Abstract
Basosquamous carcinoma (BsC) is a controversial entity and both a diagnostic and therapeutic challenge. BsC has mixed histopathological characteristics of both basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). BCC and SCC display characteristic histopathology and behaviour; on the other hand, BsC is a rare tumour, which has variable morphology and displays less predictable behaviour. An early diagnosis of BsC is important due to the particularly aggressive nature of the tumour, the increased likelihood of recurrence and the potential for metastasis. Here, we present a case of BsC presenting as an extensive ulcer on the back. The case highlights the aggressive nature of the tumour and variation in appearance. It is important for all clinicians to be aware of this diagnosis so that the urgency of adequate biopsy in specialist clinics is not underestimated.
INTRODUCTION
Basosquamous carcinoma (BsC) is both a diagnostic and therapeutic challenge. It is a differential diagnosis that should be considered when a cutaneous lesion does not behave as expected. BsC has histopathological characteristics of both basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) [1]. BCC and SCC display characteristic histopathology and behaviour, allowing for prompt diagnosis and structured management. Meanwhile, BsC is a rare tumour that has variable morphology and displays less predictable behaviour [2]. Here, we present a case of BsC presenting as an extensive ulcer, demonstrating the consequences of late presentation and the challenges in diagnosis.
CASE REPORT
A 79-year-old lady was admitted under the medical team following a fall at home. The admitting doctor noted that she had a large ulcer over her lower back measuring ~20 × 32 cm (Fig. 1). The patient had seen her general practitioner 6 months earlier who felt that the lesion was benign and did not require further investigation. The lesion progressed and as she was the primary carer for her disabled husband she had difficulty acknowledging and pursuing her own medical needs. She was otherwise fit and well, had no significant past medical history and was not on any regular medications.
Figure 1:

An extensive ulcer, 20 × 32 cm of the lower back.
Based on the examination findings, the list of differential diagnoses included: pyoderma gangrenosum, cutaneous vasculitis, infection and malignancy. A 4-mm punch biopsy was arranged from the edge of the lesion, which was reported as an invasive BCC. Routine bloods and a vasculitis screen were unremarkable and wound swabs did not show any significant growth. Clinicopathological correlation was not consistent with a morphoeic BCC and therefore a repeat incisional biopsy was arranged. This showed a large, endophytic tumour displaying both basaloid and squamoid areas. This unusual finding could represent either a ‘collision’ tumour or a BCC with some squamous differentiation, as in BsC.
Within 4 weeks of presentation, the lesion had increased in size to 36 × 48 cm. In association with this rapid expansion, the patient started to experience severe lumbosacral pain radiating down the left leg. Magnetic resonance imaging (MRI) revealed tumour invasion into the paraspinal muscles, posterior lumbar vertebrae and even the spinal canal in places (Fig. 2).
Figure 2:
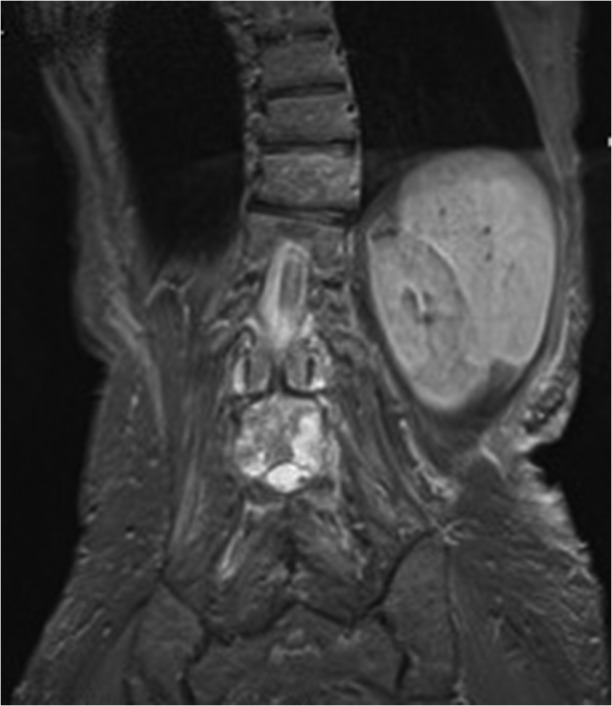
MRI of the tumour invading the underlying paraspinal muscles and lumbar vertebrae extending into the spinal canal.
