Abstract
Introduction
A substantial number of patients undergoing total hip or knee arthroplasty (THA or TKA) do not or only partially return to work. This study aimed to identify differences in determinants of return to work in THA and TKA.
Methods
We conducted a prospective, observational study of working patients aged <65 years undergoing THA or TKA for osteoarthritis. The primary outcome was full versus partial or no return to work 12 months postoperatively. Factors analysed included preoperative sociodemographic and work characteristics, alongside the Hip Disability and Osteoarthritis Outcome Score (HOOS)/Knee Injury and Osteoarthritis Outcome Score (KOOS), and Oxford Hip and Knee Scores.
Results
Of 67 THA and 56 TKA patients, 9 (13%) and 10 (19%), respectively, returned partially and 5 (7%) and 6 (11%), respectively, did not return to work 1 year postoperatively. Preoperative factors associated with partial or no return to work in THA patients were self-employment, absence from work and a better HOOS Activities of Daily Living (ADL) subscale score, whereas only work absence was relevant in TKA patients. Type of surgery modified the impact of ADL scores on return to work.
Conclusions
In both THA and TKA, absence from work affected return to work, whereas self-employment and better preoperative ADL subscale scores were also associated in THA patients. The impact of ADL scores on return to work was modified by type of surgery. These results suggest that strategies aiming to influence modifiable factors should consider THA and TKA separately.
Keywords: Arthroplasty, Return to work, Work limitations, Total hip or total knee replacement
Introduction
Total hip and knee arthroplasty (THA and TKA) are effective procedures to reduce pain and improve function in patients with hip or knee osteoarthritis.1,2 A substantial proportion (15%–45%) of patients are of working age (<65 years old) at the time of surgery.3,4 While the majority of patients return to work postoperatively (68%–95% following THA; 71%–83% after TKA),5 the absolute number of patients who do not return to work is substantial. Research into potentially modifiable factors for return to work after total joint replacements is therefore warranted.
The determinants of return to work after THA or TKA have been addressed in two systematic reviews.5,6 The authors, based on a limited number of studies (five THA, one TKA and one mixed study), concluded that sociodemographic (age, sex, educational level), work (self-employment, physical demands, preoperative work disability, accessibility of the workplace, receiving workers’ compensation), joint function and surgical- (complications) and rehabilitation-related factors (surgical approach) are associated with postoperative work status. Clinical studies of both THA and TKA published after these reviews also identified one or more of these determinants.7,8
Overall, data on the determinants of partial or no return to work after total joint arthroplasty, and potential differences between THA and TKA, is scarce, particularly as, in the aforementioned systematic reviews, no synthesis of the individual studies could be made due to their limited number and large methodological variations. Moreover, the majority of studies included only THA patients, meaning that the factors related to return to work after TKA remain largely unknown. Finally, few studies considered reductions in working hours, which indicates productivity loss as an outcome.
Given the lack of knowledge, we aimed to identify, prospectively, differences in determinants of partial or no return to work 1 year after surgery in patients undergoing THA or TKA for osteoarthritis.
Methods
This study was part of a 1-year observational study of THA and TKA outcomes, which aimed to include all consecutive patients undergoing primary THA or TKA for osteoarthritis in the Alrijne Hospital, Leiderdorp, the Netherlands, between October 2010 and September 2012. All patients were required to have a physical and mental status that allowed the completion of questionnaires, and the ability to read and understand Dutch. The study protocol was reviewed and approved by the local hospital review board (registration number 10/07), which is associated with the Medical Research Ethics Committee of the Leiden University Medical Center, Leiden, the Netherlands.
All potentially eligible patients were identified from the surgical planning list. Patients with rheumatoid arthritis, a tumor, (hemi)paresis or amputation of the (lower) leg, and patients undergoing a hemi-arthroplasty or revision THA or TKA were excluded. One day preoperatively, the treating orthopedic surgeon provided oral and written information about the study to all eligible patients, as well as a questionnaire and a consent form. Patients who returned the set of questionnaires and informed consent form when admitted to the hospital for surgery were posted the postoperative questionnaire 12 months after surgery. Patients who did not return the questionnaire were contacted by telephone 4 weeks later.
