulin pump regimen had the greatest glycemic improvement.
4. Discussion
As a complex chronic disease, diabetes imposes a unique burden on the health care system, and the people providing and/or receiving care. China's medical system still lags far behind the Western one. The existing differences among numerous diabetes patients increased health service demand and lack of health care resources is increasing acute and widespread. In classical Chinese medicine, diabetes treatment depended on patients’ enthusiasm of seeing doctors because of the lack of follow-up management system. Current care and education of individuals with type 1 diabetes remain poor. The deficient knowledge of diabetes and poor medical compliance lead to unsatisfactory outcomes, for example, high frequency of DKA. Nearly 41% of children with undiagnosed diabetes present with diabetic ketoacidosis, a life-threatening acute complication of diabetes that occurs with late or misdiagnosis.[18] Due to insufficient capital input from the government and a nonbalanced medical insurance system, the current living status of T1DM patients in underdeveloped regions of China is more serious. Therefore, it is really urgent to improve the treatment of T1DM, changing the retrograde medical mode and management system.
The type 1 diabetes disease management program, according to CDMS, includes essential components for chronic disease: supportive health policy, decision support, timely information, access to essential medicines and technology, self-management education and follow-up, innovative delivery system design, and training of health professionals. Based on the current findings, the DMP was really effective. Glycemic control was significantly improved in participants of DMP. 38.80% of individuals achieved the target HbA1c, and 70.53% showed improved overall glycemic control. Furthermore, the proportion of individuals following diabetes self-management was significantly increased, and 37.22% of individuals changed insulin regimen from premix to basal-bolus type; 39.29% checked blood glucose at least once per day, and more than 90% completed complication screening according to CPGs. In 3C study HbA1c was significantly associated with region, income, education level, and injections/day; meanwhile, injections/day was significantly associated with hours of education. In this follow-up study, changes in glycemic control were associated with insulin treatment regime, frequency of SMBG, diabetes diet adherence, physical activity, and duration of diabetes.
DMP is a highly complex intervention with the potential to improve glycemic control. A number of controlled studies have examined the efficacy of management program interventions for diabetes mellitus. A meta-analysis indicated that integrated management is associated with a significantly improvement in glycemic control and self-care activities.[19,20] Siminerio et al[21] showed a significant decrease by 0.95% in HbA1c after implementation of DMP. In Hong Kong, the proportion of patients achieving the target HbA1c was shown to be 3 times in the DMP group compared with the control group.[22] Loveman et al[23] conducted a systematic review to assess the clinical and cost effectiveness of educational interventions in 24 studies. The results showed a long lasting improvement in metabolic control and reduced complications in T1DM patients.[23]
Compared with other studies, the most important finding of this work was that insulin regimen had the strongest correlation with HbA1c in Chinese individuals with T1DM. Correcting insulin treatment (from premix insulin to basal-bolus injection 4 times/d) yielded the greatest glycemic improvement in the DMP. Intensive insulin therapy using the basal-bolus approach, whether as multiple daily injections or pump therapy, is considered the best treatment for individuals with T1DM regardless of age.[16,24,25] Yet, so many patients chose premix insulin in Shantou before. In 3C study the trend in Shantou to use premix insulin with 2 daily injections was reviewed with local experts who stated that patient compliance, convenience, and cost was the rationale for this practice. This implies availability and optimal use of insulin, tailoring the treatment according to the patient's/family's personality, preference, and way of living. Educating the patients and their families and training health care professionals are equally important. Our previous study suggested injections/day is significantly associated with hours of education. Several studies also found that with education and follow-up, reduced HbA1c and higher quality of life can be achieved without increased incidence of acute complications using multiple daily insulin injections.[26] In the present study, education and switching follow-up patients to standardized treatment yielded significantly great benefits from DMP, consistent with other reports.[25,26]
An interesting finding was that compared with changing insulin type, adjustment of insulin dose did not lead to significant glycemic improvement (P = 0.122). This suggested that rigid adjustment of insulin dosage in follow-up or outpatient visits may not be so important. There has been a change in emphasis from medical disease management to self-care by patients, in collaboration with health-care providers.[27] The terminology of adherence and compliance are gradually being replaced by self-management in T1DM care. CPGs and empowerment education place greater emphasis on the skills of self-flexible adjustment of insulin doses. Modification of insulin dosages based on diet and exercise can be challenging for patients, and should be considered an essential part of patient education. It is important that patients adjust their insulin doses appropriately in response to factors such as carbohydrate intake, lifestyle, exercise, and concurrent illness to minimize the risk of hypo- or hyperglycemia. Other programs have demonstrated that appropriate education can improve glycemic control while giving the individual more flexibility in terms of diet rather than having to adhere to rigid calorie control and fixed insulin doses.[28]
The incidence of hypoglycemia appears low in the 3C study. This may be due to the high HbA1c far above the target in Shantou. However, although HbA1c greatly decreased after systemic management, hypoglycemic events showed no significant changes. This suggested improved glycemic control does not imply increased hypoglycemia in DMP, corroborating other studies. For example, the UK-based Dose Adjustment for Normal Eating (DAFNE) program improves glycemic control and the quality of life while saving costs, without increasing the risk of severe hypoglycemia.[29] Similarly, in the Dusseldorf Diabetes Treatment and Teaching Program, HbA1c fell significantly from 8.1% to 7.3%, as did the number of severe hypoglycemic episodes.[28]
Following a diabetes diet and regularly exercising both improved glycemic control in DMP. Indeed, diabetes diet and physical activity are 2 of “5 carriages” in diabetes therapy; yet, most individuals with T1DM do not know how to put into practice. Unlike in developed countries, the barrier of carrying out management following a diabetes diet and physical activity is not hypoglycemia[30,31] but lack of education in China.
