Abstract
Background:
Both adductor canal block (ACB) and periarticular infiltration (PI) have been shown to reduce pain after total knee arthroplasty (TKA) without the motor blockade. However, the efficacy and safety of combined ACB with PI (ACB + PI) as compared to PI alone for analgesia after TKA remains controversial. We therefore performed a meta-analysis to compare the effects of ACB + PI with PI alone on pain controll after TKA.
Methods:
PubMed, Medline, Embase, Web of Science, and the Cochrane Library were searched to identify studies comparing ACB + PI with PI alone for TKA patients. The primary outcomes included pain score with rest or activity and morphine consumption. Secondary outcomes were distance walked, length of hospital stay, and postoperative complications. Relevant data were analyzed using RevMan v5.3.
Results:
Three studies involving 337 patients were included. Combined ACB with PI was associated with longer distances walked than PI alone (MD = 7.27, 95% CI: 0.43–14.12, P = 0.04) on postoperative day 1. The outcomes of pain, morphine consumption, length of hospital stay, and postoperative complications were not statistically different between the 2 groups (P > 0.05).
Conclusion:
Our meta-analysis suggests that combined ACB with PI may achieve earlier ambulation for patients after TKA without a reduction in analgesia when compared to PI alone in the early postoperative period. There were no significant differences in morphine consumption, length of hospital stay, and postoperative complications between the 2 groups. However, owing to the variation of included studies, no firm conclusions can be drawn.
Keywords: adductor canal block, meta-analysis, periarticular infiltration, postoperative analgesia, total knee arthroplasty
1. Introduction
Total knee arthroplasty (TKA) is one of the most successful surgical procedures to treat patients with end-stage knee osteoarthritis. However, TKA can be associated with moderate to severe pain in the early postoperative period, affecting the quality of life and rehabilitation of patients undergoing TKA.[1] An ideal analgesia regimen in TKA should preserve knee mobilization ability, enable earlier physical therapy, hasten recovery, shorten hospital stay, lower the risk of postoperative complications, and improve patient satisfaction.[2,3]
The traditional analgesic techniques for TKA patients are patient-controlled analgesia (PCA) opioids, epidural analgesia (EA), and femoral nerve block (FNB). Patients who received PCA often complained about nausea, vomiting, and pruritus.[4] The use of EA is usually associated with side effects such as hypotension, urinary retention, and pruritus.[5,6] FNB has been part of the standard postoperative pain relief protocols following TKA in last decade, which has many advantages over PCA or EA in TKA.[6,7] However, FNB reduces the strength of the quadriceps muscle, which may increase the risk of postoperative falls and delay early postoperative mobilization, influencing patient satisfaction.[8,9] Thus, an analgesic option with preserved motor function and adequate analgesia for TKA patients still remains a challenge for the surgeons.
Recently, there has been increased interest in the ultrasound-guided adductor canal blockade (ACB) for pain management after TKA with obvious advantages. The adductor canal involves the vastus medialis nerve, medial femoral cutaneous nerve, articular branches from the obturator nerve, as well as the medial retinacular nerve in addition to saphenous nerve that innervate the medial, lateral, and anterior aspects of the knee.[3,10] In theory, ACB is almost a pure sensory nerve block, which only influences the motor function of vastus medialis due to its impact on nerve to the muscle as it traverses the adductor canal,[11] and thus may largely decrease the incidence of fall.[11,12] Moreover, multiple clinical studies[3,10,11] and several meta-analyses[13,14] have reported that ACB could provide quadriceps muscle strength preservation, better ambulatory ability, and earlier functional recovery with similar analgesic effects and morphine consumption as compared to FNB in patients after TKA. Periarticular infiltration (PI) is an alternative regional anesthesia technique with a combined administration of local anesthetics, NSAIDs, and epinephrine injected into the knee joint during the operation, which has quickly gained popularity in TKA patients for its simplicity, apparent safety, and effectiveness over the last decade.[15] Meanwhile, PI has been shown to have an effective pain control after TKA without the motor blockade associated with EA or FNB.[15–17]
These studies demonstrate that both ACB and PI have been shown to reduce pain after TKA without the motor blockade and impairing quadriceps function. However, the duration and efficacy of a single-dose PI are not sufficient after TKA.[18] Several studies have utilized the insertion of an intraarticular catheter to prolong analgesia, but no positive benefits of this technique after TKA could be identified, in contrast it may increase expense, pain, and possibly infection risks.[19,20] An ACB in addition to single-dose PI may improve and prolong analgesia without interfering with early ambulation. Andersen et al[18] found that the combination of ACB and PI offered better pain relief than PI alone. In contrast, Perlas et al[21] did not find any difference in pain relief compared to PI alone. Whether ACB combined with PI offers superior analgesia and faster early postoperative recovery than PI alone after TKA still remains controversial. Thus, we conducted a meta-analysis to ascertain if combination of ACB and PI is superior to PI alone in reducing pain and morphine consumption in primary TKA.