Imaging and histopathology were urgently reviewed at a tertiary centre multidisciplinary team meeting. The diagnosis of BsC was confirmed. Due to the advanced nature of the tumour, it was deemed inoperable and no conventional palliative therapy was available. The tumour progressed rapidly and 14 weeks from initial presentation the patient succumbed to sepsis and large volume fluid loss via the ulcer.
DISCUSSION
BsC is a rare variant of BCC, which displays histological features of both BCC and SCC [2]. It commonly affects the head and neck [3]. Although there has been much debate about the categorization of BsC, the histological features of it are clearly defined [4, 5]. Classical features include inflammatory islands of basaloid cells with nuclei that palisade at the periphery. Within individual islands are eosinophilic squamous cells, which may show intracellular bridges of keratinization. Immunohistochemistry can facilitate the identification of BsC (Figs 3–6). The presence of a transitional zone on histopathology lends support to the idea that BsC derives from transformation of BCC into SCC thus altering its usual behaviour [6]. It is distinguished from a collision tumour, which shows discrete areas of BCC and SCC present in close proximity and lacking a transitional zone.
Figure 4:
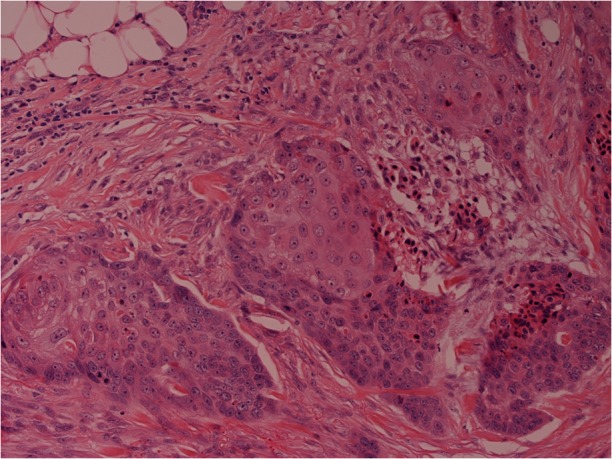
Evidence of squamous differentiation in the basaloid island in the centre of this image (original magnification x200).
Figure 5:
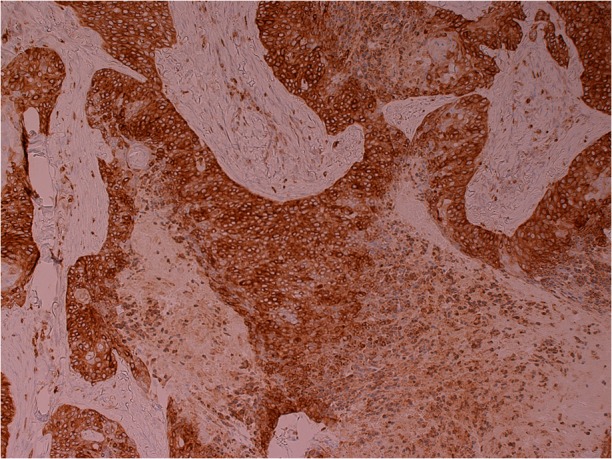
Tumour expressing the immunohistochemical marker BCL2, highlighting the presence of BCC (original magnification x200).
Figure 3:
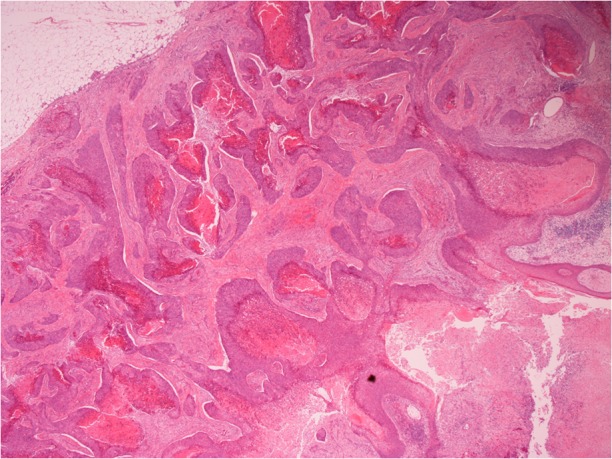
Invasive, endophytic tumour with islands of basaloid cells invading the dermis and associated with retraction artefact and prominent necrosis (haematoxylin and eosin, original magnification x40).