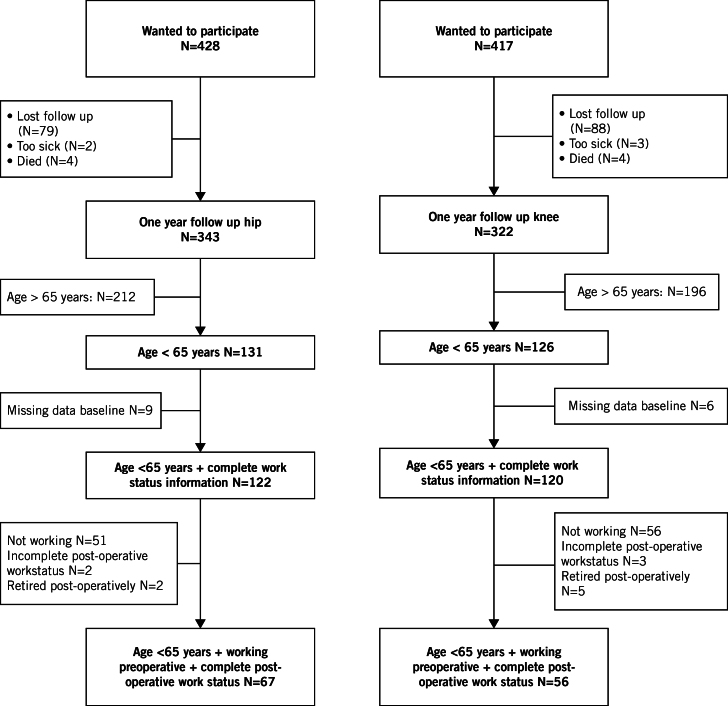
Of the 845 total joint arthroplasty patients who were interested in taking part in the study, 343 THA (80%) and 322 TKA (77%) patients completed the postoperative questionnaire. Of those, 67 THA patients and 56 TKA patients were aged under 65 years and working preoperatively, provided information on their number of working hours postoperatively and did not retire after surgery. They were therefore included in the current analysis (Figure 1).
Figure 1.
Flow diagram
Assessments
The primary outcome measure was the presence of full versus partial or no return to work 12 months after THA or TKA. Preoperative factors found to be related to work outcomes were classified as patient and work characteristics, joint functioning and health status. In case of incomplete or unclear provision of data on working hours or postoperative work status, an additional questionnaire was sent and/or a telephone interview was performed by the primary investigator (CL).
Patient characteristics included: age (years); sex; body mass index (BMI); educational attainment, which was defined as low (primary school or lower vocational education), medium (lower general secondary school or intermediate vocational education) or high (higher general secondary school, higher vocational education or university); and living status, which was defined as independent, assisted living or in a nursing home.
Preoperatively, all patients were asked to indicate whether they had a paid job (yes/no). If no, they were asked whether they were a pensioner, housewife/houseman or unemployed.
The following aspects of the patients’ working situation were recorded: amount of hours currently worked per week; self-employed or salaried; absenteeism from work due to hip or knee complaints (yes/no); and the presence of work adaptions (yes/no), with yes including at least one of the following: change of tasks; performing fewer tasks; changes in working hours; other work-related adaptations or devices.
Job title was recorded and classified as light, medium or heavy, in terms of its physical demands on the hip or knee, by two occupational physicians who independently scored the job based on work activity risk factors. The scoring system was derived from the evidence-based exposure criteria for the work relatedness of hip and knee osteoarthritis developed by the Netherlands Center for Occupational Diseases.9 Disagreements in coding were resolved by consensus.
The patients’ preoperative expectations to return to work were examined using one item of the Hospital for Special Surgery Hip Replacement and Knee Replacement Expectations Surveys,10 formulated as: “the expectation regarding being able to have a paid job”. The 5-point Likert scale was dichotomized into ‘back to normal’ or ‘less than back to normal’.
Postoperatively, all patients were asked whether they were currently working (yes/no). If yes: they were asked to report their current number of working hours per week. Based on the difference in pre- and postoperative working hours, return to work was classified as: complete return (no difference in, or higher. postoperative working hours); partial return (working fewer hours postoperatively); or no return to work (complete work disability pension, full-time sick leave or out of work). For the present analysis, partial return and no return to work were combined.