2. Materials and methods
This meta-analysis was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines for the meta-analysis of intervention trials.[22] Ethical approval for this study was unnecessary because it was a review of existing literature and did not involve any handling of individual patient data.
2.1. Search strategy
PubMed, Medline, Embase, Web of Science, and the Cochrane Library were searched up to July 2016 for comparative studies involving combined ACB with PI and PI alone for reducing pain in patients undergoing TKA. Search terms were: “saphenous nerve block” OR “adductor canal block” OR “infrapatellar block” OR “subsartorial canal block” AND “periarticular infiltration” OR “local infiltration analgesia” OR “intraarticular infiltration” AND “total knee arthroplasty” OR “total knee replacement.” The language of publications was limited to English. The title and abstract of studies identified in the search were reviewed to exclude clearly irrelevant studies. Reference lists of all eligible studies and relevant reviews were searched manually for additional trials.
2.2. Inclusion criteria and study selection
We identified studies comparing combined ACB with PI and PI alone in patients undergoing primary TKA. The primary outcomes included pain score with rest or activity and distance walked. Secondary outcomes were morphine consumption, length of hospital stay, and postoperative complications. Articles that reported at least one outcome were included and those without the outcome measures of interest were excluded. Letters, comments, editorials, and practice guidelines were excluded.
2.3. Data extraction and quality assessment
Two authors independently reviewed all titles and abstracts of studies identified by searches according to the eligibility criteria described above. Full texts of articles that met the inclusion criteria were reviewed thoroughly. Disagreements were resolved by discussion to reach consensus. Data on patient characteristics (age, sex, and other baseline characteristics), intervention, and outcomes were extracted in duplicate by the 2 authors using a standardized form. Data in other forms (ie, median, interquartile range, and mean ± 95% confidence interval [CI]) were converted to mean ± standard deviation according to the Cochrane Handbook.[23] If data were not reported numerically, we extracted them by manual measurements from published figures. When necessary, we contacted the corresponding authors of the included studies to confirm that the information met our criteria.
Methodological quality of randomized control trials (RCTs) was assessed using a modified version of the Jadad Scale (0 [“very poor”] to 7 [“rigorous”]) was used to assess the methodological strength of a clinical trial. The modified Jadad Scale (mJS) contained 2-questions each on randomization and masking, and 1 question on the reporting of dropouts and withdrawals.[24] The Newcastle–Ottawa Quality Assessment Scale (NOQAS) was used for nonrandomized control trials (nRCTs). The NOQAS is used to assess population selection, comparability of exposed and unexposed, and adequacy of outcome assessment (including ascertainment and attrition of outcome).[25] Data extraction and quality assessment were undertaken independently by 2 of the authors. If there were disagreement, the 3rd author discussed until consensus was reached.
2.4. Statistical analysis
All calculations were made using RevMan v5.3. Mean difference (MD) with a 95% CI was calculated for continuous data. Odds ratios with 95% CI were calculated for dichotomous data. Heterogeneity among studies was estimated using the I2 statistic; substantial heterogeneity was represented by I2 > 50%. A fixed-effects model was used if the heterogeneity test did not reveal significance (I2 < 50%; P > 0.1). Otherwise, we adopted the random-effects model. P < 0.05 was considered significant. Sensitivity analysis was performed to explore the impact of an individual study by deleting 1 study each time.
3. Results
3.1. Search results
The initial search resulted in 63 articles, among which 57 had been identified as duplicated studies and excluded. By screening the titles and reading the abstracts and the full texts, 3 studies were excluded without meeting the inclusion criteria. Ultimately, we included 3 studies[18,21,26] with 337 patients for data extraction and meta-analysis (Fig. 1), with sample sizes ranging from 40 to 198. Of these 337 patients, there were 171 patients in the combined group and 166 patients in the PI alone group.
