Abstract
Background:
A femoral nerve block (FNB) in combination with a sciatic nerve block (SNB) is commonly used for anesthesia and analgesia in patients undergoing hindfoot and ankle surgery. The effects of FNB on motor function, related fall risk, and rehabilitation are controversial. An adductor canal block (ACB) potentially spares motor fibers in the femoral nerve, but the comparative effect on hindfoot and ankle surgeries between the 2 approaches is not yet well defined. We hypothesized that compared to FNB, ACB would cause less weakness in the quadriceps and produce similar pain scores during and after the operation.
Methods:
Sixty patients scheduled for hindfoot and ankle surgeries (arthroscopy, Achilles tendon surgery, or medial ankle surgery) were stratified randomized for each surgery to receive an FNB (FNB group) or an ACB (ACB group) combined with an SNB. The primary outcome was the visual analog scale (VAS) pain score at each stage. Secondary outcomes included quadriceps strength, time profiles (duration of the block procedure, time to full anesthesia and time to full recovery), patients’ analgesic requirements, satisfaction, and complications related to peripheral nerve blocks such as falls, neurologic symptoms, and local anesthetic systemic toxicity were evaluated. The primary outcome was tested for the noninferiority of ACB to FNB, and the other outcomes were tested for the superiority of each variable between the groups.
Results:
A total of 31 patients received an ACB and 29 received an FNB. The VAS pain scores of the ACB group were not inferior during and after the operation compared to those of the FNB group. At 30 minutes and 2 hours after anesthesia, patients who received an ACB had significantly higher average dynamometer readings than those who received a FNB (34.2 ± 20.4 and 30.4 ± 23.7 vs 1.7 ± 3.7 and 2.3 ± 7.4, respectively), and the results were similar at 24 and 48 hours after anesthesia. There were no differences between the 2 groups with regard to time profiles and patient satisfaction. No complications were noted.
Conclusion:
ACB preserved quadriceps muscle strength better than FNB, without a significant difference in postoperative pain. Therefore, ACB may be a good alternative to FNB for reducing the potential fall risk.
Keywords: adductor canal block, femoral nerve block, foot and ankle surgery
1. Introduction
The use of regional anesthesia has gained popularity because of its positive effects on patient comfort and safety.[1,2] Most foot and ankle operations are performed on an outpatient basis, often under some form of regional anesthesia. The use of this type of anesthesia is supported by successful outcomes reported in the literature.[3–5] Ankle block and sciatic nerve block (SNB) are 2 of the most popular anesthetic techniques used in foot and ankle surgery. Both have been shown to be safe and effective for these surgical procedures.[6,7]
Blockade of the saphenous nerve is essential for surgeries that involve the medial aspect of the foot or ankle, for which a regional technique is preferred.[8–10] Numerous approaches to saphenous nerve blockade have been described using landmarks, nerve stimulation, and ultrasound.[11–13] Although a saphenous nerve block is appropriate for anesthesia and analgesia for hindfoot and ankle surgery, a more proximal block for the medial side of the hindfoot and ankle is necessary when the tourniquet is applied to the distal thigh for surgery. Recently, a study showed that femoral nerve block (FNB) provides good surgical anesthesia and good postoperative pain control for patients with hindfoot and ankle conditions.[3] However, FNB leads to femoral quadriceps muscle weakness.[14,15] Consequently, quadriceps weakness results in functional impairment and it is associated with an increased risk of postoperative falls.[16–18] Thus far, attempts to reduce quadriceps involvement after FNB without compromising analgesia have not been successful.[15,19]
Partially because of the increase in the use of ultrasound guidance, a more targeted approach that only blocks sensory fibers of the femoral nerve that supply the operative site has been attempted; thus, the feasibility of adductor canal block (ACB) has been studied.[20,21] In recent years, ACB has been successfully used for postoperative pain control after knee surgery.[22,23]
However, no randomized, control study has compared ACB to FNB for hindfoot and ankle surgeries. We hypothesized that compared to FNB, ACB would demonstrate noninferior pain scores during surgery and until 48 hours postoperatively and cause less weakness in the quadriceps.
