Abstract
Introduction
In 2013 our hospital introduced an in-hours, consultant-led, outpatient acute surgical clinic (ASC) for emergency general surgical patients. In 2014 this clinic was equipped with a dedicated ultrasonography service. This prospective cohort study evaluated this service before and after the introduction of ultrasonography facilities.
Methods
Data were recorded prospectively for all patients attending the clinic during 2013 and 2014. The primary outcome was patient destination (whether there was follow-up/admission) after clinic attendance.
Results
The ASC reviewed patients with a wide age range and array of general surgical complaints. In 2013, 186 patients attended the ASC. After the introduction of the ultrasonography service in 2014, 304 patients attended. In 2014, there was a reduction in the proportion of patients admitted to hospital from the clinic (18.3% vs 8.9%, p=0.002). However, the proportion of patients discharged after ASC review remained comparable with 2013 (30.1% in 2013 vs 38.8% in 2014, p=0.051). The proportion of patients undergoing computed tomography (CT) scans also fell (14.0% vs 4.9%, p<0.001).
Conclusions
The ASC assessed a wide array of general surgical complaints. Only a small proportion required hospital admission. The introduction of an ultrasonography service was associated with a further reduction in admission rates and computed tomography.
Keywords: General surgery, Outpatients, Emergencies, Ultrasonography, Ambulatory care facilities
The National Health Service is under increasing pressure to deliver efficient, high quality and financially viable care to patients in the community and in the secondary care setting.1 This pressure extends to general surgery departments across the UK.
A report in October 2013 on non-elective care at University Hospitals Coventry and Warwickshire NHS Trust highlighted opportunities for the improvement of emergency care in our hospital (unpublished work). It noted that many patients were admitted to hospital unnecessarily and that an increase in discharges was required. The paper emphasised a need for accessible ‘hot clinics’ to allow outpatient management of patients who may otherwise be admitted to hospital unnecessarily.
From January 2013, a consultant-led, in-hours, outpatient, acute surgical clinic (ASC) was introduced at our hospital. This clinic had several projected aims:
The ASC would allow the on-call surgical team to arrange for general surgical patients to be discharged home after their emergency department (ED) review, in order to reattend the ASC for prompt follow-up, without the need for admission.
The ASC would allow the early review of patients discharged from a surgical ward after an inpatient stay. This would give teams the freedom to discharge patients without the risk of having to wait long periods of time for follow-up.
Starting in January 2014, the ASC was equipped with a dedicated ultrasonography facility to allow early radiographic assessment of patients. Six daily ultrasonography slots were agreed on after discussion with the radiography department.
Further details on the conduct of the clinic are set out in Figure 1.
Figure 1.
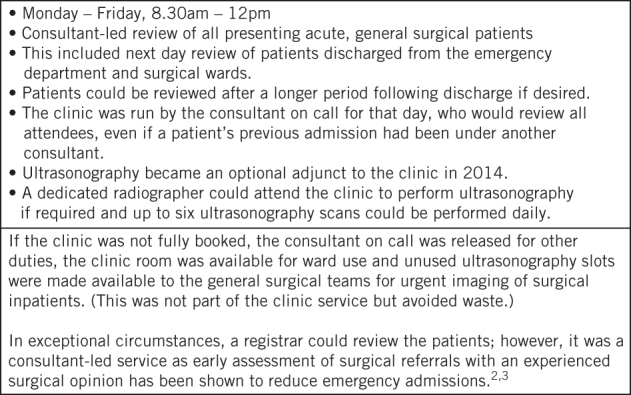
Conduct of an outpatient acute surgical clinic with ultrasonography facilities for the early evaluation of general surgical patients
The aims of this prospective, comparative, cohort study were to evaluate the outcomes of patients who attended the clinic and to examine any change in patient destination after clinic attendance that may have occurred after the introduction of the ultrasonography service.
Methods
Institutional review board approval for the work was granted by the trust’s Quality and Effectiveness Department, which affirmed its nature as a service evaluation. The study was conducted in compliance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement.4 Data were gathered prospectively by the ASC team for all patients attending the clinic at our hospital general surgical department between 1 January 2013 and 31 December 2014. A retrospective case note review was performed to supplement these data.