Hip and knee functioning and health status
The Hip disability and Osteoarthritis Outcome Score (HOOS) and Knee injury and Osteoarthritis Outcome Score (KOOS) consist of 40 and 42 items respectively, divided over 5 subscales: Pain (10 items); Symptoms, including stiffness and range of motion (5 items); Activities of Daily Living (ADL) (17 items); Sport and Recreation Function (4 items); and Quality of Life (4 items).11,12 A normalized score (100 indicating no symptoms and 0 indicating extreme symptoms) is calculated for each subscale.13
The Oxford Hip Score (OHS) and the Oxford Knee Score (OKS) are 12-item questionnaires, with each item scored from 1 to 5, and the total ranging from 12 to 60 (lower scores representing fewer symptoms).14,15
Statistical analyses
Descriptive analyses were performed for the preoperative and postoperative sociodemographic characteristics, working situation, joint function and health status.
Mean changes in scores between preoperative and postoperative clinical variables (HOOS/KOOS, OHS/OKS) and the 95% confidence interval (CI) were calculated using a paired t-test. Mann-Whitney U or Chi-squared tests were used to compare the preoperative characteristics of patients undergoing THA or TKA and the change in HOOS/KOOS and OHS/OKS scores between patients who fully returned to work and those who returned partially or not at all at 12 months. The analyses were performed for THA and TKA separately and then combined.
To explore the relative importance of preoperative factors associated with return to work on univariate analyses (p<0.15) and those known from the literature, exploratory stepwise logistic regression analyses were carried out within the THA, TKA and combined groups. All factors associated with return to work were entered into ordinary logistic regression analysis for the combined group. This included interaction terms related to the type of surgery (hip or knee) to identify the possibility of effect modification, such as the impact of THA or TKA on return to work being dependent on a third variable.
All data were analysed using SPSS Statistics version 20.0 (IBM, Armonk, NY, USA).
Results
Sixty-seven THA and 56 TKA patients, with a mean age of 56 years (standard deviation 6.6 and 5.7, respectively) were included in the analysis (Table 1).
Table 1.
Preoperative general and working characteristics of working patients <65 years of age undergoing total joint arthroplasty
| THA patients (N=67) | TKA patients (N=56) | p value | |
|---|---|---|---|
| Sex, female | 33 (49) | 31 (55) | 0.587 |
|
Mean age, years (SD) Age groups 18–45 46–55 56–65 |
56 (6.6) 8 (12) 16 (24) 43 (64) |
56 (5.7) 4 (7) 15 (27) 37 (66) |
0.612 |
| Body mass index, mean (SD) | 28 (6.0) | 30 (4.4) | 0.000* |
|
Education level Low Medium High |
(N=66) 19 (29) 26 (39) 21 (32) |
16 (29) 25 (45) 15 (27) |
0.781 |
| Living status, Living independently | (N=64) 64 (100) | (N=55) 55 (100) | 0.380 |
| Employment status, self-employed | (N=59) 11 (18) | (N=54) 8 (15) | 0.624 |
| Preoperative working hours, mean (SD) | 32 (12.5) | 31 (12.3) | 0.460 |
|
Physical demands of work Light work Medium work Heavy work |
(N=59) 41 (70) 14 (24) 4 (7) |
(N=54) 47 (87) 2 (4) 5 (9) |
0.008* |
| Preoperative sick leave from work due to hip/knee complaints | (N=59) 19 (32) | (N=50) 16 (32) | 1.000 |
| Preoperative work adaptations | (N=46) 11 (24) | (N=46) 16 (35) | 0.180 |
| Preoperative workers’ compensation | (N=59) 5 (8) | (N=54) 6 (11) | 0.437 |
|
Expectation over return to work Back to normal |
(N=48) 43 (90) |
(N=46) 41 (89) |
1.000 |
|
HOOS or KOOS baseline scores, mean (SD) ADL Pain Quality of life Sport Symptoms |
