Abstract
Introduction
Brunner’s glands are submucosal glands found in the duodenum. Proliferation of these glands can lead to the formation of Brunner’s gland hamartomas (BGHs), which are uncommon, asymptomatic and usually found incidentally. They are predominantly benign lesions, but instances of malignant transformation have been reported.
Case History
We describe a rare case in which a periampullary lesion was causing biliary obstruction on a background of weight loss, and was associated with dilatation of the common bile duct and pancreatic duct on computed tomography and magnetic resonance imaging. Further investigation with endoscopic ultrasound and biopsy did not provide a definitive diagnosis. Given the symptoms and findings upon investigations, we proceeded to pylorus-preserving pancreatoduodenectomy.
Conclusions
This was a rare case in which BGH gave rise to biliary obstruction against a background of weight loss. Due to a high index of suspicion (weight loss and evidence of dilatation of the common bile duct and pancreatic duct), this procedure was justified because the consequences of a missed periampullary cancer far outweighed surgical risks.
Keywords: Brunner’s glands, Periampullary lesion, Pancreatoduodenectomy
Brunner’s glands are submucosal mucus-secreting glands located in the duodenum, and a Brunner’s gland hamartoma (BGH) is a benign proliferative lesion arising from them. These lesions account for ≈10% of benign tumours of the duodenum.1 BGHs are found predominantly (57%) in the duodenal bulb, with decreasing frequency in the second (27%) and third part (5%) of the duodenum. This distribution corresponds to the anatomical distribution of Brunner’s glands.2
The aetiology of BGHs remains uncertain, but it has been linked to excessive local irritation from acidic gastric chyme, vagal stimuli, or unidentified antral hormones.3 Despite being predominantly benign lesions malignant transformation has been reported.4
Most patients do not experience symptoms from these lesions (which are usually incidental findings during endoscopy). If symptomatic, patients usually experience non-specific abdominal pain, bloating or nausea. More significant symptoms reported include bleeding or obstruction within the gastrointestinal tract.5 Treatment options include endoscopic removal or resection depending on the position of the lesion, and whether it is pedunculated or large and sessile.6
We describe a rare case of a periampullary BGH giving rise to dilatation of the common bile duct (CBD) and pancreatic duct (‘double duct sign’ (DDS)) with regard to imaging features for pancreatic malignancies.
Case History
A 52-year-old female was referred to the hepatopancreatobiliary unit in May 2014 with mildly deranged liver-function tests and weight loss of ≈6.3kg. Computed tomography and magnetic resonance cholangiopancreatography had shown a dilated CBD and pancreatic duct with an abrupt change in calibre at the ampulla suggestive of an obstructive ampullary lesion (DDS).
The patient had a history of stage-1A endometrial cancer for which she had undergone a total abdominal hysterectomy and bilateral salpingo-oophorectomy. In addition, a T2N0 grade-2 invasive carcinoma of the left breast had been treated with wide local excision, radiotherapy and hormones. She had undergone laparoscopic cholecystectomy after an episode of pancreatitis during which time she had endoscopic retrograde cholangiopancreatography and sphincterotomy.
Physical examination at outpatient review was unremarkable. The dilated CBD might have been attributed to the previous cholecystectomy, but the finding of the DDS was investigated further with endoscopic ultrasound, which confirmed a solid lesion in the medial aspect of the D1 and D2 regions of the ampulla. However, biopsies taken at endoscopic ultrasound demonstrated only chronic inflammation.
Figure 1.