Figure 6:
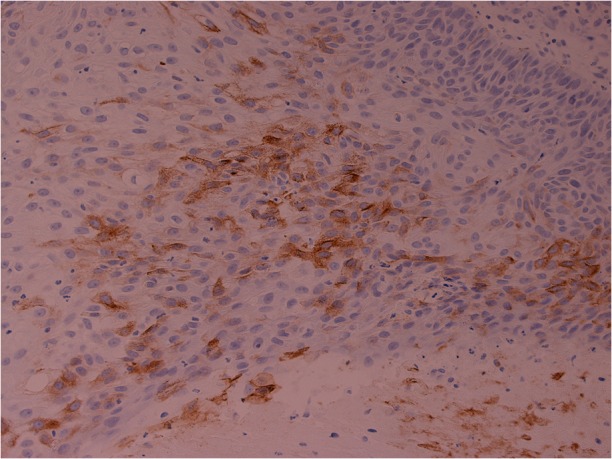
Epithelial membrane antigen highlighting squamous cells in the tumour (original magnification x200).
As this case study demonstrates, an early diagnosis of BsC is important due to the particularly aggressive nature of the tumour, the increased likelihood of recurrence and the potential for metastasis [1, 7]. In fact, BsC is reported to have greater metastatic potential than SCC [8]. The incidence of BsC is estimated to account for ~2% of skin cancers [4]. However, BsC is also believed to be under-diagnosed due to histological features that may not be apparent in all biopsies. At early stages, as in this case, BsC can appear similar to some benign lesions. However, its rapid growth should alert clinicians to an alternative diagnosis. The importance of an adequate biopsy needs to be emphasized, as squamous differentiation may only be apparent on deeper layers or in certain parts of the tumour.
Following diagnosis, surgery plays a key role in treatment when it is possible to operate [3]. Full excision with tumour-free margins is essential and there may be a need for local radiotherapy depending on tumour stage [9]. Due to the increased metastatic potential of the tumour, radiographic evaluation should be considered to fully investigate for metastases [10]. Currently, however, there is no standardized treatment protocol for BsC and further research is required to evaluate and optimize treatment for these tumours. Clinicians should be aware of the natural history of this particular malignancy as prompt excision can be a lifesaving intervention.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
This is a retrospective case report, the patient and family consented to publication. The patient is not identifiable in any of the images provided.
CONSENT
The patient consented to publication and use of images prior to her death.
GUARANTOR
Rakesh L. Anand.
REFERENCES
- 1.Garcia C, Poletti E, Crowson AN. Basosquamous carcinoma. J Am Acad Dermatol 2009;60:137–43. [DOI] [PubMed] [Google Scholar]
- 2.Betti R, Crosti C, Ghiozzi S, Cerri A, Moneghini L, Menni S. Basosquamous cell carcinoma: a survey of 76 patients and a comparative analysis of basal cell carcinomas and squamous cell carcinomas. Eur J Dermatol 2013;23:83–6. [DOI] [PubMed] [Google Scholar]
- 3.Leibovitch I, Huilgol SC, Selva D, Richards S, Paver R. Basosquamous carcinoma: treatment with Mohs micrographic surgery. Cancer 2005;104:170–5. [DOI] [PubMed] [Google Scholar]
- 4.Borel DM. Cutaneous basosquamous carcinoma. Review of the literature and report of 35 cases. Arch Pathol Lab Med 1973;95:293–7. [PubMed] [Google Scholar]
- 5.LeBoit PE, Burg G, Weedon D, Sarasin A, eds.World Health Organisation classification of tumors. Pathology and Genetics of Skin Tumors. Lyon: IARC Press, 2006,10–33. [Google Scholar]
- 6.Lima N, Verli F, Luiz de Miranda J, Marinho S. Basosquamous carcinoma: histopathological features. Indian J Dermatol 2012;57:382–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopes de Faria J, Nunes PH. Basosquamous cell carcinoma of the skin with metastases. Histopathology 1988;12:85–94. [DOI] [PubMed] [Google Scholar]
- 8.Martin R, Edwards M, Cawte T, Sewell C, McMasters K. Basosquamous carcinoma: analysis of prognostic factors influencing recurrence. Cancer 2000;88:1365–9. [DOI] [PubMed] [Google Scholar]
- 9.Ting P, Kasper R, Arlette JP. Metastatic basal cell carcinoma: report of two cases and literature review. J Cutan Med Surg 2005;9:10–5. [DOI] [PubMed] [Google Scholar]
- 10.Joshi P, Kulkarni MJ, Abhyankar A, Shet T, Basu S. Detection by (18)F-FDG PET of unsuspected extensive bone marrow metastases in a case of basosquamous carcinoma of the cheek. Hell J Nucl Med 2011;14:307–8. [PubMed] [Google Scholar]