(N=62) 42 (18) (N=64) 38 (21) (N=65) 34 (9) (N=64) 15 (18) (N=65) 31 (19) |
(N=51) 44 (16) (N=54) 36 (15) (N=53) 31 (9) (N=53) 8.8 (11) (N=54) 42 (15) |
0.421 0.596 0.135 0.079* 0.001* |
|
HOOS or KOOS changes scores, mean (95% CI) ADL Pain Quality of life Sport Symptoms |
(N=50) 49 (44–55) (N=53) 53 (47–58) (N=54) 20 (15–25) (N=52) 52 (44–59) (N=55) 52 (45–58) |
(N=44) 35 (29–41) (N=47) 42 (35–48) (N=45) 14 (9–20) (N=45) 32 (23–40) (N=47) 7 (2–11) |
0.001* 0.009* 0.052 0.000* 0.000* |
| Oxford Knee/Hip Score baseline, mean (SD) | (N=60) 23 (7) | (N=54) 24 (15) | 0.525 |
| Oxford Knee/Hip change Score, mean (95% CI) | (N=53) 20 (18–22) | (N=48) 15 (12–17) | 0.009* |
*Comparison of THA and TKA patients using Chi-squared or Mann-Whitney U tests, where appropriate. Significance level: p<0.05. All values n (%) unless otherwise stated ADL = Activities of Daily Living; HOOS/KOOS = Hip disability and Osteoarthritis Outcome Score/Knee injury and Osteoarthritis Outcome Score; SD = standard deviation; THA = total hip arthroplasty; TKA = total knee arthroplasty
The preoperative mean number of working hours was 32±12.5 hours/week (median 32 hours/week, range 4–70) in THA patients and 31±12.3 hours/week (median 32 hours/week, range 10–70) in TKA patients. Patients who underwent THA had, compared with TKA patients, a significantly lower BMI (P=0.0001), and were significantly less likely to have light physically demanding work (p=0.008). THA patients were also less likely to have adaptations at work, although the difference was not significant (p=0.180).
The only significant baseline difference in function was that patients who underwent THA had significantly lower Symptoms subscale scores on the HOOS/KOOS versus TKA patients (P=0.001).
There were significant differences between the pre- and postoperative HOOS/KOOS subscale, as well as OHS and OKS, scores, with all improvements on the HOOS subscales and on the OHS being greater than the corresponding improvements of the KOOS subscales and the OKS. The only exceptions were for improvements on the HOOS and KOOS Quality of Life scores, which were not significantly different between pre- and postoperative measures.
Fifty-three (79%) THA patients and 40 (71%) TKA patients who were working preoperatively fully returned to work 1-year postoperatively. Nine (13%) patients in the THA group and 10 (18%) in the TKA group worked fewer hours than preoperatively, while five (7%) THA patients and six (11%) TKA patients did not return to work at all.
Among the 19 patients who partially returned to work, the mean decrease in working time was 17±11.5 hours/week (range 5–35) in the THA group, 14±13.0 hours/week (range 2–38) in the TKA group and 15±12.0 hours/week in the total group. Table 2 shows the factors associated with partial or full return to work 1 year after THA or TKA in patients of working age.
Table 2.
Factors associated with return to work in working patients <65 years of age undergoing total joint arthroplasty
| THA patients working preoperatively | TKA patients working preoperatively | |||||||
|---|---|---|---|---|---|---|---|---|
| Full return to work (N=53) | No or partial return to work (N=14) | p value** | Odds ratio (95% CI)*** | Full return to work (N=40) | No or partial return to work (N=16) | p value** | Odds ratio (95% CI)*** | |
| Sex, Female | 28 (53) | 5 (36) | 0.369 | 24 (60) | 7 (44) | 0.374 | ||
|
Mean age, years (SD) 18–45 46–55 56–65 |
55.1 (6.5) 7 (13) 15 (28) 31 (59) |
58.7 (6.6) 1 (7) 1 (7) 12 (86) |
0.012* | 55.3 (5.7) 3 (8) 13 (33) 24 (60) |
57.0 (5.7) 1 (6) 2 (13) 13 (81) |
0.317 | ||
| Body mass index; mean (SD) | (N=52) 28.0 (6.2) | 26.1 (4.8) | 0.153 | (N=39) 29.7 (4.3) | 30.9 (4.7) | 0.344 | ||