The minimum sample size required for statistical power was not calculated because of the observational study design. All patients who attended the ASC were considered eligible for inclusion in the study. Duplicate attendances and records without a patient number or date were excluded. All data were extracted for each patient from the written records kept by the ASC staff and substantiated with the electronic records held centrally by the Clinical Results Reporting System.
The primary outcome was the patients’ destinations after their clinic review (Fig 2). The secondary outcomes were patient demographics, their presenting complaints, whether imaging was requested, the type of imaging that was arranged, the radiographic findings and whether a formal clinic letter or discharge summary was generated. The existence of a letter was not essential for extraction of the primary outcome. Data collection was complete by March 2015.
Figure 2.
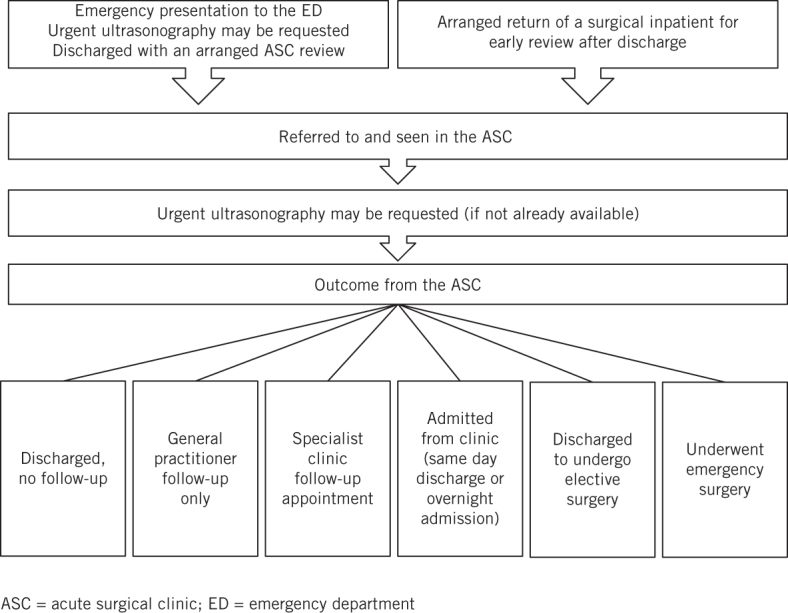
Care pathway prior to and after attending the ASC
Statistical analysis
Statistical comparison of the two cohorts from 2013 and 2014 was performed using a chi-squared test for categorical data and a two-tailed unpaired Student’s t-test for continuous data with Excel® 2007 (Microsoft, Redmond, WA, US). Data are reported for subgroups of our cohort (those who presented for an ultrasonography review, those who underwent imaging and those who underwent emergency surgery). However, these subgroups were not specified a priori and to avoid reporting bias, these groups were not tested statistically against the wider cohort.
Results
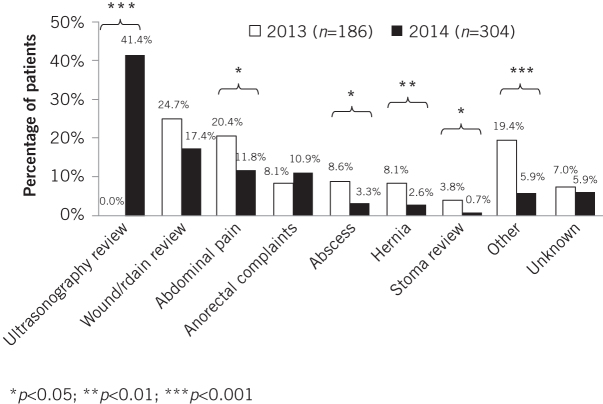
During 2013, 186 patients attended the ASC (a mean average of 15.5 patients per month and 3.6 patients a week) while in 2014, 304 patients attended (a mean average of 25.3 patients per month and 5.8 patients a week). A clinic or discharge letter was available for 118 patients (63.4%) in 2013 and 141 patients (46.4%) in 2014. The demographics, presentation, discharge destination after ASC review and imaging of the two cohorts are compared in Tables 1–3 and Figures 3–5.