Figure 1.
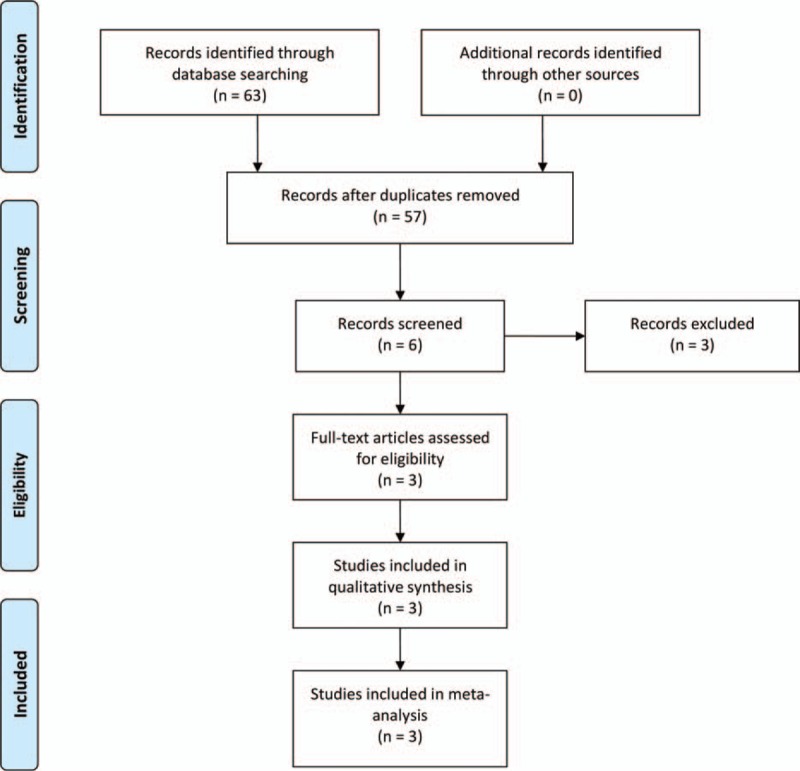
Flow chart of the literature search.
3.2. Study characteristics and quality assessment
The characteristics of the 3 involved studies are presented in Table 1. The publication dates of eligible studies ranged from 2013 to 2016. There were 2 RCTs[18,26] and 1 nRCT[21] in the included studies. All the researchers conducted were for unilateral primary TKA. In the included studies, subjects had similar demographic data in the 2 groups. All trials used spinal anesthesia. Spinal anesthesia was performed using hyperbaric bupivacaine 12.5 to 15 mg administered via the L3-4 or L2-3 vertebral interspaces in 1 trial;[18] another trial[26] used 2 mL of 0.5% bupivacaine with 0.1 mg preservative-free morphine for spinal anesthesia; all patients received a standard spinal anesthetic with 15 mg of bupivacaine and 100 μg of morphine injected at the L2-3 or L3-4 levels in one trial.[21] All studies involved the use of intraoperative PI. The variation of the contents and methods used in the PI was noted. For instance, in the study by Sawhney et al,[26] 20 mL of PI solution was injected into the posterior capsule and the medial and lateral ligaments just before implantation; after insertion of the implants, another 20 mL was infiltrated into the capsule and retinacular tissues; the remaining solution was used to infiltrate the muscle and subcutaneous tissues. In the study by Andersen et al[18] half of the PI solution was injected in the posterior joint capsule and along the meniscectomy line, and the other half was injected in the anterior joint capsule along the incision line before closure. The posterior capsule was infiltrated with PI solution before placement of the prosthesis, and the periarticular and superficial soft tissues were infiltrated after the prosthesis was in place and before wound closure in the study by Perlas et al.[21] The diversity of concomitant pain management among included studies was also noted. Outcomes of functional scores, rehabilitation, range of motion, cost, and postoperative quadriceps strength were not analyzed owing to insufficient data.
Table 1.
Characteristics of the included studies.