|
Education level# Low Medium High |
(N=52) 10 (19) 24 (46) 18 (35) |
9 (64) 2 (14) 3 (21) |
0.006* |
11 (28) 18 (45) 11 (28) |
5 (31) 7 (44) 4 (25) |
1.000 | ||
| Self employed# | (N=46) 5 (11) | (N=13) 6 (46) | 0.009* | 7.63 (1.5–39.8) | (N=39) 5 (13) | (N=15) 3 (20) | 0.390 | 2.69 (0.5–15.8) |
| Preoperative working hours, mean (SD) | 30.8 (11.9) | 36.1 (14.2) | 0.230 | 29.8 (11.4) | 34.4 (14.1) | 0.207 | ||
|
Type of work Light work Medium work Heavy work |
(N=46) 33 (72) 10 (22) 3 (7) |
(N=13) 8 (62) 4 (31) 1 (8) |
0.672 | (N=39) 33 (85) 1 (3) 5 (13) |
(N=15) 14 (93) 1 (7) 0 (0) |
0.270 | ||
| Preoperative absence from work due to hip or knee complaints# | (N=46) 10 (22) | (N=13) 9 (69) | 0.002* | 8.62 (1.9–39.0) | (N=36) 9 (25) | (N=14) 7 (50) | 0.105 |
4.18 (1.0–17.1) |
| Preoperative work adaptions# | (N=35) 6 (17) | (N=11) 5 (45) | 0.100 | (N=33) 13 (39) | (N=13) 3 (23) | 0.493 | ||
| Preoperative workers' compensation | (N=46) 3 (7) | (N=13) 2 (15) | 0.302 |
(N=39) 4 (10) | (N=15) 2 (13) | 1.000 | ||
| Expectation over return to work, Back to normal | (N=40) 36 (90) |
(N=8) 7 (88) |
1.000 |
(N=36) 33 (92) |
(N=10) 8 (80) |
0.201 |
||
|
Baseline HOOS or KOOS, mean (SD) ADL# Pain# Quality of life# Sport# Symptoms |
(N=49) 39 (16) (N=51) 36 (19) (N=52) 33 (9) (N=51) 13 (16) (N=52) 32 (18) |
(N=13) 53 (18) 50 (24.2) 35 (11) 24 (22) 29 (25) |
0.018* 0.058 0.913 0.096 0.439 |
1.03 (1.0–1.1) |
(N=36) 46 (15) (N=38) 36 (14) (N=37) 32 (10) (N=37) 10 (11) (N=37) 43 (15) |
(N=15) 40 (18) 34 (17) 28 (6) 7 (11) 41 (14) |
0.331 0.711 0.114 0.188 0.642 |
0.99 (0.9–1.0) |
|
Change in HOOS or KOOS, mean (95% CI) ADL Pain Quality of life Sport Symptoms |
(N=39) 53 (47–58) (N=42) 54 (48–60) (N=43) 19 (14–24) (N=42) 52 (43–60) (N=44) 49 (42–56) |
(N=11) 38 (27–50) (N=11) 49 (35–63) (N=11) 20 (8–32) (N=10) 51 (35–67) (N=11) 65 (48–82) |
0.016* 0.546 0.786 0.798 0.075 |
(N=31) 37 (31–44) (N=33) 44 (38–51) (N=33) 16 (9–23) (N=32) 37 (27–47) (N=33) 9 (4–14) |
(N=14) 29 (14–44) (N=15) 36 (21–50) (N=13) 10 (2–17) (N=14) 19 (6–32) (N=15) 0.7 (–7–9) |
0.166 0.278 0.299 0.039* 0.072 |
||
| Oxford Knee/Hip Score, mean (SD) | (N=48) 23 (7) | (N=12) 25 (8) | 0.244 | (N=38) 24 (7) | 24 (7) | 0.962 | ||
| Oxford Knee/Hip change score, mean (95% CI) | (N=42) 20 (1–18) | (N=11) 18 (14–23) | 0.356 | (N=34) 16 (14–19) | (N=15) 12 (5–18) | 0.086 | ||
*Comparison of full return to work versus partial or no return to work patients using Chi-squared or Mann-Whitney U tests, where appropriate
**Univariate analysis
***Multivariable stepwise regression model
#variable entered into model. Significance level: p<0.05. All values n (%) unless otherwise stated
ADL = Activities of Daily Living; HOOS/KOOS = Hip disability and Osteoarthritis Outcome Score/Knee injury and Osteoarthritis Outcome Score; SD = standard deviation;
THA = total hip arthroplasty; TKA = total knee arthroplasty
Univariate analyses indicated that, for THA patients, age (p=0.012), level of educational level (p=0.006), self-employment (p=0.009), preoperative absence from work (p=0.002) and HOOS ADL baseline score (p=0.018) were significantly different between those who did not return to work or returned only partially and those who returned to work fully. A multivariable stepwise logistic regression model including age, educational level, preoperative work adaptions and baseline HOOS Pain, QoL and Sport subscale scores, showed that being self-employed (odds ratio [OR] 7.63, 95% CI 1.5–39.8), preoperative absence from work (OR 8.62, 95% CI 1.9–39.0) and a higher preoperative HOOS ADL score (OR 1.03, 95% CI 1.0–1.1) were statistically significantly associated with partial or no return to work.