In the 3C study, due to lack of awareness and low socioeconomic conditions, most patients did not follow SMBG regularly. So a free glucometer with 100 test strips each year was provided to each patient in DMP. The results suggested that increased frequency of SMBG is another factor leading to improved glycemic control. Additional studies showed that frequent and accurate blood glucose monitoring as well as concomitant optimal adjustment of insulin to carbohydrate intake and exercise are required to attain and maintain optimal conditions.[32,33] The frequency of SMBG is associated with improved HbA1c in patients with T1DM.[32–35] Karter et al[36] found adults with T1DM who self-monitor 3 or more times per day have an HbA1c 1% lower metabolic control. Yet, to this day, most patients cannot monitor their blood glucose 4 to 6 times per day as guidelines recommend. A consistent barrier is financial situation. Few patients in China can afford blood glucose self-monitoring equipment. The government and Department of Medical Insurance should get involved in providing the needed help.
Another finding was that individuals with shorter duration showed greater improvement in glycemic control than patients with longer duration. This may be related to psychology and self-care adherence. Patients with longer duration pay insufficient attention to diabetes and self-care practices because of high study and work-related stress. Furthermore, with course extension, patients may suffer chronic complications of diabetes, which cause long-lasting psychological effects. The 3C study found that EQ index, a standardized index of health-related quality-of-life, is significantly lower in adults than in both children and adolescents. Seven adolescents with T1DM had a higher rate of depression and lower self-esteem[37] than younger children.[38] The older the participants, the worse their perceived school support and self-care behaviors.[39] Bad glycemic control would depress the patients, who consequently give up strict self-care, thus forming a vicious circle. This suggests more attention should be paid to patients with long diabetes duration, providing more psychological care and self-care education.
In the 3C study HbA1c was significantly associated with region, income, and education level. However, it was interesting that a number of other variables examined, for example age, gender, education level, and income did not appear to significantly predict glycemic control in DMP. This suggested that, in general, DMP is effective in improving glycemic control across a broad range of patients with type 1 diabetes.
This study had several limitations. Participants were recruited using convenience sampling from 6 hospitals in Shantou city. This may limit the generalizability of the results. Further studies should include larger samples, with more diverse participant populations. In addition, we used a cohort study design; case-control studies should be carried out to confirm the effectiveness of DMP. Finally, follow-up duration could be longer.
In summary, this 3-year follow-up cohort study indicated that DMP effectively improved metabolic control in patients with T1DM; the short-term management led to HbA1c decreasing by 1.7% and HbA1c compliance rate increasing by 20%, with no increase of hypoglycemia incidence. The controllable influencing factors related to glycemic improvement were basal-bolus regimen (multiple daily injections or pump therapy), more frequent SMBG, increased total physical activity, and better diabetes diet adherence. Changing the insulin regimen has the most important effect on glycemic control, while adjustment of insulin dose did not lead to significant glycemic improvement.
The above evidence suggested that the medical staff should focus on integrated management, diabetes education, and active follow-up in type 1 diabetes patients. Correcting insulin regimen (from premix to basal-bolus injection 4 times/d) is strongly recommended. The old medical management that promotes waiting in the outpatient department and adjusting insulin doses rigidly should be abandoned. Patients with short disease duration should be paid more attention because they may have greater benefits from DMP.
