Abstract
Background
This study assessed the current state of knowledge regarding the use of the integrated electronic health record (EHR) patient portal on pediatric clinical care. A systematic examination of the research on implementation, utilization, and evaluation of the integrated EHR patient portal among pediatric patients has not been previously conducted. Therefore, the purpose of the present study was to systematically review existing research on the state of the science, describe the way others have defined the patient portal, and examine pediatric patient portal utilization.
Materials and Methods
Covering a period from 1992 to 2014 a literature search was conducted on four electronic databases. Only articles in English were reviewed. Studies were included if they reported the use of a patient portal integrated with an electronic health record and captured pediatric medial encounters. Qualitative or quantitative studies of any design were eligible as long as they focused on patients (or parents) who access their health records through an electronic portal tied to an EHR and reported measures of satisfaction, attitudes on use, barriers and facilitators, adherence, or clinical and health outcomes. Content analysis of each article was performed independently by at least two authors using an extraction grid of study qualities, and quality and relevance of the studies were also assessed.
Results
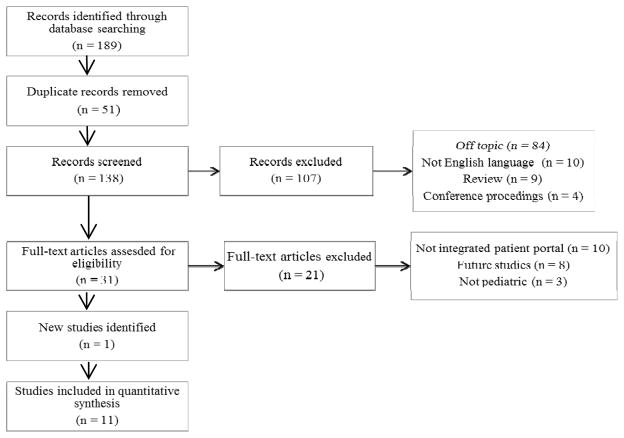
Of a total of 189 potentially relevant publications identified, 31 full-text publications were obtained after screening titles and abstracts. After a full review, 11 publications corresponding to seven studies met the inclusion criteria. The methodological approaches included cross-sectional surveys, retrospective analysis, qualitative studies, and usability testing. In general, feedback was positive. The most frequent negative comments about the portal reflected concern about teenager interaction with the portal and how that might affect communication among patient, parent, and provider. Some users were frustrated with the complexity of medical terminology used.
Conclusions
Reflecting the additional considerations of pediatric proxy access and fewer chronically ill patients, pediatric medicine has yet to use patient portal as a modality for outcomes measurement. Given the paucity of studies within this age group, it is difficult to measure outcome improvements or the effect of patient record access on healthcare behaviors. This systematic review presents innovative research on the general acceptance of the patient portal among parents and highlights that the implementation of the portal is still in its early stages and has yet to be used widely in diverse populations or studies in a longitudinal manner. Further studies should confirm that protected access to health information and secure communication and information sharing with healthcare providers have an impact in the pediatric population on healthcare outcomes.
