Abstract
Introduction
Surgical procedures to manage trauma to the wrist, forearm and elbow in children are very common. Image intensifiers are used routinely, yet studies/guidelines that quantify expected radiation exposure in such procedures are lacking.
Methods
Information on demographics, injury type, surgeon grade and dose area product (DAP) of radiation exposure per procedure was collected prospectively for 248 patients undergoing manipulation/fixation of injuries to the elbow, forearm or wrist at a paediatric hospital over 1 year.
Results
DAP exposure (in cGycm2) differed significantly across different procedures (p<0.001): wrist manipulation under anaesthesia (MUA; median, 0.39), wrist k-wiring (1.01), forearm MUA (0.50), flexible nailing of the forearm (2.67), supracondylar fracture MUA and k-wiring (2.23) and open reduction and internal fixation of the lateral humeral condyle (0.96). Fixation of a Gartland grade-3 supracondylar fracture (2.94cGycm2) was associated with higher exposure than grade-2 fixation (1.95cGycm2) (p=0.048). Fractures of the wrist or forearm necessitating metalwork fixation resulted in higher exposure than those requiring manipulation only (both p<0.001). For procedures undertaken by trainees, trainee seniority (between year-5 and year-8 and clinical fellow, p≥0.24) did not affect the DAP significantly.
Conclusions
The spectrum of radiation exposures for common procedures utilised in the management of paediatric upper limb trauma were quantified. These findings will be useful to surgeons auditing their practice and quantifying radiation-associated risks to patients. Our data may serve as a basis for implementing protocols designed to improve patient safety.
Keywords: Paediatric, Image intensifier, Radiation exposure, Upper limb, Trauma
Fractures of the upper limb are the most common fractures observed in children.1 Fractures of the distal radius, forearm and supracondylar humerus alone account for ≈50% of bony injuries in childhood.1,2 Manipulation and fixation of these fractures are, therefore, among the most common procedures undertaken in children.1 Confirmation of accurate reduction of the fracture and fragment fixation necessitates radiography with C-arm image intensifiers. These portable machines allow real-time radiographic review of anatomical structures, but raise concerns with regard to radiation exposure.3–5
Only a few studies have quantified the relative exposure to radiation using different spatial C-arm configurations.6–8 Studies on quantification of the absolute radiation exposure that patients can expect for common index procedures to manage upper-limb trauma in children are lacking, making it difficult to set standards and assess performance. Surgeons have a responsibility to provide the best possible care and to avoid the harmful effects of medical intervention. The primary concern is to achieve adequate fracture reduction (and, if required, fixation) but the amount of radiation exposure should also be a concern to surgeons. Junior and senior doctors have been reported to have poor awareness of the radiation doses associated with medical imaging.9 Surgeons may, on occasion, suspect that a particular procedure has necessitated considerable amounts of radiation but cannot quantify radiation exposure with respect to population norms.
We wished to quantify radiation exposure for the most commonly undertaken procedures for upper-limb trauma in children. A secondary aim was to ascertain if injury-related or surgeon-related factors influence radiation exposure.
Methods
In this cross-sectional study, data were collected prospectively on all patients undergoing manipulation/fixation of injuries to the elbow, forearm or wrist at the Royal Hospital for Sick Children (RHSC; Edinburgh, UK) between June 2013 and June 2014. Patients underwent open or closed treatment in an operating theatre (at the time of this study, paediatric fractures were not manipulated under local anaesthesia or sedation in the emergency department of the RHSC). The image intensifier was operated by a radiographer in all cases. Information on patient demographics, injury type, surgeon grade and the dose area product (DAP) of radiation exposure (measured in centiGray square centimetres (cGycm2)) per procedure was recorded for all cases. The DAP was measured by an inbuilt DAP meter on the image intensifier. Imaging was undertaken using Arcadis Varic image intensifiers (Siemens, Munich, Germany). A pulsed method (one pulse per second) was employed, and the dose, brightness and contrast were optimised automatically during image acquisition. Procedures were undertaken by 16 surgeons: 10 orthopaedic trainees between the fifth (ST5) and eighth year of orthopaedic training (ST8), a staff grade, a clinical fellow, and four consultants.