2. Methods
This prospective, randomized noninferiority trial was performed at Ajou University Hospital, Suwon, Republic of Korea between August 2015 and May 2016, and it was approved by our institutional ethics committee (approval no. AJIRB-MED-MDB-15-181). The study design was also prospectively registered (http://cris.nih.go.kr, kct0001624/).
After obtaining written informed consent, we enrolled 60 adult patients who were scheduled to undergo surgery on the hindfoot, medial side of the ankle, or both sides of the ankle (Achilles tendon surgery, the removal of an implanted device on the medial side, or ankle arthroscopy) under peripheral nerve blocks (PNBs); had an American Society of Anesthesiologists Physical status of I to II; and were aged 19 to 65 years. Exclusion criteria were an inability to cooperate; a history of alcohol or drug abuse; those with rheumatoid arthritis, coagulation disorders, peripheral neuropathy, and known allergies to local anesthetics; and the recent use of opioids, corticosteroids, or any other analgesics. If a patient complained of incomplete block before the end of surgery, we excluded the patient from the analysis.
Randomization was based on a computer-generated block randomization list (4 numbers per block) in a 1:1 ratio. All patients underwent SNB, and ACB (ACB group), or FNB (FNB group) according to a randomized assignment.
3. Anesthesia and postoperative analgesia
All patients were anesthetized with PNBs for surgery. PNBs were performed in a block room at least 1 hour preoperatively. All PNBs were performed under ultrasound guidance (LOGIQ P6, GE Healthcare; Chicago, IL) using a high-frequency linear transducer (3.4–10.8 MHz). All blocks were performed after skin preparation with 2% chlorhexidine gluconate by 1 orthopedic surgeon (YUP) with vast experience in ultrasound-guided nerve block techniques. A 22-ga Tuohy needle was introduced in-plane and 2 to 3 mL of saline was used to confirm the correct position of the needle tip near the target nerve. The study medication was administered through the needle as a bolus of 15 mL of a 1:1 mixed solution of ropivacaine 0.75% and lidocaine 1%.
For the SNB, the patient was placed in the supine position with the knee of the affected limb flexed at about 30°. SNB was performed immediately proximal to the bifurcation of the sciatic nerve into the tibial and common peroneal nerves. The needle was advanced until the needle tip was positioned at the anterior and posterior external surface of the sciatic nerve in the anterior–posterior plane and at the midpoint of the sciatic nerve in the mediolateral plane. The needle-tip position was adjusted as necessary to ensure the circumferential spread of study medication around the sciatic nerve.
For the ACB, the patient was placed in the supine position with the extremity to be blocked slightly externally rotated. The ultrasound transducer was placed in a transverse cross-sectional view at the midpoint of the inguinal crease and the medial femoral condyle on the medial thigh. The femoral artery and the saphenous nerve just lateral to the artery were identified underneath the sartorius muscle. After the needle tip was placed just lateral to the artery and saphenous nerve, the study medication was injected.
For the FNB, the femoral nerve was identified lateral to the femoral artery at the inguinal crease in the transverse section. The study medication was injected anterior and posterior to the nerve.
The actual or estimated needle insertion sites of ACB and FNB were covered with a dressing bandage in all patients to blind those assessing the outcome of the procedure to the treatment.
Intravenous ketorolac tromethamine (30 mg, maximum dose 90 mg/d) was given as a rescue analgesic during the first 48 hours postoperatively when a patient reported a visual analog scale (VAS) score of ≥5 or if the patient requested pain relief.
4. Assessment
The primary (noninferiority) outcome was the VAS pain score at each stage. All patients were educated preoperatively regarding the use of a 10-cm VAS pain score (0 cm, no pain; 10 cm, worst pain). VAS pain scores were evaluated during the anesthetic procedure; during surgery; immediately postoperatively; and at 2, 12, 24, and 48 hours postoperatively. Tourniquet pain during the operation was evaluated separately.