Keywords: adolescent, electronic health record, electronic patient portal, electronic medical record, pediatrics
Introduction
Improvements in the healthcare system will require greater engagement of patients and their caregivers with the system. Shared decision-making involves participation by both patients and clinicians to share treatment preferences, to set goals, and to make joint determination of the treatment plan.1
One of the engagement modalities is the patient portal. Patient portal is a general term used to describe a variety of health information access modalities, including internet sites, interactive internet-based programs, and sites to enter personal health data.2,3 The term patient portal is not used uniformly to indicate that it is integrated with the electronic health record (EHR). For the purposes of this study, patient portal will refer specifically to a secure web site, integrated with the EHR, through which patient can complete forms, communicate electronically with healthcare providers, access personal health information such as progress notes, problem lists, current medications, immunization history, laboratory data, and radiology reports, schedule appointments, request prescription refills, and pay bills.4,5 The American Medical Informatics Association’s College of Medical Informatics concluded that integrated personal health records offer more benefits.6
Development of the patient portal has been driven in part by believe that systems will enhance patient satisfaction, improve care, and make care more efficient.7 Cross-sectional studies have demonstrated that people pay more attention and become more engaged in their health and medical care when they have easy access to their health information online and become participating members of the healthcare team rather than passive recipients of care.4,8
While patient portals are increasingly common, there is little information regarding their use as a communication tool to connect patients, caregivers, and healthcare team as partners, especially in the pediatric population.4,7,9 The communication functionality is of concern since the EHR was not specifically designed and programmed initially to be a patient educational or patient involvement tool, and there are concerns that patients will see something in their record that providers never anticipated, or they might become anxious when seeing unfiltered data. Within the pediatric population there is an additional challenge of children maturing and of constructing the correct data feeds that ensure easy and appropriate access while maintaining confidentiality and privacy for both adolescent patients and their parents.5,6,10
Parents of children with chronic conditions, who use multiple healthcare systems and providers, have identified the underutilization of the patient portal within the pediatric population. Parents expressed their desire to have one point of contact to manage their child’s health condition and a one-stop electronic location for scheduling, calendars, and communication with providers. They have suggested that increased use of the portal for chronically ill children might be a tool to help alleviate some of their caregiver stresses, as well as a potential modality that helps teenagers manage chronic illness.11 Additionally, adolescents with chronic disease must develop independent disease self-management and learn to communicate with their healthcare team to transition from pediatric to adult-oriented healthcare systems.12
As health information exchanges help facilitate data sharing such as test results and clinical notes across healthcare systems through the use of data meeting nationally recognized standards for interoperability, privacy, and data security, they may work in concert with patient portals. Such broad data sharing could be very beneficial not only as paediatric patients age into adults, but also when they receive care within multiple healthcare systems, and improve the quality and efficacy of healthcare.13,14
The purpose of this systematic review is to understand the state of the science of pediatric patient portal utilization, including to describe the ways in which authors have described the implementation of the patient portal, the ways in which it is integrated in the EHR, and the methodology adopted to measure the impact of the portal. These findings will help to identify gaps in the literature and to develop recommendations for future research.
Methods
The approaches used in this systematic review were informed by guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).15
SEARCH STRATEGY
We conducted a comprehensive search of four online databases (PubMed, CINAHL Plus PsycINFO, and Academic Search Premier) for peer-reviewed literature published between 1992 and August 2014 (see Table 1 for search queries). Assisted by a librarian, we searched for literature on both electronic patient portals and electronic personal health records, including both terms since they are often used interchangeably in the literature.
Table 1.
Search terms
| Terms |
|---|
| Patient portal (and pediatric or adolescent) |
| Patient portals (and pediatric or adolescent) |
| Electronic patient portal (and pediatric or adolescent) |
| Electronic medical record patient portal (and pediatric or adolescent) |
| Online patient portal (and pediatric or adolescent) |
| Patient portal communication (and pediatric or adolescent) |
| Patient portal usage (and pediatric or adolescent) |
| Care partners and online patient portal (and pediatric or adolescent) |
| Patient portal communication (and pediatric or adolescent) |
The selection of articles is outlined in Figure 1. Each search provided citations and abstracts that were downloaded and subsequently imported into an Access database. After duplicated citations were removed, we identified a total of 138 unique references. One reviewer [R.A.B.] scanned the title and abstract (if available) of each unique reference for inclusion using the following criteria: human subjects only; peer-reviewed; published journal articles (no posters, conference proceedings, or dissertation); printed in the English language; and included some original research and data analysis (no review articles or commentary) on patient portals with some use in the 0–18-year-old age group. During our initial search we did not have any publication date restrictions for a more comprehensive search. In the second round four reviewers reviewed the full text of the 31 documents (seven or eight per reviewer) to determine final eligibility based on inclusion criteria. One discrepancy was resolved through discussion, and exclusion reasons were documented. While screening the articles, one additional paper was identified using the reference lists in the articles. Overall, the review of the selected databases and articles, based on our inclusion criteria, resulted in the compilation of 11 studies. Ten articles were eliminated because they described a pediatric patient portal that was strictly web-based and did not interact with an EHR.
Figure 1.