In TKA patients, the only variable associated with a full return to work was change in KOOS Sport subscale score from baseline (p=0.039). In a multivariable exploratory logistic regression model that included the same preoperative variables as the THA model, only preoperative absence from work (OR 4.18, 95% CI 1.0–17.1) was associated with partial or no return to work.
Table 3 shows that, on univariate analysis, patients who did not or only partially returned to work were significantly more likely be older (p=0.010), have a lower level of education (p=0.043), be self-employed (p=0.019) and have preoperative absence from work (p=0.001), In contrast, the type of surgery (hip or knee) and other factors were not significantly associated with return to work.
Table 3.
Comparison of characteristics of 123 patients undergoing Total Hip Arthroplasty (THA, n=67) or Total Knee Arthroplasty (TKA, n=56) who returned to work either completely or incompletely or not 1 year after surgery
|
Full return to work N=93 |
Partial or no return to work)
N=30 |
P value* | Odds Ratio (95% CI)** | |
|---|---|---|---|---|
| Type of prosthesis, THA# | 53 (79) | 14 (21) | 0.400 | |
| Sex, female# | 52 (56) | 12 (40) | 0.146 | |
|
Mean age, years (SD)# 18–45 46–55 56–65 |
55 (6.1) 10 (11) 28 (30) 55 (59) |
58 (6.1) 2 (7) 3(10) 25 (83) |
0.010* | |
| Body mass index, mean (SD) | (N=92) 29 (5.9) | 29 (5.3) | 0.929 | |
|
Education level# Low Medium High |
(N=92) 21 (23) 42 (46) 29 (32) |
14 (47) 9 (30) 7 (23) |
0.043* |
|
| Self employed# | (N=85) 10 (12) | (N=28) 9 (32) | 0.019* | 6.68 (1.9–23.4) |
| Preoperative hours worked, mean (SD)# | 31 (11.6) | 35 (13.9) | 0.119 | |
|
Type of work# Light work Medium work Heavy work |
(N=85) 66 (78) 11 (13) 8 (9) |
(N=28) 22 (79) 5 (18) 1 (4) |
0.627 | |
| Preoperative absence from work due to hip or knee complaints# | (N=82) 19 (23) | (N=27) 16 (59) | 0.001* | 7.22 (2.4–21.5) |
| Preoperative work adaptions# | (N=68) 19 (28) | (N=24) 8 (33) | 0.795 | |
| Preoperative workers’ compensation# | (N=85) 7 (8) | (N=28) 4 (14) | 0.461 | |
|
Expectation over return to work Back to normal |
(N=76) 69 (91) |
(N=18) 15 (83) |
0.397 |
|
|
Baseline HOOS or KOOS, mean (SD)# ADL Pain Quality of life Sport Symptoms |
(N=85) 42 (16.1) (N=89) 36 (16.9) (N=89) 33 (9.5) (N=88) 11 (13.9) (N=90) 37 (17.5) |
(N=28) 46 (18.9) (N=29) 41 (21.5) (N=29) 31 (9.1) (N=29) 15 (18.5) (N=29) 36 (20.3) |
0.272 0.308 0.187 0.875 0.840 |
1.03 (1.0–1.1) |
|
Change in HOOS or KOOS, mean (95% CI) ADL Pain Quality of life Sport Symptoms |
(N=69) 46 (18.4) (N=74) 50 (19.8) (N=75) 18 (18.0) (N=73) 45 (28.8) (N=76) 32 (27.9 |
(N=25) 33 (22.3) (N=26) 41 (25.0) (N=24) 14 (16.0) (N=24) 33 (27.2) (N=26) 28 (37.8) |
0.008* 0.169 0.475 0.055* 0.341 |
|
| Oxford Knee/Hip Score, mean (SD) | (N=86) 24 (7.0) | (N=28) 24 (7.6) | 0.341 | |
| Oxford Knee/Hip change score, mean (95% CI) | (N=75) 18.7 (7.9) | (N=26) 14 (10.1) | 0.063 |
*Comparison of full return to work versus partial or no return to work patients using Chi-squared or Mann-whitney U test, where appropriate. Stepwise logistic regression analysis used to correct for type of prosthesis, including all significant associations.