Statistical analyses
Statistical analyses were undertaken using SPSS v22 (IBM, Armonk, NY, USA). Shapiro–Wilk testing and Q–Q plots demonstrated that data for radiation exposure did not have a normal distribution. Non-normally distributed continuous data are reported with median values and ranges, and were analysed across groups using the independent-sample Kruskal–Wallis test (ISKWT) if there were more than two groups and the independent-sample Mann–Whitney U-test (ISMWUT) if there were two groups. Spearman’s rank co-efficient was used to assess the relationship between training year and radiation exposure for an individual procedure. p<0.05 was considered significant.
Results
Two hundred and forty-eight patients underwent 259 procedures on the humerus, radius or ulna for trauma during the study period (Table 1). There were 169 males and 79 females with a median age of 7 years at the time of injury (interquartile range, 5 years) and 107 right-sided, 148 left-sided and 2 bilateral procedures. The primary surgeon was identifiable in 241 cases (93%) and two primary surgeons were identified in 1 case (0.4%). The primary surgeon could not be identified in 17 cases (6.6%). Of those with a single identified primary surgeon, 92% of procedures were done by trainee surgeons, and a consultant was present in 40% of cases.
Table 1.
Procedures for management of upper-limb trauma undertaken during the study period
| Procedure | Number of cases |
|---|---|
| MUA + POP distal radius | 45 |
| MUA + k-wiring distal radius | 57 |
| MUA + POP forearm | 56 |
| MUA + flexible nails forearm | 13 |
| ORIF forearm (plates and screws) | 3 |
| Radial head MUA | 2 |
| Radial head flexible nail manipulation | 3 |
| Open reduction elbow | 1 |
| MUA + k-wiring supracondylar fracture | 60 |
| Open reduction supracondylar fracture | 2 |
| ORIF humeral lateral condyle | 13 |
| ORIF medial condyle | 1 |
| ORIF medial epicondyle | 1 |
| EUA wrist* | 1 |
| EUA elbow* | 1 |
MUA = manipulation under anaesthesia; POP = plaster of Paris; ORIF = open reduction and internal fixation; EUA = examination under anaesthesia.
*Both EUA were undertaken at the same time as other procedures.
Eleven patients underwent more than one procedure simultaneously and were excluded from calculations relating radiation exposure to injury type because the amount of radiation attributable to each injury could not be differentiated. Therefore, radiographic exposures were analysed for 237 procedures in 237 patients.
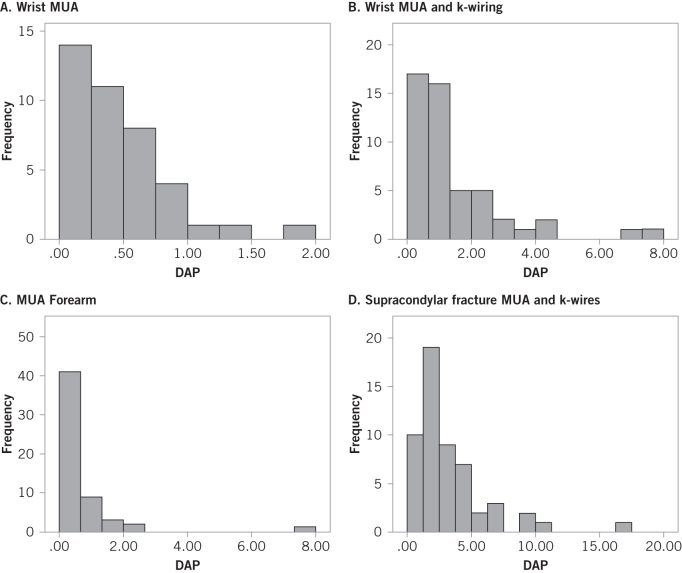
Median DAP exposures for various upper-limb injuries in the paediatric population are quantified (Table 2,Fig 1) and reported together with the range (absolute range and interquartile range) of experienced exposures. Differences in exposure across the procedure types were significant (p<0.001, ISKWT). Fractures of the forearm (p<0.001, ISMWUT) and wrist (p<0.001, ISMWUT) necessitating fixation with metalwork were associated with higher exposure to radiation than their counterparts at the same anatomical sites necessitating manipulation only.