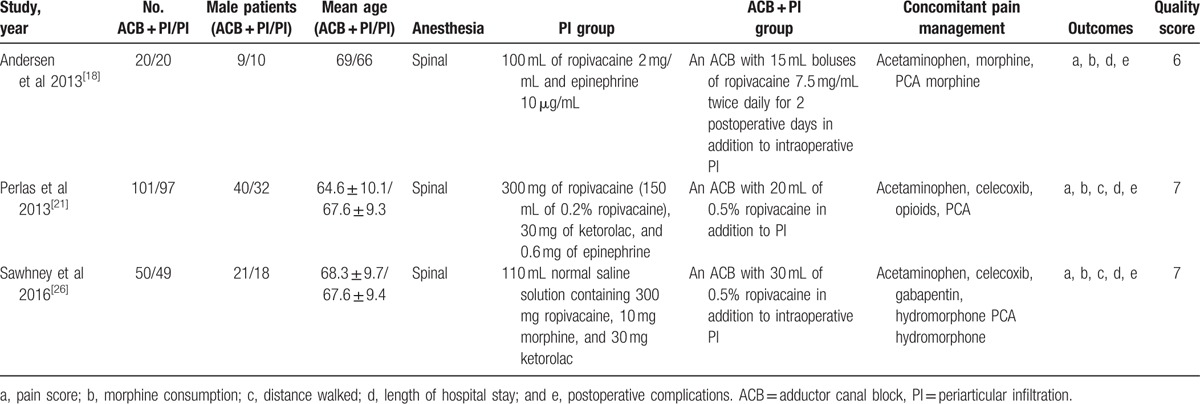
Total scores of the 2 RCTs[18,26] showed the quality of the 2 trials to be high (mJS scores = 6 and 7). According to the NOQAS, the remaining 1 study[21] scored 7 points (which denoted high quality) (Table 1).
3.3. Results of the meta-analysis
3.3.1. Numerical rating scale score
Data from 2 studies[18,21] on 238 patients were available to examine the pain score during rest on postoperative day (POD) 0. No significant difference was found between the ACB + PI and the PI groups (MD = −0.87, 95% CI: −2.92 to 1.19, P = 0.41; Fig. 2). Three studies[18,21,26] including 334 patients reported the pain score during rest on POD 1. The results were similar in the 2 groups (MD = 0.03, 95% CI: −0.53 to 0.59, P = 0.91; Fig. 2). Three studies[18,21,26] with 334 patients showed the pain score during rest on POD 2. The difference showed no statistical significance in the 2 groups (MD = 0.51, 95% CI: −0.02 to 1.03, P = 0.06; Fig. 2).
Figure 2.
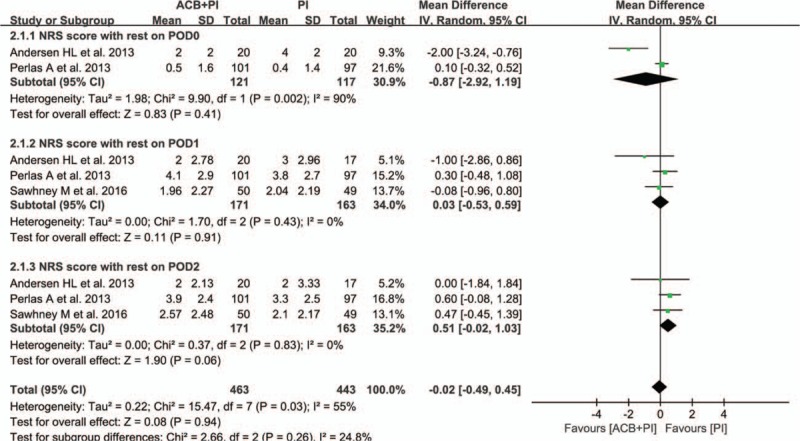
Forest plot analyses of NRS scores at rest within POD 2. NRS = numerical rating scale, POD = postoperative day.
Two studies[18,21] involving 238 patients reported the pain score during activity on POD 0, and no significant difference was found between the ACB + PI and the PI groups (MD = −1.12, 95% CI: −3.66 to 1.42, P = 0.39; Fig. 3). Three studies[18,21,26] with 334 patients showed the pain score during activity on POD 1. Meta-analysis revealed no significant differences between the 2 groups (MD = −0.61, 95% CI: −2.11 to 0.89, P = 0.43; Fig. 3). Three studies[18,21,26] including 334 patients reported the pain score during activity on POD 2. There were no significant differences between the 2 groups (MD = 0.06, 95% CI: −1.43 to 1.55, P = 0.94; Fig. 3).
Figure 3.