Search results
Data Abstraction
We extracted data from the 11 articles and created a table including: study objectives; study design; setting; participants; intervention (where applicable); outcomes measures; and results. Where a study was not labeled with a particular design type, two reviewers assessed the study design and established consensus or the best categorization of the study methodology within the said hierarchy. In cases of disagreement, resolution was achieved through discussion between the reviewers or further review by a third author. The data were subsequently compiled and are presented in this article. Conclusions were drawn based on an aggregate synthesis of results with a narrative review of the evidence to further identify themes. Given the preliminary nature of most of the reported results, the wide variation of methodology utilized in the studies, and the absence of summary measures, we were unable to conduct an outcome-level assessment evaluating the reliability and validity of the data for each important outcomes by determining the methods used to assess them in each individual study as suggested by the Grading of Recommendations Assessment Development and Evaluation (GRADE) working group.16
Results
Key findings of this systematic review include profiles and characterization of pediatric portal users and nonusers, frequency and type of portal utilization, end-user testing, development of targeted pediatric patient portals for patients with a chronic condition, and issues of proxy and total access to personal health information for teenagers. Highlights of each study are presented in Table 2.
Table 2.
Summary of Study Design and Key Findings of Publications on Pediatric Patient Portals
| REFERENCE (Year) REGION | STUDY DESIGN; POPULATION AND SAMPLE SIZE | OUTCOME MEASURES; INTERVENTION | RESULTS |
|---|---|---|---|
| Ahlers-Schmidt and Nguyen21 (2013), Wichita, KS | Cross-sectional survey; Parents (n = 64) of children in the waiting room at a university pediatric clinic (University of Kansas Pediatrics Clinic) | Familiarity with technology, knowledge of portal, and perceptions of and likelihood to use portal; in person demonstration of patient portal using on-site kiosks at the pediatric clinic. | The majority (59, [92%]) thought the patient portal was easy to use and planned to view medical records and lab results but disliked having separate accounts for each child and the lack of a “symptom checker.” Many (44, [69%]) planned for future use, (62, [97%]) found navigation helpful, and (37, [58%]) wanted access to the portal via on-site kiosks. |
| Bergman et al.22 (2008), Palo Alto, CA | Qualitative focus groups and electronic bulletin boards; Teens (n = 28) and parents (n = 23) attending a large multispecialty group (Palo Alto Medical Foundation) | Themes from focus groups transcripts regarding attitudes toward the use of patient portal; Video demonstration of patient portal | Significant themes included (1) issues about teens’ control of their own healthcare, (2) enthusiasm about the use of the portal to access providers, seek health information, and make appointments, and (3) concerns about confidentiality. |
| Britto et al.23 (2009), Cincinnati, OH | Videotaped usability testing and quantitative survey; Parents of children diagnosed with a chronic disease (CF, JIA, or DM) not enrolled in the patient portal (n = 16) at a tertiary children’s hospital (Cincinnati Children’s Hospital) | Time participants took to complete or give up on each task, themes from videotaped usability testing sessions (three iterations), and Computer Usability Satisfaction Questionnaire (i.e., participants’ opinions on the efficiency of the system, its ease of use, and the likeability of the system interface) | Mean task completion ranged from 73 ±61 s to locate a document to 431 ±286 s to graph lab results. Graphing, location of data, requesting access, and data interpretation were challenging. Only two tasks were completed by 100% (n = 16) of participants, and overall satisfaction ratings were moderate (means 4.1–5.3 on a 7-point Likert scale). Satisfaction was greatest for interface pleasantness (5.9 ± 0.7) and likeability (5.8± 0.6) and lowest for error messages (2.3±1.2) and clarity of information (4.2±1.4). Overall mean satisfaction scores improved between iteration 1 and 3. |
| Britto et al.11 (2013), Cincinnati, OH | Qualitative interview; Parents of children diagnosed with a chronic disease (CF, JIA or DM) who had used the patient portal once or more during previous year (n = 24) at Cincinnati Children’s Hospital | Themes from interview questions exploring how the portal might or might not help parents manage their child’s healthcare. | Significant themes included parents’ perception of patient portals as beneficial, providing easier communication with care providers, convenience, a sense of control, reduced anxiety and reassurance. |
| Byczkowski et al.20 (2011), Cincinnati, OH | Retrospective observational study (data collection dates: September 1, 2003–February 29,2008); Parents of children with a chronic disease (CF, JIA, or DM) enrolled in the portal by February 29,2008 (n = 1,900) at Cincinnati Children’s Hospital | Percent of families who obtained a portal account, used the portal for the first time within 3 months and again 3–6 months after registration, number of times logged in, and session length. | About 28% of families obtained a portal account. Of those, 48% used the portal within 3 months of registration, and 16% continued to use it 3–6 months after registration. Families of African American patients and of patients insured by Medicaid were less likely to obtain a portal account. More outpatient visits and having private health insurance were associated with increased portal registration and use. |