Table 2.
Dose area product exposure (in cGycm2) for procedures to manage upper-limb trauma in children
| N | Median exposure (50th percentile) | 25th Percentile | 75th Percentile | Range | |
|---|---|---|---|---|---|
| MUA distal radius | 40 | 0.39 | 0.19 | 0.64 | 0.08–1.98 |
| Wrist k-wiring | 50 | 1.01 | 0.56 | 1.93 | 0.25–7.41 |
| Forearm MUA | 56 | 0.50 | 0.26 | 0.68 | 0.04–7.65 |
| Forearm flexible nailing | 13 | 2.67 | 1.38 | 5.27 | 0.36–11.29 |
| Open reduction and k-wires elbow | 2 | 6.58* | |||
| MUA + k-wires Supracondylar | 54 | 2.23 | 1.50 | 3.92 | 0.47–17.23 |
| ORIF lateral humeral condyle | 13 | 0.96 | 0.62 | 2.32 | 0.30–3.11 |
MUA = manipulation under anaesthesia; ORIF = open reduction and internal fixation
*This value is based on two procedures and should be interpreted with caution.
Figure 1.
Graphs showing distribution of measured dose area product (cGycm2) for wrist manipulation under anaesthesia (MUA) (a), wrist k-wiring (b), forearm MUA (c) and supracondylar MUA + k-wiring (d)
For procedures carried out primarily by a trainee, we could not identify a correlation between year in training (ST5–ST8 or clinical fellow) and radiation exposure for any procedure type (Spearman’s rank correlation coefficient): wrist manipulation under anaesthesia (MUA) (ρ=0.03; p=0.85), wrist k-wiring (ρ=–0.19; p=0.24), forearm MUA (ρ=0.04; p=0.81), supracondylar MUA and k-wiring (ρ=0.14; p=0.39). These analyses were not undertaken on fixation of the lateral condyle, flexible nailing of the forearm, or open supracondylar fixation due to the relatively small numbers of these procedures.
Supracondylar fractures were graded according to the Gartland classification system.10 Only type-2 and type-3 fractures were encountered because Gartland type-1 fractures are managed by non-surgical methods. Radiation exposure (in cGycm2) was higher (p=0.048, ISMWUT) in Gartland type-3 injuries (median, 2.94; 25th percentile, 1.74; 75th percentile, 6.21; range, 0.67–17.23) than Gartland type-2 injuries (1.96; 1.30; 3.42; 0.47–8.88).
Discussion
Radiation exposure for commonly undertaken paediatric trauma procedures was quantified over a range of cases carried out by multiple surgeons. Fractures of the wrist or forearm necessitating fixation were associated with higher radiation exposure than those requiring manipulation only. Supracondylar fractures with more severe fracture patterns were associated with higher exposure to radiation.
Radiographs are used to guide reduction and fixation of fractures in the operating theatre. They are linked to potential risks, including carcinogenesis,11 and these risks are higher in children.12 UK legislation mandates periodic audit of practice relating to medical exposure to ionising radiation,13 whereas European Union legislation14 requires use of diagnostic reference levels (DRLs). DRLs for departmental radiographs are available widely,15–17 and provide useful standards against which to audit practice. However, data for C-arm image intensifiers are lacking. Three diagnostic procedures (none of which are orthopaedic) are included in UK guidelines,16–17 but studies/guidelines that quantify radiation exposure in procedures for upper-limb fractures are lacking. This hiatus raises concerns about the ability to audit practice and to quantify exposure risks to patients. Clinicians have been reported to have poor insight into radiation exposure associated with medical imaging,9 but improving awareness is challenging in the absence of guidelines or studies characterising expected radiation exposure. The DAP is calculated by multiplying radiation dose by irradiation area, and 75th-percentile values are used to determine the DRL.12,16–19 The DAP is a more reliable indicator of overall stochastic risk of adverse events (eg induction of cancer) than the dose in isolation.20 Image intensifiers are fitted with DAP meters, which facilitates monitoring.