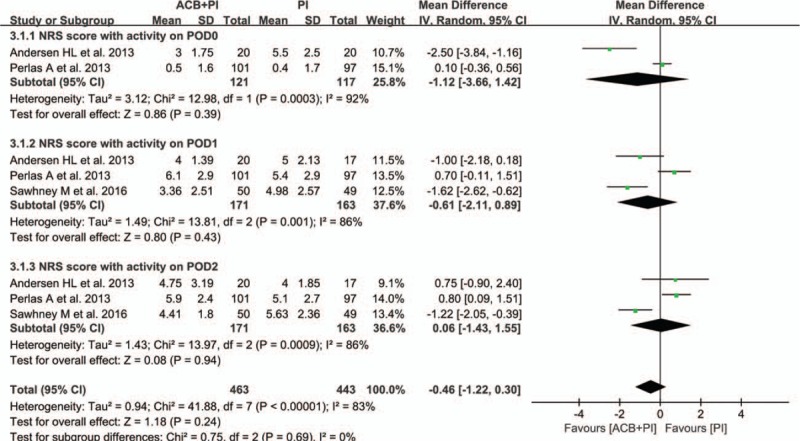
Forest plot analyses of NRS scores at activity within POD 2. NRS = numerical rating scale, POD = postoperative day.
3.3.2. Morphine consumption
Two studies[18,21] with 238 patients reported morphine consumption. There were no significant differences in morphine consumption between the ACB + PI and the PI groups on POD 0, POD 1, and POD 2 (MD POD 0 = −6.81, 95% CI:–19.06 to 5.44, P = 0.28; MD POD 1 = 1.86, 95% CI: −3.56 to 7.28, P = 0.50; MD POD 2 = 3.72, 95% CI: −0.27 to 7.71, P = 0.07) (Fig. 4).
Figure 4.
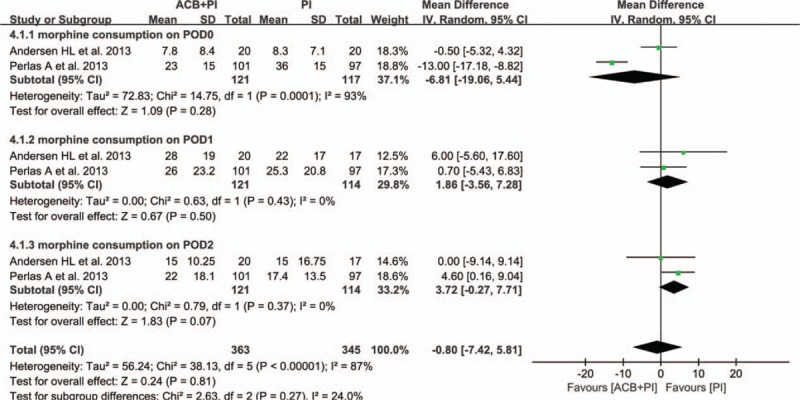
Forest plot analyses of morphine consumption within postoperative day (POD) 2.
3.3.3. Distance walked
Two studies[21,26] with 297 patients reported the early postoperative ambulation defined as the distance walked, measured in meters, on POD 1 and 2. The ACB + PI group was associated with longer distances walked than the PI group on POD 1 (MD = 7.27, 95% CI: 0.43 to 14.12, P = 0.04; Fig. 5). There were no significant differences in distance walked between the 2 groups on POD 2 (MD = 0.64, 95% CI:–5.67 to 6.96, P = 0.84; Fig. 5).
Figure 5.
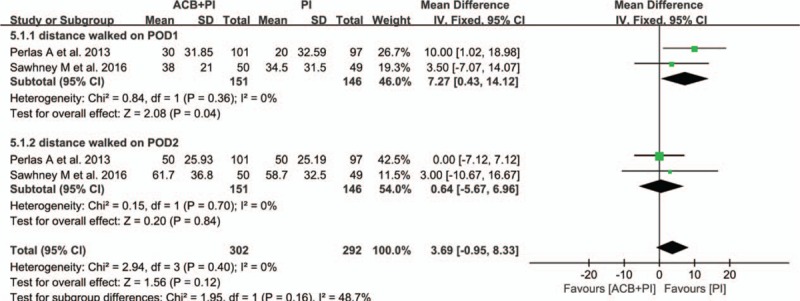
Forest plot analyses of distance walked within postoperative day (POD) 2.