The secondary (superiority) comparative outcomes included motor strength of the quadriceps muscle, time profiles (i.e., the duration of the procedure, time to full anesthesia, recovery time, and operative time), postoperative analgesic requirements, patient satisfaction, and the incidence of complications.
The quadriceps strength was assessed as the maximum voluntary isometric contraction at 30 minutes, 2 hours, 24 hours, and 48 hours postoperatively compared to baseline (preoperatively). We used a handheld dynamometer (HHD; microFET2, Hoggan Industries; Salt Lake City, UT) to measure muscle strength. The HHD is a reliable and valid instrument, and we used standardized, recommended procedures to obtain valid measurements.[14,21] To evaluate the quadriceps muscle strength, we placed the patient in a seated position with the knees flexed 60°. We used a nonelastic strap with Velcro closures to fix the HHD to the leg. We attached the Velcro strap to a chair and around the patient's ankle, perpendicular to the lower leg. The HHD was placed under the Velcro strap on the anterior surface of the tibia (5 cm above the transmalleolar axis). We instructed the patient to take 3 seconds to reach and maintain maximum effort, and then relax. For each assessment, the patient performed 3 consecutive contractions, separated by a 30-second pause between each trial. We used the mean value at each time point to calculate muscle strength.
The duration of the procedure was defined as the time interval from needle insertion to pull out. Time to full anesthesia was defined when a patient verbally responded “no” when asked if cutaneous pressure or a pinprick was being applied to the area in question. The recovery time (time elapsed between the onset of anesthesia and full motor and sensory recovery) was also documented.
Additional data collected included the following: the numbers and proportions of patients requiring a rescue analgesic during the first 48 hours; patient satisfaction (each patient was interviewed using a scale of 1 to 5 (5 being the most satisfied) at 48 hours postoperatively); and the incidence of complications related to a PNB (if any), including falls, neurologic symptoms, and local anesthetic toxicity.
5. Statistical analysis
The sample size determination was based on a recently completed trial[3] at our institution evaluating anesthetic and analgesic effects of sciatic and FNBs in the hindfoot and ankle surgeries involving the medial side of ankle. We chose a noninferior design to demonstrate that ACB was not inferior to FNB as an anesthetic and analgesic technique while demonstrating the superiority of preservation of quadriceps motor strength after ACB compared to FNB. The sample size was determined by assuming a standard deviation of 1.47 cm and an upper end confidence limit of 1 cm. We calculated a sample size of 27 patients in each group with a predicted 10% dropout rate, totaling 60 patients. This would permit a type-1 error rate of 0.05, with a type-2 error rate of 0.20.
Data were analyzed using SPSS version 13.0 (SPSS Inc.; Chicago, IL). Data are presented as the mean ± standard deviation, median (interquartile range), or the number (percentage) of patients. For the primary outcome variable, the noninferiority of ACB versus FNB was demonstrated if the upper 95% confidence interval limit of the difference between the groups excluded the defined noninferiority margin of 1 cm. We compared secondary outcomes using a t test for parametric variables, a Mann–Whitney U test for nonparametric variables, and either a chi-square or Fisher exact test for categorical data. A P value <0.05 was considered statistically significant.
6. Results
We enrolled 60 patients during a 12-month period beginning in June 2015. Patients were randomized to receive either ACB (N = 31) or FNB (N = 29) (Table 1). The PNBs used in this study were the sole anesthetic techniques used for hindfoot and ankle surgery in 59 patients. One patient in the FNB group complained of incomplete block; therefore, this patient received general anesthesia. Surgical procedures performed in this study were arthroscopy (N = 32), Achilles tendon surgery (N = 9), and medial ankle surgery (medial malleolar old fracture, N = 19).
Table 1.
Patients’ demographic characteristics.

The VAS pain scores were comparable between the 2 groups (Table 2). The upper confidence limits of VAS pain scores were less than the δ at every stage, except the block procedure. Therefore, the ACB was not inferior to the FNB with regard to the pain score during and after hindfoot and ankle surgery.
Table 2.
VAS pain scores over time.