| Byczkowski et al.6 (2014), Cincinnati, OH | Cross-sectional phone survey and semi-structured qualitative interviews; Phone surveys with parents of children with a chronic disease (CF, JIA, or DM) enrolled and using the portal (n = 126), and semistructured interviews with parents of children with a chronic disease enrolled but not using the portal (n= 15) at Cincinnati Children’s Hospital | Parent ratings of their experiences with and the value of a Web-based portal and reasons for not using the portal | Most parents agreed portal information was accurate, timely and useful. One hundred one (80%) used the portal once or more per month. Use did not replace calling providers. Eighty-eight (70%) said the portal improved ability to manage and understand child’s condition. Confidentiality and seeing worrisome health-related information about child were not major concerns. The portal helped improve parents’ understanding of and ability to manage their child’s condition. |
| Fiks et al.1 (2014), Philadelphia, PA | Semistructured qualitative interviews, focus groups, usability testing; semistructured interviews with parents of children with asthma (n = 7), focus groups with clinicians (n = 51), and usability testing with parents and clinicians (n = 10) at one urban and two suburban practices allied with Children’s Hospital of Philadelphia | Themes from interviews and focus groups regarding the utility and usability of specific features and overall portal system | Significant themes included the need for the portal to support sustained family-clinical team communication and ensure patient safety. Parents and clinicians prioritized (1) collecting parent and child concerns and goals, (2) symptom, side effect, and medication adherence tracking with decision support, and (3) accessible educational materials. More than 80% of participants (n = 8) were able to complete each scenario, and satisfaction ratings were high (means 8.2–8.4 on a 9-point Likert scale). |
| Hannan17 (2010), Hyde and Stockport, United Kingdom | Descriptive cross-sectional case study of one practice; Adult (n = 9,453) and pediatric patients ages 0–16 (n = 2,747) in two semirural practices associated with Haughton Thornley Medical Centres | Description of strategies used to enable patients to sign up for access to an electronic health record through an explicit consent process in-person and web-based video demonstrations of patient portal, and encouragement by clinicians for patients to get access to the portal | Key findings included 6% of patients gained access to their health records via an explicit consent process. There were over 100,000 viewings of the practice Web portal. There were no problems as a result of providing access. |
| Ketterer et al.19 (2013), Philadelphia, PA | Retrospective cross-sectional analysis (data collection dates: December 1,2007–November 30,2011) of data from a primary care database of an academic children’s hospital; children (n = 84,015) attending 1 of 13, urban and rural, primary care practices of an academic children’s hospital (Nemours Academic Children’s Hospital) | Enrolment in portal, activation of account, use of portal, demographics, practice characteristics, and presence of a chronic disease | About 38% enrolled in the portal; of these, about 26% activated the account. Portal enrolment was lower for adolescents, Medicaid recipients, low-income, Asian, other race and Hispanics and higher for patients with more office visits and autism on problem list. Once users were enrolled, portal activation was lower for Medicaid recipients, uninsured, African Americans, other race and Hispanics and higher for infants, going to a resident continuity practice, living farther from the practice, having more office visits, and having more problem list items. |
| Shaw and Ferranti8 (2011), Durham, NC | Cross-sectional secondary analysis of data (data collection dates: November 2009) from a database of large academic hospital (Duke University Medical Center); Patients (n = 5,963) diagnosed with type 1 or 2 diabetes enrolled in a provider-centered decision support tool. Age range,10–19 (n = 91). | Demographics and laboratory data | About 30% used the portal. Use was not a predictor of low-density lipoprotein and total cholesterol levels. Portal use was a significant predictor of glycosylated hemoglobin (p < .001). As patient-provider portals are increasingly implemented and used, clinical and nonclinical impacts must be evaluated. Portals provide patients with the opportunity to be increasingly involved in their own care, enhance patient-provider communication, and potentially reduce inequity, improve clinical outcomes, and increase access. |
| Tom et al.18 (2012), Washington State | Cross-sectional survey; Parents (n = 256) of children with chronic disease ≤ 5 years old and enrolled at an integrated healthcare system for ≥ 1 year. The healthcare system (Group Health Cooperative) provides care to 660,000 members in the Washington State. | Demographics, portal use in last 12 months (e.g., frequency of portal use, and barriers to use), parent ratings of care experiences (i.e., attention to growth and development, attention to safety and health, getting care quickly, getting needed care, prescription medications, and care coordination) | About 65% (n = 166) were portal users and 35% (n = 90) were nonusers. Top portal services were viewing medical and immunization records, secured messaging and scheduling appointments. Top reasons for not using the portal were “too busy,” “forgot login and/or password,” and “my child does not have healthcare needs.” No significant differences were found between users and nonusers. |
CF, cystic fibrosis; DM, diabetes mellitus; JIA, juvenile idiopathic arthritis.