3.3.4. Length of hospital stay
Data were available from 2 studies[18,21] involving 238 patients. There were no statistical differences in the length of hospital stay between the 2 groups (MD = −0.00, 95% CI: –0.19, 0.19, P = 1.00) (Fig. 6).
Figure 6.
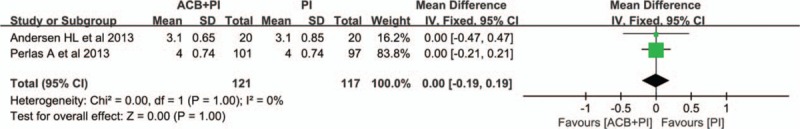
Forest plot analyses of length of hospital stay.
3.3.5. Complications
Three studies[18,21,26] including 337 patients described complications such as opioid-related adverse effects, local anesthetic systemic toxicity (LAST), and complications directly attributable to the nerve blocks. Total prevalence of complications showed no significant difference (RD = −0.01, 95% CI: −0.04 to 0.02, P = 0.69) between the ACB + PI and the PI groups (Fig. 7).
Figure 7.
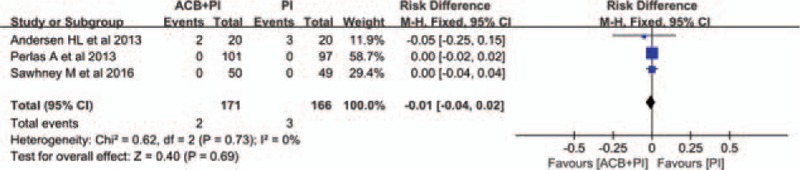
Forest plot analyses of postoperative complications.
4. Discussion
To our knowledge, this is the first meta-analysis to investigate the efficacy and safety of combined ACB with PI as compared to PI alone for pain management after TKA. We found that combined ACB with PI for patients undergoing TKA achieved earlier ambulation compared with PI alone in the early postoperative period. However, there was no significant difference in pain score, morphine consumption, and length of hospital stay between the 2 groups. Furthermore, combined ACB with PI did not increase the risk of opioid-related adverse effects, LAST, complications directly attributable to the nerve blocks, or other complications.
With respect to mobilization ability recovery, the meta-analysis showed that patients in the ACB + PI group promoted earlier postoperative ambulation than those in the PI group. This difference may be considered clinically relevant, given the desire for early and effective rehabilitation after TKA. Early ambulation within 24 hours after TKA has been shown to help increase range of motion, decrease deep venous thrombosis of the legs, enhance muscle strength and gait control, and reduce length of hospital stay.[27,28] Sawhney et al[26] performing a prospective RCT examining the effect of ACB with PI versus PI only and suggested that there was no difference between the groups regarding distance walked. PI has gained widespread acceptance and use because of its effectiveness in providing postoperative analgesia and promoting rehabilitation without quadriceps muscle strength weakness.[15–17,19] Nevertheless, the problem is that intraoperative LIA is only effective for the first 6 to 12 hours after TKA.[18,19] The adductor canal is an aponeurotic space in the thigh, extending from the apex of the femoral triangle to the adductor hiatus.[22] Most nerves in the adductor canal are sensory nerves dominating knee joints.[13] The ACB therefore seems to induce sensory anesthesia to the knee with potentially limited impact on motor function. Andersen et al[18] suggested that the ACB was effective as a rescue block when PI failed to control pain. Perlas et al[21] demonstrated that the addition of ACB to PI was associated with further improvement in early ambulation benchmarks and a higher rate of home discharge compared with PI alone. Besides, Andersen et al[18] conducted an RCT including 40 patients undergoing TKA (20 patients receiving ACB in addition to PI and 20 patients receiving PI) found that all patients in the ACB + PI group were able to ambulate on the day of surgery versus 13 patients in the PI group (P = 0.004). It appears that the addition of a selective ACB to PI is preferable to PI alone for early postoperative rehabilitation after TKA.
Regarding the pain control and morphine consumption, Sawhney et al[26] found that the combination of AC block and PI provided better pain relief and did not compromise ambulation compared with PI block only. The results of this trial are similar to the results reported in other trial by Andersen et al.[18] They detected that a saphenous nerve block at mid-thigh level, as a supplement to single-dose PI after TKA, significantly reduced pain scores during knee movement and at rest on the day of surgery compared with PI alone with no differences in morphine consumption. The possible reason for combined ACB with PI inducing more complete analgesic effect compared with using PI alone is that ACB combined with PI has the ability to provide local anesthetic to the anterior, medial, lateral, and posterior aspects of the knee.[26] However, our study failed to demonstrate any significant difference in pain control and morphine consumption between the ACB + PI and PI groups. Our findings were consistent with 1 recently published study that showed no significant difference in pain relief and morphine consumption between the ACB + PI and PI groups after TKA.[21] Thus, the combination of ACB and PI seems to allow for earlier rehabilitation exercise than PI alone with equivalent pain control.