Table 1.
Demographics and presentation of patients attending the acute surgical clinic
| 2013 | 2014 | Both years | p-value* (2013 vs 2014) | |
|---|---|---|---|---|
| Male | 83 (44.6%) | 104 (34.2%) | 187 (38.2%) | 0.021 |
| Female | 103 (55.4%) | 200 (65.8%) | 303 (61.8%) | |
| Median age in years | 45.3 | 43.7 | 43.9 | 0.202 |
| Age range in years | 11.8–89.8 | 17.3–91.9 | 11.8–91.9 | – |
| Presentation | ||||
| Ultrasonography review | 0 (0%) | 126 (41.4%) | 126 (25.7%) | <0.001 |
| Wound/drain review | 46 (24.7%) | 53 (17.4%) | 99 (20.2%) | 0.051 |
| Abdominal pain | 38 (20.4%) | 36 (11.8%) | 74 (15.1%) | 0.010 |
| Anorectal complaints | 15 (8.1%) | 33 (10.9%) | 48 (9.8%) | 0.313 |
| Abscess | 16 (8.6%) | 10 (3.3%) | 26 (5.3%) | 0.011 |
| Hernia | 15 (8.1%) | 8 (2.6%) | 23 (4.7%) | 0.006 |
| Stoma review | 7 (3.8%) | 2 (0.7%) | 9 (1.8%) | 0.013 |
| Other | 36 (19.4%) | 18 (5.9%) | 54 (11.0%) | <0.001 |
| Unknown | 13 (7.0%) | 18 (5.9%) | 31 (6.3%) | 0.637 |
| Total | 186 (100%) | 304 (100%) | 490 (100%) | – |
*Chi-squared test for categorical data; two-tailed unpaired Student’s t-test for continuous data
Table 3.
Imaging arranged via the acute surgical clinic
| Imaging | 2013 | 2014 | Both years | p-value* (2013 vs 2014) |
|---|---|---|---|---|
| Ultrasonography (abdomen / groin / KUB) | 39 (21.0%) | 136 (44.7%) | 175 (35.7%) | <0.001 |
| CT (abdomen / pelvis) | 26 (14.0%) | 15 (4.9%) | 41 (8.4%) | <0.001 |
| MRI (abdomen) | 2 (1.1%) | 5 (1.6%) | 7 (1.4%) | 0.606 |
| Breast ultrasonography / mammography | 3 (1.6%) | 1 (0.3%) | 4 (0.8%) | 0.125 |
| Plain radiography | 2 (1.1%) | 1 (0.3%) | 3 (0.6%) | 0.304 |
| Other | 1 (0.5%) | 1 (0.3%) | 2 (0.4%) | 0.725 |
| Total | 73 (39.2%) | 159 (52.3%) | 232 (47.3%) | – |
CT = computed tomography; MRI = magnetic resonance imaging; KUB = kidneys, ureters and bladder
*Chi-squared test
Figure 3.
Presenting complaints at attendance to the acute surgical clinic
Figure 5.
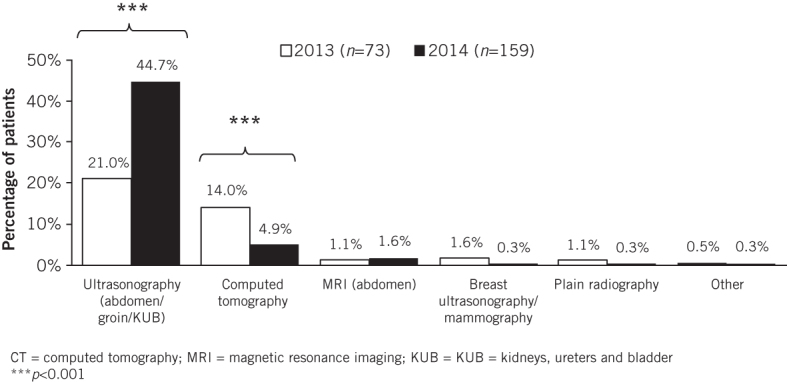
Imaging arranged through the acute surgical clinic
Table 2.