CHARACTERISTICS OF THE STUDIES
Seven studies (64%) assessed the use of portals and described characteristics of portal registrants and users. Two studies (18%) focused on usability testing, including portal utility and ease of navigation. One study (9%) explored how the portal might be used specifically to help manage healthcare for a child with a chronic disease. The final study (9%) targeted issues of the transition from partial to complete access to their own personal health information by teenagers. Patient or caregiver satisfaction with the portal was measured in nine studies. Study design included focused interviews (n = 4), cross-sectional surveys (n = 3), retrospective observational analysis (n = 4), and usability testing (n = 1). One study combined both cross-sectional surveys and focused interviews. The studies were conducted primarily in academic settings (n = 8), with a focus on children with a chronic disease or ongoing medical condition (n = 8), and relied on parental rather than patient input (n = 8). The size of the study sample ranged from 7 parents to 84,015 patient records, but almost half (n = 5) of the studies had fewer than 100 participants.
Most were focused entirely on pediatric delivery; two of the studies examined children as part of a multi-aged cross-sectional analysis. None was prospective, and none was a randomized controlled trial. Ten studies were from the United States, and one was from the United Kingdom. Three articles were published in 2010 or earlier and eight in 2011 or later, indicating a recent, substantial increase in the evaluation of the patient portal in the pediatric environment. (See Table 2 for article information and excerpts from the data about study objectives, settings, methods, participants, and outcomes.)
The patient portals varied considerably in the services that they provided. Many provided access to test results, secure messaging, and access to notes or visit summaries, while others were still the prototype phase. A few studies had additional applications that had been specially created by the healthcare institutions, such as additional attributes for pediatric asthma patients.1 The portals were part of different types of EHRs, including Epic and Cerner, as well as the United Kingdom computerized system.
Studies addressed utilization rates (n=4), satisfaction (n=6), barriers (n=6), patient characteristics (n=4), and chronic illness (n=6). Some studies addressed more than one item.
PORTAL UTILIZATION
Reported utilization of the patient portal was generally low, especially in light of the cross-sectional nature of most of the studies, which did not follow adherence over time. Registration was as low as 4% (110/2,747) of 0 to16 year olds in a United Kingdom general practice study to 65% (256/166) of eligible responders to a survey of parent of children 0–5 years of age with at least one chronic disease17,18. Three studies reported account activation of 26–29% (8,409/31,765, 5937/14,085 and 530/1,900) of children8,19,20. Of note, in the only longitudinal analysis, Byczkowski et al.20 reported that only 16% (79/498) of children in their initial focus population comprised children with chronic diseases were still using the portal 3–6 months after registration. One study enumerated why the portal is used; parents with chronically ill children enrolled in a large health organization most frequently used immunization records, secured messaging and scheduling appointments18.