**Univariate analysis
***Multivariable stepwise regression model
#variable entered into model. Significance level: p<0.05. All values n (%) unless otherwise stated
ADL = Activities of Daily Living; HOOS/KOOS = Hip disability and Osteoarthritis Outcome Score/Knee injury and Osteoarthritis Outcome Score; SD = standard deviation;
THA = total hip arthroplasty; TKA = total knee arthroplasty
Exploratory multivariable stepwise logistic regression taking into account prosthesis, sex, age, educational level, self-employment, preoperative working hours, type of job, absence from work, work adaptions, receipt of workers’ compensation and all baseline HOOS/KOOS subscale and OHS/OKS scores indicated that self-employment, preoperative absence from work and baseline HOOS/KOOS ADL subscale scores were associated with a return to work.
Following logistic regression analysis, only the interaction between prosthesis and the baseline HOOS/KOOS ADL subscale scores was found to be associated with return to work (p=0.023). A higher preoperative HOOS ADL subscale score was associated with partial or no return to work in THA patients (p=0.018), whereas in TKA patients the reverse association was seen, although this did not reach statistical significance (p=0.331).
Discussion
This prospective study showed that there are differences in the determinants of no or partial return to work 1 year after primary THA and TKA surgery. In THA patients, self-employment, preoperative absence from work and a better preoperative HOOS ADL subscale score were associated with partial or no return to work versus only preoperative absence from work in TKA patients. We also found that type of surgery (hip or knee) modifies the impact of preoperative HOOS/KOOS ADL subscale scores on return to work.
Few studies on the determinants of return to work following THA or TKA are available for comparison. Moreover, comparisons are hampered by the use of different definitions of work outcomes (number of hours before and after intervention, return to work yes/no, etc). Our finding that older age, lower educational level and preoperative absenteeism from work were associated with partial or no return to work appear to be in accordance with previous studies.5,7 In our analysis, self-employment was also found to be associated with partial or no return to work whereas it was associated with a faster return to work in previous research.16 It should be noted, however, that, in that study, the speed of return to work was the outcome, regardless the number of working hours. Our finding may be related to the observation that self-employed patients in all likelihood work more hours than wage earners and above the average for full-time workers (approximately 36–40 hours per week),17 yielding a larger potential for productivity loss. The observation that self-employed persons reported working hours exceeding the national average warrants the need to develop valid instruments to measure their productivity.
In contrast with previous studies, we did not find female gender, physical work and receiving workers’ compensation5,6,8 to be associated with worse work outcomes, which is most likely, again, due to differences in work outcome measurements.
Our study was unique in that we compared the determinants of partial or no return to work between THA and TKA, showing that preoperative absence from work was a factor in both groups. This can be identified easily in patients, allowing the provision of extra postoperative guidance to at-risk patients.
In the overall group, the preoperative HOOS/KOOS ADL score was found to be related to return to work. This was based on a better HOOS ADL score being significantly associated with partial or no return to work, whereas for the KOOS ADL score the reverse, yet non-significant, association was seen. Although not statistically significant, the direction of the association seen in TKA is in line with the literature.8 We have, however, no plausible explanation for the relationship seen in patients who underwent THA, other than that the average improvement in patients partially or not returning to work was relatively small compared to those who fully returned to work.
One of the main strengths of our study is that, in contrast with previous research, we included patients prospectively and provided multivariable analyses. Moreover, we included both patients with THA and TKA, and analyzed the results separately. We also looked at full return to work versus partial or no return to work. We showed that 13% of THA patients and 19% of TKA patients returned to work with a substantially reduction in working hours. It remains to be established the extent to which the reduction in working hours was related to THA or TKA, or can be explained by other factors.
Limitations of our study are that data were gathered by telephone interviews in the case of incomplete data on working hours or postoperative work status. Consequently, part of the information was gathered retrospectively, making it prone to recall bias. Second, only THA and TKA patients from one hospital in The Netherlands were included, while a multicentre study would have been preferable. However, given the patients’ baseline characteristics and their mean improvement in patient-reported outcomes, they appear to be a representative group of osteoarthritis patients undergoing THA or TKA.18-20 Third, we included a relative small sample size, as the majority of arthroplasty patients are not of working age at the time of surgery. Comparisons between full and no or partial return to work were therefore hampered by a lack of power.