At the RHSC, the DAP associated with a chest radiograph is 13cGycm2 for those aged 1–5 years and 25cGycm2 for those aged 6–10 years. Exposures for upper-limb trauma are, in general, relatively low. The highest recorded exposure in our series (17.23cGycm2 for a supracondylar fracture MUA and k-wiring) equates to approximately one chest radiograph, which is known to be associated with a low stochastic risk of inducing malignancy (1.3 per one million males and 1.9 per one million females).12 However, unnecessary risks must be minimised and furthermore the legal/ethical requirements for audit and monitoring discussed above are not absolved by the relatively low radiation doses in these procedures.
Our finding that different procedures are associated with different radiation exposures are unsurprising: a supracondylar fracture and distal radial fracture present different management challenges and degrees of complexity. Observed variations in exposure for individual procedure types may be due (at least in part) to varying degrees of injury complexity, as demonstrated by the association between radiation exposure and Gartland grade of supracondylar fractures. Higher exposures were observed in fractures necessitating fixation, which may reflect increased instability or use of radiation to monitor metalwork placement in these fractures.
We acknowledge that these results represent the experience from a single institution and, therefore, may not be entirely representative of the experience of other institutions. However, the reported values represent practice by several surgeons, and the fracture-management protocols they used are not controversial. We hope that our study will raise awareness of the importance of monitoring radiation use in the operating theatre. We also hope that it will stimulate more widespread data collection, which would facilitate data pooling to enable formation of UK guidelines. Such data and standards would facilitate audit of practice and enable surgeons to identify cases in which large amounts of radiation are used. Surgeons who consistently use larger amounts of radiation than their colleagues should re-examine their practice to ascertain if such use is justified (eg complex subspecialist practice) or whether measures to reduce over-exposure are required. Training in reduction of radiation exposure may be required if high exposures are not justified.
Some authors have suggested protocols in which the surgeon is informed intra-operatively if specific threshold exposures have been surpassed, and for mandatory review of each case surpassing the 95th percentile, to ascertain if the exposure was justified.21 These measures could improve surgeon awareness and patient safety. We have instituted a similar system at the RHSC, and discuss outlying cases at morbidity and mortality meetings. Higher radiation doses may be justified (eg in complex cases) and case review does not necessarily imply wrongdoing. Discussion of such cases could provide excellent learning opportunities (or identify deficiencies that can be addressed).
We could not identify a relationship between trainee seniority (second half of training) and radiation exposure. Junior trainees do not work at the RHSC, and these findings must be interpreted in this context. Comparison of senior trainees with junior trainees to ascertain if radiation use decreases initially in the earlier stages of training before plateauing would be interesting. Furthermore, we acknowledge that this may represent type-II error but identification of such a relationship was not a primary aim of the study.
The present study had two main limitations. First, we did not include radiation data for the 11 patients undergoing two simultaneous procedures, but this group accounted for 4.4% of the cohort. Second, analysis of injuries according to fracture classification or use of metal fixation results in some standardisation, but there is potential for some variation within each group. This scenario reflects the spectrum of injuries commonly encountered in standard practice, and which we believe is accounted for in our report of exposure ranges. Further research should focus on the analysis of preoperative predictors of increased exposure to radiation so that patients can be counselled adequately and modifiable risk factors corrected preoperatively.
Conclusions
Radiation exposure in the acute management of paediatric upper-limb trauma is dependent on injury type and the procedure being undertaken (though considerable variation can be expected for a given procedure). We have quantified the spectrum of radiation exposure encountered by multiple surgeons over the most commonly undertaken procedures. These findings may facilitate audit of practice and quantification of radiation-associated risks to patients. It may also serve as a basis for the development of protocols to review outlying cases and improve patient safety.