PATIENT SATISFACTION
Parents of both healthy and chronically ill children like the concept of the patient portal. Following a demonstration of the portal to parents in an academic practice waiting room, 92% (59/64) thought the patient portal was easy to use, and they planned to view medical records and laboratory results in the future.21 Parents who were part of a prototype demonstration felt that a good system will sustain communication and ensure patient safety.1 Parents of chronically ill children (diabetes mellitus, cystic fibrosis, and juvenile idiopathic arthritis) reported that the portal was accurate and timely, helping them to communicate with their children’s care providers. Additionally, the portal helped to manage and understand child’s condition, reducing anxiety and offering reassurance.6,11 The portal has not replaced telephone calls. Eighty percent of parents in one study used the portal at least once a month but reported that it had not replaced calling the healthcare provider.6 Teenagers felt enthusiastic about contacting their providers, seeking health information, and making appointments.22
REPORTED BARRIERS
There were a number of reported reasons for not using an integrated personal health record, and they varied by study. Two studies in which chronically ill children reported that drawbacks include difficulty in graphing and interpreting data, the need for more explanation of test results, and understanding medical terminology.6,23 Other barriers include dislike of having separate accounts for each child and the lack of a symptom checker.21 Logistical reasons included being too busy and forgetting the login/password for the system.18 Concerns about confidentiality, especially among teenagers and their parents, are also seen as a barrier to use.17,22
RACIAL AND SOCIOECONOMIC DISPARITIES
Among the study groups, portal users have a different profile than nonusers. Several studies reported that individuals of color and those with Medicaid or who were low income were less likely to obtain a portal account.19,20 Although Tom et al.18 reported no significant difference as measured by Consumer Healthcare Providers and Systems composite measure, subanalysis demonstrated that users were likely to have more education and commercial insurance versus nonusers. Adolescents are also less likely to activate the patient portal.19
CHRONIC DISEASE
Four of the 11 studies were working with parents of children with diabetes mellitus, juvenile idiopathic arthritis, and cystic fibrosis at a large academic hospital.6,11,20,23 Additionally, Tom et al.18 studied parents of children with at least one reported chronic disease, and Ketterer et al.19 found that use of the portal was higher for children with autism and those who had more conditions listed on the medical report problem list.
CLINICAL OUTCOMES
The one study that looked at a clinical outcome found that among the study population aged 10–99, portal use was statistically significant predictor of glycosylated hemoglobin level but not of low-density lipoprotein and total cholesterol levels.8
Discussion
The 11 studies included in this systematic review each contributed results relevant to the understanding of factors associated with use of the electronic patient portal within pediatric patient populations. In spite of the variations in methodology used to capture implementation, acceptance, and use relative to each study, the reviewed studies consistently demonstrated that parents are interested in using the patient portal. The highly descriptive nature of the studies reflects that incorporation of the patient portal within workflows is still often in the implementation stage and that it has yet to be used by the majority of patient-parent dyads. The primary findings were those of short-term, patient-level measures to help clinicians document how successful they are at implementing a patient portal. Long–term measures to help document the impact on clinical outcomes and operational efficiency have yet to be reported. The studies did not consider the implications of the portal and for patient data sharing that will be enhaced by the health information exchange. For example, the health information exchange may enhance patient-provider communication and function as a personal health record comprising electronic data gathered from various sources, including the EHR. 14
More than half of the pediatric patient portal research to date has been focused on chronic disease patients and their parents, including management of diabetes mellitus, juvenile idiopathic arthritis, cystic fibrosis, asthma, and chronic disease not specified.1,6,8,11,18,20,23 The research has focused on whether parents have registered to use the portal, are using the portal, and barriers to use of the portal. One study among a disparate age group examined health outcomes and found a benefit among portal users.8 Further investigation of the role, if any, of the portal in supporting parents and patients in addressing pediatric chronic disease outcomes, promoting partnerships between patients and providers, supporting self-care, and enabling informed decision-making has yet to be reported. While the technology did seem to be overwhelming, medical terminology is still perceived as a barrier.6,23
Only one study had a longitudinal component, and there are still unanswered questions and metrics to gather regarding frequency of use, adherence to use, effect on work patterns for clinicians, and whether there are changes in outcomes among the effected patients. There remain gaps in the literature about pediatric clinical outcomes, healthcare utilization, and the utility of patient-provider communication.
With the exception of Tom et al.,18 the studies did not drill down into what defined convenience for the parent or the patient, such as being able to contact the doctor out of hours24 or specific ease of test results accessibility.25 Similarly, although the benefits of improved communication between patient and provider were cited as benefits of the portal, the research did not report or describe the mechanics behind the improved communication. Although parents in one study mentioned that they felt that the portal reduced their anxiety,11 there was no evidence in this qualitative study that the parent-caregivers would describe this access as empowerment.