Patient destination after clinic review
| Destination | 2013 | 2014 | Both years | p-value* (2013 vs 2014) |
|---|---|---|---|---|
| Discharged without follow-up | 56 (30.1%) | 118 (38.8%) | 174 (35.5%) | 0.051 |
| General practitioner follow-up | 9 (4.8%) | 8 (2.6%) | 17 (3.5%) | 0.195 |
| Clinic appointment follow-up | 75 (40.3%) | 142 (46.7%) | 217 (44.3%) | 0.167 |
| Discharged to undergo elective surgery | 12 (6.5%) | 9 (3.0%) | 21 (4.3%) | 0.064 |
| Admitted from clinic | 34 (18.3%) | 27 (8.9%) | 61 (12.4%) | 0.002 |
| Admitted and discharged that day | 12 (6.5%) | 3 (1.0%) | 15 (3.1%) | <0.001 |
| Admitted overnight | 22 (11.8%) | 24 (7.9%) | 46 (9.4%) | 0.147 |
| Admitted for emergency surgery | 14 (7.5%) | 11 (3.6%) | 25 (5.1%) | 0.056 |
| Total | 186 (100%) | 304 (100%) | 490 (100%) | – |
*Chi-squared test
Figure 4.
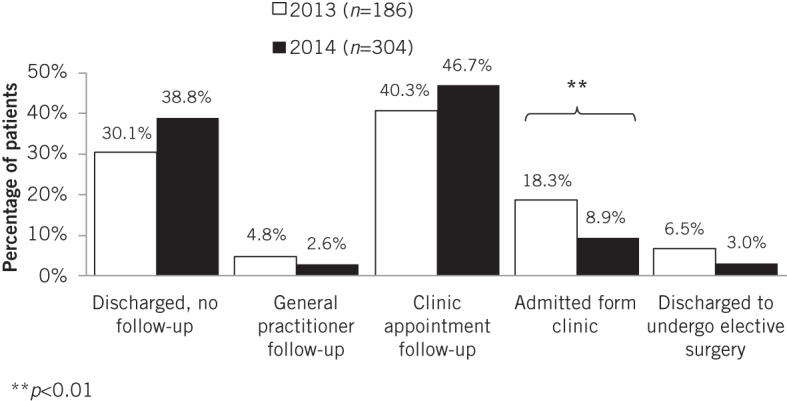
Destination of patients after attendance at the acute surgical clinic
In 2014, 126 patients presented for an ultrasonography review (Table 1). These patients had been reviewed (usually in the ED), had undergone ultrasonography and returned to the clinic for clinical assessment with the results of the ultrasonography. Of these, 68 patients (54.0%) had normal imaging, 21 (16.7%) had gallstones, 18 (14.3%) had ovarian cysts, 2 (1.6%) had collections, 1 (0.8%) had a malignancy and 10 (7.9%) had other findings. In six patients (4.8%), the results were not known (unrecorded). After clinic review, 64 patients (50.8%) were discharged without follow-up, 3 (2.4%) were followed up by their general practitioner, 54 (42.9%) were followed up in a specialist outpatient clinic, 1 (0.8%) was discharged to undergo elective surgery and 4 (3.2%) were admitted from clinic. One of these four patients underwent emergency surgery (for appendicitis).
Over the 2-year study period, 232 patients underwent radiological imaging. The majority of these (n=126, 54.3%) had attended the ASC for an ultrasonography review (only available for those patients attending in 2014). Among the remaining patients, 54 (23.3%) underwent imaging for abdominal pain, 17 (7.3%) for other complaints, 16 (6.9%) for a wound review, 7 (3.0%) for a hernia, 5 (2.2%) for an abscess, 4 (1.7%) for a stoma review and 3 (1.3%) for anorectal complaints.