The main concern regarding combined application of ACB and PI has been the incidence of LAST events in TKA. LAST is an uncommon complication associated with local infiltration analgesia in TKA but can be fatal if it develops into cardiac arrest.[29] In our meta-analysis, no significant differences were observed in the prevalence of postoperative complications including LAST between the ACB + PI and PI groups. Moreover, numerous studies[18,21,26] have shown that there were no documented cases of major or minor symptoms suggestive of LAST after TKA, and no changes in neurologic status, evidence of seizure activity, or evidence of cardiac toxicity were noted in any patient in their studies. However, they did not test plasma levels of local anesthetic to assess for the concentration of local anesthetic in the blood stream and thus cannot conclude there is no risk of LAST. Additional research on the safety of the 2 analgesic techniques including the risk of LAST needs to be conducted.
Our meta-analysis had 4 main limitations. First, we included only studies written in English, so some relevant studies in other languages may have been missed. Second, only 3 reports were included and the sample size of each study was small, which limited the statistical power of our meta-analysis. Third, the variation of the contents and doses of analgesics in ACB + PI and PI groups between studies may influence direct comparison between them. And the concomitant anesthesia methods were not entirely consistent among included studies, which presented challenges in evaluating the value of the intervention techniques alone. Fourth, we only assessed the participants in hospital without a long-term follow-up, which might underestimate the rates of some complications such as infection. Last, the functional outcome, range of motion, cost, and postoperative quadriceps strength measures could not be analyzed due to insufficient data. Therefore, high-quality and large-scale clinical trials and systemic reviews are needed to confirm these findings in the future.
5. Conclusions
Combined ACB with PI appeared to be associated with improved early ambulation without a reduction in analgesia compared with PI alone for pain management in patients undergoing TKA. No significant differences were seen in the morphine consumption, length of hospital stay, and postoperative complications between the 2 groups. However, due to the limitations in the included studies, more large-sample and high-quality clinical trials and systemic reviews are needed in the future to demonstrate the efficacy and safety of combined ACB with PI as compared to PI alone after TKA.
Acknowledgments
The authors thank the National Natural Science Foundation of China (81372013) and the Research Fund of China-Japan Friendship Hospital (2013-MS-27, 2014–4-QN-29); and China-Japan Friendship Hospital Youth Science and technology excellence project (2014-QNYC-A-06) for the support. The authors also thank all the participating patients of this study and the staff members of this trial, our colleagues, and all the study staff for their enormous efforts in collecting and ensuring the accuracy and completeness of all the data.
Footnotes
Abbreviations: ACB = adductor canal block, CI = confidence interval, EA = epidural analgesia, FNB = femoral nerve block, LAST = local anesthetic systemic toxicity, MD = mean difference, NOQAS = Newcastle–Ottawa Quality Assessment Scale, OA = osteoarthritis, PCA = patient-controlled analgesia, PI = periarticular infiltration, POD = postoperative day, RCT = randomized controlled trial, TKA = total knee arthroplasty.
JM and FG are joint first authors.
This study was supported by the National Natural Science Foundation of China (81372013) and the Research Fund of China-Japan Friendship Hospital (2013-MS-27, 2014-4-QN-29), and China-Japan Friendship Hospital Youth Science and technology excellence project (2014-QNYC-A-06).
The authors have no conflicts of interest to disclose.