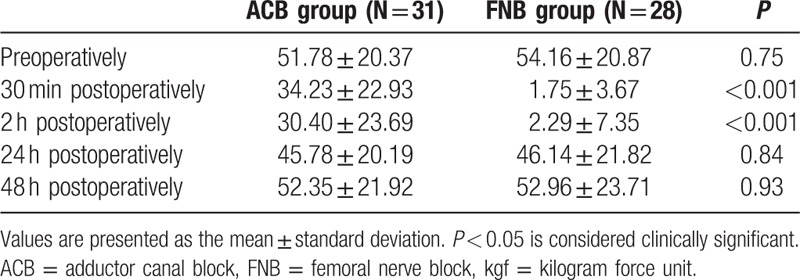
Table 3 presents data for the motor strength of the quadriceps muscle over time. We compared dynamometer readings between the groups at each time point. At 30 minutes and 2 hours postoperatively, the mean strength during extension of the knee was significantly higher in the ACB group than in the FNB group (ACB/FNB: 34.23 ± 22.93 vs 1.75 ± 3.67 at 30 minutes postoperatively and 30.40 ± 23.69 vs 2.29 ± 7.35, respectively) (P < 0.001). At 24 and 48 hours, there was no significant difference between the ACB and FNB groups, P values = 0.84 and 0.93, respectively.
Table 3.
Motor strength (kgf) of the quadriceps muscle over time.
The time profiles (duration of the procedure, time to full anesthesia, operative time, and recovery time) were not different between the 2 groups (Table 4).
Table 4.
Time profiles of the 2 groups.

The numbers and proportions of patients requiring a rescue analgesic during the first 48 hours were not different between the 2 groups (Table 5).
Table 5.
Number of patients requiring analgesic rescue in the first 48 hours after surgery.

Eleven patients were very satisfied, 41 were satisfied, and 6 were fairly satisfied, and no patients were unsatisfied. Patient satisfaction was similar for both types of nerve blocks (P = 0.80). Eight patients complained of temporary numbness in their operated leg 24 hours postoperatively (ACB: 3, FNB: 5, P = 0.46). However, their symptoms completely recovered without specific management.
7. Discussion
This prospective study demonstrated that ACB is an effective alternative to FNB for patients undergoing hindfoot and ankle surgery. The most important finding of this study was that ACB significantly spared quadriceps strength at 30 minutes to 2 hours postsurgery, and it was not inferior to FNB in terms of pain scores, analgesic requirements, and time profiles.
For intraoperative anesthesia or postoperative pain control after hindfoot and ankle surgery, a popliteal SNB is an effective method when the surgery does not involve the medial side of the hindfoot and ankle.[6,7,9] When the surgery involves the medial side of the hindfoot and ankle, the saphenous nerve should be blocked to ensure proper anesthesia or analgesia in combination with an SNB. Although FNB can be used for the saphenous nerve block,[3,24] ACB or a saphenous nerve block instead of an FNB is sufficient anesthesia or analgesia for hindfoot and ankle surgery. Several studies have already validated ACB as an effective analgesic method compared to an FNB, as it spares quadriceps muscle strength, but most studies have investigated arthroscopic knee surgery or total knee replacement.[25–27] This advantage of ACB over FNB was also demonstrated beyond knee surgery in our study, which is the first study to directly compare multiple outcomes of ACB versus FNB in patients undergoing hindfoot and ankle surgery.
The noninferiority of VAS pain scores after hindfoot and ankle surgery with ACB compared to FNB is not surprising, because an ACB and FNB can effectively block the saphenous nerve, which innervates the medial side of the hindfoot and ankle. Although the saphenous nerve block instead of an ACB can provide sufficient anesthesia and analgesia for hindfoot and ankle surgery, we performed an ACB because we applied a tourniquet on the lower thigh during the surgery. To reduce tourniquet-related discomfort, we think that an ACB rather than the saphenous nerve block is appropriate, because an ACB performed at the level of the mid-thigh involves the saphenous nerve and several other sensory nerves that innervate the medial, lateral, and anterior aspects of the knee, encompassing the superior pole of the patella to the proximal tibia.[26] In the present study, all patients in both groups tolerated tourniquet-related discomfort well, and there was no difference in tourniquet-related pain between the 2 groups.