Although not a primary point of analysis for the many qualitative studies, several of the cross-sectional studies indicated that income, race, and educational level are predictive of portal adoption. Individuals of color, those with Medicaid, and those with low income were less likely to obtain a portal account. Those with more education and greater income were more likely to use the portal. This is somewhat different than the adult literature, in which somewhat lower adoption among African Americans but reasonable adoption across all racial groups have been found.8 Security and privacy were not overwhelming issues, unless it was in the context of adolescent access to a patient portal and what they and their parents might see. Although also not the primary topic of interest of the majority of the studies to date, the issue regarding adolescent access to their medical records is still to be resolved.
LIMITATIONS
This systematic review approach is affected by several limitations. Larger institutions were among the early adopters for EHRs and are more likely to have data to report at this point. Pediatric academic institutions are over-represented in this review. There is not a variety of methodological approaches to support the conclusions presented. Half of the studies are qualitative in nature and designed to test a prototype or to be hypothesis generating for a larger research study. Most data gathering was cross-sectional, and longitudinal measure of adherence, tracking of those lost to follow up, or capture of the effect of time on a health condition was not assessed. An additional limitation was that none of the studies measured if the consumption of services changed or other measurements of utilization. It is noteworthy that providers and their role in patient adoption of the patient portal and the impact of the patient portal are only tangentially mentioned.
Quantitative data including frequency of use over time, phone and web-messaging volume, the impact on types of patient contact following portal adoption, provider productivity, and potential cost saving estimates are needed. Additionally, the issue of access of an adolescent to his or her medical record versus parent and guardian information access and the effect of such access or lack thereof needs to be undertaken so that the patient portal as a potential means of supporting the transition from pediatric to adult healthcare may be assessed. Is the patient portal a tool for greater focus on patient- and family-centered care?
Conclusion
The review sought to examine the use of the patient portal in pediatric populations. There is a limited body of research that has addressed the integrated pediatric patient portal. The majority of studies have been conducted in academic settings among parents of children with chronic conditions. Studies in more varied settings, using a variety of methodologies including prospective approaches with more participants, including providers and adolescent patients are needed to study the longitudinal impact of the patient portal on pediatric patient care and clinical outcomes. The initial results from the studies in this review do not yet provide implications for clinical practice but do indicate that there is great potential for pediatric consumer informatics studies and patient empowerment.
Acknowledgments
The authors thank Patricia Calero, MS for her assistance and contributions to the structure of this manuscript. Dr. Bush’s work was supported by grant K99 HS022404 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Disclosure Statement
No competing financial interests exist.
References
- 1.Fiks AG, Mayne S, Karavite DJ, DeBartolo E, Grundmeier RW. A shared e-decision support portal for pediatric asthma. J Ambul Care Manage. 2014;37(2):120–126. doi: 10.1097/JAC.0000000000000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zomer-Kooijker K, van Erp FC, Balemans WAF, van Ewijk BE, van der Ent CK. The expert network and electronic portal for children with respiratory and allergic symptoms: rationale and design. BMC Pediatr. 2013;13:9. doi: 10.1186/1471-2431-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stinson J, McGrath P, Hodnett E, et al. Usability testing of an online self-management program for adolescents with juvenile idiopathic arthritis. J Med Internet Res. 2010;12(3):e30. doi: 10.2196/jmir.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emont S. [Last Accessed: July 28, 2015];Measuring the Impact of Patient Portals: What the Literature Tells Us. 2011 :1–19. Available at http://www.chcf.org/publications/2011/05/measuring-impact-patient-portals.