Conclusions
Our study showed that, although the majority of patients return to work after THA or TKA, a considerable proportion of those work fewer hours postoperatively. Furthermore, preoperative absence from work is an important and modifiable determinant of partial or no return to work in both THA and TKA.
Self-employment plays a role in return to work following THA, whereas activities of daily living had the opposite effect in both THA and TKA. This latter finding implies that there are differences in the determinants of return to work following THA and TKA, warranting further research.
Conflicts of interest
None of the authors declare a conflict of interest.
Funding
This study was supported by the Anna Fonds/Nederlands Orthopedisch Research en Educatie Fonds [grant number 02012/09] and the Dutch Arthritis Association [grant number LLP13].
References
- 1.Mobasheri R, Gidwani S, Rosson JW. The effect of total hip replacement on the employment status of patients under the age of 60 years. Ann R Coll Surg Engl 2006; : 131–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lyall H, Ireland J, El-Zebdeh MY. The effect of total knee replacement on employment in patients under 60 years of age. Ann R Coll Surg Engl 2009; : 410–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurtz S, Ong K, Lau E et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007; : 780–785. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz S, Mowat F, Ong K et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg [Am] 2005; : 1,487–1,497. [DOI] [PubMed] [Google Scholar]
- 5.Tilbury C, Schaasberg W, Plevier JW et al. Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology (Oxford) 2014; : 512–525. [DOI] [PubMed] [Google Scholar]
- 6.Kuijer PP, de Beer MJ, Houdijk JH et al. Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: a systematic review. J Occup Rehabil 2009; : 375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kleim BD, Malviya A, Rushton S et al. Understanding the patient-reported factors determining time taken to return to work after hip and knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015; : 3,646–3,652. [DOI] [PubMed] [Google Scholar]
- 8.Sankar A, Davis AM, Palaganas MP et al. Return to work and workplace activity limitations following total hip or knee replacement. Osteoarthritis Cartilage 2013; : 1,485–1,493. [DOI] [PubMed] [Google Scholar]
- 9.Kuijer PP, Van der Molen HF, Frings-Dresen MH. Evidence-based exposure criteria for work-related musculoskeletal disorders as a tool to assess physical job demands. Work 2012; Suppl 1: 3,795–3,797. [DOI] [PubMed] [Google Scholar]
- 10.van den Akker-Scheek I, van Raay JJ, Reininga IH et al. Reliability and concurrent validity of the Dutch hip and knee replacement expectations surveys. BMC Musculoskelet Disord 2010; : 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nilsdotter AK, Lohmander LS, Klassbo M et al. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003; : 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003; : 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Groot IB, Reijman M, Terwee CB et al. Validation of the Dutch version of the Hip disability and Osteoarthritis Outcome Score. Osteoarthritis Cartilage 2007; : 104–109. [DOI] [PubMed] [Google Scholar]
- 14.Gosens T, Hoefnagels NH, de Vet RC et al. The “Oxford Heup Score”: the translation and validation of a questionnaire into Dutch to evaluate the results of total hip arthroplasty. Acta Orthop 2005; : 204–211. [DOI] [PubMed] [Google Scholar]
- 15.Haverkamp D, Breugem SJ, Sierevelt IN et al. Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop 2005; : 347–352. [PubMed] [Google Scholar]
- 16.Styron JF, Barsoum WK, Smyth KA et al. Preoperative predictors of returning to work following primary total knee arthroplasty. J Bone Joint Surg Am 2011; : 2–10. [DOI] [PubMed] [Google Scholar]
- 17.Meeste werknemers tevreden met aantal werkuren Centraal Bureau voor de Statistiek. https://www.cbs.nl/NR/rdonlyres/65E42E80-882C-4B11-AEA0-BFA49FB0BA6F/0/2012k1v4p20art.pdf (cited April 2016).
- 18.de Groot IB, Favejee MM, Reijman M et al. The Dutch version of the Knee Injury and Osteoarthritis Outcome Score: a validation study. Health Qual Life Outcomes 2008; : 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paulsen A, Roos EM, Pedersen AB et al. Minimal clinically important improvement (MCII) and patient-acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthop 2014; : 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 2003; : 17. [DOI] [PMC free article] [PubMed] [Google Scholar]