Our results showed that the mean strength during extension of the knee was significantly higher for the ACB compared to the FNB group at 30 minutes and 2 hours postoperatively, and the strength became similar between the 2 groups at 24 and 48 hours. This result is similar to that reported in other studies.[15,26] Jaeger et al[15] reported that motor strength was reduced by a mean of 49% with FNB (vs 8% with ACB) compared to baseline. Kim et al[26] reported a steeper decrease in motor strength after FNB, 81.5% after FNB and 53.2% after ACB compared to baseline. In the present study, the mean reduction of quadriceps strength from baseline was 95.8% 2 hours after FNB and 41.3% 2 hours after ACB. The relatively low motor strength in our findings compared to those of other studies is most likely due to the concentration and dose of local anesthetic solution used.
No postoperative falls were noted in this study. However, given the small sample size (N = 59), we cannot draw conclusions about a risk reduction of falls. Other secondary outcomes such as patient satisfaction, time profiles, and complications related to PNB were not significantly different between the groups. This can be attributed to the ACB providing analgesia that is not different from that of an FNB.
Our study has several limitations. First, patients and the investigator who performed the nerve blocks were not blinded to the treatment. We did not find it appropriate to perform 2 invasive procedures in each patient. Instead, a dressing covered the actual or estimated needle insertion site of ACB and FNB for all patients, with the purpose of blinding those assessing the outcome to the procedure. Second, our observation period was limited to 48 hours postoperatively, and we could not account for conclusions and potential complications detected thereafter. However, we are not aware of any untoward events associated with the use of either type of block in any of our patients. Finally, our data should be interpreted in the context of 3 kinds of hindfoot and ankle surgeries (arthroscopy, Achilles tendon surgery, and medial ankle surgery) involving the medial side of the ankle, and the use of our techniques may be different depending on the kind of surgery.
In conclusion, we found that the use of ACB compared to FNB for hindfoot and ankle surgery yielded similar results in pain scores, time profiles, and patient satisfaction with preserving quadriceps muscle strength better than FNB at 30 minutes to 2 hours postoperatively. Thus, ACB may represent a good alternative anesthetic and analgesic technique to FNB for reducing the potential fall risk in hindfoot and ankle surgery.
Footnotes
Abbreviations: ACB = adductor canal block, FNB = femoral nerve block, HHD = handheld dynamometer, PNB = peripheral nerve block, SNB = sciatic nerve block, VAS = visual analog scale.
Funding/support: This study was supported by the new faculty research fund of Ajou University School of Medicine (M-2015-c0460-00079).
The authors have no conflicts of interest to disclose.
References
- [1].Feely NM, Popat MT, Rutter SV. Regional anaesthesia for limb surgery: a review of anaesthetists’ beliefs and practice in the Oxford region. Anaesthesia 2008;63:621–5. [DOI] [PubMed] [Google Scholar]
- [2].Pearce CJ, Hamilton PD. Current concepts review: regional anesthesia for foot and ankle surgery. Foot Ankle Int 2010;31:732–9. [DOI] [PubMed] [Google Scholar]
- [3].Lee KT, Park YU, Jegal H, et al. Femoral and sciatic nerve block for hindfoot and ankle surgery. J Orthop Sci 2014;19:546–51. [DOI] [PubMed] [Google Scholar]
- [4].Myerson MS, Ruland CM, Allon SM. Regional anesthesia for foot and ankle surgery. Foot Ankle 1992;13:282–8. [DOI] [PubMed] [Google Scholar]
- [5].Sarrafian SK, Ibrahim IN, Breihan JH. Ankle-foot peripheral nerve block for mid and forefoot surgery. Foot Ankle 1983;4:86–90. [DOI] [PubMed] [Google Scholar]