- 5.Bourgeois FC, Taylor PL, Emans SJ, Nigrin DJ, Mandl KD. Whose personal control? Creating private, personally controlled health records for pediatric and adolescent patients. J Am Med Inform Assoc. 2008;15(6):737–743. doi: 10.1197/jamia.M2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byczkowski TL, Munafo JK, Britto MT. Family perceptions of the usability and value of chronic disease web-based patient portals. Health Informatics J. 2014;20(2):151–162. doi: 10.1177/1460458213489054. [DOI] [PubMed] [Google Scholar]
- 7.Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159(10):677–687. doi: 10.7326/0003-4819-159-10-201311190-00006. [DOI] [PubMed] [Google Scholar]
- 8.Shaw RJ, Ferranti J. Patient-provider internet portals--patient outcomes and use. Comput Inform Nurs. 2011;29(12):714–718. doi: 10.1097/NCN.0b013e318224b597. quiz 719–720. [DOI] [PubMed] [Google Scholar]
- 9.Rosen P, Spalding SJ, Hannon MJ, Boudreau RM, Kwoh CK. Parent satisfaction with the electronic medical record in an academic pediatric rheumatology practice. J Med Internet Res. 2011;13(2):e40. doi: 10.2196/jmir.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Britto MT, Tivorsak TL, Slap GB. Adolescents’ needs for health care privacy. Pediatrics. 2010;126(6):e1469–e1476. doi: 10.1542/peds.2010-0389. [DOI] [PubMed] [Google Scholar]
- 11.Britto MT, Hesse EA, Kamdar OJ, Munafo JK. Parents’ perceptions of a patient portal for managing their child’s chronic illness. J Pediatr. 2013;163(1):280–281. e1–e2. doi: 10.1016/j.jpeds.2013.02.041. [DOI] [PubMed] [Google Scholar]
- 12.Huang JS, Terrones L, Tompane T, et al. Preparing adolescents with chronic disease for transition to adult care: a technology program. Pediatrics. 2014;133(6):e1639–e1646. doi: 10.1542/peds.2013-2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adler-Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long-term funding remains a concern. Health Aff (Millwood) 2013;32:1486–1492. doi: 10.1377/hlthaff.2013.0124. [DOI] [PubMed] [Google Scholar]
- 14.Fontaine P, Ross SE, Zink T, Schilling LM. Systematic review of health information exchange in primary care practices. J Am Board Fam Med. 2010;23:655–670. doi: 10.3122/jabfm.2010.05.090192. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 17.Hannan A. Providing patients online access to their primary care computerised medical records: a case study of sharing and caring. [Accessed August 2, 2014];Inform Prim Care. 2010 18(1):41–49. doi: 10.14236/jhi.v18i1.752. http://www.ncbi.nlm.nih.gov/pubmed/20429977. [DOI] [PubMed] [Google Scholar]
- 18.Tom JO, Mangione-Smith R, Solomon C, Grossman DC. Integrated personal health record use: association with parent-reported care experiences. Pediatrics. 2012;130(1):e183–e190. doi: 10.1542/peds.2011-1786. [DOI] [PubMed] [Google Scholar]
- 19.Ketterer T, West DW, Sanders VP, Hossain J, Kondo MC, Sharif I. Correlates of patient portal enrollment and activation in primary care pediatrics. Acad Pediatr. 2013;13(3):264–271. doi: 10.1016/j.acap.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Byczkowski TL, Munafo JK, Britto MT. Variation in use of Internet-based patient portals by parents of children with chronic disease. Arch Pediatr Adolesc Med. 2011;165(5):405–411. doi: 10.1001/archpediatrics.2011.55. [DOI] [PubMed] [Google Scholar]
- 21.Ahlers-Schmidt CR, Nguyen M. Parent intention to use a patient portal as related to their children following a facilitated demonstration. Telemed J E Health. 2013;19(12):979–981. doi: 10.1089/tmj.2013.0041. [DOI] [PubMed] [Google Scholar]
- 22.Bergman DA, Brown NL, Wilson S. Teen use of a patient portal: a qualitative study of parent and teen attitudes. [Accessed August 2, 2014];Perspect Health Inf Manag. 2008 5:13. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2556441&tool=pmcentrez&rendertype=abstract. [PMC free article] [PubMed] [Google Scholar]
- 23.Britto MT, Jimison HB, Munafo JK, Wissman J, Rogers ML, Hersh W. Usability testing finds problems for novice users of pediatric portals. J Am Med Inform Assoc. 2009;16(5):660–669. doi: 10.1197/jamia.M3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haun JN, Lind JD, Shimada SL, et al. Evaluating user experiences of the secure messaging tool on the Veterans Affairs’ patient portal system. J Med Internet Res. 2014;16(3):e75. doi: 10.2196/jmir.2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zarcadoolas C, Vaughon WL, Czaja SJ, Levy J, Rockoff ML. Consumers’ perceptions of patient-accessible electronic medical records. J Med Internet Res. 2013;15(8):e168. doi: 10.2196/jmir.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]