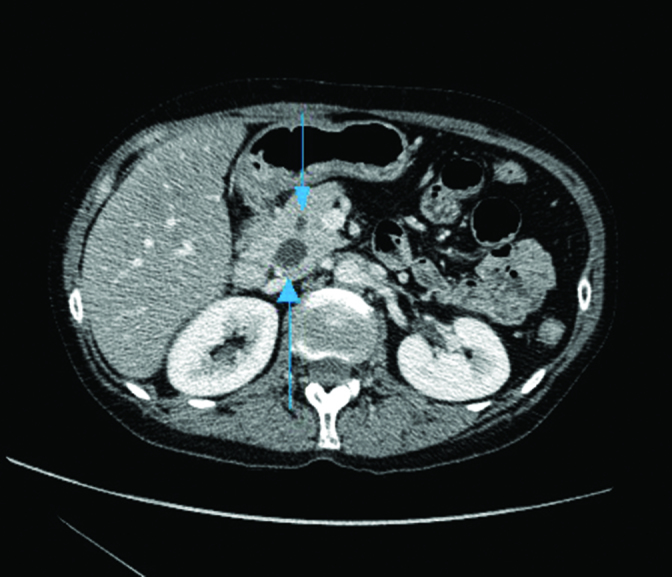
Axial CT showing a dilated common bile duct and pancreatic duct (arrows).
After discussion at the local multidisciplinary meeting, a decision was made to proceed to pylorus-preserving pancreatoduodenectomy.
Histological examination of the resected specimen revealed marked prominence of Brunner’s glands with nodularity and focal cystic change in the periampullary region and duodenum. These findings were in accordance with that of a BGH without dysplasia or malignancy.
Discussion
This rare case demonstrates the ability of a BGH to give rise to the DDS on CT and MRI and thus mimic an ampullary or pancreatic malignancy.7 This was an extremely concerning finding taken in the context of the presentation. The lesion was assessed further with endoscopic ultrasound and biopsies, but the diagnosis of BGH could not be established. Biopsies are often indeterminate due to the submucosal position of these lesions, so they are missed and not diagnosed preoperatively.8
Medical management of BGHs has focussed on control of gastric acidity but it causes regression of these lesions only rarely. Excision is usually first-line treatment and can be done via endoscopic or surgical means.
Despite extensive investigations undertaken in our patient, a high index of suspicion of underlying malignancy justified resection. Consequences of a missed periampullary tumour far outweighed the risks associated with surgery.
This is the first reported case of a BGH giving rise to the DDS and thus mimicking a periampullary or pancreatic malignancy.
References
- 1.Chattopadhyay P, Kundu AK, Bhattacharyya S, Bandyophadyay A. Diffuse nodular hyperplasia of Brunner’s gland presenting as upper gastrointestinal haemorrhage. Singapore Med J 2008; : 81–83. [PubMed] [Google Scholar]
- 2.Yantis RK, Antonioli DA. Polyps of the small intestine In: Odze RD, Goldblum JR, Crawford JM. Surgical pathology of the GI tract, liver, biliary tract and pancreas. 1st ed Pennsylvania: Saunders Press; 2004. p. 295–296. [Google Scholar]
- 3.Peison B, Benisch B. Brunner’s gland adenoma of the duodenal bulb. Am J Gastroenterol 1982; : 276–278. [PubMed] [Google Scholar]
- 4.Brooks MJ, Majunatha S, Allen CA, Cox M. Malignant potential in a Brunner’s gland hamartoma. Postgrad Med J 2003; : 416–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levine JA, Burgart LJ, Batts KP, Wang KK. Brunner’s gland hamartomas: clinical presentation and pathological features of 27 cases. Am J Gastroenterol 1995; : 290–294. [PubMed] [Google Scholar]
- 6.Jansen JM, Stuifbergen WN, Van Milligen AW. Endoscopic resection of a large Brunner’s gland adenoma. Neth J Med 2002; : 253–255. [PubMed] [Google Scholar]
- 7.Ahualli J. The double duct sign. Radiology 2007; : 314–315. [DOI] [PubMed] [Google Scholar]
- 8.Iusco D, Roncoroni L, Violi V et al. Brunner’s gland hamartoma: ‘over-treatment’ of a voluminous mass simulating a malignancy of the pancreatic-duodenal area. J Pancreas (Online) 2005; : 348–353. [PubMed] [Google Scholar]