Acknowledgments
The authors sincerely thank Helen McGuire (IDF, Brussels, Belgium. Programmes and Policy), David Whiting (IDF, Brussels, Belgium. Programmes and Policy), Katarzyna Kissimova-Skarbek (Department of Health Economics and Social Security, Jagiellonian University, Institute of Public Health, Krakow, Poland), and JI Linong (Department of Endocrine, Peking University People's Hospital) for their outstanding contributions to 3C study. The authors also thank Sanofi Diabetes for unrestricted grant for 3C study. They thank Johnson & Johnson for providing free glucometers and test strips in DMP.
Footnotes
Abbreviations: 3C study = coverage cost and care of type 1 diabetes in China, ACR = urinary albumin/creatinine ratio, ADA = American Diabetes Association, CDMS = chronic disease management systems, CPGs = clinical practice guidelines, DAFNE = dose adjustment for normal eating, DCCT = diabetes control and complications trial, DKA = diabetic ketoacidosis, DMP = diabetes disease management program, HbA1c = hemoglobin A1C, IDF = International Diabetes Federation, ISPAD = International Society for Paediatric and Adolescent Diabetes, LDL = low-density lipoprotein cholesterol, SMBG = self-monitoring of blood glucose, T1DM = type 1 diabetes mellitus.
This work was sponsored by Shantou University Medical College Clinical Research Enhancement Initiative and Science and Technology Planning Project of Guangdong Province, China.
The authors have no conflicts of interest to disclose.
References
- [1].DCCT, Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–86. [DOI] [PubMed] [Google Scholar]
- [2].Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. The diabetes control and complications trial /epidemiology of diabetes interventions and complications (DCCT /EDIC) study research group. N Engl J Med 2005;353:2643–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].White NH, Sun W, Cleary PA, et al. Prolonged effect of intensive therapy on the risk of retinopathy complications in patients with type 1 diabetes mellitus: 10 years after the diabetes control and complications trial. Arch Ophthalmol 2008;126:1707–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].International Diabetes Federation Global IDF/ISPAD Guideline for Diabetes in Childhood and Adolescence. International Diabetes Federation 2011. [Google Scholar]
- [5].American Diabetes Association ADA Standards of Medical Care in Diabetes. Diabetes Care 2012;35:S11–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].International Diabetes Federation International Standards of Diabetes Education. International Diabetes Federation 2009. [Google Scholar]
- [7].Lin K, Yang X, Yin G, et al. Diabetes self-care activities and health related quality of life of individuals with Type 1 diabetes mellitus in Shantou, China. J Int Med Res 2016;44:147–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].McGuire H, Kissimova-Skarbek K, Whiting D, et al. The 3C study: coverage cost and care of type 1 diabetes in China-study design and implementation. Diabetes Res Clin Pract 2011;94:307–10. [DOI] [PubMed] [Google Scholar]
- [9].McGuire H, Ji L. China's 3C study—the people behind the numbers. Diabetes Voice 2012;57:6–9. [Google Scholar]
- [10].McGuire H, Ji L. The 3-C study—strong partnerships to improve care for people with type 1 diabetes in China. Diabetes Voice 2011;56: [Google Scholar]
- [11].McGuire H, Whiting D, Kissimova-Skarbek K, et al. Type 1 diabetes care and education in Beijing and Shantou: results of 3C study—coverage, cost and care. EASD Abstract 2012. [Google Scholar]
- [12].McGuire H, Kissimova-Skarbek K, Whiting D, et al. Coverage, cost and care of type 1 diabetes in Beijing and Shantou. ADA Abstract 2012;6. [Google Scholar]
- [13].McGuire H, Kissimova-Skarbek K, Whiting D, et al. Coverage, cost, care and education of type 1 diabetes in children and adolescents in Beijing and Shantou. 38th Annual Meeting of the International Society for Pediatric and Adolescent Diabetes-Abstract Preview 2012. [Google Scholar]
- [14].Kissimova-Skarbek K, McGuire H, Whiting D, et al. Health related quality of life of persons with Type 1 diabetes mellitus in Beijing and Shantou, China. EQ-5D results from 3C study: coverage, costs and care. Session: Assessing Health Status Indicators 2012. [Google Scholar]
- [15].Petitti DB, Klingensmith GJ, Bell RA, et al. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr 2009;155:668–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Mortensen HB, Hougaard P. Comparison of metabolic control in a cross-sectional study of 2873 children and adolescents with IDDM from 18 countries. The Hvidøre Study Group on Childhood Diabetes. Diabetes Care 1997;20:714–20. [DOI] [PubMed] [Google Scholar]