- [6].Monso A, Santaliestra J, Barbal F, et al. Sciatic nerve block at the popliteal fossa for foot surgery. Rev Esp Anestesiol Reanim 1996;43:27–9. [PubMed] [Google Scholar]
- [7].Rongstad K, Mann RA, Prieskorn D, et al. Popliteal sciatic nerve block for postoperative analgesia. Foot Ankle Int 1996;17:378–82. [DOI] [PubMed] [Google Scholar]
- [8].Blumenthal S, Borgeat A, Neudorfer C, et al. Additional femoral catheter in combination with popliteal catheter for analgesia after major ankle surgery. Br J Anaesth 2011;106:387–93. [DOI] [PubMed] [Google Scholar]
- [9].Hansen E, Eshelman MR, Cracchiolo A., 3rd Popliteal fossa neural blockade as the sole anesthetic technique for outpatient foot and ankle surgery. Foot Ankle Int 2000;21:38–44. [DOI] [PubMed] [Google Scholar]
- [10].Chen J, Lesser J, Hadzic A, et al. The importance of the proximal saphenous nerve block for foot and ankle surgery. Reg Anesth Pain Med 2013;38:372. [DOI] [PubMed] [Google Scholar]
- [11].De Mey JC, Deruyck LJ, Cammu G, et al. A paravenous approach for the saphenous nerve block. Reg Anesth Pain Med 2001;26:504–6. [DOI] [PubMed] [Google Scholar]
- [12].Comfort VK, Lang SA, Yip SW. Saphenous nerve anaesthesia (a nerve stimulator technique. Can J Anaesth 1996;43:852–7. [DOI] [PubMed] [Google Scholar]
- [13].Gray AT, Collins AB. Ultrasound guided saphenous nerve block. Reg Anesth Pain Med 2003;28:148. [DOI] [PubMed] [Google Scholar]
- [14].Charous MT, Madison SJ, Suresh PJ, et al. Continuous femoral nerve blocks varying local anesthetic delivery method (bolus versus basal) to minimize quadriceps motor block while maintaining sensory block. Anesthesiology 2011;115:774–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Jaeger P, Nielsen ZJ, Henningsen MH, et al. Adductor canal block versus femoral nerve block and quadriceps strength: a randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology 2013;118:409–15. [DOI] [PubMed] [Google Scholar]
- [16].Ilfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg 2010;111:1552–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Johnson R, Kopp SL, Hebl JR, et al. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth 2013;110:518–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Muraskin SI, Conrad B, Zheng N, et al. Falls associated with lower-extremity–nerve blocks: a pilot investigation of mechanisms. Reg Anesth Pain Med 2007;32:67–72. [DOI] [PubMed] [Google Scholar]
- [19].Charous MT, Madison SJ, Suresh PJ, et al. Continuous femoral nerve blocks: varying local anesthetic delivery method (bolus versus basal) to minimize quadriceps motor block while maintaining sensory block. Anesthesiology 2011;115:774–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Horn JL, Pitsch T, Salinas F, et al. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med 2009;34:486–9. [DOI] [PubMed] [Google Scholar]
- [21].Manickam B, Perlas A, Duggan E, et al. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med 2009;34:578–80. [DOI] [PubMed] [Google Scholar]
- [22].Jaeger P, Grevstad U, Henningsen MH, et al. Effect of adductor-canal-blockade on established, severe post-operative pain after total knee arthroplasty: a randomised study. Acta Anaesthesiol Scand 2012;56:1013–9. [DOI] [PubMed] [Google Scholar]
- [23].Jenstrup MT, Jæger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012;56:357–64. [DOI] [PubMed] [Google Scholar]
- [24].Szucs S, Morau D, Iohom G. Femoral nerve blockade. Med Ultrason 2010;12:139–44. [PubMed] [Google Scholar]
- [25].Grevstad U, Mathiesen O, Valentiner LS, et al. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg Anesth Pain Med 2015;40:3–10. [DOI] [PubMed] [Google Scholar]
- [26].Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology 2014;120:540–50. [DOI] [PubMed] [Google Scholar]
- [27].Memtsoudis SG, Yoo D, Stundner O, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop 2015;39:673–80. [DOI] [PubMed] [Google Scholar]