The results of the imaging were normal for 115 patients (49.6%) while 28 (12.1%) had gallstones, 19 (8.2%) had ovarian cysts, 15 (6.5%) had collections, 5 (2.2%) had abscesses, 4 (1.7%) had malignancy and 35 (15.1%) had other findings. For 11 patients (4.7%) the imaging results were unknown (unrecorded). Of the 73 patients who underwent imaging in 2013, 34 (46.6%) had normal imaging findings. In 2014, 159 patients underwent imaging and 81 (50.9%) had normal findings. There was no statistically significant difference between the two cohorts.
Of the 25 patients admitted for emergency surgery, the majority had presented to the ASC with an abscess (n=8, 32.0%). Four patients presented with abdominal pain (16.0%), four with hernias (16.0%), three presented for a wound review (12.0%), two had anorectal complaints (8.0%), two had other complaints (8.0%), one attended for a stoma review (4.0%) and one attended for an ultrasonography review (4.0%). Data were not collected on the operations they underwent. Seven of the patients who were admitted for emergency surgery underwent imaging as part of their management. Of these, the imaging results showed appendicitis (n=1), an enterocutaneous fistula (n=1), an abscess (n=1), free fluid (n=1), colitis (n=1) and normal imaging findings (n=1). The results were unknown/unrecorded in one patient.
For the 2013 calendar year from 1 April 2013 to 31 March 2014, 1,494 inpatient ultrasonography scans were performed for general surgical departments at our hospital (data sourced by our Performance and Programme Management Office). In the ASC, there was capacity for 6 ultrasonography slots a day, 5 days per week for 52 weeks per year (1,560 ultrasonography scans per year, without accounting for leave, bank holidays etc). In 2014, 136 patients attending the ASC underwent ultrasonography. Any redundancy in the service and any unused ultrasonography slots became available to general surgical inpatients, reducing any waste (Fig 1).
Discussion
Our unit is a busy tertiary referral centre, trauma unit and general surgical hospital. This is demonstrated by data sourced by our Performance and Programme Management Office: between 1 April 2013 and 31 March 2014, 176,483 patients presented to the ED and 5,421 were admitted under general surgical specialties (breast, colorectal, general, upper gastrointestinal or vascular surgery, or urology). A total of 6,964 inpatient ultrasonography scans were performed throughout the hospital during this period and 1,494 of these were requested by general surgical specialties.
Our hospital faced significant challenges in 2013, adopting a drive to reduce unnecessary admissions and inpatient stay. The general surgical department adapted with the introduction of the ASC, allowing acute surgical patients to be investigated in the ED, reviewed, safely discharged and then followed up promptly without compulsory admission to hospital. Patients who were admitted and then discharged home were reviewed early to avert emergency readmission. This was complemented by the introduction of an in-clinic ultrasonography service in 2014.
The prevention of unnecessarily acute surgical admissions by discharging patients from an assessment unit is a viable cost saving measure.2 However, evaluation of outpatient follow-up of emergency surgical patients presenting to the ED has not been well reported in the literature.5 Onur et al conducted a randomised controlled trial showing that patients presenting to the ED with acute non-specific abdominal pain who were discharged home and followed up daily displayed no significant differences in either complications or morbidity compared with those admitted to hospital for observation.6 Outpatient follow-up was deemed a safe course of management for these patients. This work supports the use of our ASC and is consistent with our findings that the majority of patients referred to our clinic could be managed without admission (88% of the cohort over two years).
Toorenvliet et al commented that review of surgical patients in an acute clinic would allow disease that has progressed to be identified more reliably whereas symptoms of mild, self-limiting disease would regress.5 They prospectively evaluated patients presenting to the ED with acute abdominal pain who were not admitted to hospital but were asked to reattend a consultant-led outpatient clinic after 24 hours for re-evaluation. Following this re-evaluation, 46% were discharged home after only one visit to the clinic while 17% of reattending patients had their management plan changed, with 4% requiring a laparotomy (where previously only outpatient follow-up had been arranged). The proportion of our patients discharged without a need for follow-up review was similar in both years of our study, supporting the findings of Toorenvliet et al that many of these patients can be discharged after just one appointment.5
Early assessment of acute surgical referrals coupled with an experienced surgical opinion reduces emergency admissions.2,3 The appointment of a dedicated emergency surgical consultant at one unit significantly shortened the hospital stay for emergency admissions.7 Urgent consultant opinion (either in the ED or in clinic) would have prevented almost all unnecessary acute surgical admissions in another unit.8 Our ASC is consultant-led, which may explain our low admission rates.