References
- [1].Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 1999;91:8–15. [DOI] [PubMed] [Google Scholar]
- [2].Maheshwari AV, Blum YC, Shekhar L, et al. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res 2009;467:1418–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology 2014;120:540–50. [DOI] [PubMed] [Google Scholar]
- [4].Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am 2011;93:1075–84. [DOI] [PubMed] [Google Scholar]
- [5].Choi PT, Bhandari M, Scott J. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst Rev 2003;3:CD003071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fowler SJ, Symons J, Sabato S, et al. Epidural analgesia compared with peripheral nerve blockade after major knee surgery: a systematic review and meta-analysis of randomized trials. Br J Anaesth 2008;100:154–64. [DOI] [PubMed] [Google Scholar]
- [7].Paul JE, Arya A, Hurlburt L, et al. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology 2010;113:1144–62. [DOI] [PubMed] [Google Scholar]
- [8].Sharma S, Iorio R, Specht LM, et al. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res 2010;468:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lareau JM, Robbins CE, Talmo CT, et al. Complications of femoral nerve blockade in total knee arthroplasty and strategies to reduce patient risk. J Arthroplasty 2012;27:564–8. [DOI] [PubMed] [Google Scholar]
- [10].Jaeger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med 2013;38:526–32. [DOI] [PubMed] [Google Scholar]
- [11].Shah NA, Jain NP. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: a randomized controlled trial. J Arthroplasty 2014;29:2224–9. [DOI] [PubMed] [Google Scholar]
- [12].Memtsoudis SG, Yoo D, Stundner O, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop 2015;39:673–80. [DOI] [PubMed] [Google Scholar]
- [13].Gao F, Ma J, Sun W, et al. Adductor Canal Block Versus Femoral Nerve Block for Analgesia After Total Knee Arthroplasty: A Systematic Review and Meta-analysis. Clin J Pain 2016;DOI: 10.1097/AJP.0000000000000402. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [14].Li D, Ma GG. Analgesic efficacy and quadriceps strength of adductor canal block versus femoral nerve block following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2016;24:2614–9. [DOI] [PubMed] [Google Scholar]
- [15].Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop 2008;79:174–83. [DOI] [PubMed] [Google Scholar]
- [16].Busch CA, Shore BJ, Bhandari R, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am 2006;88:959–63. [DOI] [PubMed] [Google Scholar]
- [17].Toftdahl K, Nikolajsen L, Haraldsted V, et al. Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial. Acta Orthop 2007;78:172–9. [DOI] [PubMed] [Google Scholar]
- [18].Andersen HL, Gyrn J, Møller L, et al. Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty. Reg Anesth Pain Med 2013;38:106–11. [DOI] [PubMed] [Google Scholar]
- [19].Kehlet H, Andersen LØ. Local infiltration analgesia in joint replacement: the evidence and recommendations for clinical practice. Acta Anaesthesiol Scand 2011;55:778–84. [DOI] [PubMed] [Google Scholar]
- [20].Reeves M, Skinner MW. Continuous intra-articular infusion of ropivacaine after unilateral total knee arthroplasty. Anaesth Intensive Care 2009;37:918–22. [DOI] [PubMed] [Google Scholar]
- [21].Perlas A, Kirkham KR, Billing R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med 2013;38:334–9. [DOI] [PubMed] [Google Scholar]
- [22].Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;10:1006–12. [DOI] [PubMed] [Google Scholar]
- [23].Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane collaboration; 2011. [http://www. cochrane-handbook.org] Accessed March 20, 2011. [Google Scholar]
- [24].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [25].Wells GA, O’Connell SB, Peterson D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; 2013. http://www.ohri.ca/Programs/clinical epidemiology/oxford.asp [Accessed January, 27]. [Google Scholar]
- [26].Sawhney M, Mehdian H, Kashin B, et al. Pain after unilateral total knee arthroplasty: a prospective randomized controlled trial examining the analgesic effectiveness of a combined adductor canal peripheral nerve block with periarticular infiltration versus adductor canal nerve block alone versus periarticular infiltration alone. Anesth Analg 2016;122:2040–6. [DOI] [PubMed] [Google Scholar]
- [27].Labraca NS, Castro-Sanchez AM, Mataran-Penarrocha GA, et al. Benefits of starting rehabilitation within 24 hours of primary total knee arthroplasty: randomized clinical trial. Clin Rehabil 2011;25:557–66. [DOI] [PubMed] [Google Scholar]
- [28].Pearse EO, Caldwell BF, Lockwood RJ, et al. Early mobilisation after conventional knee replacement may reduce the risk of postoperative venous thromboembolism. J Bone Joint Surg Br 2007;89:316–22. [DOI] [PubMed] [Google Scholar]
- [29].Tomita A, Satani M, Suzuki K, et al. A case of cardiac arrest following intra-articular administration of levobupivacaine during total knee arthroplasty. Masui 2016;65:179–83. [PubMed] [Google Scholar]