- [17].Nathan DM, Zinman B, Cleary PA, et al. DCCT /EDIC Research Group Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the Diabetes Control and Complications Trial /Epidemiology of Diabetes Interventions and Complications and Pittsburgh Epidemiology of Diabetes Complications experience (1983–2005). Arch Intern Med 2009;169:1307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Xin Y, Yang M, Chen XJ, et al. Clinical features at the onset of childhood type 1 diabetes mellitus in Shenyang, China. J Paediatr Child Health 2010;46:171–5. [DOI] [PubMed] [Google Scholar]
- [19].Knight K, Badamgarav E, Henning JM, et al. A systematic review of diabetes disease management program. Am J Manag Care 2005;11:242–50. [PubMed] [Google Scholar]
- [20].Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA 2006;296:427–40. [DOI] [PubMed] [Google Scholar]
- [21].Siminerio LM, Piatt GA, Emerson S, et al. Deploying the chronic care model to implement and sustain diabetes self-management training programs. Diabetes Educ 2006;32:253–60. [DOI] [PubMed] [Google Scholar]
- [22].Chan JC, So WY, Yeung CY, et al. Effects of structured versus usual care on renal endpoint in type 2 diabetes: the SURE study: a randomized multicenter translational study. Diabetes Care 2009;32:977–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Loveman E, Cave C, Green C, et al. The clinical and cost effectiveness of patient education models for diabetes: a systematic review and economic evaluation. Health Technol Assess 2003;7:1–90. [DOI] [PubMed] [Google Scholar]
- [24].Canadian Diabetes Association Clinical practise guidelines for the prevention and management of diabetes in Canada, 2008. Can J Diabetes 2008;32:S1–201. [DOI] [PubMed] [Google Scholar]
- [25].Bangstad HJ, Danne T, Deeb L, et al. Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes 2009;10:82–99. [DOI] [PubMed] [Google Scholar]
- [26].Usher-Smith JA, Thompson MJ, Sharp SJ, et al. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ 2011;7:343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Debono M, Cachia E. The impact of diabetes on psychological well being and quality of life. The role of patient education. Psychol Health Med 2007;12:545–55. [DOI] [PubMed] [Google Scholar]
- [28].Samann A, Muhlhauser I, Bender R, et al. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Diabetologia 2005;48:1965–70. [DOI] [PubMed] [Google Scholar]
- [29].DAFNE., Study Group Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325:746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Plotniko ff RC, Taylor LM, Wilson PM, et al. Factors associated with physical activity in Canadian adults with diabetes. Med Sci Sports Exerc 2006;38:1526–34. [DOI] [PubMed] [Google Scholar]
- [31].Brazeau AS, Rabas a-Lhoret R, Strych ar I, et al. Barriers to physical activity among patients with type 1 diabetes. Diabetes Care 2008;31:2108–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Anderson B, Ho J, Brackett J, et al. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin dependent diabetes mellitus. J Pediatr 1997;130:257–65. [DOI] [PubMed] [Google Scholar]
- [33].Svoren BM, Volkening LK, Butler DA, et al. Temporal trends in the treatment of pediatric type 1 diabetes and impact on acute outcomes. J Pediatr 2007;150:279–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Haller MJ, Stalvey MS, Silverstein JH. Predictors of control of diabetes: monitoring may be the key. J Pediatr 2004;144:660–1. [DOI] [PubMed] [Google Scholar]
- [35].Schneider S, Iannotti RJ, Nansel TR, et al. Identification of distinct self-management styles of adolescents with type 1 diabetes. Diabetes Care 2007;30:1107–12. [DOI] [PubMed] [Google Scholar]
- [36].Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med 2001;111:1–9. [DOI] [PubMed] [Google Scholar]
- [37].International Society for Pediatric, Adolescent Diabetes International declarations In: ISPAD Guidelines, Medical Forum International, Zeist 2000;121–4. [Google Scholar]
- [38].Grey M, Davidson M, Boland E, et al. Clinical and psychosocial factors associated with achievement of treatment goals in adolescents with diabetes. J Adoles Health 2001;28:377–85. [DOI] [PubMed] [Google Scholar]
- [39].Mandali SL, Gordon TA. Management of type 1 diabetes in schools: whose responsibility? J Sch Health 2009;79:599–601. [DOI] [PubMed] [Google Scholar]