Use of imaging in the acute surgical setting is widespread. Ultrasonography is non-invasive, inexpensive and increasingly popular. While it improves the diagnostic accuracy of abdominal pain,9 the controversies around this are outside the scope of this paper. Grubel examined the use of ultrasonography by gastroenterologists and found that abdominal pain was the most common presenting complaint among patients who subsequently underwent ultrasonography performed in an outpatient gastroenterology clinic.10 In Grubel’s study, almost half (48%) of all ultrasonography was normal. Our rates of normal imaging (49.6% of all scans performed) are comparable. Centres that have employed ultrasonography in the ED to investigate paediatric abdominal pain have shown that ultrasonography is diagnostic in 45% of cases and prevented laparotomy in 20%.11
There was no significant difference in the proportion of imaging that detected no abnormality in 2013 compared with 2014 (after the introduction of the ultrasonography service). It seems that easier access to ultrasonography has not worsened the ability of clinicians to assess which patients are likely to have pathology and therefore require imaging. Our high rates of normal imaging could suggest that more emphasis should be placed on appropriate patient selection so as to avoid unnecessary imaging. On the other hand, negative imaging results are likely to improve clinician confidence with a diagnosis of normality.
Since the introduction of the ultrasonography service, there has been a significant reduction in the proportion of patients admitted from clinic. This could be due to satisfactory outpatient investigation with ultrasonography that no longer warrants admitting patients to acquire appropriate imaging results. In 2014 there was also a rise in those patients attending for the results of their ultrasonography, with a proportionate drop in other presenting complaints. This can be explained by those patients who were seen in the ED, referred for ultrasonography by the on-call team and then reviewed in the clinic the next day.
No ultrasonography service was present at our ASC in 2013, and we acknowledge the limits of comparing data from 2013 and 2014. The proportion of ultrasonography organised through the clinic increased significantly in 2014. This was accompanied by a reduction in computed tomography (CT) and therefore a reduction in patient exposure to ionising radiation. In one study, CT for patients with non-traumatic abdominal pain in the ED reportedly averted 24% of hospital admissions that would have otherwise taken place without the imaging.12 However, as described previously, the move to more ultrasonography and less computed tomography at our unit did not result in increased admissions or emergency operations. We therefore advocate the use of ultrasonography in an ASC setting to reduce the frequency of CT where it is not required and to assist with appropriate discharge.
Study limitations
Our study is limited by the observational study design. There were also inherent differences between the 2013 and 2014 cohorts that mean the results should be judged cautiously. Other factors may have led to the observed service improvement over time. A ‘learning curve’ may have existed (consultants may have become more confident in safely discharging patients home over time) or the clinic may have been increasingly used to review patients with ultrasonography who may have otherwise been discharged home without investigation.
The reduction in CT use may have been a dilutional effect. More ultrasonography being undertaken may have reduced the proportion of patients undergoing CT but it did not result in a fall in the number of other imaging modalities requested, even though numbers were small. We also note that the proportion of patients presenting with abdominal pain in 2014 was lower than in 2013. However, we do not believe that this represents a true reduction in patients presenting with abdominal pain as this observation could be explained by patients with abdominal pain in 2014 presenting to the ED, undergoing ultrasonography and then presenting to the ASC for an ‘ultrasonography review’.
We acknowledge that in cases where no documented evidence was found that follow-up had been arranged, it was assumed that no routine follow-up had taken place and that the patient had been discharged. Nevertheless, our extensive review of the patients’ electronic records will have reduced the number of patients with incomplete data.