References
- 1.Randsborg PH, Gulbrandsen P, Saltyte BJ et al. Fractures in children: epidemiology and activity-specific fracture rates. J Bone Joint Surg Am 2013; : e42. [DOI] [PubMed] [Google Scholar]
- 2.Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma 1993; : 15–22. [DOI] [PubMed] [Google Scholar]
- 3.Noordeen MH, Shergill N, Twyman RS, Cobb JP, Briggs T. Hazard of ionizing radiation to trauma surgeons: reducing the risk. Injury 1993; : 562–564. [DOI] [PubMed] [Google Scholar]
- 4.Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg 2005; : 69–76. [DOI] [PubMed] [Google Scholar]
- 5.Cousins C. Radiological protection of the patient: an integral part of quality of care. Health Phys 2013; : 430–433. [DOI] [PubMed] [Google Scholar]
- 6.Tremains MR, Georgiadis GM, Dennis MJ. Radiation exposure with use of the inverted-c-arm technique in upper-extremity surgery. J Bone Joint Surg Am 2001; : 674–678. [DOI] [PubMed] [Google Scholar]
- 7.Eismann EA, Wall EJ, Thomas EC, Little MA. Direct beam radiation exposure to surgeons during pinning of supracondylar humerus fractures: does C-arm position and the attending surgeon matter? J Pediatr Orthop 2014; : 166–171. [DOI] [PubMed] [Google Scholar]
- 8.Hsu RY, Lareau CR, Kim JS et al. The effect of Carm position on radiation exposure during fixation of pediatric supracondylar fractures of the humerus. J Bone Joint Surg Am 2014; : e129. [DOI] [PubMed] [Google Scholar]
- 9.Soye JA, Paterson A. A survey of awareness of radiation dose among health professionals in Northern Ireland. Br J Radiol 2008; : 725–729. [DOI] [PubMed] [Google Scholar]
- 10.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959; : 145–154. [PubMed] [Google Scholar]
- 11.Berrington de GA, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004; : 345–351. [DOI] [PubMed] [Google Scholar]
- 12.Wall BF, Haylock R, Jansen JTM et al. Radiation risks from medical X-ray examinations as a function of the age and sex of the patient. Issued 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/340147/HPA-CRCE-028_for_website.pdf (cited 28 June 2016).
- 13.Department of Health Ionising radiation (medical exposure) regulations 2000 (IRMER) with notes on good practice. Issued 2012 www.gov.uk/government/uploads/system/uploads/attachment_data/file/227075/IRMER_regulations_2000.pdf (cited 28 June 2016).
- 14.European Council European Council Directive 2013/59/EURATOM. Laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation. OJ 2014; L13/1. [Google Scholar]
- 15.Carmichael JHE, Maccia C, Moores BM. European guidelines on quality criteria for diagnostic radiographic images Brussels: European Commission, 1996. [Google Scholar]
- 16.Hart D, Hillier MC, Shrimpton PC. Doses to patients from radiographic and fluoroscopic X-ray imaging procedures in the UK – 2012 review. Issued 2012 www.gov.uk/government/uploads/system/uploads/attachment_data/file/342780/HPA-CRCE-034_Doses_to_patients_from_radiographic_and_fluoroscopic_x_ray_imaging_procedures_2010.pdf (cited 28 June 2016). [Google Scholar]
- 17.Hart D, Hillier MC, Wall BF. National reference doses for common radiographic, fluoroscopic and dental X-ray examinations in the UK. Br J Radiol 2009; : 1–12. [DOI] [PubMed] [Google Scholar]
- 18.Bogaert E, Bacher K, Lemmens K et al. A large-scale multicentre study of patient skin doses in interventional cardiology: dose-area product action levels and dose reference levels. Br J Radiol 2009; : 303–312. [DOI] [PubMed] [Google Scholar]
- 19.Miller DL, Balter S, Cole PE et al. Radiation doses in interventional radiology procedures: the RAD-IR study: part I: overall measures of dose. J Vasc Interv Radiol 2003; : 711–727. [DOI] [PubMed] [Google Scholar]
- 20.Balter S, Cusma JT. Interventional fluoroscopy physics, technology, safety. New York: Wiley; 2001. [Google Scholar]
- 21.Stecker MS, Balter S, Towbin RB et al. Guidelines for patient radiation dose management. Vasc Interv Radiol 2009; : S263–S273. [DOI] [PubMed] [Google Scholar]