It is not possible to comment on the cost effectiveness of the service as this was not part of the remit of this study; however, subsequent work could examine the financial impact of such services to further assess their value. Additional work could also seek feedback from patients and general practitioners as this information was not sought by our study but may provide valuable qualitative data in the future.
Conclusions
An ASC allows patients a timely consultant review with early, focused management plans while limiting unnecessary or prolonged inpatient admissions. A large number of patients attended over the study period and this increased over time. The clinic reviewed a wide array of general surgical complaints. Low numbers of patients were admitted from clinic or required emergency surgery.
The introduction of an ultrasonography service was associated with a reduction in patient admissions and in the proportion of patients undergoing CT. Our results support the use of a locally implemented ASC to improve the efficiency of an emergency general surgery on-call service.
Acknowledgements
The authors are grateful to Anna Brown (Library and Knowledge Services, University Hospitals Coventry and Warwickshire NHS Trust [UHCW]), who performed an initial literature search for relevant academic papers, and to Anwar Shaikh (Performance and Programme Management Office, UHCW), who provided data on hospital-wide imaging.
The material in this article was presented in part at meetings of the Association of Surgeons of Great Britain and Ireland held in Harrogate, May 2014, and in Manchester, April 2015, as well as at meetings of the West Midlands Surgical Society held in Birmingham, May 2014 and November 2014. No funding was received for this work. None of the authors have any conflicts of interest to declare.
References
- 1.Kumar R, DeBono L, Sharma P, Basu S. The general surgical care practitioner improves surgical outpatient streamlining and the delivery of elective surgical care. J Perioper Pract 2013; : 138–141. [DOI] [PubMed] [Google Scholar]
- 2.Dookeran KA, Bain I, Moshakis V. Audit of general practitioner referrals to a surgical assessment unit: new methods to improve the efficacy of the acute surgical service. Br J Surg 1996; : 1,544–1,547. [DOI] [PubMed] [Google Scholar]
- 3.Gaskell DJ, Lewis PA, Crosby DL et al. Improving the primary management of emergency surgical admissions: a controlled trial. Ann R Coll Surg Engl (Suppl) 1995; : 239–241. [PubMed] [Google Scholar]
- 4.von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014; : 1,495–1,499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toorenvliet BR, Bakker RF, Flu HC et al. Standard outpatient re-evaluation for patients not admitted to the hospital after emergency department evaluation for acute abdominal pain. World J Surg 2010; : 480–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Onur OE, Guneysel O, Unluer EE et al. ‘Outpatient follow-up’ or ‘active clinical observation’ in patients with nonspecific abdominal pain in the emergency department. A randomized clinical trial. Minerva Chir 2008; : 9–15. [PubMed] [Google Scholar]
- 7.Sorelli PG, El-Masry NS, Dawson PM, Theodorou NA. The dedicated emergency surgeon: towards consultant-based acute surgical admissions. Ann R Coll Surg Engl 2008; : 104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Denman-Johnson M, Bingham P, George S. A confidential enquiry into emergency hospital admissions on the Isle of Wight, UK. J Epidemiol Community Health 1997; : 386–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allemann F, Cassina P, Röthlin M, Largiadér F. Ultrasound scans done by surgeons for patients with acute abdominal pain: a prospective study. Eur J Surg 1999; : 966–970. [DOI] [PubMed] [Google Scholar]
- 10.Grubel P. Evaluation of abdominal ultrasound performed by the gastroenterologist in the office. J Clin Gastroenterol 2011; : 405–409. [DOI] [PubMed] [Google Scholar]
- 11.Khalid M, Redhu N, Nazir B et al. Diagnostic value of ultrasonography in evaluation and management of acute abdominal conditions in the paediatric age group. Afr J Paediatr Surg 2012; : 198–201. [DOI] [PubMed] [Google Scholar]
- 12.Rosen MP, Sands DZ, Longmaid HE et al. Impact of abdominal CT on the management of patients presenting to the emergency department with acute abdominal pain. Am J Roentgenol 2000; : 1,391–1,396. [DOI] [PubMed] [Google Scholar]